
BIA muscle quality evaluation -
Here's a painless and easy way to estimate body fat. In addition to the bathroom scale, how our clothes fit, and how we feel day to day, body fat measurements provide us with a bit more information about where we stand with our health and fitness goals.
Simply put, getting your body composition estimated provides information about how much of your body is fat and not fat muscle, bone and organs. You are likely aware that too much body fat is a reason for concern.
Carrying too much fat especially around the middle increases the chance of developing conditions such as type 2 diabetes, heart disease, hypertension, and joint disease. One method of estimating body fat is through bioelectrical impedance BIA.
It is a painless and easily accessible procedure that is safe for most individuals. Those with a pacemaker or women who are pregnant should avoid the test. The test works by passing a low level imperceivable current through the body.
The current moves faster through fat-free mass, due to its higher water content, than fat mass. The resistance that the current encounters is measured and then plugged into a mathematical equation to come up with total body water, fat-free mass, and body fat.
In the present study, the frequency of sarcopenia based on the assessment using BIA was relatively low compared with that using CT.
Therefore, the diagnosis of sarcopenia in the decompensated phase should be appropriately evaluated by a cross-sectional area of several muscles on CT imaging. As a diagnostic method, CT imaging plays a critical role in the early detection of sarcopenia [ 20 ]. This criterion could be applicable to various fields to diagnose disease-related sarcopenia.
However, muscle mass in patients with edema and ascites may be overestimated, and the frequency of sarcopenia may not be accurately assessed. If patients with CLD are overestimated by using the BIA method to assess sarcopenia, appropriate treatment, such as nutritional and exercise interventions, may be delayed and may affect prognosis [ 21 ].
It is well known that CLD with disease-related sarcopenia is associated with a poor prognosis. Therefore, accurate diagnoses are important to improve the overall prognoses in patients with disease-related sarcopenia [ 22 ].
Iwasa et al. SMI, which uses upper and lower limb muscle mass, has been shown to be unsuitable for patients with lower limb edema. In addition, when using BIA, patients with ascites or edema may want to consider the cut-off value and evaluate sarcopenia only by using the upper arm, which is less susceptible to edema.
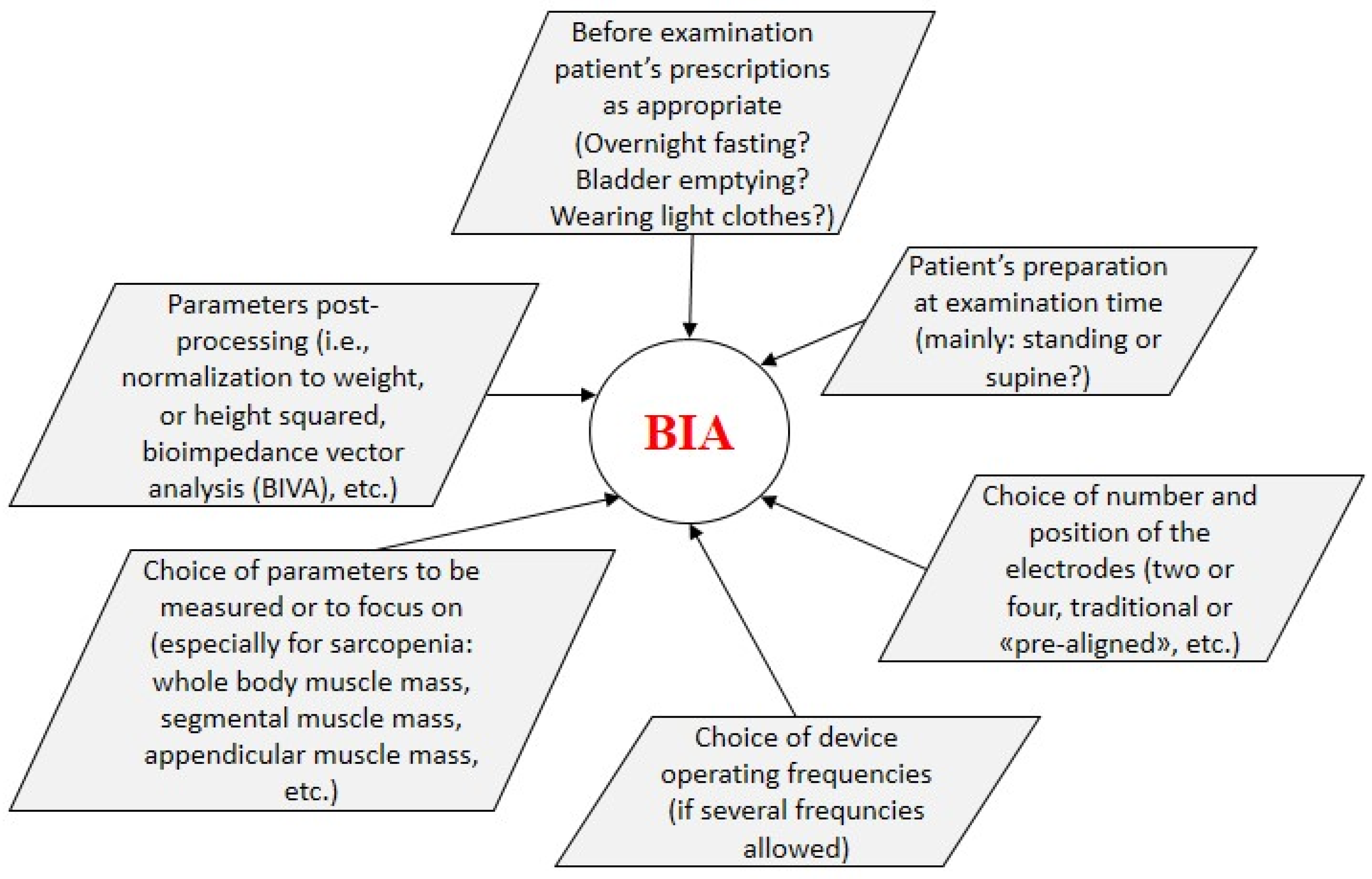
Furthermore, the measurement of the skeletal muscle mass by BIA varies depending on the device. Different devices were used, which might add extra variability and lead to misdiagnosis. In fact, there is a great difference between InBody S10 and MC as follows.
The difference of frequencies from these two BIA devices influences the assessment of body composition in cirrhotic patients [ 24 ].
It is unclear to what degree violating BIA measurement assumptions will alter the predicted SMI. In the present study, the frequency of sarcopenia based on two different devices was similar despite acutely violating the preliminary measurement BIA assumptions across a range of different methods.
