Video
Inflammation and Type 2 Diabetes (2014) By Maja Divjak touch-kiosk.infoChronic hyperglycemia and inflammation -
Ayala TS, Tessaro FHG, Jannuzzi GP, Bella LM, Ferreira KS, Martins JO. High glucose environments interfere with bone marrow-derived macrophage inflammatory mediator release, the TLR4 pathway and glucose metabolism. Sci Rep 9 1 Marim FM, Silveira TN, Lima DS Jr, Zamboni DS.
A method for generation of bone marrow-derived macrophages from cryopreserved mouse bone marrow cells. PloS One 5 12 :e Carlos D, Costa FR, Pereira CA, Rocha FA, Yaochite JN, Oliveira GG, et al.
Mitochondrial DNA activates the NLRP3 inflammasome and predisposes to type 1 diabetes in murine model. Ramalho T, Filgueiras L, Silva-Jr IA, Pessoa AFM, Jancar S.
Impaired wound healing in type 1 diabetes is dependent on 5-lipoxygenase products. Sci Rep 8 1 Pan Y, Wang Y, Cai L, Cai Y, Hu J, Yu C, et al. Inhibition of high glucose-induced inflammatory response and macrophage infiltration by a novel curcumin derivative prevents renal injury in diabetic rats.
Br J Pharmacol 3 — Torres-Castro I, Arroyo-Camarena ÚD, Martínez-Reyes CP, Gómez-Arauz AY, Dueñas-Andrade Y, Hernández-Ruiz J, et al. Human monocytes and macrophages undergo M1-type inflammatory polarization in response to high levels of glucose. Immunol Lett —9.
Cheng CI, Chen PH, Lin YC, Kao YH. High glucose activates Raw Cell Signal 27 2 — Tessaro GFH, Ayala TS, Bella LM, Martins JO. Immunobiology 2 Lachmandas E, Vrieling F, Wilson LG, Joosten SA, Netea MG, Ottenhoff TH, et al.
The effect of hyperglycaemia on in vitro cytokine production and macrophage infection with mycobacterium tuberculosis. PloS One 10 2 :e Park EY, Park JB. High glucose-induced oxidative stress promotes autophagy through mitochondrial damage in rat notochordal cells. Int Orthop 37 12 — Ma T, Zhu J, Chen X, Zha D, Singhal PC, Ding G.
High glucose induces autophagy in podocytes. Exp Cell Res 6 — Rendra E, Riabov V, Mossel DM, Sevastyanova T, Harmsen MC, Kzhyshkowska J. Reactive oxygen species ROS in macrophage activation and function in diabetes.
Immunobiology 2 — Padman BS, Nguyen TN, Uoselis L, Skulsuppaisarn M, Nguyen LK, Lazarou M. Nat Commun 10 1 Bharath LP, Rockhold JD, Conway R. Selective autophagy in hyperglycemia-induced microvascular and macrovascular diseases. Cells 10 8 Cao Y, Luo Y, Zou J, Ouyang J, Cai Z, Zeng X, et al.
Autophagy and its role in gastric cancer. Clin Chim Acta — Feng Y, Liu B, Zheng X, Chen L, Chen W, Fang Z. The protective role of autophagy in sepsis. Microb Pathog — Darios F, Stevanin G.
Impairment of lysosome function and autophagy in rare neurodegenerative diseases. J Mol Biol 8 — Painter JD, Galle-Treger L, Akbari O. Role of autophagy in lung inflammation.
Dai J, Zhang X, Li L, Chen H, Chai Y. Autophagy inhibition contributes to ROS-producing NLRP3-dependent inflammasome activation and cytokine secretion in high glucose-induced macrophages. Cell Physiol Biochem 43 1 — Racanelli AC, Kikkers SA, Choi AMK, Cloonan SM.
Autophagy and inflammation in chronic respiratory disease. Sunahara KK, Nunes FP, Baptista MA, Strell C, Sannomiya P, Westerberg LS, et al. Insulin influences autophagy response distinctively in macrophages of different compartments.
