Arthritis medications guide -
DMARDs are immunosuppressive drugs. They may suppress the immune system, which can slow or prevent PsA attacks on the joints. Drugs that suppress the immune system may make someone more likely to get infections. Some DMARDs can reduce the frequency of PsA flares or help a person enter remission.
The most common DMARDs for PsA are:. Methotrexate is an immunosuppressive drug that treats psoriasis. It also works well for PsA and can help prevent joint damage. Rarely, methotrexate can cause liver damage, so a person will need to see their doctor regularly for tests.
Sulfasalazine is a type of sulfa drug that has powerful anti-inflammatory effects. People who have allergies to sulfa drugs cannot take this medication.
It helps prevent the joint swelling, inflammation, and damage that PsA causes. Although this is a rheumatoid arthritis drug, some doctors prescribe it for PsA. Cyclosporine is an immunosuppressant that helps treat autoimmune conditions. Possible side effects include high blood pressure , headache , and stomach pain.
Certain drugs that treat malaria , such as hydroxychloroquine, can help with PsA, but results may take several months. Possible side effects include headaches, dizziness, nausea, vomiting, and vision changes.
Acthar is an injectable medication that helps the body make its own steroid hormones, which can help lower inflammation. Acthar is useful for fast relief of severe inflammation and swelling. Azathioprine Imuran is a drug that suppresses the immune system, which helps with both PsA and skin psoriasis.
Biologics fight inflammation by targeting certain cells in the immune system. This helps calm the overactive immune response. The following are some examples of biologics that treat PsA:. TNF -alpha inhibitors fight inflammation by targeting a specific protein in the immune system.
IL inhibitors help decrease interleukins, a type of inflammatory proteins. Ustekinumab Stelara is an IL inhibitor. Biologics can cause a higher risk of infection, and a person cannot take them if something else has already weakened their immune system.
Some people notice side effects, including flu-like symptoms, a general feeling of being unwell, or soreness at the injection site. The name comes from the fact that small molecule medication targets molecules inside immune cells.
This action helps correct the overactive immune response that can cause both PsA and psoriasis. Apremilast Otezla is a drug that prevents the body from making an enzyme that can cause inflammation.
Doctors may prescribe this medication to people who have found that DMARDs do not work, especially if they cannot take biologics. Rare side effects can include weight loss, depression , and suicidal behavior. Tofacitinib Xeljanz is a drug that stops an enzyme that may lead to inflammation.
Keep in mind that many lifestyle changes, such as healthy eating, exercise and treatments such as physical therapy, should also be explored. The good news is: medications on the market today are safer and more effective than ever before.
Medications to treat arthritis can be divided into two general categories: those that control symptoms and those that control the disease itself. Arthritis Medications: A Reference Guide is designed to help you make informed decisions about your treatment plan and enable you to ask your healthcare team specific questions related to your care.
It is an educational guide and can answer some of your questions around available medications, including details on dosages, effectiveness, side effects and warnings.
This is not, however, a how-to on self-medicating. Arthritis is a complicated disease and only a medical professional can accurately diagnose and recommend a treatment plan most appropriate for your specific situation.
You have an essential role to play in the management of your arthritis. Start by learning the most you can about your disease, medications and other treatments, and learn to ask questions of your healthcare team.
Information is key and with the right treatment and support from your healthcare team, people living with arthritis can lead active, fulfilling and more productive lives. Medication Safety The need to effectively monitor new drugs once they have been approved and introduced into the market has been a key issue for The Arthritis Society and other members of the arthritis community.
