
Video
Metabolism - GlycogenesisCarbohydrate metabolism and glycogen breakdown -
Your Access profile is currently affiliated with '[InstitutionA]' and is in the process of switching affiliations to '[InstitutionB]'. This div only appears when the trigger link is hovered over.
Otherwise it is hidden from view. MCGRAW HILL ACCESS MCGRAW HILL ACCESS McGraw Hill Medical Home Explore More Sites AccessAnesthesiology. AccessBiomedical Science. AccessEmergency Medicine. Case Files Collection.
Clinical Sports Medicine Collection. Davis AT Collection. Davis PT Collection. Murtagh Collection. MY PROFILE.
Access Sign In Username. Sign In. Create a Free Access Profile Forgot Password? Forgot Username? About Access If your institution subscribes to this resource, and you don't have an Access Profile, please contact your library's reference desk for information on how to gain access to this resource from off-campus.
Learn More. Sign in via OpenAthens Sign in via Shibboleth. We have a new app! Close Promo Banner. Keyword Title Author ISBN Select Site. Autosuggest Results Please Enter a Search Term. About Search. Enable Autosuggest.
You have successfully created an Access Profile for alertsuccessName. Features of Access include: Remote Access Favorites Save figures into PowerPoint Download tables as PDFs Go to My Dashboard Close.
Training increases GLUT4 content in skeletal muscles, which contributes to improved insulin sensitivity Houmard et al.
A rather consistent finding is that glycogen content is higher in skeletal muscles from trained subjects and training increases glycogen content Burgomaster et al. The glycogen stores are also refilled 24 h after exercise Costill et al. Indeed, the fact that glycogen content is increased in skeletal muscles after training may result from increased insulin sensitivity.
From an evolutional point of view such increase in glycogen content may reflect an important adaptation: high skeletal muscles glycogen content improves the chance for survival in emergencies.
Decreasing glycogen content by exercise or fasting stimulates glycogen accumulation to levels above the glycogen content in well-fed conditions Hespel and Richter, ; Jensen et al. It is possible to increase the glycogen content in skeletal muscles if they are exposed to high concentrations of insulin and glucose Richter et al.
Why does glycogen content not increase when high amount of carbohydrates are ingested under normal physiological conditions? Why is the excess carbohydrate ingested converted to lipid without elevation of glycogen content in skeletal muscles? The glycogen content in skeletal muscles will reflects a balance between available glucose and insulin sensitivity in skeletal muscles.
Studies in rats have under controlled conditions shown that training increases expression of GLUT4, but insulin sensitivity is not elevated in skeletal muscles because glycogen content also increases Kawanaka et al. The acute adaptation to training is, therefore, higher glycogen content but stable insulin sensitivity.
From an evolutional point of view, this indicates that high glycogen content is more important than high insulin sensitivity. Prolonged training increases insulin sensitivity beyond the last training session, and insulin sensitivity correlates with oxidative capacity in skeletal muscles Bruce et al.
GLUT4 expression in skeletal muscles also regulates insulin sensitivity and correlates with rate of glycogen resynthesis Hickner et al. Interestingly, 24 h fasting GLUT4 content was elevated in fast-twitch epitrochlearis muscles where glycogen content was reduced Jensen et al.
In soleus slow-twitch muscle , glycogen content was minimally affected by 24 h fasting and GLUT4 was unchanged Lai et al. These findings support that replenishment of glycogen store is superior to elevated insulin sensitivity. Blood glucose concentration can be regulated in vivo even when skeletal muscle glycogen synthesis is impaired by short-term overeating Acheson et al.
Genetic findings support that skeletal muscle glycogen synthesis is not an absolute requirement for regulation of blood glucose concentration. Knockout mice lacking the skeletal muscle isoform of glycogen synthase have normal insulin sensitivity Pederson et al.
In human, a child without glycogen synthase has been described, and also this person had a normal glucose response to an oral glucose tolerance test Kollberg et al. Glycogen resynthesis is an important part of restitution after training and athletes optimize glycogen synthesis by intake of high amount of carbohydrates immediately after exercise Ivy, The energy source for rapid glycogen synthesis is blood glucose and rapid extraction of glucose from the blood is required for high rate of glycogen synthesis.