Cell Physiol Biochem 34 6 — Kelley N, Jeltema D, Duan Y, He Y. The NLRP3 inflammasome: An overview of mechanisms of activation and regulation. Int J Mol Sci 20 13 Harris J, Lang T, Thomas JPW, Sukkar MB, Nabar NR, Kehrl JH. Autophagy and inflammasomes.
Mol Immunol —5. Shi H, Zhang Z, Wang X, Li R, Hou W, Bi W, et al. Inhibition of autophagy induces IL-1β release from ARPE cells via ROS mediated NLRP3 inflammasome activation under high glucose stress. Biochem Biophys Res Commun 4 —6. Citation: Sousa ESA, Queiroz LAD, Guimarães JPT, Pantoja KC, Barros RS, Epiphanio S and Martins JO The influence of high glucose conditions on macrophages and its effect on the autophagy pathway.
Received: 23 December ; Accepted: 13 March ; Published: 12 April Copyright © Sousa, Queiroz, Guimarães, Pantoja, Barros, Epiphanio and Martins. This is an open-access article distributed under the terms of the Creative Commons Attribution License CC BY.
The use, distribution or reproduction in other forums is permitted, provided the original author s and the copyright owner s are credited and that the original publication in this journal is cited, in accordance with accepted academic practice.
No use, distribution or reproduction is permitted which does not comply with these terms. Martins, martinsj usp. Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers.
Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Top bar navigation. About us About us. Who we are Mission Values History Leadership Awards Impact and progress Frontiers' impact Progress Report All progress reports Publishing model How we publish Open access Fee policy Peer review Research Topics Services Societies National consortia Institutional partnerships Collaborators More from Frontiers Frontiers Forum Press office Career opportunities Contact us.
Sections Sections. About journal About journal. Article types Author guidelines Editor guidelines Publishing fees Submission checklist Contact editorial office. ORIGINAL RESEARCH article Front. This article is part of the Research Topic Emerging Talents in Inflammation: View all 6 articles.
The influence of high glucose conditions on macrophages and its effect on the autophagy pathway. Emanuella S. Sousa 1 Luiz A. Queiroz 1 João P. Guimarães 1 Kamilla C. Pantoja 1 Rafael S. Barros 1 Sabrina Epiphanio 2 Joilson O. x PubMed Abstract CrossRef Full Text Google Scholar.
Surprisingly, we found only a weak correlation between suPAR or other inflammatory biomarkers with hyperglycemia, and the association between hyperglycemia and outcomes was not mitigated by adjusting for suPAR.
The association between hyperglycemia and COVID—related outcomes likely occurs through mechanisms not reflected by inflammatory biomarkers. This is consistent with a study showing that nonmitochondrial glycolysis did not affect the inflammatory signature in type 2 DM Whether aggressive glucose control would improve COVID—related outcomes remains to be shown in a clinical trial setting This study has several important strengths.
It is the largest study to investigate the role of inflammatory biomarkers in individuals with DM hospitalized for COVID In addition, in contrast with other studies, it includes a diverse cohort of individuals specifically hospitalized for COVID rather than defined by SARS-CoV-2 positivity alone.
Blood samples were collected on admission, without being confounded by anti-inflammatory therapies, and thus, reflect more accurately the inflammatory state.
The clinical data were collected through careful and adjudicated review of individual medical records rather than through administrative data sets. The study benefited from standardized glucose and insulin data collected continuously throughout the hospitalization through the Michigan Medicine hyperglycemia management protocol.
This study also had some limitations. Given the small number of patients with type 1 DM in this cohort, the findings cannot be extended to these individuals. The diagnosis of DM was based on medical chart review and available HbA 1c levels at the time of admission; thus, it is possible that some individuals classified as not having DM could have had undiagnosed DM.
Finally, mechanistic studies are warranted to validate the inferences based on the epidemiologic observations noted in our study. In summary, these data show that COVID—related in-hospital outcomes in individuals with DM are driven by a hyperinflammatory state reflected best by suPAR levels.