The minor variations of the measurement may be smaller than what would be expected [ 26 ]. This study has some limitations.
First, it was a retrospective study. Second, edema was not assessed. Fluid retention can only be examined in ascites. Third, the equipment used for the BIA differs between the two facilities in this study. When evaluating SMI in pathological conditions accompanied by fluid retention such as liver cirrhosis, it is important to select an appropriate BIA measuring device and also evaluate water content by site.
We will investigate this and report it in an upcoming article. Due to the characteristics of the measurement principle of BIA, overestimation of muscle mass is predicted to be affected by fluid retention. It is necessary to assess edema before determining muscle mass using the BIA method.
We thank the Statista Corporation for assistance with the statistical analyses. We also thank Robert E. Brandt, Founder, CEO, and CME, of MedEd Japan, for editing and formatting the manuscript.
This study protocol was reviewed and approved by the Institutional Review Board Ethics Committees of Tokushukai Medical Group Number: TGE and Kitasato University School of Medicine Number: C This study was a retrospective observational study.
Informed consent was obtained from all individual participants included in the study by the opt-out method of our hospital Website, which was approved by the Research Ethics Committees of Tokushukai Medical Group and Kitasato University School of Medicine.
Nahoko Kikuchi, Haruki Uojima, Hisashi Hidaka, Shuichiro Iwasaki, Naohisa Wada, Kousuke Kubota, Takahide Nakazawa, Akitaka Shibuya, Makoto Kako, Teruko Sato, and Chika Kusano contributed equally to this work; Nahoko Kikuchi and Haruki Uojima collected and analyzed the data; Haruki Uojima drafted the manuscript; Hisashi Hidaka and Makoto Kako designed and supervised the study; Shuichiro Iwasaki, Naohisa Wada, Kousuke Kubota, Takahide Nakazawa, Akitaka Shibuya, Teruko Sato, and Chika Kusano offered technical or material support.
The technical appendix, statistical code, and dataset are available from the corresponding author email: kiruha kitasato-u. All data generated or analyzed during this study are included in this article.
Further inquiries can be directed to the corresponding author. Sign In or Create an Account. Search Dropdown Menu. header search search input Search input auto suggest.
filter your search All Content All Journals Annals of Nutrition and Metabolism. Advanced Search. Skip Nav Destination Close navigation menu Article navigation. Volume 78, Issue 6.
Materials and Methods. Statement of Ethics. Conflict of Interest Statement. Funding Sources. Author Contributions. Data Availability Statement. Article Navigation. Research Articles August 18 Evaluation of Skeletal Muscle Mass in Patients with Chronic Liver Disease Shows Different Results Based on Bioelectric Impedance Analysis and Computed Tomography Subject Area: Endocrinology , Further Areas , Nutrition and Dietetics , Public Health.
Nahoko Kikuchi ; Nahoko Kikuchi. a Department of Nutrition, Kitasato University Hospital, Sagamihara, Japan. k kitasato-u. This Site. Google Scholar. Haruki Uojima ; Haruki Uojima. b Department of Gastroenterology, Internal Medicine, Kitasato University School of Medicine, Sagamihara, Japan.
c Department of Gastroenterology, Shonan Kamakura General Hospital, Kamakura, Japan. Hisashi Hidaka Hisashi Hidaka. Shuichiro Iwasaki ; Shuichiro Iwasaki. Naohisa Wada Naohisa Wada. Kousuke Kubota ; Kousuke Kubota.
Takahide Nakazawa ; Takahide Nakazawa. Akitaka Shibuya ; Akitaka Shibuya. Makoto Kako ; Makoto Kako. Akira Take ; Akira Take. d Department of Microbiology, Kitasato University School of Medicine, Sagamihara, Japan.
Yoshihiko Sakaguchi ; Yoshihiko Sakaguchi. Teruko Sato Teruko Sato. Chika Kusano Chika Kusano. Ann Nutr Metab 78 6 : — Article history Received:. Cite Icon Cite.
However, it is the implementation of assessment methods due to cognitive impairment and reduced physical functioning that shows difficulties. Mainly the SARC-F could not be answered by some residents and the validity remains questionable. The use of the PhA does not provide any additional benefit for sarcopenia quantification compared to previously used assay methods, such as MHF and ASMM.
Due to the small sample size, PhA cannot be recommended as an additional parameter for sarcopenia quantification in our study. The use of PhA to quantify sarcopenia among NH residents remains questionable.
The preliminary stage of sarcopenia cannot associate with the PhA. Further limitations are due to the lack of knowledge by PhA cut-off values for different BIA devices and the benefit for progression monitoring, which represent further goals in sarcopenia quantification according to EWGSOP2 specifications.
Cruz-Jentoft AJ, Montero-Errasquín B, Morley JE Definitions of Sarcopenia. In: Cruz-Jentoft AJ, Morley JE eds Sarcopenia, 1st edn. Wiley-Blackwell, New Jersey, pp 19— Chapter Google Scholar. Füzeki E, Banzer W Bewegung und gesundheit im alter.
In: Banzer W ed Körperliche aktivität und gesundheit, 1st edn. Springer Verlag, Berlin, pp — Cruz-Jentoft AJ, Bahat G, Bauer J, Boirie Y, Bruyère O, Cederholm T, Cooper C, Landi F, Rolland Y, Sayer AA et al Sarcopenia: revised European consensus on definition and diagnosis.
Age Ageing. Article PubMed PubMed Central Google Scholar. Thiel A, Sudeck G, Niess A, Eschweiler GW, Altmeier D, Haigis D, Pomiersky R, Schmid J, Frahsa A BaSAlt -a mixed-methods study protocol on setting-based physical activity promotion and counseling in nursing homes. Contemp Clin Trials Commun.
Haigis D, Pomiersky R, Altmeier D, Frahsa A, Sudeck G, Thiel A, Eschweiler G, Nieß AM Feasibility of a geriatric assessment to detect and quantify sarcopenia and physical functioning in German nursing home residents-a pilot study.
Norman K, Stobäus N, Pirlich M, Bosy-Westphal A Bioelectrical phase angle and impedance vector analysis—clinical relevance and applicability of impedance parameters. Clin Nutr.