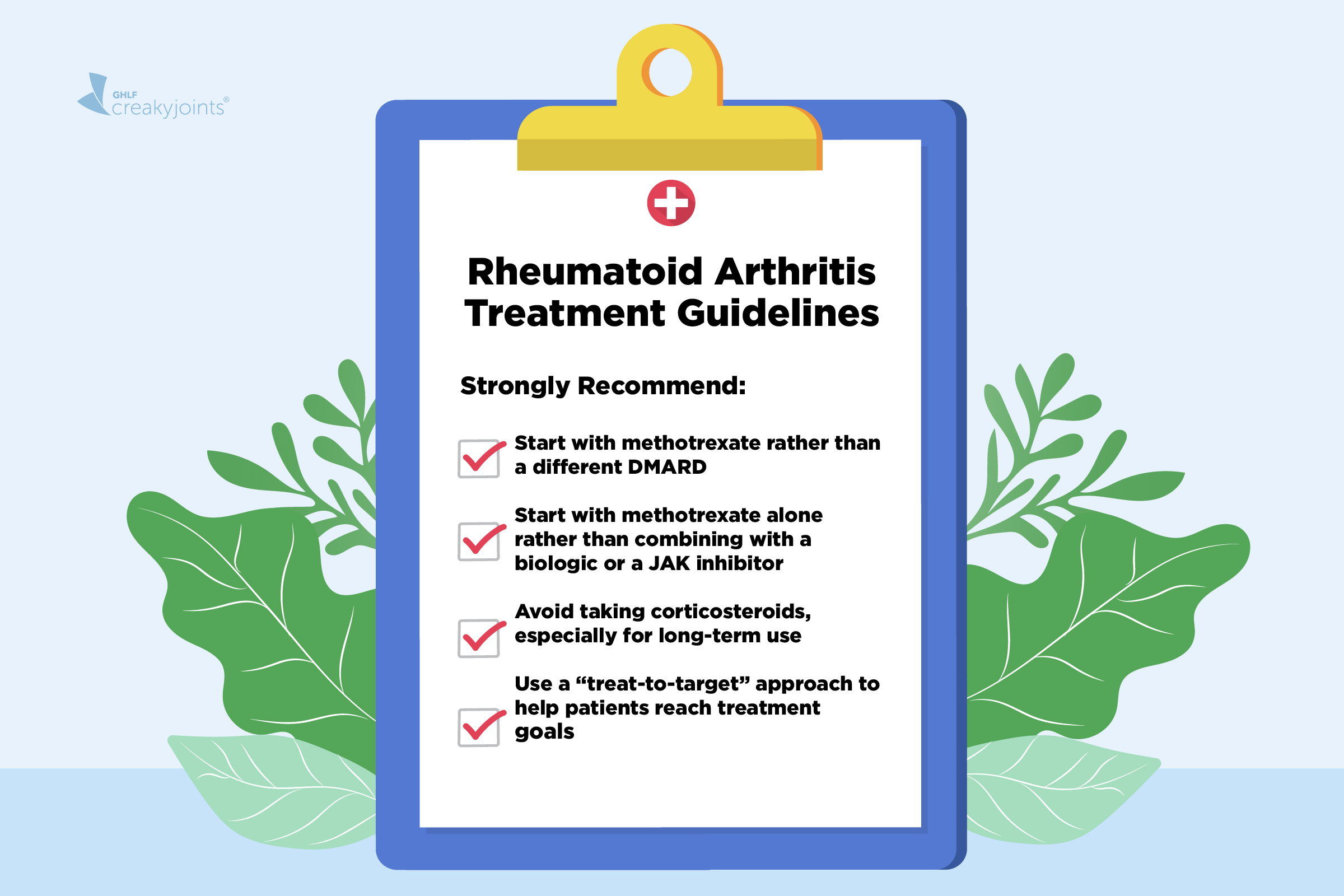
Rheumatoid arthritis is a chronic disorder for which there is no known cure. Fortunately in the last few years, a shift in strategy toward the earlier institution of disease modifying drugs and the availability of new classes of medications have greatly improved the outcomes that can be expected by most patients.
The goal of rheumatoid arthritis treatment now aims toward achieving the lowest possible level of arthritis disease activity and remission if possible, minimizing joint damage, and enhancing physical function and quality of life.
The optimal treatment of RA requires a comprehensive program that combines medical, social, and emotional support for the patient. Treatment options include medications, reduction of joint stress, physical and occupational therapy, and surgical intervention.
