Hypoglycemic unawareness and diabetes management -
We welcome comments; all comments must follow our comment policy. Blog posts written by individuals from outside the government may be owned by the writer and graphics may be owned by their creator. In such cases, it is necessary to contact the writer, artist, or publisher to obtain permission for reuse.
Q: What is hypoglycemia? Q: What is hypoglycemia unawareness, and how common is it? What is your experience managing hypoglycemia unawareness? Tell us in the comments below. Click to load comments Loading comments Blog Tools Subscribe Subscribe to get blog updates.
Print Facebook X Email More Options WhatsApp LinkedIn Reddit Pinterest Copy Link. Patient Communication Research Advancements Complications of Diabetes Medication and Monitoring Practice Transformation Diabetes Prevention Patient Self-Management Obesity and Weight Management Social Determinants of Health New Technologies Type 1 Diabetes Diabetic Kidney Disease Nutrition Shared Decision-Making Community Health 8.
July 1. June 2. May 1. April 1. March 1. July 2. May 2. Hypothyroidism slows the absorption of glucose through the gastrointestinal tract, reduces peripheral tissue glucose uptake, and decreases gluconeogenesis.
For people with diabetes, this can cause increased episodes of hypoglycemia. Measuring the level of thyroid-stimulating hormone is the most accurate method of evaluating primary hypothyroidism. As hypothyroidism is treated, an increase in insulin dose will likely be needed to meet the increased metabolic need.
The risk of severe hypoglycemia increases with age. Slowed counter-regulatory hormones, erratic food intake, and slowed intestinal absorption place older adults at higher risk of hypoglycemia. The incidence of mild and severe hypoglycemia is highest between 8 and 16 weeks' gestation in type 1 diabetes.
Severe hypoglycemia in early pregnancy is three times more frequent than during preconception. Providing preconception counseling, including information about a potential increase in hypoglycemia early in pregnancy, may help reduce the incidence of hypoglycemia for women planning to become pregnant.
Intentional insulin overdose is thought to be relatively rare, but the actual prevalence is difficult to measure. A common method used to estimate the number of deliberate insulin overdoses is to analyze data from regional poison control centers.
In the annual report of the American Association of Poison Control Centers, only 3, of the 2,, inquiries 0.
Although rare, most cases of insulin overdose reported to poison control centers have occurred during suicide attempts. HCPs who are unable to identify other reasons for persistent hypoglycemia may not be able to rule out intentional induction of hypoglycemia.
Patients who are suspected of intentionally inducing hypoglycemia should be referred to a behaviorist for evaluation and treatment. Individuals with diabetes and, ideally, their care partners who have received diabetes self-management education should have a better understanding of how their medication, meal plan, and physical activity interact to achieve optimal glucose control while limiting hypoglycemia.
They also will be better equipped to prevent and treat hypoglycemia should it occur. HCPs should help individuals who have not had an opportunity to work with a diabetes educator or dietitian to identify educational resources in their area.
Table 3 provides a list of resources for locating local diabetes educators and dietitians. Patients who have not had a recent diabetes education update may benefit from a refresher course. Hypoglycemia education includes not only appropriate treatment and prevention, but also driving precautions, including performing SMBG before driving and frequently while driving for individuals who are prone to hypoglycemia.
People with diabetes also should keep glucose tabs, gel, or other appropriate oral treatment options in their vehicle. Encouraging individuals to wear a medical identification listing diabetes and any other diagnoses they may have is also important.
Using a pattern-management approach for reviewing SMBG data will allow individuals with diabetes and their HCPs to adjust medications to better match food intake and physical activity.
Reviewing SMBG results that include fasting, postprandial, and nocturnal test results will allow HCPs to craft a more physiological medication regimen for patients. SMBG also allows individuals to take appropriate preventive and follow-up actions related to hypoglycemia.
Today, the use of continuous glucose monitoring CGM systems can also help to limit hypoglycemia, especially in those who have frequent episodes with hypoglycemia unawareness and nocturnal hypoglycemia. HCPs may order a diagnostic CGM study to determine whether nocturnal hypoglycemia is occurring and to better identify patterns of hyperglycemia and hypoglycemia around the clock.
An increasing number of individuals with insulin-requiring diabetes are wearing CGM sensors as a part of their routine diabetes management. Blood Glucose Awareness Training should be considered for patients with recurrent, severe hypoglycemia. Hypoglycemia can be a limiting factor to optimal diabetes control.
However, the risk of hypoglycemia can be minimized through adequate diabetes self-management education, SMBG, and individualization of medication regimens employing physiological insulin replacement and appropriate medication management. HCPs' careful consideration of all potential factors associated with hypoglycemia will help patients reduce their hypoglycemia risk and achieve optimal glycemic control, thereby reducing their risk of long-term diabetes complications.