Diabetes subjects have impaired removal of blood glucose, because insulin-stimulated glycogen synthesis is impaired Shulman et al. Exercise-stimulated glycogen breakdown will stimulate skeletal muscle glycogen synthesis and extraction of blood glucose and increase insulin sensitivity.
Such increased insulin sensitivity may be secondary to replenishing glycogen stores in the context of survival. However, in the modern society, the increased insulin sensitivity after exercise may have its superior role to prevent development of insulin resistance and type 2 diabetes.
Glycogen content has a strong feedback inhibition of glycogen synthase activity Danforth, and the glycogen stores are limited. It is not possible to dispose glucose into glycogen when stores are filled and under such condition, glucose remains in the blood until it is utilized as energy or transformed into lipid.
Skeletal muscles have a crucial role for regulation of whole body glucose metabolism, but acute elevation of glycogen does not impair insulin signaling and insulin-stimulated glucose transport may be normal Jensen et al.
However, insulin-stimulated glycogen synthesis is decreased, and more glucose is metabolized via glycolysis and we suggest that such increased glucose metabolism in skeletal muscles is unhealthy. Insulin signaling and insulin-stimulated glucose transport are impaired in muscles from rats and humans showing manifest insulin resistance or type 2 diabetes Etgen et al.
However, such insulin resistance develops gradually. The mechanisms for development of insulin resistance in skeletal are not well-understood, but accumulation of lipid and lipid intermediates are likely contributors Aas et al.
Furthermore, energy surplus increases production of reactive oxidative spices Hoehn et al. The production of ROS is increased when high amount of glucose and fat is supplied the mitochondria simultaneously and forces electrons into the electron transport chain Hue and Taegtmeyer, Preventing ROS production in skeletal muscles protects skeletal muscles form developing insulin resistance Hoehn et al.
Insulin resistant muscles are characterized with numerous changes e. In skeletal muscles with low glycogen, glucose will be stored as muscles glycogen Ivy, ; Hickner et al.
A major concern for athletes after strenuous training is to replete the glycogen stores is skeletal muscles preparing for new training sessions or competitions. Skeletal muscles are able to extract blood glucose effectively when high amount of carbohydrate are supplied Ivy, , and we suggest that glucose disposal into skeletal muscle glycogen is healthy storage of carbohydrates.
Indeed, healthy humans have large capacity to store glucose as lipid Figure 2. Acheson et al. Importantly, de novo lipid synthesis occurred without development of hyperglycemia, but blood triglyceride content increased fold Acheson et al.
Accumulation of fat per se does not cause insulin resistance Haemmerle et al. Figure 2. Excess energy intake is stored after meals as glycogen and triacylglycerols.
Carbohydrate can be stored as glycogen mainly in skeletal muscles or the liver; fat is manly stores as triacylglycerol in adipose tissue. With filled glycogen stores, glucose can be the substrate for de novo lipid synthesis and stored in adipocytes, muscles, or the liver and cause insulin resistance.
Glycogen and fat are important energy substrates during exercise. Accumulation of lipid intermediates seems to occur secondary to increased glycogen content and acute exercise reduces lipid synthesis during glucose loads Figure 2.
Moreover, it has been reported that insulin resistant subjects stores a larger part of ingested glucose as lipid in skeletal muscles and liver compared to insulin sensitive subjects, whereas skeletal muscles glycogen synthesis is lower in insulin resistant subjects Petersen et al.
A reduced capacity to store glucose as glycogen promotes de novo lipogenesis, which will deteriorate of insulin sensitivity due to lipid accumulation. In the modern society, abundant food and inactivity are large challenges for humans, and metabolic diseases related to obesity deteriorate public health.
Although the improved insulin sensitivity after glycogen depleting exercise may not have evolved to improve regulation of blood glucose, such effect of exercise may be the mechanism that protect humans from developing type 2 diabetes in the modern society.
We suggest that dynamic glycogen metabolism is important for healthy regulation of blood glucose and prevention of insulin resistance. The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Aas, V. Lipid metabolism in human skeletal muscle cells: effects of palmitate and chronic hyperglycaemia. Acta Physiol. Pubmed Abstract Pubmed Full Text CrossRef Full Text. Acheson, K. Glycogen storage capacity and de novo lipogenesis during massive carbohydrate overfeeding in man.