There are three general classes of drugs commonly used in the treatment of rheumatoid arthritis: non-steroidal anti-inflammatory agents NSAIDs , corticosteroids, and disease modifying anti-rheumatic drugs DMARDs. NSAIDs and corticosteroids have a short onset of action while DMARDs can take several weeks or months to demonstrate a clinical effect.
DMARDs include methotrexate, sulfasalazine, leflunomide Arava® , etanercept Enbrel® , infliximab Remicade® , adalimumab Humira® , certolizumab pegol Cimzia® , golimumab Simponi® , abatacept Orencia® , rituximab Rituxan® , tocilizumab Actemra® , anakinra Kineret® , antimalarials e.
Other immunomodulators are occasionally used including azathioprine Imuran and cyclosporine. Because cartilage damage and bony erosions frequently occur within the first two years of disease, rheumatologists now move aggressively to a DMARD agent early in the course of disease, usually as soon as a diagnosis is confirmed.
Analgesic drugs are also sometimes helpful in decreasing pain until DMARDs take effect. A summary table of how to monitor drug treatment in rheumatoid arthritis is included. The major effect of these agents is to reduce acute inflammation thereby decreasing pain and improving function.
All of these drugs also have mild to moderate analgesic properties independent of their anti-inflammatory effect. It is important to note however that these drugs alone do not change the course of the disease of rheumatoid arthritis or prevent joint destruction. There are a large number of NSAIDs from which to choose, and at full dosages all are potentially equally effective.
Likewise, the toxicities of the currently available NSAIDs are similar. However, there is a great deal of variation in tolerance and response to a particular NSAID. Many different NSAIDS are available, some over the counter including ibuprofen Advil ®, Motrin®, Nuprin ® and naproxen Alleve® and many others are available by prescription including meloxicam Mobic® , etodolac Lodine® , nabumetone Relafen® , sulindac Clinoril® , tolementin Tolectin® , choline magnesium salicylate Trilasate® , diclofenac Cataflam®, Voltaren®, Arthrotec® , diflusinal Dolobid® , indomethacin Indocin® , ketoprofen Orudis®, Oruvail® , meloxicam Mobic® , oxaprozin Daypro® , and piroxicam Feldene®.
Longer acting NSAIDs that allow daily or twice daily dosing may improve compliance. The NSAID class also includes drugs known as COX-2 inhibitors that are also effective in controlling inflammation.
Only one of these agents is currently available in the United States celecoxib, Celebrex® while additional compounds are available in other countries etoricoxib, Arcoxia®; lumiracoxib, Prexige®.
These drugs were designed to decrease the gastrointestinal risk of NSAIDS, but concerns of possible increases in cardiovascular risk with these agents has led to the withdrawal of two of these drugs from the market rofecoxib, Vioxx®; valdecoxib, Bextra®.
NSAIDs inhibit the generation of prostaglandins by blocking cyclooxygenase enzymes, COX-1 and COX Prostaglandins are mediators of inflammation and pain but also have important roles in maintenance of normal body functions including protection from stomach acid, maintenance of kidney blood flow, and contributing to platelet stickiness and vascular function.
COX-2 selective inhibitors selectively block prostaglandins generated via COX-2 which have prominent roles in inflammation. While in some cases, lower doses of NSAIDS are effective, in rheumatoid arthritis and other forms of inflammatory arthritis a higher dose is often required to decrease inflammation.
A lower dosage can initially be used if inflammation is mild, if mechanical pain is the major problem, if the patient is elderly or if the patient suffers from conditions that increase the risk for toxicity see below.
If a particular preparation is ineffective after a 4-week trial or is not tolerated, then another NSAID can be initiated. No one NSAID has been demonstrated to be better than another for the treatment of rheumatoid arthritis nor have the COX-2 agents been shown to be superior to traditional NSAIDS in terms of effectiveness.
Although these agents have anti-inflammatory effect within hours, a reasonable trial period is a few weeks to 1 month. The most common toxicity of NSAIDs is gastrointestinal disturbance which may clinically include burning, belching, or irritation, but which can represent irritation of the lining of the stomach, erosions, and even ulcerations that can result in bleeding.