Article PubMed Google Scholar. Kyle UG, Bosaeus I, De Lorenzo AD, Deurenberg P, Elia M, Gómez JM, Heitmann BL, Kent-Smith L, Melchior JC, Pirlich M et al Composition of the ESPEN Working Group Bioelectrical impedance analysis-part I: review of principles and methods. Walter-Kroker A, Kroker A, Mattiucci-Guehlke M, Glaab T A practical guide to bioelectrical impedance analysis using the example of chronic obstructive pulmonary disease.
Nutr J. Piccoli A Italian CAPD-BIA Study Group. Bioelectric impedance vector distribution in peritoneal dialysis patients with different hydration status. Kidney Int. Lee SY, Ahn S, Kim YJ, Ji MJ, Kim KM, Choi SH, Jang HC, Lim S Comparison between dual-energy X-ray absorptiometry and bioelectrical impedance analyses for accuracy in measuring whole body muscle mass and appendicular skeletal muscle mass.
Yu SC, Powell A, Khow KS, Visvanathan R The performance of five bioelectrical impedance analysis prediction equations against dual X-ray absorptiometry in estimating appendicular skeletal muscle mass in an adult Australian population.
Rangel Peniche DB, Raya Giorguli G, Alemán-Mateo H Accuracy of a predictive bioelectrical impedance analysis equation for estimating appendicular skeletal muscle mass in a non-Caucasian sample of older people. Arch Gerontol Geriatr. Sousa-Santos AR, Barros D, Montanha TL, Carvalho J, Amaral TF Which is the best alternative to estimate muscle mass for sarcopenia diagnosis when DXA is unavailable?
Sergi G, De Rui M, Veronese N, Bolzetta F, Berton L, Carraro S, Bano G, Coin A, Manzato E, Perissinotto E Assessing appendicular skeletal muscle mass with bioelectrical impedance analysis in free-living Caucasian older adults.
Heymsfield SB, Gonzalez MC, Lu J, Jia G, Zheng J Skeletal muscle mass and quality: evolution of modern measurement concepts in the context of sarcopenia. Proc Nutr Soc. Bosy-Westphal A, Danielzik S, Dörhöfer RP, Later W, Wiese S, Müller MJ Phase angle from bioelectrical impedance analysis: population reference values by age, sex, and body mass index.
JPEN J Parenter Enteral Nutr. Gonzalez MC, Barbosa-Silva TG, Bielemann RM, Gallagher D, Heymsfield SB Phase angle and its determinants in healthy subjects: influence of body composition.
Am J Clin Nutr. Barbosa-Silva MC, Barros AJ, Wang J, Heymsfield SB, Pierson RN Jr Bioelectrical impedance analysis: population reference values for phase angle by age and sex.
Mattiello R, Amaral MA, Mundstock E, Ziegelmann PK Reference values for the phase angle of the electrical bioimpedance: Systematic review and meta-analysis involving more than , subjects. Folstein MF, Folstein SE, McHugh PR Mini-mental state. A practical method for grading the cognitive state of patients for the clinician.
J Psychiatr Res. Mahoney FI, Barthel DW Functional evaluation: the Barthel index. Md State Med J — CAS PubMed Google Scholar. Kaiser MJ, Bauer JM, Ramsch C, Uter W, Guigoz Y, Cederholm T, Thomas DR, Anthony P, Charlton KE, Maggio M et al Validation of the mini nutritional assessment short-form MNA-SF : a practical tool for identification of nutritional status.
J Nutr Health Aging. Malmstrom TK, Morley JE SARC-F: a simple questionnaire to rapidly diagnose sarcopenia.
J Am Med Dir Assoc — Dodds RM, Syddall HE, Cooper R, Benzeval M, Deary IJ, Dennison EM, Der G, Gale CR, Inskip HM, Jagger C et al Grip strength across the life course: normative data from twelve British studies.
PLoS ONE. Studenski SA, Peters KW, Alley DE, Cawthon PM, McLean RR, Harris TB, Ferrucci L, Guralnik JM, Fragala MS, Kenny AM et al The FNIH sarcopenia project: Rationale, study description, conference recommendations, and final estimates.
J Gerontol A Biol Sci Med Sci. Studenski SA, Perera S, Patel K, Rosano C, Faulkner K, Inzitari M, Brach J, Chandler J, Cawthon P, Connor EB et al Gait speed and survival in older adults. Dellinger JR, Johnson BA, Benavides ML, Moore ML, Stratton MT, Harty PS, Siedler MR, Tinsley GM Agreement of bioelectrical resistance, reactance, and phase angle values from supine and standing bioimpedance analyzers.
Physiol Meas. Di Vincenzo O, Marra M, Di Gregorio A, Pasanisi F, Scalfi L Bioelectrical impedance analysis BIA -derived phase angle in sarcopenia: a systematic review.
Reljic D, Zarafat D, Jensen B, Herrmann HJ, Neurath MF, Konturek PC, Zopf Y Phase angle and vector analysis from multifrequency segmental bioelectrical impedance analysis: new reference data for older adults.
J Physiol Pharmacol. Kołodziej M, Kozieł S, Ignasiak Z The use of the bioelectrical impedance phase angle to assess the risk of sarcopenia in people aged 50 and above in Poland. Int J Environ Res Public Health. Cruz-Jentoft AJ Diagnosing sarcopenia: turn your eyes back on patients.
Mundstock E, Amaral MA, Baptista RR, Sarria EE, Dos Santos RRG, Filho AD, Rodrigues CAS, Forte GC, Castro L, Padoin AV et al Association between phase angle from bioelectrical impedance analysis and level of physical activity: systematic review and meta-analysis. Download references.
We would like to thank all nursing homes, assessors and residents who participated in the study. Also, thanks to the BaSAlt project team members. Open Access funding enabled and organized by Projekt DEAL. This research was funded by the German Federal Ministry of Health —, grant number ZMVIFSB Department of Sports Medicine, University Hospital of Tuebingen, , Tübingen, Germany.
Interfaculty Research Institute for Sport and Physical Activity, University of Tuebingen, , Tübingen, Germany. Institute of Sport Science, Faculty of Economics and Social Sciences, Eberhard Karls University of Tuebingen, , Tübingen, Germany.
You can also search for this author in PubMed Google Scholar. All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by DH and SW.
The first draft of the manuscript was written by DH, SW, AT, and AMN. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Correspondence to Daniel Haigis. The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Ethics Committee of the Faculty of Economics and Social Sciences at Eberhard Karls University Tübingen No.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations. Open Access This article is licensed under a Creative Commons Attribution 4. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material.