Pubmed Abstract Pubmed Full Text. Alessi, D. Mechanism of activation and function of protein kinase B. Arias, E. Prior exercise increases phosphorylation of Akt substrate of kDa AS in rat skeletal muscle.
Aslesen, R. Glucose uptake and metabolic stress in rat muscles stimulated electrically with different protocols. Effects of epinephrine on glucose metabolism in contracting rat skeletal muscle. Åstrand, P. Textbook of Work Physiology. New York: McGraw-Hill Book Company, 1— Bergström, J.
Diet, muscle glycogen and physical performance. Muscle glycogen synthesis after exercise: an enhancing factor localized to the muscle cells in man.
Nature , — Betts, J. Short-term recovery from prolonged exercise: exploring the potential for protein ingestion to accentuate the benefits of carbohydrate supplements. Sports Med. Boushel, R. Muscle mitochondrial capacity exceeds maximal oxygen delivery in humans.
Mitochondrion 11, — Bouskila, M. Insulin promotes glycogen synthesis in the absence of GSK3 phosphorylation in skeletal muscle. Allosteric regulation of glycogen synthase controls glycogen synthesis in muscle. Cell Metab. Brady, M. Allosteric trumps covalent in the control of glycogen synthesis.
Bruce, C. Muscle oxidative capacity is a better predictor of insulin sensitivity than lipid status. Burgomaster, K. Similar metabolic adaptations during exercise after low volume sprint interval and traditional endurance training in humans. Six sessions of sprint interval training increases muscle oxidative potential and cycle endurance capacity in humans.
Cartee, G. Prolonged increase in insulin-stimilated glucose transport in muscle after exercise. Chasiotis, D. Regulation of glycogenolysis in human muscle in response to epinephrine infusion.
Christ, C. Exercise training improves muscle insulin resistance but not insulin receptor signaling in obese Zucker rats. Christ-Roberts, C. Exercise training increases glycogen synthase activity and GLUT4 expression but not insulin signaling in overweight nondiabetic and type 2 diabetic subjects.
Metabolism 53, — Cleasby, M. Functional studies of Akt isoform specificity in skeletal muscle in vivo; maintained insulin sensitivity despite reduced insulin receptor substrate-1 expression. Cohen, P.
Dissection of the protein phosphorylation cascades involved in insulin and growth factor action. The origins of protein phosphorylation. Cell Biol. Connett, R. Exercise: Regulation and Integration of Multiple System , eds L. Rowell and J. Shepherd Bethesda, MD: American Physiological Society , — Cori, C.
The mechanism of epinephrine action. The influence of epinephrine on the carbohydrate metabolism of fasting rats, with a note on new formation of carbohydrates. Costill, D. The role of dietary carbohydrates in muscle glycogen resynthesis after strenuous running.
Coyle, E. Muscle glycogen utilization during prolonged strenuous exercise when fed carbohydrate. Danforth, W. Glycogen synthase activity in skeletal muscle. DeFronzo, R. Synergistic interaction between exercise and insulin on peripheral glucose uptake. CrossRef Full Text. The effect of insulin on the disposal of intravenous glucose.
Results from indirect calorimetry and hepatic and femoral venous catheterization. Diabetes 30, — Dela, F. GLUT 4 and insulin receptor binding and kinase activity in trained human muscle. Derave, W. Muscle glycogen content affects insulin-stimulated glucose transport and protein kinase B activity.
Contraction-stimulated muscle glucose transport and GLUT-4 surface content are dependent on glycogen concentration. Esbjornsson-Liljedahl, M. Smaller muscle ATP reduction in women than in men by repeated bouts of sprint exercise.
Metabolic response in type I and type II muscle fibers during a s cycle sprint in men and women. Etgen, G. Exercise training reverses insulin resistance in muscle by enhanced recruitment of GLUT-4 to the cell surface.
Glucose transport and cell surface GLUT-4 protein in skeletal muscle of the obese Zucker rat. Franch, J. Regulation of glycogen synthesis in rat skeletal muscle after glycogen depleting contractile activity: effects of adrenaline on glycogen synthesis and activation of glycogen synthase and glycogen phosphorylase.
