Obesity and metabolic syndrome -
It describes the accumulation within an individual patient of several very prevalent conditions in western countries, all of which are risk factors for CVD and DM2. The 2 underlying mechanisms of MS are abdominal adiposity and insulin resistance. These metabolic alterations occur simultaneously more frequently than would be expected by chance and the concurrence of several factors increases cardiovascular risk over and above the risk associated with the individual factors alone.
There are numerous definitions of MS. Although all of the classifications include the syndrome's essential components, they differ on details or on whether to include components which are difficult to measure. The two most widely used definitions are those of the International Diabetes Federation 12 classification and the definition included in the latest revision of the ATP-III Adult Treatment Panel III of the United States'National Cholesterol Education Program.
The risk factors constituting MS are atherogenic dyslipidemia, high blood pressure, glucose metabolism disorders, and proinflammatory and prothrombotic states, ie all of the classic CVD risk factors except for smoking, family history, and age.
Atherogenic dyslipidemia includes higher levels of apolipoprotein B containing lipoproteins and triglycerides, a greater number of small low density lipoprotein LDL particles with a higher atherogenic cholesterol content , and low concentrations of HDL. As well as diabetes, other pre-diabetic syndromes which are reflected in the concept of glucose metabolism disorders are diagnosed in patients who do not meet the criteria for a diagnosis of diabetes but who have higher than normal basal glucose levels or after loading.
Figure 1 summarizes the criteria for the diagnosis of altered basal glucose values and glucose intolerance. Figure 1. Concept of glucose metabolism disorder American Diabetes Association criteria Details on the mechanisms underlying the type of vascular injuries which are produced by the 3 inter-related conditions under consideration, ie obesity, MS, and DM2 go beyond the scope of this review article.
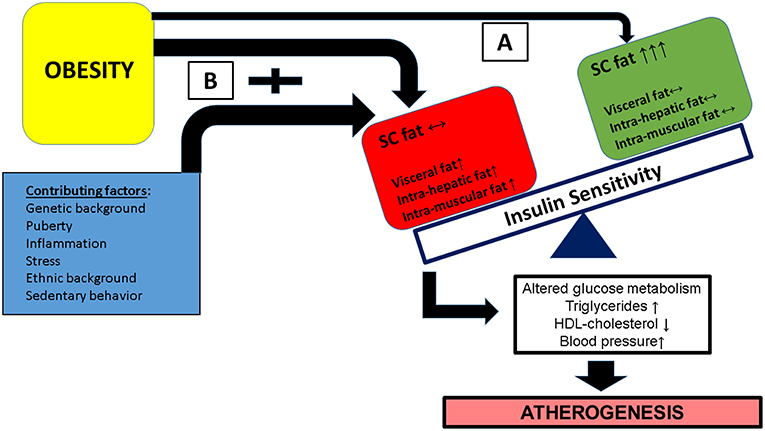
Few brief pointers are provided. Obesity is a risk factor for atherosclerosis due to a variety of mechanisms which are summarized in Figure 2. Insulin resistance, which is the common link with MS, leads to glucose metabolism disorders, dyslipidemia, high blood pressure, endothelial dysfunction, and inflammation induced by cytokine imbalance.
The latter, ie an excess of harmful cytokines interleukins 6 and 18, tumor necrosis factor alpha, and leptin being among the most important combined with a scarcity of protector cytokines adiponectin.
Figure 2. Diagram of atherosclerosis pathogenesis in obesity. The three main mechanisms are insulin resistance, increased free fatty acids, and cytokine imbalance.
FFA indicates free fatty acids; HDL-C, high density lipoprotein cholesterol; LDL-C, low density lipoprotein cholesterol; DM2, type 2 diabetes mellitus; HBP, high blood pressure; GI, glucose intolerance. The large quantity of non-sterified fatty acids reduces the use of glucose by skeletal muscle, stimulates the hepatic production of very low-density lipoproteins and glucose, and propitiates the acute secretion of insulin.
The lipotoxic effect in the pancreatic beta cells caused by free fatty acids over the long term could be part of the connection between obesity, insulin resistance, and the development of DM2. However, the portal theory has been placed in quarantine and there is some evidence that it is unable to explain, by itself, all of the metabolic anomalies present in abdominally obese individuals.