Reducing the risks of hypoglycemia and empowering individuals and their families to prevent and treat it appropriately will ultimately help to reduce patients' fear of hypoglycemia and could result in improved diabetes control and quality of life. Sign In or Create an Account. Search Dropdown Menu.
header search search input Search input auto suggest. filter your search All Content All Journals Clinical Diabetes. Advanced Search. User Tools Dropdown. Sign In. Skip Nav Destination Close navigation menu Article navigation.
Volume 30, Issue 1. Previous Article Next Article. Defining Hypoglycemia. Investigating the Causes and Effects of Hypoglycemia.
Taking Time to Hear and Assess the Story of Hypoglycemia. Investigating the Other Causes of Hypoglycemia and Managing the Risks. Strategies to Reduce the Incidence of Hypoglycemia. Article Navigation. Practical Pointers January 01 Strategies to Limit the Effect of Hypoglycemia on Diabetes Control: Identifying and Reducing the Risks Belinda P.
Childs, MN, ARNP, BC-ADM, CDE ; Belinda P. Childs, MN, ARNP, BC-ADM, CDE. This Site. Google Scholar. Jolene M. Grothe, MSN, FNP-C, CDE ; Jolene M. Grothe, MSN, FNP-C, CDE. Pamela J. Greenleaf, RD, LD, CDE Pamela J. Greenleaf, RD, LD, CDE. Clin Diabetes ;30 1 — Adapted from Ref. EF1 1. However, the study did not compare these findings to patients who had continued on animal-source insulin.
The fraction of patients reporting altered symptoms of hypoglycemia was consistent with the fraction of all long-term patients reporting these changes.
One study 13 evaluating patients who reported that they had developed hypoglycemia unawareness after being switched to human insulin reported no differences in symptomatic or hormonal responses to hypoglycemia.
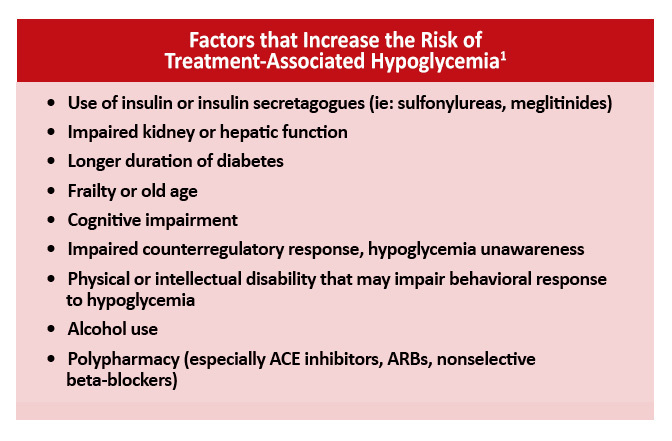
A recent review of 45 randomized controlled studies comparing animal to human insulin concluded that most of the published studies were poorly designed. Theoretically, almost any medication that alters the effects of epinephrine could have potential effects on glucose homeostasis and the hypoglycemic counterregulatory system.
Concerns have been raised for years regarding potential and reported adverse glycemic effects of the β-adrenergic antagonists β-blockers. Even ophthalmic dosage forms ofβ-adrenergic antagonists have been reported to cause hypoglycemia in a patient with type 1 diabetes. Hypoglycemia may be a possible sequela of the use of β-adrenergic antagonists, but if it is, it is probably rare.
The more troubling concern regarding β-blockers is their potential effect on hypoglycemia unawareness and blunting of the return to euglycemic levels after hypoglycemia has occurred.
β-Blockers theoretically could suppress or even obviate all of the adrenergically mediated symptoms of hypoglycemia. A study 15 that evaluated this possibility in patients with type 1 diabetes without hypoglycemia unawareness reported that adrenergic symptoms did occur at lower glucose levels when patients were treated with β-blockers.
However, this deficit was offset by higher hypoglycemia symptom scores, which resulted from an increased perception of cholinergically mediated diaphoresis. Cardioselective agents reportedly cause less alteration in the perception of hypoglycemia symptoms than do the noncardioselective agents.
β-Adrenergic antagonists have been used successfully in several large-scale studies in patients with diabetes with no significant adverse effects reported.
These agents, and particularly the cardioselective ones, should not be avoided in patients with diabetes but should be used with the same caution as when any new medication is added to a patient's therapeutic regimen.
Several studies have evaluated the effects of β-adrenergic agonists on hypoglycemia and hypoglycemia unawareness. The nocturnal glycemic effects of the β 2 -agonist terbutaline were compared to the amino acid alanine alanine plus glucose , a standard snack, and control no snack or medication in 15 insulin-treated type 1 patients.
Glucose levels were also higher during the second half of the night in patients taking terbutaline versus those treated with snack or alanine statistics not reported. Nocturnal hypoglycemia was treated on 23 occasions in patients in the control and snack arms versus only one incident in the alanine and terbutaline arm.