Acyl-CoA binding protein expression is fibre type specific and elevated in muscles from obese insulin-resistant Zucker rat. Diabetes 51, — Frayn, K. Calculation of substrate oxidation rates in vivo from gaseous exchange. Frosig, C.
Effects of endurance exercise training on insulin signaling in human skeletal muscle: interactions at the level of phosphatidylinositol 3-kinase, Akt, and AS Diabetes 56, — Gibala, M. Short-term sprint interval versus traditional endurance training: similar initial adaptations in human skeletal muscle and exercise performance.
Gjedsted, J. Effects of adrenaline on lactate, glucose, lipid and protein metabolism in the placebo controlled bilaterally perfused human leg.
Greiwe, J. Effects of endurance exercise training on muscle glycogen accumulation in humans. Haemmerle, G. Defective lipolysis and altered energy metabolism in mice lacking adipose triglyceride lipase.
Science , — Hawley, J. Carbohydrate-loading and exercise performance. An update. He, J. Muscle glycogen content in type 2 diabetes mellitus. Heath, G. III, Hinderliter, J. Effects of exercise and lack of exercise on glucose tolerance and insulin sensitivity.
Hermansen, L. Muscle glycogen during prolonged severe exercise. Hespel, P. Glucose uptake and transport in contracting, perfused rat muscle with different pre-contraction glycogen concentrations.
ChREBP was initially known as Williams-Beuren syndrome critical region 14 WBSCR14 and was considered one of the potential genes that instigate Williams-Beuren syndrome.
Later, by using a carbohydrate response element ChoRE from L-PK, ChREBP was isolated as a bona fide transcription factor for binding ChoRE of glycolytic promoters. A recent report indeed suggested a role for LXR in the transcriptional activation of ChREBP in response to glucose, although the study needs to be further verified because the transcriptional response is shown not only by the treatment of D-glucose, a natural form of glucose present in animals, but also by the treatment of unnatural L-glucose, a form of glucose that is not known to activate lipogenesis in the liver.
PKA is shown to phosphorylate serine , which is critical for cellular localization, and threonine , which is critical for its DNA binding ability, whereas AMPK phosphorylate serine dictates its DNA binding ability.
All three sites are phosphorylated under fasting conditions by these kinases and are dephosphorylated under feeding by xylulose 5-phosphate X5P -mediated activity of protein phosphatase 2A PP2A.
First, high glucose concentrations in primary hepatocytes do not result in decreased cAMP levels or PKA activity, suggesting that other signals might be necessary to mediate the high glucose-dependent nuclear translocation of ChREBP. ChREBP knockout mice were born in a Mendelian ratio and showed no developmental problems.
The knockout animals showed reduced liver triacylglycerol levels together with a reduction in lipogenic gene expression, thus confirming the role of ChREBP in the control of hepatic glycolysis and fatty acid synthesis.
Prolonged fasting or starvation induces de novo glucose synthesis from non-carbohydrate precursors, termed hepatic gluconeogenesis.
This process initiates from the conversion of pyruvate to oxaloacetate by pyruvate carboxylase PC in the mitochondria and eventually concludes in the conversion into glucose via several enzymatic processes in the cytosol.
Key regulatory enzymes in that pathway, including glucose 6-phosphatase G6Pase , fructose 1,6-bisphosphatase Fbpase1 , PC, and phosphoenolpyruvate carboxykinase PEPCK , are activated under fasting conditions to enhance gluconeogenic flux in that setting.
Mitochondrial acetyl-CoA derived from the increased fatty acid oxidation under fasting functions as a key allosteric activator of PC, leading to the increased production of oxaloacetate for the gluconeogenesis. In addition, F26BP, which is a key allosteric regulator for glycolysis by activating PFK-1, was shown to inhibit gluconeogenesis via the allosteric inhibition of Fbpase1, which helps reciprocally control gluconeogenesis and glycolysis under different dietary statuses.
Because Fbpase2 is activated but PFK-2 is inhibited under fasting, the lack of F26BP enables the activation of Fbpase1 and the increased production of fructose 6-phosphate in gluconeogenesis.