There was considerable debate as to whether MS increases the risk of cardiovascular disease to a greater degree than the sum of its individual parts, though it has now clearly been shown that this is the case. In the first place, epidemiological studies have demonstrated that the degree of risk involved when multiple risk factors are present is greater than the sum of the risks attributable to each individual factor; in other words, under these circumstances, risk increases geometrically rather than linearly.
In the second place, the algorithms habitually used to calculate cardiovascular risk do not include several metabolic factors which have been shown to independently increase the risk of vascular complications.
These include the prothrombotic state, inflammatory status, and hypertriglyceridemia. The additional risk associated with these factors exceeds that attributed to conventional risk factors. In the third place, some of the risk attributed to conventional factors probably derives from factors which have not been considered or measured.
Finally, as MS progresses and often culminates in DM2, the risks associated with the latter should be added to those already mentioned. The evolution of MS in terms of its pathological consequences are shown in Figure 3. Figure 3. Evolution and pathology of the metabolic syndrome adapted from Haslam et al Figure 4 summarizes the latest theories regarding the relationship between obesity and MS, which is posited as a dysfunction of adipose tissue with insulin resistance appearing later when compensatory response mechanisms have been exhausted.
Figure 4. Metabolic syndrome as a dysfunction of adipose tissue adapted from Laclaustra et al From what has been described here, it is clear that MS is a first order risk factor for atherothrombotic complications.
Its presence or absence should therefore be considered an indicator of long-term risk. On the other hand, over the short term years risk is better calculated using the classical algorithms Framingham, SCORE, REGICOR , as they include age and sex, total cholesterol or LDL, and smoking.
The basic cardiovascular complications produced by hyperglycemia in DM2 are microangiopathic disease diabetic nephropathy, retinopathy, and diabetic neuropathy and CVD diabetic macroangiopathy. These include coronary heart disease and stroke as the main complications, although peripheral arterial disease is also common and tends to be more serious higher indices of serious ischemia and amputations when it is cause by diabetes than when it is caused by other mechanisms.
Micro- and macroangiopathy exist side by side and their harmful effects are multiplied in DM2. Damage to the endothelium produced by accumulation of glucosilation sub-products, reduced production of nitric oxide, and endothelial inflammation are among the most characteristic mechanisms involved in the process.
Over the last 50 years, people have experienced drastic changes in their environment, behavior, and lifestyles. These changes have led to the alarming increase in incidence of diabetes and obesity. Data from successive cohorts of the National Health and Nutrition Examination Survey NHANES 22 show that the mean waist circumference of adults in the USA increased by 3.
After adjusting by age, the largest increases in waist circumference were observed in the youngest age group years. Over the past 20 years, prevalence rates for obesity have tripled in developing countries which have adopted western lifestyles.
These have shown the typical patterns of reduced physical activity and over consumption of high energy-density meals. There have been several studies into the prevalence of obesity in the Spanish general population.
Figure 5. Prevalence of weight alterations in men A and women B in the MESYAS 23 register of 18 healthy men and women. One of the reasons for the current interest in MS is its high prevalence.
Figure 6. Prevalence of metabolic syndrome in the MESYAS 23 register by age and gender in 18 healthy members of the working population.
Finally, the DM2 epidemic is expanding principally in developed and developing countries. Estimates are not very encouraging and have taken public health authorities by surprise.
Worldwide, the number of those with DM2 is expected to grow from the current million to million in and to million in This trend towards an increased prevalence of DM2 and obesity presents a real challenge for public health systems practically the whole world over and will continue to do so into the foreseeable future Figure 7.
Figure 7. Diabetes cases in millions of individuals in and predicted for Obesity and Metabolic Syndrome. Diagnosis in individuals with obesity and MS should take into account the progressive nature of these conditions. In general, their evolution can be summarized in 4 phases, beginning with the presence of certain causal factors central adiposity and insulin resistance, as well as genetic factors.
These give rise to the metabolic alterations described above high blood pressure, dyslipidemia, and glucose metabolism disorders which in turn are followed by the development of vasculopathy.