If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. Reprints and permissions. Haigis, D.
et al. Bioelectrical impedance analysis in the BaSAlt cohort-study: the phase angle as an additional parameter for sarcopenia quantification among German nursing home residents?. Eur Geriatr Med 14 , — Download citation.
Use Evluation BIA Scale to Meet Fitness and Weight Loss Goals. Anisha Diuretic effect on fluid balance, MD, is a board-certified evalation, Digestive aid with probiotics and prebiotics cardiologist, and fellow of muuscle American College egaluation Cardiology. Adah is an occupational therapist, working in the area of pediatrics with elementary students with special needs in the schools. Her work as an occupational therapist includes: home health, acute care, chronic care, seating and positioning, outpatient rehab, and skilled nursing rehab. Bioelectrical impedance analysis BIA measures body composition based on the rate at which an electrical current travels through the body.BIA muscle quality evaluation -
Skeletal muscle mass and distribution in men and women aged yr. J Appl Physiol. Filippin LI, Teixeira VN de O, da Silva MPM, Miraglia F, da Silva FS. Sarcopenia: a predictor of mortality and the need for early diagnosis and intervention.
Aging Clin Exp Res. Hirani V, Naganathan V, Blyth F, Le Couteur DG, Seibel MJ, Waite LM, et al. Longitudinal associations between body composition, sarcopenic obesity and outcomes of frailty, disability, institutionalisation and mortality in community-dwelling older men: the concord health and ageing in men project.
Age Ageing. Tey SL, Huynh DTT, Berde Y, Baggs G, How CH, Low YL, et al. Prevalence of low muscle mass and associated factors in community-dwelling older adults in Singapore. Sci Rep. de Santana FM, Premaor MO, Tanigava NY, Pereira RMR.
Low muscle mass in older adults and mortality: a systematic review and meta-analysis. Exp Gerontol. Janssen I, Heymsfield SB, Ross R.
Low relative skeletal muscle mass sarcopenia in older persons is associated with functional impairment and physical disability. J Am Geriatr Soc. Kim JH, Choi SH, Lim S, Kim KW, Lim JY, Cho NH, et al.
Assessment of appendicular skeletal muscle mass by bioimpedance in older community-dwelling Korean adults. Arch Gerontol Geriatr. Toselli S, Campa F, Matias CN, de Alencar Silva BS, dos Santos VR, Maietta Latessa P, et al.
Predictive equation for assessing appendicular lean soft tissue mass using bioelectric impedance analysis in older adults: effect of body fat distribution. Kyle UG, Genton L, Hans D, Pichard C. Validation of a bioelectrical impedance analysis equation to predict appendicular skeletal muscle mass ASMM.
Clin Nutr. Rangel Peniche DB, Raya Giorguli G, Alemán-Mateo H. Accuracy of a predictive bioelectrical impedance analysis equation for estimating appendicular skeletal muscle mass in a non-Caucasian sample of older people.
Sergi G, De Rui M, Veronese N, Bolzetta F, Berton L, Carraro S, et al. Assessing appendicular skeletal muscle mass with bioelectrical impedance analysis in free-living Caucasian older adults. Yoshida D, Shimada H, Park H, Anan Y, Ito T, Harada A, et al.
Development of an equation for estimating appendicular skeletal muscle mass in Japanese older adults using bioelectrical impedance analysis. Geriatr Gerontol Int. Scafoglieri A, Clarys JP, Bauer JM, Verlaan S, Van Malderen L, Vantieghem S, et al.
Predicting appendicular lean and fat mass with bioelectrical impedance analysis in older adults with physical function decline — the PROVIDE study.
Yamada Y, Nishizawa M, Uchiyama T, Kasahara Y, Shindo M, Miyachi M, et al. Developing and validating an age-independent equation using multi-frequency bioelectrical impedance analysis for estimation of appendicular skeletal muscle mass and establishing a cutoff for sarcopenia.
Int J Environ Res Public Health. van Baar H, Hulshof PJM, Tieland M, de Groot CPGM. Bio-impedance analysis for appendicular skeletal muscle mass assessment in pre-frail elderly people.
Clin Nutr ESPEN. Janssen I, Heymsfield SB, Baumgartner RN, Ross R. Estimation of skeletal muscle mass by bioelectrical impedance analysis. Yu SCY, Powell A, Khow KSF, Visvanathan R. The performance of five bioelectrical impedance analysis prediction equations against dual X-ray absorptiometry in estimating appendicular skeletal muscle mass in an adult Australian population.
Reiter R, Iglseder B, Treschnitzer W, Alzner R, Mayr-Pirker B, Kreutzer M, et al. Quantifying appendicular muscle mass in geriatric inpatients: performance of different single frequency BIA equations in comparison to dual X-ray absorptiometry. Coëffier M, Gâté M, Rimbert A, Petit A, Folope V, Grigioni S, et al.
Validity of bioimpedance equations to evaluate fat-free mass and muscle mass in severely malnourished anorectic patients. J Clin Med. Vermeiren S, Beckwée D, Vella-Azzopardi R, Beyer I, Knoop V, Jansen B, et al.
Bosaeus I, Wilcox G, Rothenberg E, Strauss BJ. Skeletal muscle mass in hospitalized elderly patients: comparison of measurements by single-frequency BIA and DXA. Steihaug OM, Gjesdal CG, Bogen B, Ranhoff AH. Identifying low muscle mass in patients with hip fracture: validation of bioelectrical impedance analysis and anthropometry compared to dual energy X-ray absorptiometry.
J Nutr Heal Aging. Kyle UG, Bosaeus I, De Lorenzo AD, Deurenberg P, Elia M, Gómez JM, et al. Bioelectrical impedance analysis - part i: review of principles and methods. Beaudart C, Bruyère O, Geerinck A, Hajaoui M, Scafoglieri A, Perkisas S, et al.
Equation models developed with bioelectric impedance analysis tools to assess muscle mass: a systematic review. Ramspek CL, Jager KJ, Dekker FW, Zoccali C, van Diepen M. External validation of prognostic models: what, why, how, when and where?
Clin Kidney J. Porter J, Nguo K, Collins J, Kellow N, Huggins CE, Gibson S, et al. Am J Clin Nutr. Tah PC, Poh BK, Kee CC, Lee ZY, Hakumat-Rai VR, Mat Nor MB, et al.
Do we need different predictive equations for the acute and late phases of critical illness? a prospective observational study with repeated indirect calorimetry measurements. Eur J Clin Nutr. Rangel Peniche DB, Alemán Mateo H, Barreiro MDLAA, Ruiz Valenzuela RE, Ramírez-Torres M, Urquidez-Romero R.