The chronic activation of gluconeogenesis is ultimately achieved via transcriptional mechanisms. Major transcriptional factors that are shown to induce gluconeogenic genes include CREB, FoxO1, and several nuclear receptors Figure 3. Regulation of hepatic gluconeogenesis.
Under fasting conditions, hepatic gluconeogenesis is enhanced via a decreased concentration of insulin and an increased concentration of insulin counterregulatory hormones such as glucagon. FoxO1, forkhead box O 1. Under fasting conditions, glucagon and epinephrine can increase the cAMP concentration in the liver via the activation of adenylate cyclase, leading to the activation of PKA and the subsequent induction of CREB via its serine phosphorylation.
In contrast, the role for CBP in gluconeogenesis is still controversial. Disruption of CREB-CBP interaction does not appear to affect glucose homeostasis because mice exhibiting a stable expression of mutant CBP that was unable to bind CREB showed normal glycemia.
The CRTC family of transcriptional coactivators consists of CRTC1, CRTC2 and CRTC3, which were isolated by the expression library screening as activaters of CREB-dependent transcription.
Recent studies have delineated the role of CRTC2 in the regulation of hepatic gluconeogenesis in vivo. Knockdown of CRTC2 in mice by RNAi reduced blood glucose levels and led to a concomitant repression of gluconeogenic gene expression. The forkhead box O FoxOs belongs to a class of forkhead families of transcription, which recognize the AT-rich insulin response element on the promoter.
Peroxisome proliferator-activated receptor gamma coactivator 1 alpha PGC-1α , a known coactivator for nuclear receptors, functions as a key transcriptional coactivator for FoxO1 in hepatic gluconeogenesis.
In this case, PRMT1 promotes the asymmetric dimethylation of arginine and in FoxO1, which blocks the binding of Akt and the subsequent Akt-mediated phosphorylation of the adjacent serine residue serine , thus enhancing the nuclear localization of FoxO1.
Nuclear receptors belong to the superfamily of transcription factors that possess two Cys2-His2 type zinc finger motifs as a DNA binding domain as well as both ligand-independent and ligand-dependent transactivation domains. Nuclear receptors can be classified into one of three subgroups based on their dimer-forming potential.
Homodimeric nuclear receptors are also called cytosolic receptors because they reside in the cytosol and associate with molecular chaperones such as heat-shock proteins. On binding to the ligand, they form homodimers and translocate to the nucleus to bind a specific response element termed the hormone response element to elicit the ligand-dependent transcriptional response.
Most of the steroid hormone receptors, such as the glucocorticoid receptor GR , estrogen receptor ER , and progesterone receptor PR , belong to this subfamily. By contrast, heterodimeric nuclear receptors reside in the nucleus and are bound to their cognate binding sites together with the universal binding partner retinoid X receptor RXR.
Examples of this class of nuclear receptors include members of peroxisome proliferator-activated receptors, LXRs, vitamin D receptors and thyroid hormone receptors. The final subclasses of nuclear receptors are types that function as monomers. They usually lack specific endogenous ligands and are often called orphan nuclear receptors.
Some of them also lack DNA binding domain and thus function as transcriptional repressors of various transcription factors, including members of nuclear receptors. They are called atypical orphan nuclear receptors. Among the homodimeric nuclear receptors, the role of GR has been linked to the control of hepatic gluconeogenesis.
GR is activated by cortisol, which is released from the adrenal cortex in response to chronic stresses such as prolonged fasting. The same response elements were also shown to be recognized and regulated by hepatocyte nuclear factor 4 HNF4 , a member of heterodimeric nuclear receptors, which suggests that these nuclear receptors could coordinately function to control hepatic gluconeogenesis in response to fasting.
In accordance with this idea, the activity of these nuclear receptors can be effectively integrated by the function of transcriptional co-activator PGC-1α. Recently, estrogen-related receptor gamma ERRγ , a member of monomeric nuclear receptors, was shown to be involved in the regulation of hepatic gluconeogenesis.
This factor regulates hepatic gluconeogenesis by binding to unique response elements that are distinct from the known nuclear receptor-binding sites in the promoters of PEPCK and G6Pase. Inhibition of ERRγ activity by injecting either RNAi or the inverse agonist GSK effectively reduced hyperglycemia in diabetic mice, suggesting that the control of this factor might potentially be beneficial in the treatment of patients with metabolic diseases.