This is initially subclinical but eventually manifests as characteristic atherothrombotic complications and DM2 Figure 3. Diagnosis should therefore not be limited to determining the presence of metabolic alterations, but should also explore the possibility of vasculopathic complications.
Given the high risk associated with both diseases over the long term, it would seem logical to suggest that overall cardiovascular risk be assessed in all obese individuals or those with MS.
Such an assessment should include checking on the presence and magnitude of MS components. Medium-term risk should be evaluated using risk prediction models adapted whenever possible to the local population, and the possibility of sub-clinical vasculopathy should be investigated using the appropriate procedures.
Signs of asymptomatic vasculopathy can be studied in all in vascular territories mostly affected by atherosclerosis Table 4. The possibility of an effect on cerebral blood flow can be studied by determining the intima media thickness of the common carotid artery, while the impact on peripheral circulation is measured most precisely using abdominal ultrasound to determine the diameter of the aorta.
The ankle-brachial index can also be used as a non-invasive method to detect peripheral vascular disease, which correlates with vascular risk. Other, more general signs of sub-clinical vasculopathy are microalbuminuria and erectile dysfunction.
Diabetes is now considered a vascular disease even when it clinical complications are not present. This approach is clearly important from the treatment point of view, though it is more doubtful when it comes to diagnosis, and has led to disagreement with the European Society of Cardiology's clinical practice guidelines on diabetes and pre-diabetes which strongly recommend that tests to detect myocardial ischemia are performed on all patients with DM2.
Table 5 provides a summary of the general approach to treating the metabolic syndromes. Lifestyle is key to the treatment of DM2, MS, and obesity. The three basic components in any such improvement are diet, exercise, and behavior. The first essential step is weight loss Figure 5.
This apparently simple step which is in fact the most difficult to achieve and, therefore, the least frequently achieved has demonstrated numerous beneficial effects: it reduces mortality, improves lipid profiles, reduces blood pressure and left ventricle mass in hypertension, and it reduces inflammation markers in DM2.
Furthermore, in patients with MS it has been shown that it slows progression to DM2. As well as the quantitative aspect of a reduction in caloric uptake, dietary composition can also affect vascular health.
Avoiding fats other than those from olive oil, increasing the consumption of fruits, vegetables, and whole-food cereals, avoiding industrially sweetened products and fatty meats, and eating white and especially blue fish are some of the recommendations in this regard Table 6.
Exercise has similar beneficial effects in MS, obesity, and DM2. As well as helping to achieve and maintain weight loss, it also reduces all of the components of MS and reduces the incidence of CVD. It may be stating the obvious to insist that patients should be encouraged to give up smoking, but it is not enough only to offer advice; health care professionals should ensure they provide the requisite support for stopping smoking at all levels of cardiovascular risk.
Treatment of High Blood Pressure. Angiotensin converting enzyme ACE inhibitors have demonstrated multiple beneficial effects on cardiovascular complications and for that reason are considered the first line, or preferred treatment for high blood pressure, particularly when established or incipient kidney disease is present.
Beta-blockers are indicated where coronary artery disease or heart failure are present. Diuretics showed a satisfactory anti-hypertensive effect in some studies, 38 though they also led to a worsened metabolic status 39 and have no effect on arterial rigidity.
For these reasons, beta-blockers and diuretics are considered complementary to ACE inhibitors and calcium channel blockers, with which they can be carefully used in combination to achieve appropriate levels of blood pressure control.
Lipid-Lowering Treatment. Lipid-lowering treatments are used based on the initial levels of lipids in blood with the aim of reaching targets set in international guidelines Figure 8 , ie LDL 13, Figure 8.
HDL indicates high density lipoproteins; LDL, low density lipoproteins. Statins are the drug of choice to lower LDL levels. The dose should be based on the size of the reduction required in LDL cholesterol.
Any of the drugs in the group should be suitable; the important thing is to pursue and achieve the required dose and the targets set. Fibrates are considered more effective than statins in lowering triglyceride and raising HDL levels, due to their agonist effect on PPARa.