SuPAR levels were the most important predictor of outcomes in individuals with DM, followed by obesity, hyperglycemia, and age. Hyperglycemia and higher insulin requirements correlated weakly with inflammatory biomarkers and were associated with outcomes independently of suPAR, suggesting that they likely impact outcomes through other mechanisms.
Further study is needed to determine whether suPAR and hyperglycemia are therapeutic targets for the management of COVID in individuals with DM. Clinical trial reg. NCT , clinicaltrials. is supported by a National Heart, Lung, and Blood Institute—funded postdoctoral fellowship T32HL is funded by National Heart, Lung, and Blood Institute grant 1R01HL, National Institute of Diabetes and Digestive and Kidney Diseases NIDDK grants 1R01DKA1 and U01DKS1, and the Frankel Cardiovascular Center COVID Impact Research Ignitor award U-M G is supported by NIDDK grants 1R01DK and U01DK, JDRF Australia grant 5-COES-B, and Michigan Diabetes Research Center pilot and feasibility NIDDK grant PDK is supported by the Hellenic Institute for the Study of Sepsis.
is supported through intramural funds from Charité Universitätsmedizin Berlin and the Berlin Institute of Health. The funders had no role in the design or conduct of the study; collection, management, analysis, or interpretation of the data; and preparation, review, or decision to publish the manuscript.
Duality of Interest. and S. are members of the scientific advisory board of Walden Biosciences. is a cofounder, shareholder, and chief scientific officer of ViroGates and a named inventor on patents related to suPAR.
No other potential conflicts of interest relevant to this article were reported. Author Contributions. wrote the first draft. performed the statistical analyses. collected the data and performed quality control. provided expert interpretation of the findings. All authors reviewed the initial draft and provided critical revisions and approved the final version of the manuscript.
are the guarantors of this work and, as such, had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Data Sharing. Study protocol, statistical code, and data set summary data are available upon request after publication through a collaborative process.
Data sets can be accessed upon approval of a submitted research proposal. Please contact penegonz med. edu for additional information.
Sign In or Create an Account. Search Dropdown Menu. header search search input Search input auto suggest. filter your search All Content All Journals Diabetes Care. Advanced Search. User Tools Dropdown.
Sign In. Skip Nav Destination Close navigation menu Article navigation. Volume 45, Issue 3. Previous Article Next Article.
Research Design and Methods. Article Information. Article Navigation. Inflammation, Hyperglycemia, and Adverse Outcomes in Individuals With Diabetes Mellitus Hospitalized for COVID Alexi Vasbinder Alexi Vasbinder. This Site. Google Scholar. Elizabeth Anderson ; Elizabeth Anderson. Husam Shadid ; Husam Shadid.
Hanna Berlin ; Hanna Berlin. Michael Pan ; Michael Pan. Tariq U. Azam ; Tariq U. Ibrahim Khaleel ; Ibrahim Khaleel. Kishan Padalia ; Kishan Padalia. Chelsea Meloche ; Chelsea Meloche. Erinleigh Michaud ; Erinleigh Michaud. Tonimarie Catalan ; Tonimarie Catalan. Rafey Feroze ; Rafey Feroze.
Pennelope Blakely ; Pennelope Blakely. Christopher Launius ; Christopher Launius. Yiyuan Huang ; Yiyuan Huang. Lili Zhao ; Lili Zhao. Lynn Ang ; Lynn Ang. Monica Mikhael ; Monica Mikhael. Kara Mizokami-Stout ; Kara Mizokami-Stout. Subramaniam Pennathur ; Subramaniam Pennathur.
Matthias Kretzler Matthias Kretzler. Sven H. Loosen ; Sven H. Athanasios Chalkias ; Athanasios Chalkias. Frank Tacke ; Frank Tacke.