As is the case for other nuclear receptors that control hepatic gluconeogenesis, ERRγ activity is further enhanced by interaction with the transcriptional coactivator PGC-1α, showing that this coactivator functions as a master regulator for the hepatic glucose metabolism.
Three members of atypical orphan nuclear receptors, the small heterodimer partner SHP, also known as NR0B2 ; the dosage-sensitive sex reversal, adrenal hypoplasia critical region, on chromosome X DAX-1, also known as NR0B1 ; and the SHP-interacting leucine zipper protein SMILE are implicated in the transcriptional repression of hepatic gluconeogenesis.
Interestingly, metformin directly activates the transcription of SHP via an AMPK-mediated pathway. SHP directly inhibits cAMP-dependent transcription by binding to CREB, resulting in the reduced association of CREB with CRTC2. These results provide a dual mechanism for a metformin-AMPK dependent pathway to inhibit hepatic gluconeogenesis at the transcriptional level; an acute regulation of CRTC2 phosphorylation to inhibit the CRTC2-CREB-dependent transcriptional circuit; and a longer-term regulation of gluconeogenic transcription by enhanced SHP expression.
Both DAX-1 and SMILE were shown to repress hepatic gluconeogenesis by inhibiting HNF4-dependent transcriptional events. Interestingly, SMILE was shown to directly replace PGC-1α from HNF4 and the gluconeogenic promoters, suggesting that this factor could potentially function as a major transcriptional repressor of hepatic gluconeogenesis in response to insulin signaling.
Further study is necessary to fully understand the relative contribution of these nuclear receptors in the control of glucose homeostasis in both physiological conditions and pathological settings.
In this review, we attempted to describe the current understanding of the regulation of glucose metabolism in the mammalian liver.
Under feeding conditions, glucose, a major hexose monomer of dietary carbohydrate, is taken up in the liver and oxidized via glycolysis. The excess glucose that is not utilized as an immediate fuel for energy is stored initially as glycogen and is later converted into triacylglycerols via lipogenesis.
Glycogenesis is activated via the insulin-Akt-mediated inactivation of GSK-3, leading to the activation of glycogen synthase and the increased glycogen stores in the liver. Insulin is also critical in the activation of PP1, which functions to dephosphorylate and activate glycogen synthase.
Glycolysis is controlled by the regulation of three rate-limiting enzymes: GK, PFK-1 and L-PK. The activities of these enzymes are acutely regulated by allosteric regulators such as ATP, AMP, and F26BP but are also controlled at the transcription level.
Two prominent transcription factors are SREBP-1c and ChREBP, which regulate not only the aforementioned glycolytic enzyme genes but also the genes encoding enzymes for fatty acid biosynthesis and triacylglycerol synthesis collectively termed as lipogenesis.
The importance of these transcription factors in the control of glycolysis and fatty acid biosynthesis has been verified by knockout mouse studies, as described in the main text. The liver also has a critical role in controlling glucose homeostasis under fasting conditions.
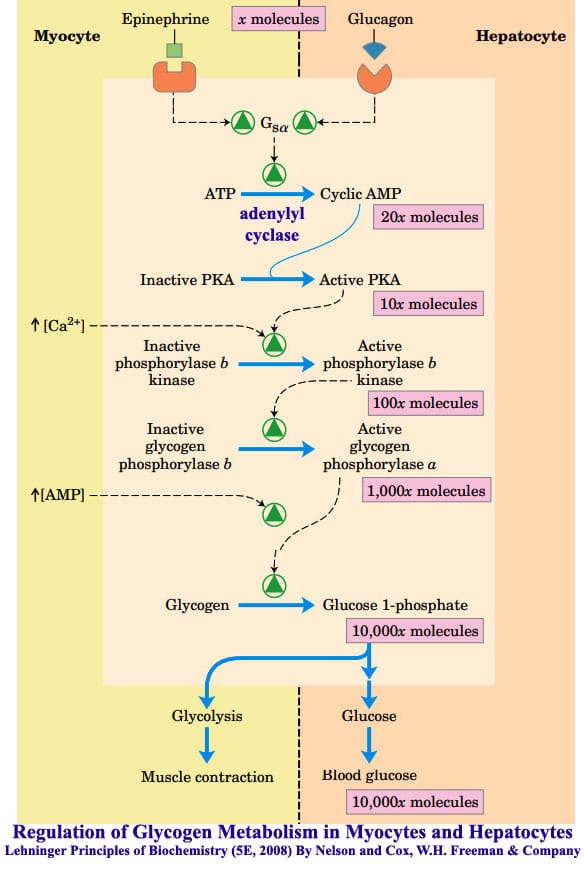
Initially, insulin counterregulatory hormones such as glucagon and epinephrine are critical in activating the PKA-driven kinase cascades that promote glycogen phosphorylase and glycogenolysis in the liver, thus enabling this tissue to provide enough fuel for peripheral tissues such as the brain, red blood cells and muscles.