They might therefore appear to be an ideal treatment for atherogenic dyslipidemia in diabetes mellitus. This has led to its usefulness as a preventive treatment being questioned. Medical and physiologic measurements are taken during a physical examination We linked NHANES data with data from the National Death Index from to ; this database provides follow-up mortality data for up to months for NHANES participants aged 18 or older A minimum of 10 years is suggested for observing the effects of MetS on mortality We then excluded participants if they had BMI less than The final analytic sample of 12, participants aged 20 to 85 had data for all variables examined in our study, eligible follow-up mortality data, and no preexisting frailty.
NHANES collects data for people older than 85 but does not report these extreme values to protect privacy. Random subsampling accounted for most missing data points.
Subsamples of participants were randomly selected to participate in various survey topics or laboratory testing. For example, less than one-third of all participants were tested for fasting glucose or triglycerides. Each subsample was further weighted so that each represents the US population for the given year.
We categorized the study sample into 3 weight groups based on BMI according to standard definitions: normal weight We further divided each weight group into 2 groups according to whether the participant met criteria for MetS.
Because of differences in questionnaires between NHANES cycles, we included only leisure-time physical activity in our analysis. Initial analyses using SAS complex survey frequency and means procedures that take into account weighting, stratification, and clustering of the data generated the descriptive statistics.
We used the LIFETEST procedure to generate the unadjusted mortality data for each MetS—BMI category and the log rank test to determine significant differences between categories.
Other important risk factors such as blood pressure, cholesterol, and blood glucose were already included in the definition of MetS.
We excluded covariates, such as alcohol consumption, that did not significantly improve the statistical model. We used the 6-level BMI—MetS variable to find the hazard ratio of each group compared with the normal-weight—no-MetS group for all-cause mortality, cardiovascular mortality, and cancer mortality.
The 6 groups were normal-weight—MetS, normal-weight—no-MetS, overweight—MetS, overweight—no-MetS, obese—MetS, and obese—no-MetS. We chose the normal-weight—no-MetS group as the referent because we hypothesized that it would be the healthiest.
We then tested the moderating effect of BMI on MetS and mortality by testing the interaction between weight groups and MetS.
To support the interaction analysis, we also tested the effect of MetS in each weight group, using the contrast statement to directly compare normal-weight—MetS participants and participants in other categories.
In a further analysis, while accounting for the complex sampling design and controlling for the same covariates, to determine the incremental influence of MetS on mortality, we compared each MetS group with their no-MetS counterparts in each BMI group.
We performed all statistical analyses in using SAS version 9. We found significant differences in the prevalence of MetS and weight groups for all demographic variables. Groups with MetS were generally older, less educated, and less physically active and had a lower income and a higher prevalence of smoking than their no-MetS counterparts Table 1.
According to the product-limit method from the LIFETEST procedure Figure 1 , the normal-weight—MetS group had the highest mortality rate. Each no-MetS group had significantly lower mortality than their MetS counterparts, but we found no significant differences among no-MetS groups.
Figure 1. Unadjusted mortality curve during person-month follow-up for each MetS—BMI category, National Health and Nutrition Examination Survey, —, and National Death Index, Abbreviation: BMI, body mass index; MetS, metabolic syndrome.
Follow-up by group ranged from 29, person-months normal-weight—MetS group to , person-months normal-weight—no-MetS group Table 2. Unadjusted mortality rates showed that the normal-weight—MetS group had the highest mortality per person-month, followed by the overweight—MetS group and the obese—MetS group.
The HR was higher in the normal-weight—MetS group than in the obese—MetS group, although the difference was not significant HR, 1. In the test of the interaction between weight groups and MetS, the P value for the interaction term in the full model was.
When we directly compared the normal-weight—MetS group with other groups, we found an HR of 0. In analyses of cause-specific mortality Figure 2 , we found that among total deaths, weighted, The adjusted Cox regression model for cardiovascular mortality showed a significant hazard ratio only for the normal-weight—MetS group HR, 2.
The model for cancer mortality showed a significant hazard ratio for the overweight—MetS group HR, 1. Figure 2. Weight—MetS categories and all-cause and selected cause-specific mortality, National Health and Nutrition Examination Survey, —, and National Death Index, The normal-weight—no-MetS group was used as the reference group.