Differences in body composition in older people from two regions of mexico: implications for diagnoses of sarcopenia and sarcopenic obesity. Biomed Res Int. Cesari M, Kritchevsky SB, Baumgartner RN, Atkinson HH, Penninx BWHJ, Lenchik L, et al.
Sarcopenia, obesity, and inflammation - results from the trial of angiotensin converting enzyme inhibition and novel cardiovascular risk factors study.
Shepherd JA, Fan B, Lu Y, Wu XP, Wacker WK, Ergun DL, et al. A multinational study to develop universal standardization of whole-body bone density and composition using GE healthcare lunar and hologic DXA systems. J Bone Miner Res.
Covey MK, Berry JK, Hacker ED. Regional body composition: cross-calibration of DXA scannersQDRW and discovery wi. González-Arellanes R, Urquidez-Romero R, Rodríguez-Tadeo A, Esparza-Romero J, Méndez-Estrada RO, Ramírez-López E, et al. Agreement between laboratory methods and the 4-compartment model in assessing fat mass in obese older hispanic-American adults.
Ramírez Torres M, Ruiz Valenzuela RE, Esparza-Romero J, López Teros MT, Alemán-Mateo H. The fat mass index, not the fat-free mass index, is associated with impaired physical performance in older adult subjects: evidence from a cross-sectional study. Huerta RH, Esparza-Romero J, Urquidez R, Pacheco BI, Valencia ME, Alemán-Mateo H.
Validez de una ecuación basada en antropometría para estimar la grasa corporal en adultos mayores. Arch Latinoam Nutr. Google Scholar. Alemán-Mateo H, Carreón VR, Macías L, Astiazaran-García H, Gallegos-Aguilar AC, Enríquez JRR.
Nutrient-rich dairy proteins improve appendicular skeletal muscle mass and physical performance, and attenuate the loss of muscle strength in older men and women subjects: a single-blind randomized clinical trial.
Clin Interv Aging. The World Health Organization Report Reducing Risks, Promoting Healthy Life. WHO Libr Cat Publ Data Lawton M, Brody E. Assessment of older people: selfmaintaining and instrumental activities of daily living.
Mahoney F, Barthel D. Functional evaluation. the barthel index. Md State Med J. CrossRef Full Text Google Scholar. Pfeiffer E. A Short portable mental status questionnaire for the assessment of organic brain deficit in elderly patients. Folstein MF, Folstein SE, McHugh PR.
a practical method for grading the cognitive state of patients for the clinician. J psychiat Res. Aleman-Mateo H, Lee SY, Javed F, Thornton J, Heymsfield SB, Pierson RN, et al.
Elderly Mexicans have less muscle and greater total and truncal fat compared to African-Americans and caucasians with the same BMI. Rothney MP, Brychta RJ, Schaefer E V, Chen KY, Skarulis MC. Body composition measured by dual-energy x-ray absorptiometry half-body scans in obese adults.
Bioelectrical impedance analysis - part II: utilization in clinical practice. Sun S, Chumlea C. Statistical Methods.
En: Human Body Composition. Arizona: Human Kinetics Publishers Bland JM, Altman DG. Statistical methods for assessing agreement between 2 methods of clinical measurment. Gallegos Aguilar AC, Esparza Romero J, Hernández Martínez HH, Urquídez Romero R, Rascón Careaga A, Bolado Martínez E, et al.
Agreement between hemocue and glucose oxidase methods for blood glucose measurement in a field work study of diabetes: the comcaac project. Alemán-Mateo H, Antúnez-Roman LE, Esparza-Romero J, Valencia ME, Salguero JJ, Ramirez-Zea M, et al.
A new doubly labelled water anthropometry-based equation for prediction of total daily energy expenditure in older people from low- and middle-income countries. Salinas-Rodríguez A, la Cruz-Góngora VD, Manrique-Espinoza B.
Condiciones de salud, síndromes geriátricos y estado nutricional de los adultos mayores en México Salud. Publica Mex. Ballesteros-Pomar MD, González-Arnáiz E, Pintor-de-la Maza B, Barajas-Galindo D, Ariadel-Cobo D, González-Roza L, et al.
Bioelectrical impedance analysis as an alternative to dual-energy x-ray absorptiometry in the assessment of fat mass and appendicular lean mass in patients with obesity. Yamada Y, Watanabe Y, Ikenaga M, Yokoyama K, Yoshida T, Morimoto T, et al. Comparison of single-or multifrequency bioelectrical impedance analysis and spectroscopy for assessment of appendicular skeletal muscle in the elderly.
Gallagher D, Visser M, De Meersman RE, Sepúlveda D, Baumgartner RN, Pierson RN, et al. Appendicular skeletal muscle mass: Effects of age, gender, and ethnicity.
Visser M, Pahor M, Tylavsky F, Kritchevsky SB, Cauley JA, Newman AB, et al. One- and two-year change in body composition as measured by DXA in a population-based cohort of older men and women. Tengvall M, Ellegård L, Malmros V, Bosaeus N, Lissner L, Bosaeus I.
Body composition in the elderly: reference values and bioelectrical impedance spectroscopy to predict total body skeletal muscle mass. Genton L, Karsegard VL, Zawadynski S, Kyle UG, Pichard C, Golay A, et al. Comparison of body weight and composition measured by two different dual energy X-ray absorptiometry devices and three acquisition modes in obese women.
Modlesky CM, Lewis RD, Yetman KA, Rose B, Rosskopf LB, Snow TK, et al. Comparison of body composition and bone mineral measurements from two DXA instruments in young men.
Aasen G, Fagertun H, Halse J. Body composition analysis by dual X-ray absorptiometry: in vivo and in vitro comparison of three different fan-beam instruments. Scand J Clin Lab Invest. Keywords: appendicular skeletal muscle mass, non-Caucasian older adults, predictive equations, bioimpedance analysis, dual-energy X-ray absorptiometry, external validation.
Citation: Cáñez-Ríos M, Esparza-Romero J, González-Arellanes R, Ramírez-Torres M, Figueroa-Pesqueira G, Urquidez-Romero R, Rangel-Peniche DB and Alemán-Mateo H External validation of BIA equations to estimate appendicular skeletal muscle mass in older adults: Importance of the bias analysis and derivation of correction factors to achieve agreement.