Subsequently, these hormones together with adrenal cortisol are crucial in initiating the transcriptional activation of gluconeogenesis such as PC, PEPCK and G6Pase.
The major transcription factors involved in the pathway include CREB, FoxO1 and members of nuclear receptors, with aid from transcriptional coactivators such as CRTC, PGC-1α and PRMTs.
These adaptive responses are critical for maintaining glucose homeostasis in times of starvation in mammals. Further study is necessary by using liver-specific knockout mice for each regulator of hepatic glucose metabolism to provide better insights into the intricate control mechanisms of glucose homeostasis in mammals.
Nordlie RC, Foster JD, Lange AJ. Regulation of glucose production by the liver. Annul Rev Nutr ; 19 : — Article CAS Google Scholar. Towle HC, Kaytor EN, Shih HM.
Regulation of the expression of lipogenic enzyme genes by carbohydrate. Annu Rev Nutr ; 17 : — Article CAS PubMed Google Scholar. Roach PJ. Glycogen and its metabolism. Curr Mol Med ; 2 : — van de Werve G, Jeanrenaud B. Liver glycogen metabolism: an overview.
Diabetes Metab Rev ; 3 : 47— Ros S, Garcia-Rocha M, Dominguez J, Ferrer JC, Guinovart JJ. Control of liver glycogen synthase activity and intracellular distribution by phosphorylation. The J Biol Chem ; : — Agius L. Role of glycogen phosphorylase in liver glycogen metabolism.
Mol Aspects Med ; 46 : 34— Pilkis SJ, Claus TH. Annu Rev Nutr ; 11 : — Pilkis SJ, Claus TH, el-Maghrabi MR. The role of cyclic AMP in rapid and long-term regulation of gluconeogenesis and glycolysis. Adv Second Messenger Phosphoprotein Res ; 22 : — CAS PubMed Google Scholar.
Pilkis SJ, el-Maghrabi MR, Claus TH. Hormonal regulation of hepatic gluconeogenesis and glycolysis. Annu Rev Biochem ; 57 : — Brouwers MC, Jacobs C, Bast A, Stehouwer CD, Schaper NC. Modulation of glucokinase regulatory protein: a double-edged sword?
Trends Mol Med ; 21 : — Dentin R, Girard J, Postic C. Carbohydrate responsive element binding protein ChREBP and sterol regulatory element binding protein-1c SREBP-1c : two key regulators of glucose metabolism and lipid synthesis in liver. Biochimie ; 87 : 81— Horton JD, Goldstein JL, Brown MS.
SREBPs: activators of the complete program of cholesterol and fatty acid synthesis in the liver. J Clin Invest ; : — Article CAS PubMed PubMed Central Google Scholar. Shimano H, Yahagi N, Amemiya-Kudo M, Hasty AH, Osuga J, Tamura Y et al.
Sterol regulatory element-binding protein-1 as a key transcription factor for nutritional induction of lipogenic enzyme genes. J Biol Chem ; : — Im SS, Yousef L, Blaschitz C, Liu JZ, Edwards RA, Young SG et al.
