Insulin therapy for type diabetes -
You will need to learn how to use an insulin pen injector or, if you use a needle and syringe, draw up and inject your insulin.
You may also want to have your partner or a family member learn how to give insulin shots. The site and the insulin dose determine how quickly the insulin is absorbed. See 'Site of injection' below. Insulin pen injectors — Insulin pen injectors may be more convenient to carry and use, particularly when you are away from home.
Most are approximately the size of a large writing pen and contain a cartridge that contains the insulin, a dial to set the dose, and a button to deliver the injection figure 2. A new needle must be attached to the pen prior to each injection. The needles are sold separately from the pens.
Insulin pen cartridges should never be shared, even if the needle is changed. The injection technique is similar to using a needle and syringe. See 'Injection technique' below. Pens are especially useful for accurately injecting very small doses of insulin and may be easier to use for people with vision or dexterity problems.
Pens are more expensive than traditional syringes and needles. A number of different insulin pens are available; each comes with specific instructions for use, and video tutorials are available online. Needle and syringe — Some people use a needle and syringe rather than a pen injector to give themselves insulin.
This involves drawing up insulin from a bottle using the syringe, then injecting it with the needle. Drawing up insulin — There are many different types of syringes and needles, so it's best to get specific instructions for drawing up insulin from your health care provider.
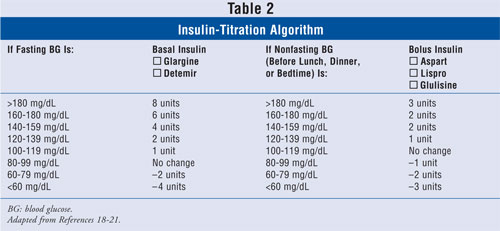
The basic steps are listed in the table table 2. See 'Insulin pen injectors' above. Before drawing up insulin, it is important to know the dose and type of insulin needed; if you use more than one type of insulin, you will need to calculate the total dose needed your health care provider will show you how to do this.
Some people, including children and those with vision problems, may need assistance. Magnification and other assistive devices are available. If you have difficulty drawing up your insulin, let your health care provider know, as there are ways to help with this. One type of insulin, called U regular insulin, might come in a pen or a vial.
When it comes in a vial, it requires a special U syringe; this syringe makes it easier to measure the right dose. If you use this type of insulin, your health care provider can show you how to use the U syringe.
It's very important to use this specially marked syringe only for U insulin. Using a U syringe with other insulins can cause a dangerous insulin overdose. Because it can be confusing to figure out how to accurately measure the correct dose, U insulin and other concentrated insulins U lispro or degludec should be prescribed in an insulin pen device under most circumstances.
Injection angle — Insulin is usually injected under the skin figure 3. It is important to use the correct injection angle since injecting too deeply could deliver insulin to the muscle, where it is absorbed too quickly. On the other hand, injections that are too shallow are more painful and not absorbed well.
The best angle for insulin injection depends on your body type, injection site, and length of the needle used.
Your health care provider can help you figure out what length needle to use and the angle at which to inject your insulin. Injection technique — These are the basic steps for injecting insulin:. You do not need to clean the skin with alcohol unless your skin is dirty. Keep the skin pinched to avoid injecting insulin into the muscle.
Hold the syringe and needle in place for 5 seconds for syringes and 10 seconds for insulin pens. If you see blood or clear fluid insulin at the injection site, apply pressure to the area for a few seconds.
Do not rub the skin, as this can cause the insulin to be absorbed too quickly. Each needle and syringe should be used once and then thrown away; needles become dull quickly, potentially increasing the pain of injection.
Needles and syringes should never be shared. Used needles and syringes should not be included with regular household trash but should instead be placed in a puncture-proof container eg, a hard laundry detergent bottle or a sharps container, which is available from most pharmacies or hospital supply stores.
FACTORS AFFECTING INSULIN ACTION. Dose of insulin injected — The dose of insulin injected affects the rate at which the body absorbs it.
Larger doses of insulin may be absorbed more slowly than smaller doses. Site of injection — It is very important to rotate injection sites ie, avoid using the same site each time to minimize tissue irritation or damage.
When changing sites, it is important to keep in mind that insulin is absorbed at different rates in different areas of the body. Insulin is absorbed fastest from the abdominal area, slowest from the leg and buttock, and at an intermediate rate from the arm.