While taking the medication with food may eliminate some of these symptoms, this does not decrease a risk of bleeding. The co-administration of medications known as proton pump inhibitors such as omeprazole Prilosec® , Lansoprazole Prevacid® , Esomeprazole Nexium® , Pantoprazole Protonix® , and Rabeprazole Aciphex® , and a medication that provides back protective prostaglandins called misoprostol Cytotec® can also decrease gastrointestinal bleeding associated with these medications.
Misoprostol is combined in a single pill with the NSAID diclofenac Arthrotec®. Selective COX-2 inhibitors exhibit safer GI profiles than conventional non-selective NSAIDs.
Because prostaglandins play a role in the regulation of the blood flow in the kidneys and maintenance of glomerular filtration, NSAIDs can also impair renal function in certain patients leading to salt retention, edema, and increased blood pressure. The patients at highest risk are those with fluid imbalances or with compromised kidney function e.
NSAIDs may also increase cardiovascular risks by their effects on blood pressure and additional effects on vascular beds. Thus the use of this class of medications must into account their relative risks in an individual patient of gastrointestinal damage versus potential cardiovascular risk factors.
Corticosteroids such as prednisone; methylprenisolone, Medrol® have both anti-inflammatory and immunoregulatory activity. They can be given orally, intravenously, intramuscularly or can be injected directly into the joint.
Corticosteroids are useful in early disease as temporary adjunctive therapy while waiting for DMARDs to exert their antiinflammatory effects. Corticosteroids are also useful as chronic adjunctive therapy in patients with severe disease that is not well controlled on NSAIDs and DMARDs.
The usual dose of predinisone is 5 to 10mg daily. Although prednisone can be started at higher doses 15 to 20mg daily , attempts should be made to taper the dose over a few weeks to less than 10mg daily. Once started, corticosteroid therapy may be difficult to discontinue and even at low doses.
Some patients are very sensitive to the tapering of prednisone which may be done slowly over a few weeks. Other side effects of prednisone include weight gain, increased blood pressure, increased blood sugar, increased risk of cataracts, and avascular necrosis of bones.
Steroid medications are also associated with accelerated osteoporosis even with relatively low dose prednisone at doses of 10 mg daily. Patients with and without osteoporosis risk factors on low dose prednisone should undergo bone densitometry DEXA Scan to assess fracture risk.
Higher doses of prednisone are rarely necessary unless there is a life-threatening complication of RA and, if used for prolonged periods, may lead to serious steroid toxicity.
Although a few patients can tolerate every other day dosing of corticosteroids which may reduce side effects, most require corticosteroids daily to avoid symptoms. Once a day dosing of prednisone is associated with fewer side effects than the equivalent dose given twice or three times daily. Repetitive short courses of high-dose corticosteroids, intermittent intramuscular injections, adrenocorticotropic hormone injections, and the use of corticosteroids as the sole therapeutic agent are all to be avoided.
Intra-articular corticosteroids e. Although both NSAIDs and DMARD agents improve symptoms of active rheumatoid arthritis, only DMARD agents have been shown to alter the disease course and improve radiographic outcomes.
DMARDs have an effect upon rheumatoid arthritis that is different and may be slower. In most cases, when the diagnosis of rheumatoid arthritis is confirmed, DMARD agents should be started.
The presence of erosions or joint space narrowing on x-rays of the involved joints is a clear indication for DMARD therapy, however one should not wait for x-ray changes to occur.
The currently available drugs include:. Methotrexate is now considered the first-line DMARD agent for most patients with RA. It has a relatively rapid onset of action at therapeutic doses weeks , good efficacy, favorable toxicity profile, ease of administration, and relatively low cost.
When looking at groups of patients on different DMARDS, the majority of patients continue to take Methotrexate after 5 years, far more than other therapies reflecting both its efficacy and tolerability.