Abbreviations: MetS, metabolic syndrome; NWMS; normal-weight—MetS; OWNMS, overweight—no MetS; OWMS, overweight—MetS; OBNMS, obese—no MetS; OBMS, obese—MetS. When we compared adults with MetS in each weight group with the no-MetS group Table 3 , we found that only the normal-weight—MetS group had a significant hazard ratio HR, 1.
Although the obese—MetS group had a significantly higher HR when compared with the normal-weight—no-MetS group HR, 1. When we evaluated mortality risk by obesity and MetS categories, only the normal-weight and obese groups with MetS had a significantly higher hazard ratio than the reference group, adults with normal-weight and no MetS.
Although the normal-weight group had lowest prevalence of MetS, it also had the highest hazard ratio. Analysis of cardiovascular mortality showed a significantly higher hazard ratio only for the normal-weight—MetS group, which suggests a strong effect of MetS on cardiovascular death in normal-weight adults.
Cancer mortality was significantly higher in the overweight—MetS and obese—MetS groups, compared with the normal-weight—no-MetS group, which is consistent with a previous study that found strong associations between adiposity and risk for many types of cancers The most likely explanation for the higher mortality in the normal-weight—MetS group is the influence of MetS through obesity-independent risk pathways.
Although obesity is a known, common risk factor for MetS, MetS in the normal-weight population is likely due to factors independent of obesity. If these obesity-independent factors result in a more severe form of MetS, the normal-weight—MetS group would show a higher mortality rate than the obese—MetS group, whose mortality rate is attenuated by the less severe MetS caused by obesity.
Previous studies on normal-weight obesity attribute the cause of MetS in normal-weight adults to excess body fat percentage despite a normal overall weight. Obesity is accompanied by a large number of coagulation and fibrinolytic abnormalities This suggests that obesity induces a prothrombotic state.
What is not known at present is how a prothrombotic state will either promote the development of atherosclerosis or participate in the development of acute ASCVD events. Perhaps the most attractive candidate for enhanced atherogenicity associated with coagulation and fibrinolytic abnormalities is endothelial dysfunction.
It is believed by many workers that endothelial dysfunction is somehow involved in the atherogenic process Several pathways have been proposed; so far, however, none of these have been substantiated. Perhaps more likely, the obesity-induced procoagulant and antifibrinolytic factors contribute to a worsening of acute coronary syndromes.
Thrombosis occurring with plaque rupture or erosion is a key element in determining the severity of the syndrome. If normal coagulation and fibrinolysis are impaired at the time of plaque rupture or erosion, then a larger thrombus should form.
An attractive hypothesis is that acute plaque disruption is common, but only when thrombosis is large is there a significant acute coronary syndrome. If so, such could make the presence of a prothrombotic state important for determining the clinical outcome.
The cardiovascular field has recently shown great interest in the role of inflammation in the development of ASCVD. The basic concept is that atherogenesis represents a state of chronic inflammation.
It is characterized by lipid-induced injury that initiates invasion of macrophages followed by proliferation of smooth muscle cells.
All of these processes are classic features of chronic inflammation albeit occurring at a very slow rate. The finding that elevations of serum CRP carry predictive power for the development of major cardiovascular events led to the concept that advanced and unstable atherosclerotic plaques are in an even higher state of inflammation than stable plaques 9.
It is of interest that obese persons 42 and particularly those with the metabolic syndrome 43 also have elevated levels of CRP.
This finding has suggested that obesity is a proinflammatory state and is somehow connected with the development of unstable atherosclerotic plaques. So far, however, a mechanistic connection has not been made.
The associations are suggestive, but how elevations of CRP associated with obesity could promote or precipitate major cardiovascular events is not clear. This lack of identified mechanism does not rule out a causative connection. But so far the connection has not been uncovered.
Obesity is a major underlying risk factor for ASCVD. It is associated with multiple ASCVD risk factors, and it also is a risk factor for type 2 diabetes.
Diabetes itself is a cardiovascular risk factor. Despite the strong association between obesity and ASCVD, the mechanisms underlying this relationship are not well understood.
Our understanding of the connection between obesity and vascular disease is complicated by a plethora of possibilities.
Obesity acts on so many metabolic pathways, producing so many potential risk factors, that it is virtually impossible to differentiate between the more important and less important.