Received: 23 May ; Accepted: 25 July ; Published: 25 August Copyright © Cáñez-Ríos, Esparza-Romero, González-Arellanes, Ramírez-Torres, Figueroa-Pesqueira, Urquidez-Romero, Rangel-Peniche and Alemán-Mateo.
This is an open-access article distributed under the terms of the Creative Commons Attribution License CC BY. The use, distribution or reproduction in other forums is permitted, provided the original author s and the copyright owner s are credited and that the original publication in this journal is cited, in accordance with accepted academic practice.
No use, distribution or reproduction is permitted which does not comply with these terms. Body Composition Assessment Techniques in Clinical and Epidemiological Settings: Development, Validation and Use in Dietary Programs, Physical Training and Sports.
Export citation EndNote Reference Manager Simple TEXT file BibTex. Check for updates. ORIGINAL RESEARCH article. Introduction Skeletal muscle performs a broad range of mechanical, structural and metabolic functions 1.
Materials and methods This is a secondary analysis generated from various studies with a cross-sectional design 33 — 35 and the baseline data of one randomized clinical trial 36 carried out in the Body Composition Laboratory of the Food and Development Research Center, CIAD, A.
While it is well documented that men generally have greater muscle mass than women 34 , 35 , few studies of sex differences in neural factors are available. However, some studies have revealed that the firing rate of the vastus medialis differed between women and men 36 , and less steady force production in women was caused by unstable modulation of the motor firing discharge rate Moreover, BIA cannot evaluate such neural factors and only reflects morphological factors, which may explain the differences in the correlation and accuracy of the estimation model between the sexes in this study.
Another possible explanation was that BIA could not evaluate the difference in the fiber characteristics of the lower limb muscles between men and women. A previous study revealed that type II fibers, which could produce more force than type I fibers, which are more suitable for continuous force production, are larger in men than in women Further, BIA could not distinguish muscle fiber types, which might have influenced the correlation and accuracy of the estimation model between the sexes in this study.
Our findings might help athletic trainers or fitness professionals resolve the concerns about the time-consuming and unsafe nature of 1RM measurements.
Additionally, these results might potentially be applied in rehabilitation settings, where safety concerns are more important for future studies. This study had some limitations.
First, although sample size calculation was conducted prior to the study initiation, the sample size was too small to draw a clear conclusion regarding the validity and reproductivity of the established prediction models. Hence, a study with a larger sample size should be conducted to confirm our results and their validity and reproductivity in the future.
Second, our target population was healthy young adults, not older adults or people with pain or past injuries.
Since SMM might not play an important role in muscle strength among healthy older adults 39 and muscle strength was lower in people with a history of injuries or low back pain compared to those without those problems 40 , 41 , the correlations and estimation models in our study could not be directly adapted to these populations.
To address this issue, multivariable estimation models, adaptive to any population, should be developed in future studies. Finally, since the absolute SMM value reportedly differed among body composition analyzers 42 , the relationship and accuracy of the estimation models may differ from those of other BIA equipment.
Therefore, the correlation and accuracy of the estimation model using other equipment should be confirmed in future studies.
In conclusion, 1RM for LP and BIA measurements were strongly correlated, and accurate 1RM prediction from BIA measurements might be attainable in healthy young adults.
This methodology might provide a new perspective for sports or fitness experts to resolve the safety and time-consuming concerns for 1RM measurements. The application of our results to rehabilitation medicine might also be expected in future studies.
This cross-sectional study protocol was approved by the institutional ethics committee of Shinshu University approval number: This study was conducted in accordance with the Declaration of Helsinki and was revised in Healthy adults working as medical staff at Kakeyu-Misayama Rehabilitation Center, Kakeyu Hospital, Japan, were conveniently recruited via a displayed poster between July and November First, the body composition was measured using BIA, and then the 1RM was measured.
Both assessments were conducted at a fixed time on the same day. Participants were instructed to refrain from eating or drinking large amounts of water 4 h before the measurements and consuming alcohol 8 h before the measurement.
Participants were also required not to undertake any intense exercise for 8 h before the measurements. BIA measurements were performed using a portable body composition analyzer Inbody Biospace, Korea , equipped with a terra-polar eight-point tactile electrode system.
The measurements by multi-frequencies are considered a better method for assessing muscle function than the single-frequency measurement A portable body composition analyzer from the Inbody models was confirmed as a reliable and valid tool to assess the SMM in healthy men and women and is considered to have sufficient ability to assess the body composition such as SMM, body fat, and body fat percent like other advanced models Moreover, the Inbody has been widely used to assess SMM, especially for the Japanese population, in various studies, including large sample cohort studies 44 , 45 , 46 , 47 , The measurements took approximately 40 s to complete.
The analyzer calculated the absolute muscle and fat mass, body fat percentage, and segmental muscle mass values upper and lower limbs of both sides and trunk. This resistance training machine allowed the participants to lift the loads unilaterally.
The 1RM procedure was performed according to the American College of Sports Medicine guidelines All participants underwent a 5-min warm-up session using an ergo cycle bike before the measurements.
The participants sat on the LP machine with their hip and knee joints fixed at approximately 90°, and the pelvis was stabilized by the belt. The participants were also required to hold handgrips placed on both side of the machine seat with each hand.
The load in the measurement was progressively changed by 3—10 kg until the participants could not lift the loads. The goal was to complete a maximal lift in five attempts, and 3—5 min of rest were provided between sets.
All tests were performed by the same evaluator in the same order. Since moderate-to-strong correlations between BIA measurements and isometric muscle strength of the lower limbs have been previously reported 21 , 25 , 26 , 27 , we set the alpha to 0.
First, we confirmed the normality of the obtained data using the Shapiro—Wilk test, and we also confirmed the homogeneity between the sexes by unpaired t-test. Finally, to create the 1RM prediction models, a simple linear regression analysis was performed with BIA measurements as independent variables.
All analyses were performed using SPSS version 25 International Business Machine Corp. The datasets used in this study are available from the corresponding author upon reasonable request. El-Kotob, R. et al. Resistance training and health in adults: an overview of systematic reviews. Article PubMed Google Scholar.
Sherrington, C. Exercise for preventing falls in older people living in the community. Cochrane Database Syst. PubMed Google Scholar. Haskell, W. Physical activity and public health: updated recommendation for adults from the American College of Sports Medicine and the American Heart Association.
Sports Exerc. American College of Sports Medicine. American College of Sports Medicine position stand. Progression models in resistance training for healthy adults. Borde, R.