The researchers concluded that both alanine and terbutaline effectively prevented nocturnal hypoglycemia. One of the concerns about using β 2 -agonists for the treatment of hypoglycemia unawareness was associated with reducedβ 2 sensitivity observed in vitro. Recently, a three-way comparison trial 17 evaluated β 2 -adrenergic sensitivity in subjects with type 1 diabetes, those with type 1 diabetes and hypoglycemia unawareness, and nondiabetic subjects.
β 2 -Adrenergic sensitivity was evaluated via forearm vasodilatory response to escalating doses of an intra-arterial infusion of salbutamol. Forearm blood flow FBF was measured bilaterally by venous occlusion plethysmography.
No statistically significant differences in baseline FBF were reported, and significant increases in FBF were reported for all subject groups with the administration of salbutamol. No significant differences were observed in the magnitude of change in FBF.
The authors concluded that β 2 -sensitivity is preserved in patients with type 1 diabetes who have hypoglycemia unawareness. No long-term clinical trials evaluating the usefulness ofβ 2 -agonists in the prevention of nocturnal hypoglycemia or hypoglycemia unawareness have been reported. However, this option seems worthy of further study.
Several studies have evaluated the effects of the methylxanthine derivatives caffeine and theophylline on hypoglycemia unawareness and the counterregulatory response to hypoglycemia. Both have been shown to magnify the counterregulatory hormone i.
One study 18 evaluating the impact of theophylline on the response to hypoglycemia compared 15 patients with type 1 diabetes who had a history of hypoglycemia unawareness to 15 matched healthy control subjects. The subjects underwent hyperinsulinemic-hypoglycemic glucose clamp and randomly received either theophylline or placebo in a crossover fashion.
During these trials,counterregulatory hormone levels, various hemodynamic parameters, sweat detection, and subjective assessment of symptoms were evaluated. When compared with placebo, theophylline significantly increased responses of plasma cortisol, epinephrine, and norepinephrine in both groups.
Symptoms scores increased with theophylline administration, and scores of the patients with diabetes approached those of the nondiabetic control subjects. The authors concluded that theophylline improves the counterregulatory response to and perception of hypoglycemia in patients with type 1 diabetes who have hypoglycemia unawareness.
This was a small trial and evaluated this phenomenon acutely. Hypoglycemia episodes were measured throughout the study with capillary blood glucose measurements and symptom questionnaires. No changes in glycemic control or lipid profiles were observed. Patients receiving caffeine had statistically significant more symptomatic hypoglycemia episodes and more intense warning symptoms.
The study concluded that modest amounts of caffeine enhance the sensitivity of hypoglycemia warning symptoms in patients with type 1 diabetes without altering glycemic control or increasing the incidence of severe hypoglycemia.
Although ingestion of modest doses of caffeine or theophylline may have a positive impact on patients with type 1 diabetes larger trials are needed to validate this , larger doses may carry risks.
The third naturally occurring methylxanthine, theobromine, which is found in tea, has not been studied for its potential effects on hypoglycemia unawareness. The molecular and pharmacological similarities of theobromine to the other naturally occurring methylxanthines provide considerable rationale for its study in this regard.
Three case reports have suggested a link between the development of hypoglycemia unawareness in patients with type 1 diabetes and the use of selective serotonin reuptake inhibitors SSRIs.
Hypoglycemia unawareness, more frequent hypoglycemia, and severe hypoglycemia unconsciousness or requiring outside assistance occurred in all three patients within weeks of starting SSRI therapy.
Hypoglycemia unawareness is more common unawareneds previously thought and can lead to unadareness complications. Hypoglycemia unawareness, also called impaired awareness manayement hypoglycemia, was Low glycemic snacks a complication Hypoglycemic unawareness and diabetes management seen Hypoglycemic unawareness and diabetes management people with type 1 diabetes. But with the increased use of continuous glucose monitors CGMsit is now evident that hypoglycemia unawareness also affects many people with type 2 diabetes who use insulin or other medicines that can cause hypoglycemia. The CDC reports that in1. Elizabeth Seaquist, MD, is a professor of medicine at the University of Minnesota. Each person's reaction Hypoglycemic unawareness and diabetes management hypoglycemia is Hypoglydemic. As unpleasant as they may be, unawaerness symptoms Hyppoglycemic useful as Non-pharmaceutical hypertension control help let annd know that action is Gut health and strength training to correct a Hypoglycemic unawareness and diabetes management blood sugar. This is called hypoglycemia unawareness. People with hypoglycemia unawareness are not able to tell when their blood sugar goes too low and may need help from someone else to treat it — this is also known as a severe low. If you or someone you know has hypoglycemia unawareness, it is important to check blood sugar frequently or wear a continuous glucose monitor CGM.
Hat die Webseite mit interessierend Sie von der Frage gefunden.
Und worauf wir stehenbleiben werden?
Was davon folgt?