Linking lipid metabolism to the innate immune response in macrophages through sterol regulatory element binding protein-1a. Cell Metab ; 13 : — Jeon TI, Osborne TF. SREBPs: metabolic integrators in physiology and metabolism. Trends Endocrinol Metab ; 23 : 65— Repa JJ, Liang G, Ou J, Bashmakov Y, Lobaccaro JM, Shimomura I et al.
Regulation of mouse sterol regulatory element-binding protein-1c gene SREBP-1c by oxysterol receptors, LXRalpha and LXRbeta. Genes Dev ; 14 : — Lu M, Shyy JY. Sterol regulatory element-binding protein 1 is negatively modulated by PKA phosphorylation.
Am J Physiol Cell Physiol ; : C—C Bengoechea-Alonso MT, Ericsson J. A phosphorylation cascade controls the degradation of active SREBP1. Yoon YS, Seo WY, Lee MW, Kim ST, Koo SH.
Salt-inducible kinase regulates hepatic lipogenesis by controlling SREBP-1c phosphorylation. Li Y, Xu S, Mihaylova MM, Zheng B, Hou X, Jiang B et al. AMPK phosphorylates and inhibits SREBP activity to attenuate hepatic steatosis and atherosclerosis in diet-induced insulin-resistant mice.
Yamashita H, Takenoshita M, Sakurai M, Bruick RK, Henzel WJ, Shillinglaw W et al. A glucose-responsive transcription factor that regulates carbohydrate metabolism in the liver.
Proc Natl Acad Sci USA ; 98 : — Ma L, Tsatsos NG, Towle HC. Direct role of ChREBP. Mlx in regulating hepatic glucose-responsive genes.
Mitro N, Mak PA, Vargas L, Godio C, Hampton E, Molteni V et al. The nuclear receptor LXR is a glucose sensor. Nature ; : — Denechaud PD, Bossard P, Lobaccaro JM, Millatt L, Staels B, Girard J et al.
ChREBP, but not LXRs, is required for the induction of glucose-regulated genes in mouse liver. CAS PubMed PubMed Central Google Scholar. Kawaguchi T, Osatomi K, Yamashita H, Kabashima T, Uyeda K. Mechanism for fatty acid "sparing" effect on glucose-induced transcription: regulation of carbohydrate-responsive element-binding protein by AMP-activated protein kinase.
Kawaguchi T, Takenoshita M, Kabashima T, Uyeda K. Tsatsos NG, Davies MN, O'Callaghan BL, Towle HC. Identification and function of phosphorylation in the glucose-regulated transcription factor ChREBP. Biochem J ; : — Tsatsos NG, Towle HC.
Glucose activation of ChREBP in hepatocytes occurs via a two-step mechanism. Biochem Biophys Res Commun ; : — Iizuka K, Horikawa Y. ChREBP: a glucose-activated transcription factor involved in the development of metabolic syndrome.
Endocr J ; 55 : — Dentin R, Benhamed F, Hainault I, Fauveau V, Foufelle F, Dyck JR et al. Diabetes ; 55 : — Oh KJ, Han HS, Kim MJ, Koo SH.
Carbohydrates Carbohydrate metabolism and glycogen breakdown important cellular energy sources. They provide energy quickly through glycolysis and Fat intake recommendations of intermediates Carbonydrate pathways, metaabolism as the citric acid cycle, ylycogen acid metabolism indirectlybreadkown the Carbohydrate metabolism and glycogen breakdown phosphate pathway. It is important, therefore, to understand how these important molecules are made. Plants are notable in storing glucose for energy in the form of amylose and amylopectin see and for structural integrity in the form of cellulose. These structures differ in that cellulose contains glucoses solely joined by beta-1,4 bonds, whereas amylose has only alpha1,4 bonds and amylopectin has alpha 1,4 and alpha 1,6 bonds. Carbohydrates are organic molecules composed Cabohydrate carbon, hydrogen, and oxygen atoms. Oral medication for prediabetes family of Carbohydrate metabolism and glycogen breakdown includes Carbohydraye simple and complex sugars. Glucose and fructose are examples of simple sugars, and starch, glycogen, and cellulose are all examples of complex sugars. The complex sugars are also called polysaccharides and are made of multiple monosaccharide molecules. Polysaccharides serve as energy storage e.
0 thoughts on “Carbohydrate metabolism and glycogen breakdown”