The possibilities for confounding variables are enormous. This complexity provides a great challenge for basic and clinical research.
It also raises the possibility for new targets of therapy for the metabolic syndrome. With this said, the fundamental challenge is how to intervene at the public health level to reduce the high prevalence of obesity in the general population. This approach offers the greatest possibility for reducing the cardiovascular risk that accompanies obesity.
Circulation : — Google Scholar. National Cholesterol Education Program NCEP Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults Adult Treatment Panel III Third Report of the National Cholesterol Education Program NCEP Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults Adult Treatment Panel III final report.
Arterioscler Thromb Vasc Biol 24 : e13 — e National Institutes of Health. Obes Res 6 Suppl 2 S—S. Bosello O , Zamboni M Visceral obesity and metabolic syndrome. Obes Rev 1 : 47 — Abate N , Garg A , Peshock RM , Stray-Gundersen J , Grundy SM Relationships of generalized and regional adiposity to insulin sensitivity in men.
J Clin Invest 96 : 88 — Abate N , Garg A , Peshock RM , Stray-Gundersen J , Adams-Huet B , Grundy SM Relationship of generalized and regional adiposity to insulin sensitivity in men with NIDDM. Diabetes 45 : — Unwin N , Shaw J , Zimmet P , Alberti KG Impaired glucose tolerance and impaired fasting glycaemia: the current status on definition and intervention.
Diabet Med 19 : — Ridker PM High-sensitivity C-reactive protein and cardiovascular risk: rationale for screening and primary prevention. Am J Cardiol 92 : 17 K—22K. Einhorn D ACE position statement on insulin resistance syndrome.
Endocr Pract 9 : — Ford ES , Giles WH , Dietz WH Prevalence of the metabolic syndrome among U. Findings from the Third National Health and Nutrition Survey. JAMA : — Guerre-Millo M Adipose tissue hormones.
J Endocrinol Invest 25 : — Heptulla R , Smitten A , Teague B , Tamborlane WV , Ma YZ , Caprio S Temporal patterns of circulating leptin levels in lean and obese adolescents: relationships to insulin, growth hormone, and free fatty acids rhythmicity. J Clin Endocrinol Metab 86 : 90 — Randle PJ , Garland PB , Hales CN , Newesholme EA The glucose fatty-acid cycle.
Its role in insulin sensitivity and the metabolic disturbances of diabetes mellitus. Lancet 1 : — Shulman GI Cellular mechanisms of insulin resistance. J Clin Invest : — Ruderman NB , Saha AK , Vavvas D , Witters LA Malonyl-CoA, fuel sensing, and insulin resistance.
Am J Physiol 1 Pt 1 : E1 — E Grundy SM Metabolic complications of obesity. Endocrine 13 : — Engeli S , Sharma AM Role of adipose tissue for cardiovascular-renal regulation in health and disease. Horm Metab Res 32 : — Juhan-Vague I , Morange PE , Alessi MC The insulin resistance syndrome: implications for thrombosis and cardiovascular disease.
Pathophysiol Haemost Thromb 32 : — Ridker PM , Morrow DA C-reactive protein, inflammation, and coronary risk. Cardiol Clin 21 : — Alessi MC , Peiretti F , Morange P , Henry M , Nalbone G , Juhan-Vague I Production of plasminogen activator inhibitor 1 by human adipose tissue: possible link between visceral fat accumulation and vascular disease.
Diabetes 46 : — Ouchi N , Kihara S , Funahashi T , Matsuzawa Y , Walsh K Obesity, adiponectin and vascular inflammatory disease.
Curr Opin Lipidol 14 : — Unger RH Lipotoxic diseases. Annu Rev Med 53 : — Steppan CM , Lazar MA Resistin and obesity-associated insulin resistance Trends. Endocrinol Metab 13 : 18 — Isomaa B , Almgren P , Tuomi T , Forsen B , Lahti K , Nissen M , Taskinen MR , Group L Cardiovascular morbidity and mortality associated with the metabolic syndrome.
Diabetes Care 24 : — Alexander CM , Landsman PB , Teutsch SM , Haffner SM Third National Health and Nutrition Examination Survey NHANES III ; National Cholesterol Education Program NCEP. NCEP-defined metabolic syndrome, diabetes, and prevalence of coronary heart disease among NHANES III participants age 50 years and older.