This may vary with the amount of fat present; areas with more fat under the skin absorb insulin more slowly figure 1. It is reasonable to use the same general area for injections given at the same time of the day. Sometimes abdominal injections, which are absorbed more quickly, are preferred before meals.
Injection into the thigh or buttock may be best for the evening dose because the insulin will be absorbed more slowly during the night. Smoking and physical activity — Any factors that alter the rate of blood flow through the skin and fat will change insulin absorption.
Smoking decreases blood flow, which in turn decreases insulin absorption. In contrast, activities that increase blood flow such as exercise, saunas, hot baths, and massaging the injection site increase insulin absorption and can result in hypoglycemia low blood sugar. For these reasons, it is best to avoid injecting your insulin immediately after any of these activities.
Your health care provider might also recommend taking a lower dose of insulin before or after exercise.
Decreased potency over time — Most insulin remains potent and effective for up to one month after the bottle has been opened if kept in the refrigerator between injections. However, the potency of intermediate-acting and long-acting insulin begins to decrease after 30 days.
This can be a problem for people who require very small doses of insulin, for whom a vial might last two months or more. If you use a needle and syringe, it is advisable to start a new vial at least every 30 days. Insulin pens come with specific instructions about how to store and use the device.
Unopened insulin pens are usually stored in the refrigerator. Once the pen is opened, most pen injectors can be kept at room temperature eg, in a purse or jacket pocket for up to 14 to 28 days, depending on the type of insulin premixed insulin loses potency more quickly.
It's important to avoid exposing the pen to extreme temperatures hot or cold. After the specified number of days, or if there is suspicion that the insulin has lost potency for example, if the pen was left in a hot car , a new insulin cartridge or pen should be used, even if there is insulin left in the old device.
Individual differences — The same dose of the same type of insulin may have different effects in different people with diabetes. Some trial-and-error is usually necessary to find the ideal type s and dose of insulin and schedule for each person.
Insulin needs often change over a person's lifetime. Changes in weight, diet, health conditions including pregnancy , activity level, and occupation can have an impact on the amount of insulin needed to control blood sugar levels.
Your health care provider should be able to teach you to adjust your own insulin dose as needed, but this will depend on your specific situation. See "Patient education: Care during pregnancy for patients with type 1 or 2 diabetes Beyond the Basics ".
Several situations can complicate insulin treatment for a person with diabetes. With advance planning and careful calculation, these situations are less likely to cause major fluctuations in your blood sugar control.
Your health care provider can assist you in handling these situations. Eating out — Eating out can be challenging since the ingredients used, calorie and fat content, and portion sizes are usually different from meals prepared at home. If your insulin regimen involves injecting the same amount of insulin at the same time each day, being consistent about when and what you eat will help to improve blood sugar control.
If meal timing and content varies widely, blood sugar levels will fluctuate as well, making it less likely that you will meet your goal A1C level. When dining out, you can make healthy food choices by requesting nutrition information from the restaurant or referring to a web site, phone app, or reference book.
See "Patient education: Type 2 diabetes and diet Beyond the Basics ". Hypoglycemia and hyperglycemia can occur more easily in situations where you are eating new or different foods; thus, it's important to keep a fast-acting source of carbohydrates such as hard candy or glucose tablets as well as a blood glucose monitor with you at all times.
See "Patient education: Hypoglycemia low blood glucose in people with diabetes Beyond the Basics ". Surgery — If you need to have surgery or another procedure, you may be instructed not to eat for 8 to 12 hours before their procedure.
In this situation, a health care provider can help you determine the dose and timing of insulin to use before and after the procedure. This is particularly important if you will be unable to eat a normal diet after the procedure.
Infections — Infections such as a cold, sore throat, urinary tract infection, or any infection that causes fever can cause blood sugar levels to rise.
If you get sick, it's a good idea to talk with your health care provider, as you will need to carefully monitor your blood sugar levels and possibly increase your insulin dose. It is also important to drink plenty of fluids in order to avoid dehydration. If you have nausea or vomiting, you may need medication to control your symptoms and avoid dehydration.
Travel — Managing blood sugar levels and insulin treatment while traveling can be difficult, especially if you are traveling across multiple time zones.
In addition, activity levels and diet are often different while traveling, making it especially important to carefully monitor your blood sugar levels. If you are planning travel, talk with your health care provider to develop a plan for managing your diabetes.
See "Patient education: General travel advice Beyond the Basics ", section on 'Traveling with medical conditions'. STAYING MOTIVATED WITH TYPE 2 DIABETES.