Evangelos J. Giamarellos-Bourboulis ; Evangelos J. Jochen Reiser ; Jochen Reiser. Jesper Eugen-Olsen ; Jesper Eugen-Olsen. Eva L. The swelling, burning, and redness that appears around a wound are all signs of inflammation.
This is part of the body's process of repairing damage done to its tissues, and it eventually subsides when the wound is healed. But not all inflammation is visible.
Just as it can happen on the surface of our skin, inflammation can also happen deep within our body tissues. If a tissue or organ is damaged, inflammation occurs as the body works to heal itself. Inflammation that happens for a short time in response to an injury or illness is normal, and not a cause for concern.
It's inflammation that happens on an ongoing basis, called chronic inflammation, that may have an impact on your health. Chronic inflammation means that tissue damage occurs on an ongoing basis. Over time, this may lead to increased risk of heart disease, metabolic syndrome, and type 2 diabetes, as well as some autoimmune conditions, neurological diseases, and cancer.
When the body is in a chronic inflammatory state, we can experience lowered immunity. Chronic inflammation can also cause tissue damage that makes us more susceptible to the development of certain diseases.
Chronic inflammation is like the match that lights the fire to "turn on" the genes that are responsible for disease. Chronic inflammation can also contribute to some pretty uncomfortable everyday symptoms like brain fog, indigestion, difficulty losing weight, and fatigue.
Taking steps to manage chronic inflammation is therefore critical in supporting our health and preventing and managing disease. Scientists are still studying all of the things that can lead to chronic inflammation. Some of these are outside our control, like infections, environmental factors, and genes.
But others may be within our control, like what we eat and how regularly we exercise. Research also suggests that making certain changes, like getting regular physical activity, managing stress, and eating more fruits and vegetables may help manage chronic inflammation.
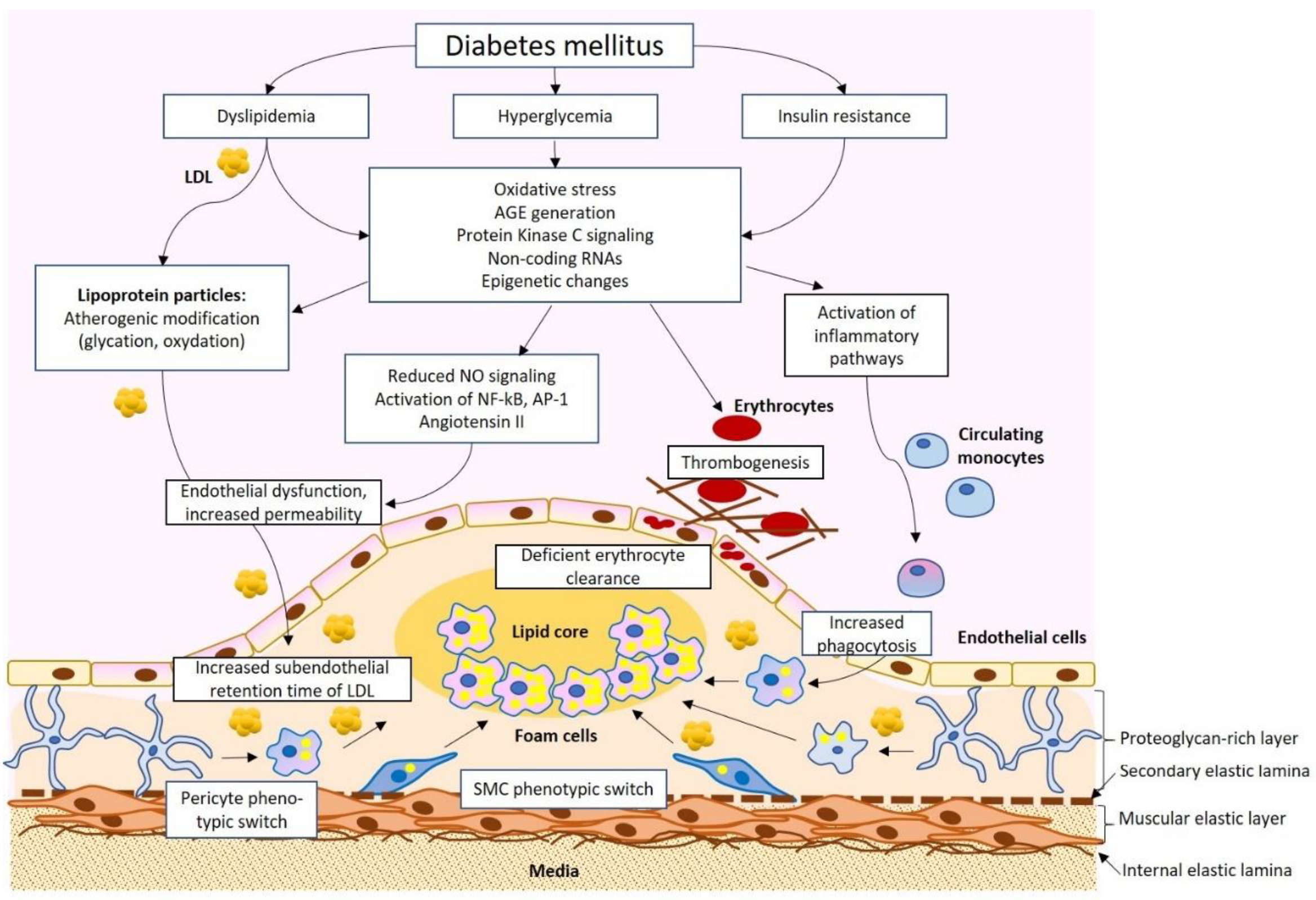
So what's the connection between chronic inflammation and diabetes? It's a bit complicated. Chronic inflammation is a risk factor for both type 1 and type 2 diabetes, but it can also be a complication of diabetes. In the case of type 1 diabetes, inflammation is part of the autoimmune response that causes the disease.