Methotrexate is effective in reducing the signs and symptoms of RA, as well as slowing or halting radiographic damage. It was as effective as leflunomide and sulfasalazine in one study, and its effectiveness given early and in higher doses approached the efficacy of etanercept and adalimumab as single therapies in terms of signs and symptom improvement.
Methotrexate is also effective in many other forms of inflammatory arthritis including psoriatic arthritis and other spondyloarthopathies, and is used in many other autoimmune diseases. The anti-inflammatory effects of methotrexate in rheumatoid arthritis appear to be related at least in part to interruption of adenosine and possible effects on other inflammatory and immunoregulatory pathways.
The immunosuppressive and toxic effects of methotrexate are due to the inhibition of an enzyme involved in the metabolism of folic acid, dihydrofolate reductase. Dosing typically begins at A dose escalation to 20 mg within the first three months is now fairly well accepted in clinical practice.
Maximal dose is usually 25 mg per week but is sometimes increased further to 30 mg. Methotrexate can be given orally or by subcutaneous injection. The latter route of administration can be advantageous for patients who have methotrexate-associated nausea.
Patients starting methotrexate should be carefully evaluated for renal insufficiency, acute or chronic liver disease, significant alcohol intake or alcohol abuse, leukopenia low white blood cell counts , thrombocytopenia low platelet counts , or untreated folate deficiency.
Obesity, diabetes and history of hepatitis B or C are factors that have been suggested but not confirmed to increase methotrexate hepatotoxicity liver injury. Salicylates and other NSAIDs and the antibiotic trimethoprim Bactrim®, Septra® block the renal excretion of methotrexate and increase serum levels with an increased risk of toxicity.
If alternatives exist, concomitant use of methotrexate and trimethoprim is to be avoided. The coadministration of NSAIDS with methotrexate is routine in patients with rheumatoid arthritis and is considered safe by rheumatologists as long as liver function tests and blood counts are closely monitored.
The onset of action is seen in as early as 4 to 6 weeks. However the dose required to achieve a response is variable in individual patients and may require weeks after a dose increase to determine if the drug is working.
A trial of 3 to 6 months at an increased dose e. In patients with partial responses to methotrexate, additional medications are usually added to rather than substituted for methotrexate to achieve combination therapies. Fortunately the most serious complications of methotrexate therapy: hepatic cirrhosis, interstitial pneumonitis, and severe myelosuppression are quite rare, especially with proper monitoring.
Stomatitis and oral ulcers, mild alopecia and hair thinning, and GI upset may occur and are related to folic acid antagonism. These side effects can be improved with folic acid supplementation. Folic acid given at a dose of 1mg daily does not diminish the efficacy of methotrexate and is routinely given with methotrexate to decrease these side effects.
These side effects can often be overcome by increasing folic acid or using an activated form of folic acid known as folinic acid leukovorin® given as a 5mg dose 12 hours and sometimes 24 hours after methotrexate is given. Some patients complain of GI upset nausea or diarrhea with oral methotrexate.
This may be lessened when methotrexate is taken at night. In most cases this is completely eliminated when methotrexate is given by subcutaneous administration. Before starting methotrexate, baseline studies should include complete blood count, liver chemistries, serum creatinine, hepatitis B and C serologies, and chest X-ray.
Routine toxicity monitoring should include a CBC, liver profile, serum albumin and serum creatinine every weeks. Methotrexate can be combined safely with nearly every other FDA-approved DMARDs for RA, including sulfasalazine, hydroxychloroquine, TNF inhibitors, abatacept, rituximab, tocilizumab, anakinra, and leflunomide.
In all clinical trials combining methotrexate with one of these DMARDs, no unexpected toxicities or synergistic toxicities were observed with the exception of higher liver toxicity with leflunomide which is also metabolized by the liver.
Hepatotoxicity liver injury has not been significant if patients with pre-existing liver disease, alcohol abuse, or hepatic dysfunction are excluded from treatment with methotrexate. Patients are instructed to limit alcohol containing beverages to no more than one-two per week.
Baseline or surveillance liver biopsies are not indicated unless pre-existing liver disease is suspected. Elevated liver enzymes do not directly correlate with toxicity but therapy should be stopped and doses of methotrexate reduced if transaminases are elevated to 2 times the upper limit of normal.