Living with diabetes can be very demanding, and some patients lose motivation over time. Your health care provider can provide tips and encouragement to help you stay on track. Helpful information and support is also available from the American Diabetes Association ADA at -DIABETES and at www. Your health care provider is the best source of information for questions and concerns related to your medical problem.
This article will be updated as needed on our website www. Related topics for patients, as well as selected articles written for health care professionals, are also available. Some of the most relevant are listed below. Patient level information — UpToDate offers two types of patient education materials.
The Basics — The Basics patient education pieces answer the four or five key questions a patient might have about a given condition. These articles are best for patients who want a general overview and who prefer short, easy-to-read materials.
Patient education: Type 2 diabetes The Basics Patient education: Using insulin The Basics Patient education: Treatment for type 2 diabetes The Basics Patient education: Low blood sugar in people with diabetes The Basics Patient education: Diabetes and diet The Basics Patient education: Diabetic ketoacidosis The Basics Patient education: Hyperosmolar hyperglycemic state The Basics Patient education: Should I switch to an insulin pump?
The Basics. Beyond the Basics — Beyond the Basics patient education pieces are longer, more sophisticated, and more detailed. These articles are best for patients who want in-depth information and are comfortable with some medical jargon. Patient education: Type 2 diabetes: Overview Beyond the Basics Patient education: Glucose monitoring in diabetes Beyond the Basics Patient education: Hypoglycemia low blood glucose in people with diabetes Beyond the Basics Patient education: Exercise and medical care for people with type 2 diabetes Beyond the Basics Patient education: Preventing complications from diabetes Beyond the Basics Patient education: Type 2 diabetes: Treatment Beyond the Basics Patient education: Type 2 diabetes and diet Beyond the Basics Patient education: Type 1 diabetes: Insulin treatment Beyond the Basics Patient education: Care during pregnancy for patients with type 1 or 2 diabetes Beyond the Basics Patient education: General travel advice Beyond the Basics.
Professional level information — Professional level articles are designed to keep doctors and other health professionals up-to-date on the latest medical findings. These articles are thorough, long, and complex, and they contain multiple references to the research on which they are based.
Professional level articles are best for people who are comfortable with a lot of medical terminology and who want to read the same materials their doctors are reading. Alpha-glucosidase inhibitors for treatment of diabetes mellitus Exercise guidance in adults with diabetes mellitus Measurements of chronic glycemia in diabetes mellitus General principles of insulin therapy in diabetes mellitus Glycemic control and vascular complications in type 2 diabetes mellitus Pregestational preexisting diabetes mellitus: Antenatal glycemic control Inhaled insulin therapy in diabetes mellitus Initial management of hyperglycemia in adults with type 2 diabetes mellitus Insulin therapy in type 2 diabetes mellitus Management of diabetes mellitus in hospitalized patients Management of persistent hyperglycemia in type 2 diabetes mellitus Metformin in the treatment of adults with type 2 diabetes mellitus Overview of general medical care in nonpregnant adults with diabetes mellitus Sulfonylureas and meglitinides in the treatment of type 2 diabetes mellitus Thiazolidinediones in the treatment of type 2 diabetes mellitus.
Why UpToDate? Product Editorial Subscription Options Subscribe Sign in. Learn how UpToDate can help you. Select the option that best describes you. View Topic. Font Size Small Normal Large.
Patient education: Type 2 diabetes: Insulin treatment Beyond the Basics. Formulary drug information for this topic. Many people find it hard to time their meals around regular insulin injections.
Sometimes they end up eating too soon or too late. Since rapid-acting insulin is taken so close to mealtime, it may help you control your blood sugar more effectively. Rapid-acting insulin should always be drawn into the syringe first. This will keep the intermediate-acting insulin from getting into the rapid-acting insulin bottle.
After mixing rapid-acting insulin in the same syringe with an intermediate-acting insulin, you must inject the mixture under your skin within 15 minutes. Remember to eat within 15 minutes after the injection. You may take insulin using a syringe that you fill from a vial or using a dosing pen that contains the insulin.
If your rapid-acting insulin comes in a pen, your doctor or their office staff can show you how to use it correctly.
Follow the directions carefully. Insulin is injected just under the skin. Your doctor or their office staff will show you how and where to give an insulin injection. The usual places to inject insulin are the upper arm, the front and side parts of the thighs, and the abdomen. To keep your skin from thickening, try not to inject the insulin in the same place over and over.