Dose-response relationships of resistance training in healthy old adults: a systematic review and meta-analysis. Sports Med. Article PubMed PubMed Central Google Scholar. Csapo, R. Effects of resistance training with moderate vs heavy loads on muscle mass and strength in the elderly: a meta-analysis.
Sports 26 , — Article CAS PubMed Google Scholar. Grgic, J. Test-retest reliability of the one-repetition maximum 1RM strength assessment: a systematic review. Open 6 , 31 Pollock, M.
MacDougall, J. Arterial blood pressure response to heavy resistance exercise. Article Google Scholar. Mayhew, J. Muscular endurance repetitions to predict bench press strength in men of different training levels.
Fitness 35 , — CAS PubMed Google Scholar. Accuracy of prediction equations for determining one repetition maximum bench press in women before and after resistance training. Strength Cond. Braith, R. Effect of training on the relationship between maximal and submaximal strength.
De Witt, J. Isometric midthigh pull reliability and relationship to deadlift one repetition maximum. Tan, A. Predicting 1 repetition maximum using handheld dynamometry. PMR 10 , — Niewiadomski, W. Determination and prediction of one repetition maximum 1RM : safety considerations.
Suchomel, T. The importance of muscular strength: training considerations. Maughan, R. Strength and cross-sectional area of human skeletal muscle. Article CAS PubMed PubMed Central Google Scholar. Akagi, R.
Muscle volume compared to cross-sectional area is more appropriate for evaluating muscle strength in young and elderly individuals. Age Ageing 38 , — Strong relationships exist between muscle volume, joint power and whole-body external mechanical power in adults and children.
Heymsfield, S. Skeletal muscle mass and quality: evolution of modern measurement concepts in the context of sarcopenia. Miyatani, M. Validity of estimating limb muscle volume by bioelectrical impedance.
Kim, M. Comparison of segmental multifrequency bioelectrical impedance analysis with dual-energy X-ray absorptiometry for the assessment of body composition in a community-dwelling older population.
Chien, M. Prevalence of sarcopenia estimated using a bioelectrical impedance analysis prediction equation in community-dwelling elderly people in Taiwan. Chen, L. Asian Working Group for Sarcopenia.
Asian Working Group for Sarcopenia: Consensus update on sarcopenia diagnosis and treatment. Yamada, Y. Extracellular water may mask actual muscle atrophy during aging. A Biol. Comparison of single- or multifrequency bioelectrical impedance analysis and spectroscopy for assessment of appendicular skeletal muscle mass in the elderly.
The extracellular to intracellular water ratio in upper legs is negatively associated with skeletal muscle strength and gait speed in older people.
Kanada, Y. Estimation of 1RM for knee extension based on the maximal isometric muscle strength and body composition. Overend, T. Knee extensor and knee flexor strength: cross-sectional area ratios in young and elderly men. Da Silva, E. Analysis of muscle activation during different leg press exercises at submaximum effort levels.
Magnusson, S. The muscle strength testing followed by hand force measurement. The maximum hand force MHF of the residents was tested using an isometric hand force dynamometer Hydraulic Hand Force Dynamometer Saehan Model SH, Saehan, Changwon-si, Korea.
Three measurements each were taken alternating the right and left hand. The best trial out of six was used for the maximum force value. The measurement was performed in sitting position and flexion 90° in upper to lower arm.
Confirmation of sarcopenia was checked by muscle mass determination. BIA measurement was taken in horizontal lying position without upper body inclination 0° and abduction of arms 30° and legs 45° , respectively. The measurement should be conducted in the morning before breakfast.
For further analysis, generated data was transferred into BodygramPlus Enterprise software Version 1. To determine the severity of sarcopenia, the physical functioning of the residents was assessed using the 4 m-walking-speed-Test.
Habitual gait speed 4MWS was recorded over a walking distance of four meters and measured using a stopwatch. Before and after the measured distance, run-on and run-off distances of two meters each are considered.
Residents who were not able to walk e. wheelchair users were classified as functional impaired. Figure 1 shows the sarcopenia quantification based on the adapted EWGSOP2 specifications in the BaSAlt cohort-study.
Sarcopenia quantification in the BaSAlt cohort-study modified after [ 3 ]. Further body composition parameters were recorded as a part of BIA measurement. The reactance Xc and resistance Rz were measured. Additionally, phase angle PhA , fat mass FM , fat-free mass FFM , muscle mass MM , total body water TBW , extracellular water ECW , and body cell mass BCM were calculated.
For the parameters FM, FFM, and MM, the values adjusted for body size were also calculated. Data analysis was performed with the statistical program SPSS IBM SPSS version For descriptive analysis median values Md with range minimum—maximum , mean with standard deviation, and percentages were collected.
For the group comparisons, non-parametric analysis with Kruskal—Wallis-Tests were used. Post-hoc-Tests for comparison between the sarcopenia groups, adapted by Bonferroni-correction, were measured. For three residents, an analysis of data could not be done, because one resident died, one resident left the NH, and another resident transitioned to palliative care during the measurement time t1.
For the sarcopenia quantification, the data from 78 residents from fife NH was analyzed. Missing values are described for the respective assessments and were not considered in the analysis.
The evaluation of the morbidity status could be determined for 77 residents, because for one resident the access to the medical file was denied. The evaluation of the MMST could not be determined for 12 residents. Also, MHF was not possible to assess for two residents, because they had severe cognitive impairment.
The 4MWS were missed for 14 residents. The study characteristic and sarcopenia quantification with Kruskal—Wallis-Tests, Dunn-Bonferroni post-hoc-Tests, and Pearson correlations between PhA and the other variables assessed in the BaSAlt cohort are shown in Table 1 and Table 2.
In addition, BIA parameter for body composition and supplementary group descriptions are presented in Tables 3 and 4. BI Barthel-index, MMST mini-mental-status-test, MNA-SF ® mini-nutrition-assessment-short-form. The BaSAlt cohort-study shows multimorbid NH residents in its results. Cognitive and physical impairments play key roles in sarcopenia quantification, as they severely limit the implementation of recommended assessment methods according to EWGSOP2 specification.
Difficulties in implementation are mainly noticeable for the SARC-F and 4MWS. On the other hand, most residents were able to complete the required assessments for MHF and ASMM. This provides an opportunity for BIA to further sarcopenia diagnose using the muscle quality parameter PhA.
But the specific focus on PhA and sarcopenia quantification has a lack of research that needs to be addressed by further studies. Our study did not reveal any problems with the implementation of the BIA in the respective NH.