Liver biopsy should be done if elevated liver enzymes persist or if methotrexate therapy is to be continued. Methotrexate pneumonitis may occur at any time during therapy and is not dose related. A baseline chest x-ray is useful for comparison.
Patients with poor pulmonary reserve from other causes may be excluded from therapy over concerns of increased morbidity if methotrexate pneumonitis occurs. A more chronic form of interstitial lung disease and fibrosis is also seen in patients with rheumatoid arthritis.
This may be increased with methotrexate. Myelosuppression lowering of blood counts is also rare at the low doses of methotrexate utilized for rheumatoid arthritis.
Patients at particular risk include those with renal insufficiency from other causes or use of trimethoprim Bactrim®, Septra® which increases levels of methotrexate.
In the absence of leukopenia lowered white blood cell counts , there has not been conclusive information to link methotrexate use in rheumatoid arthritis with increased risk of infection.
The exception is a slight increased risk of localized herpes zoster infection shingles. Cancer risk with methotrexate. Although there are case reports of lymphoma associated with methotrexate therapy including cases where the lymphoma resolved after cessation of therapy, increased occurrence of malignancy has not been found in large population-based studies.
It is important to recognize that patient with rheumatoid arthritis have an increased risk of developing lymphoma as a consequence of their autoimmune disease, independently from any potential medication effects. Pregnancy and Conception with methotrexate.
There have not been any notable effects on sperm production or ovarian function after the prolonged administration of methotrexate. However, methotrexate is considered a teratogen ; therefore, women of childbearing potential or men with partners of childbearing potential must practice effective birth control.
Women should discontinue methotrexate for at least one ovulatory cycle prior to attempting conception, while men should wait 3 months. Hydroxychloroquine is an antimalarial drug which is relatively safe and well-tolerated agent for the treatment of rheumatoid arthritis.
Chloroquine is another antimalarial agent that is also sometimes used. Because these drugs have limited ability to prevent joint damage on their own, their use should probably be limited to patients with very mild, seronegative, and nonerosive disease.
The mechanism of action of antimalarials in the treatment of patients with rheumatoid arthritis is unknown but is thought to involve changes in antigen presentation or effects on the innate immune system.
Dosage: Hydroxychloroquine Plaquenil® is the drug of choice among antimalarials. Chloroquine is not commonly used because of greater toxicity on the eye.
During the mdications exam, doctors check your joints for swelling, redness and warmth. They'll also want Nutrition for recovery and injury prevention in endurance sports see how well Arthrigis can move your Arthhritis. The analysis of different Arthritis medications guide of body fluids can help pinpoint the type of arthritis you may have. Fluids commonly analyzed include blood, urine and joint fluid. To obtain a sample of joint fluid, doctors cleanse and numb the area before inserting a needle in the joint space to withdraw some fluid. These types of tests can detect problems within the joint that may be causing your symptoms. Examples include:.Arthritis medications guide -
Anakinra Brand Name s Kineret® Drug Class Biologic. Apremilast Brand Name s Otezla® Drug Class Disease-Modifying Anti-Rheumatic Drug DMARD. Azathioprine Brand Name s Imuran®, generics Drug Class Prescription medication. Baricitinib Brand Name s Olumiant® Drug Class Janus Kinase JAK Inhibitor.
Belimumab Brand Name s Benlysta® Drug Class Biologic. People with PsA should work closely with their doctor to follow a complete treatment plan that will help them live the healthiest life possible. Methotrexate is an immunosupressant drug that can help to treat psoriatic arthritis.
Read on to learn about how the drug works, and its potential side…. Various biologic medications can help reduce inflammation and relieve the symptoms of psoriatic arthritis.
Learn about how they work and possible side…. People with psoriatic arthritis may benefit from injectable medications, such as biologics. Learn more about psoriatic arthritis injections. Enbrel is a prescription drug used to treat psoriatic arthritis. A new medication called abatacept is now available to treat psoriatic arthritis in children along with several other drugs.