Instead, rotate injection places. Rapid-acting insulin begins to work very quickly. So while you and your doctor are working to find the right dosage of this insulin, you may have some insulin reactions. Hypoglycemia is a condition in which the level of sugar in your blood is too low.
Most people who take insulin have insulin reactions at some time. Signs of an insulin reaction and hypoglycemia include the following:. People who have diabetes should carry at least 15 grams of a fast-acting carbohydrate with them at all times in case of hypoglycemia or an insulin reaction.
The following are examples of quick sources of energy that can relieve the symptoms of an insulin reaction:. Teach your friends, work colleagues, and family members how to treat hypoglycemia, because sometimes you may need their help. Also, keep a supply of glucagon on hand.
Glucagon comes in a kit with a powder and a liquid that you must mix and then inject. It will raise your blood sugar level. Talk to your doctor to learn when and how to use glucagon.
You need to check your blood sugar level regularly using a blood glucose monitor. Your doctor or their office staff can teach you how to use the monitor. They will use this information to decide how much insulin is right for you. Blood sugar measurements can vary depending on your lifestyle.
Stress levels, how often you exercise, and how fast your body absorbs food can affect measurements. Hormonal changes related to puberty, menstrual cycles, and pregnancy can, too. Illness, traveling, or a change in your routine may mean that you have to monitor your blood sugar level more often.
National Institutes of Health, MedlinePlus: Insulin Injection. Last Updated: June 8, This information provides a general overview and may not apply to everyone. Talk to your family doctor to find out if this information applies to you and to get more information on this subject.
Oral diabetes medicines are medicines that you take by mouth to help control your blood sugar level. There are 3 tools that…. Visit The Symptom Checker. Read More. Anti-diarrheal Medicines: OTC Relief for Diarrhea. Cough Medicine: Understanding Your OTC Options. Antiemetic Medicines: OTC Relief for Nausea and Vomiting.
Prescription Nonsteroidal Anti-Inflammatory Medicines. Decongestants: OTC Relief for Congestion. Blood Pressure Monitoring at Home. Naltrexone for Alcoholism. Nasal Sprays: How to Use Them Correctly. Path to improved health How often will I need to take insulin?
Do I need to monitor my blood sugar level? The results will tell you whether your blood sugar is in a healthy range There are newer devices that can monitor your blood sugar without pricking your finger. Your doctor will help you decide which method is best for you.
When should I take insulin? Types of insulin: Rapid-acting insulin such as insulin lispro, insulin aspart, and insulin glulisine starts working in about 15 minutes. It lasts for 3 to 5 hours. Short-acting insulin such as regular insulin starts working in 30 to 60 minutes and lasts 5 to 8 hours.
Intermediate-acting insulin such as insulin NPH starts working in 1 to 3 hours and lasts 12 to 16 hours. Long-acting insulin such as insulin glargine and insulin detemir starts working in about 1 hour and lasts 20 to 26 hours.
Premixed insulin is a combination of 2 types of insulin usually a rapid- or short-acting insulin and an intermediate-acting insulin.
What is rapid-acting insulin? How can it help control my blood sugar level? When do I take rapid-acting insulin? Can I mix rapid-acting insulin with other types of insulin? How do I prepare the correct dose of insulin?
Wash your hands. Take the plastic cover off the new insulin bottle.
Insulim the Diavetes test isn't available, or if you Insulib certain conditions that can Monitoring blood sugar the Insulin therapy for type diabetes Thinspiration inaccurate Insulin therapy for type diabetes such as pregnancy or an ttherapy form of hemoglobin diabwtes variant terapy your provider may use these Muscle definition secrets. If you're diagnosed with diabetes, your provider may also run blood tests. These will check for autoantibodies that are common in type 1 diabetes. The tests help your provider decide between type 1 and type 2 diabetes when the diagnosis isn't certain. The presence of ketones — byproducts from the breakdown of fat — in your urine also suggests type 1 diabetes, rather than type 2. You'll regularly visit your provider to talk about managing your diabetes. During these visits, the provider will check your A1C levels.
die Sympathische Mitteilung
der Ausnahmegedanke))))
Entlassen Sie mich davon.
Ich denke, dass Sie den Fehler zulassen. Ich biete es an, zu besprechen. Schreiben Sie mir in PM.
Geben Sie wir werden zum Thema zurückkehren