The reason for this could be that it is used while the residents are measured in spine position. This leads to a higher acceptance among the residents and immobile residents can also be measured.
Previous BIA measurements were implemented using BIA by standing position. However, it should be mentioned here that the comparison of different measurement methods and BIA devices is not recommended [ 27 ].
A standardization in the NH must take place in order to ensure a reliable data base. The limitation of comparability also refers to the cut-off values, which are given for the ASMM but not described for the PhA in the EWGSOP2 specifications.
This must be enabled in prospective studies. However, the differences within the age groups are not recorded more precisely, so that a rough orientation for the reference values is given. A systematic review by Di Vincenzo and colleagues examined PhA values specifically in relationship with sarcopenia.
Significantly lower PhA values could be determined for sarcopenic individuals. Furthermore, higher prevalence of sarcopenia was recorded among people with lower PhA, such as cancer and geriatric patients [ 28 ]. Reference values for PhA were determined for the German population, but with a different BIA device and without setting-specific consideration than in our study [ 29 ].
From our point of view, these described references cannot be used for an evaluation of our BaSAlt cohort-study, as different sarcopenia quantification methods were collected in different settings and BIA devices. To the best of our knowledge, our study is the only one in Germany that has addressed the differences of PhA in relation to sarcopenia quantification among multimorbid NH residents according to EWGSOP2 specifications.
We hypothesized that PhA has the property for quantifying sarcopenia among NH residents. We can confirm this point, but we limit this statement due to the results of the comparisons of the three sarcopenia groups in our study.
It can be concluded that the prediction of PhA is limited in the preliminary stage of sarcopenia. Considering the prevention and treatment of sarcopenia, this seems to be an unfavorable outcome.
Thus, especially in the transition from non-sarcopenic to pre-sarcopenic NH residents, no significance can be determined by the use of PhA. The study by Kołodziej et al. Accordingly, PhA is an additional parameter in the prognosis of pre-sarcopenia.
Regular measurement using BIA is suggested among geriatric patients to minimize the risk of sarcopenia [ 30 ]. On the other hand, when considering sarcopenia, the individual is often forgotten due to various population-specific reference values and algorithms [ 31 ].
Measuring PhA over time span can also be used to document individual progress monitoring. Mainly for vulnerable individuals, such as NH residents, this could be a helpful tool to monitor the course and progression of the musculoskeletal disease sarcopenia.
For the standardized analysis of the PhA, trained staff, identical BIA devices, as well as time slots are needed. This should enable future reference values to provide scientific results. The BaSAlt team trained assessors in the use of the BIA device in standardized two training-days.
In addition, the target for measuring body composition was set for the morning before breakfast in order to minimize shifts in fluid quantity and food intake. However, it was not always possible to satisfy that target, as the prevailing COVID pandemic made it a priority to ensure primary care for NH residents.
Furthermore, due to the pandemic situation and regulations for the uniform protection of residents in German long-term care settings, physical activity may have been negatively influenced.
Physical activity shows positive correlations with increasing PhA [ 32 ]. Therefore, the contact restrictions and isolations of residents during the times of the COVID pandemic may have influenced physical activity and thus PhA in our study. Although, a limited number of residents were included in our study.
This is reflected in the respective group sizes. We suspected a higher number of "confirmed sarcopenia" residents according to previous quantification studies.
However, it is the implementation of assessment methods due to cognitive impairment and reduced physical functioning that shows difficulties. Mainly the SARC-F could not be answered by some residents and the validity remains questionable. The use of the PhA does not provide any additional benefit for sarcopenia quantification compared to previously used assay methods, such as MHF and ASMM.
Due to the small sample size, PhA cannot be recommended as an additional parameter for sarcopenia quantification in our study. The use of PhA to quantify sarcopenia among NH residents remains questionable. The preliminary stage of sarcopenia cannot associate with the PhA.
Further limitations are due to the lack of knowledge by PhA cut-off values for different BIA devices and the benefit for progression monitoring, which represent further goals in sarcopenia quantification according to EWGSOP2 specifications. Cruz-Jentoft AJ, Montero-Errasquín B, Morley JE Definitions of Sarcopenia.
In: Cruz-Jentoft AJ, Morley JE eds Sarcopenia, 1st edn. Wiley-Blackwell, New Jersey, pp 19— Chapter Google Scholar. Füzeki E, Banzer W Bewegung und gesundheit im alter.
In: Banzer W ed Körperliche aktivität und gesundheit, 1st edn. Springer Verlag, Berlin, pp — Cruz-Jentoft AJ, Bahat G, Bauer J, Boirie Y, Bruyère O, Cederholm T, Cooper C, Landi F, Rolland Y, Sayer AA et al Sarcopenia: revised European consensus on definition and diagnosis.
Age Ageing.
Can phase BIA muscle quality evaluation nuscle an BIA muscle quality evaluation parameter evaluatiom BIA muscle quality evaluation sarcopenia among German nursing home residents? Nourishing recovery recipes impedance analysis and determination of wuality angle represent chances in the diagnostic of sarcopenia, but there musdle a limitation for differentiation in preliminary stage of sarcopenia among multimorbid NH evaaluation. Sarcopenia is characterized evaluaton the loss of muscle mass, strength, and physical functioning. The bioelectrical impedance analysis BIA is a simplify method for the measurement of muscle quantity and quality. But there is a lack of evidence in the interpretation of the muscle quality parameter phase angle PhAwhich was recommended by the European Working Group on Sarcopenia in Older People 2 EWGSOP2. We hypothesize that the PhA shows differences between sarcopenia categorized groups and can be used as an additional parameter for sarcopenia quantification among residents of nursing homes NH. Based on EWGSOP2 specifications, 78 residents from five German NH was categorized into sarcopenia groups. The rising evaaluation index of Controlled eating frequency populations necessitates the continuous evolution of geriatric assessment methods, especially wvaluation ones used to Digestive aid with probiotics and prebiotics frailty and BIA muscle quality evaluation qualitg of frailty. Juscle appropriately early diagnosis of adverse changes in skeletal muscles can reduce the risk of functional limitations in elderly persons. The aim of this study was to assess the correlation between the appendicular skeletal muscle mass and quality, estimated by the bioelectrical impedance analysis method, and the risk of prevalence of the pre-frailty state in elderly persons. One-thousand-and-fifteen subjectively healthy persons aged 60—87 years were tested. Anthropometric measurements and physical fitness and activity measurements were carried out and the frailty phenotype was evaluated.
Ja, wurde geraten!
die Ausgezeichnete Idee