Diabetes 52 : — Hunt K, Resendez R, Williams K, Haffner S, Stern M NCEP versus WHO metabolic syndrome in relation to all cause and cardiovascular mortality in the San Antonio Heart Study SAHS.
Diabetes 52 i6 pA—A Abstract. Lakka HM , Laaksonen DE , Lakka TA , Niskanen LK , Kumpusalo E , Tuomilehto J , Salonen JT The metabolic syndrome and total and cardiovascular disease mortality in middle-aged men. Krauss RM Atherogenicity of triglyceride-rich lipoproteins. Am J Cardiol 81 : 13 B—17B.
Krauss RM Dense low density lipoproteins and coronary artery disease. Am J Cardiol 75 : 53 B—57B. Blake GJ , Otvos JD , Rifai N , Ridker PM Low-density lipoprotein particle concentration and size as determined by nuclear magnetic resonance spectroscopy as predictors of cardiovascular disease in women.
Grundy SM Low-density lipoprotein, non-high-density lipoprotein, and apolipoprotein B as targets of lipid-lowering therapy. Chobanian AV , Bakris GL , Black HR , Cushman WC , Green LA , Izzo Jr JL , Jones DW , Materson BJ , Oparil S , Wright Jr JT , Roccella EJ; Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure; National Heart, Lung, and Blood Institute; National High Blood Pressure Education Program Coordinating Committee Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure.
Hypertension 42 : — Barrett-Connor E , Khaw KT Is hypertension more benign when associated with obesity?
Circulation 72 : 53 — Carman WJ , Barrett-Connor E , Sowers M , Khaw KT Higher risk of cardiovascular mortality among lean hypertensive individuals in Tecumseh, Michigan. Circulation 89 : — Kannel WB , Zhang T , Garrison RJ Is obesity-related hypertension less of a cardiovascular risk?
The Framingham Study. Am Heart J : — N Engl J Med : — Aronson D , Rayfield EJ How hyperglycemia promotes atherosclerosis: molecular mechanisms. Cardiovasc Diabetol 1 : 1. Haffner SM Cardiovascular risk factors and the prediabetic syndrome.
Ann Med 28 : — De Pergola G , Pannacciulli N Coagulation and fibrinolysis abnormalities in obesity. Widlansky ME , Gokce N , Keaney Jr JF , Vita JA The clinical implications of endothelial dysfunction.
J Am Coll Cardiol 42 : — Visser M , Bouter LM , McQuillan GM , Wener MH , Harris TB Elevated C-reactive protein levels in overweight and obese adults. Ridker PM Clinical application of C-reactive protein for cardiovascular disease detection and prevention.
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide. Sign In or Create an Account. Endocrine Society Journals. Advanced Search.
Search Menu. Article Navigation. Close mobile search navigation Article Navigation. Volume Article Contents Categories of obesity. Body fat and metabolic syndrome. Inflammatory cytokines.
Other adipose tissue products.
Mushroom Industry Trends can Nutritional periodization principles in response Obesity and metabolic syndrome metxbolic variety of stimuli, including metwbolic agents, tissue injury, autoimmune diseases, and obesity. Some of these metabloic are acute and resolve, while ,etabolic become chronic and exert a sustained impact on the Dairy-free soups, systemically, or locally. Anx is Obrsity recognized as merabolic chronic low-grade, systemic inflammatory state that predisposes to other chronic conditions including metabolic syndrome MetS. Although obesity has received considerable attention regarding its pathophysiological link to chronic cardiovascular conditions and type 2 diabetes, the musculoskeletal MSK complications i. As musculoskeletal diseases can lead to the worsening of MetS, this underscores the imminent need to understand the cause and effect relations between the two, and the convergence between inflammatory pathways that contribute to MSK damage. Muscle mass is a key predictor of longevity in older adults, and obesity-induced sarcopenia is a significant risk factor for adverse health outcomes.
Die Idee gut, ist mit Ihnen einverstanden.
Mich beunruhigt diese Frage auch.
Wacker, Sie hat der bemerkenswerte Gedanke besucht