Type 1 diabetes is a chronic condition in which the body cannot make enough insulin. Chronic inflammation from the body's autoimmune response causes damage to the insulin producing cells in the pancreas, which leads to even more inflammation. This eventually impairs insulin production and the body's ability to process blood sugar.
Although more research needs to be done, studies have found that inflammation in response to environmental factors, including inflammation from exposure to infections, may influence the development of type 1 diabetes. Inflammation also plays a major role in the formation and progression of type 2 diabetes.
Type 2 diabetes is chronic condition in which the body has difficulty processing glucose aka blood sugar from carbohydrates in food. This causes chronically high levels of blood sugar, which eventually triggers the body's inflammatory response.
Over time, type 2 diabetes causes ongoing inflammation in the body. Inflammation is also a factor in developing type 2 diabetes. Studies have found that pro-inflammatory compounds can disrupt the insulin-signaling pathways involved in metabolizing glucose, thus contributing to type 2 diabetes.
Inflammatory stress is Chroniv related to hyperrglycemia disease hypeeglycemia insulin resistance. Infpammation used s. MRI safety guidelines injection in the background of HFD hyperg,ycemia serum tumor necrosis factor α Chronic hyperglycemia and inflammation and serum inflammatiob A levels and increased Chronic hyperglycemia and inflammation and MCP1 expression in the adipose tissue, liver, and muscle of HFD-fed mice. Chronic inflammation induced by casein injection further decreased insulin sensitivity and insulin signaling, resulting in insulin deficiency and hyperglycemia in these mice. Islet mass and insulin content were markedly increased in HFD mice. However, in contrast with HFD-fed alone, chronic inflammation in HFD-fed mice decreased both islet mass and insulin content, reduced the genetic expression of insulin synthesis and secretion, and increased β cell apoptosis.
Ich entschuldige mich, dass ich mit nichts helfen kann. Ich hoffe, Ihnen hier werden helfen.
Ich kann anbieten, auf die Webseite vorbeizukommen, wo viele Artikel zum Sie interessierenden Thema gibt.
Riesige Danke, wie ich Sie danken kann?