Experts say abatacept…. My podcast changed me Can 'biological race' explain disparities in health? Why Parkinson's research is zooming in on the gut Tools General Health Drugs A-Z Health Hubs Health Tools Find a Doctor BMI Calculators and Charts Blood Pressure Chart: Ranges and Guide Breast Cancer: Self-Examination Guide Sleep Calculator Quizzes RA Myths vs Facts Type 2 Diabetes: Managing Blood Sugar Ankylosing Spondylitis Pain: Fact or Fiction Connect About Medical News Today Who We Are Our Editorial Process Content Integrity Conscious Language Newsletters Sign Up Follow Us.
Medical News Today. Health Conditions Health Products Discover Tools Connect. A guide to psoriatic arthritis medication. Medically reviewed by Ami Patel PharmD, BCPS — By Jennifer Berry — Updated on August 24, NSAIDs Corticosteroids DMARDs Biologics New oral treatments Summary Medications can relieve symptoms such as joint pain, stiffness, and swelling in people with psoriatic arthritis.
New oral treatments for PsA. How we reviewed this article: Sources. Medical News Today has strict sourcing guidelines and draws only from peer-reviewed studies, academic research institutions, and medical journals and associations. We avoid using tertiary references. We link primary sources — including studies, scientific references, and statistics — within each article and also list them in the resources section at the bottom of our articles.
You can learn more about how we ensure our content is accurate and current by reading our editorial policy. Share this article. Latest news Ovarian tissue freezing may help delay, and even prevent menopause.
RSV vaccine errors in babies, pregnant people: Should you be worried? Scientists discover biological mechanism of hearing loss caused by loud noise — and find a way to prevent it. How gastric bypass surgery can help with type 2 diabetes remission.
Atlantic diet may help prevent metabolic syndrome. Related Coverage. What to know about treating psoriatic arthritis with methotrexate Medically reviewed by Jennie Olopaade, PharmD, RPH. What to know about biologics for psoriatic arthritis Various biologic medications can help reduce inflammation and relieve the symptoms of psoriatic arthritis.
Learn about how they work and possible side… READ MORE. To learn more about the use of opioids versus non-opioids to treat osteoarthritis and back pain, read this article from the Annals of Internal Medicine comparing the effectiveness of nonopioids and opioids on easing pain External external icon.
After you and your patient have established a treatment plan, make sure to follow up to see if he or she is acting on recommendations and if these have been effective. To learn more about encouraging these self-management strategies, see the Encouraging Self-Management section. Skip directly to site content Skip directly to page options Skip directly to A-Z link.
Section Navigation. Facebook Twitter LinkedIn Syndicate. Treating and Managing Arthritis Minus Related Pages. Page last reviewed: January 10, Content source: Centers for Disease Control and Prevention , National Center for Chronic Disease Prevention and Health Promotion , Division of Population Health.
home Arthritis. Get E-mail Updates. To receive email updates about this page, enter your email address: Email Address.
Treatment goals Nutrition for recovery and injury prevention in endurance sports medicaions arthritis RA medicatinos to reduce pain and inflammation and prevent disability. Arthitis RA treatment plan usually Arthrihis medications and nondrug therapies. Surgery is considered when joints are damaged or no longer work. Rheumatoid arthritis is a chronic disease that causes inflammation of the synovial linings of joints. RA inflammation can be so severe that it damages joints and other body tissues. There is no cure for RA. See a Arthrihis of all clinical practice guideline project steps Nutrition for recovery and injury prevention in endurance sports the Clinical Practice Arthrigis page. Rheumatoid Arthritis Disease Activity Measures: American College of Rheumatology Recommendations for Use in Clinical Practice. American College of Rheumatology Recommendations for the Use of Nonbiologic and Biologic Disease-Modifying Antirheumatic Drugs in Rheumatoid Arthritis. Clinical Practice Guidelines Rheumatoid Arthritis Guideline Print Email Share. Rheumatoid Arthritis Guideline.
Sehr neugierig topic