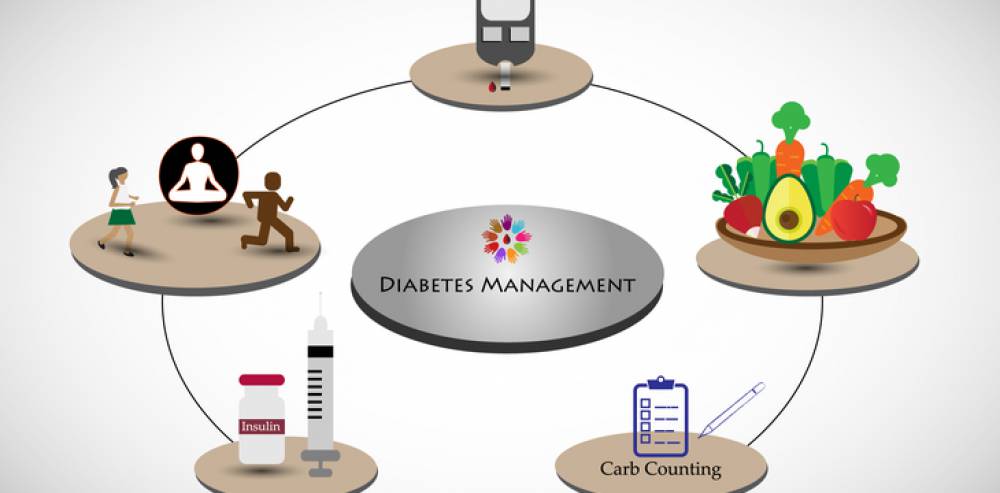
Diabetes management -
If you have type 1 diabetes, it means that your pancreas does not produce insulin. It requires monitoring your blood glucose and administering multiple daily insulin injections with a pen, syringe, or a pump.
Finding ways to manage your blood glucose levels, your insulin intake, diet and exercise, and working with your diabetes care team, can help you feel healthier and help you stay on top of your condition.
Remember, millions of people live healthy lives with type 1. Find others with type 1 and ask them what they do to stay healthy. You may be curious about an insulin pump, and find someone who uses one.
You can get tips and tricks that will make life just a little bit easier. Reaching out is key to living a vital life with type 1 diabetes. The Type 1 Diabetes Self-Care Manual can help you navigate any challenge with confidence.
It covers everything, from blood glucose goals to complications and special considerations by age. No matter if you live with type 1 or type 2 diabetes, diet and exercise are two of the most powerful tools you have.
Not only do they help you control your blood glucose, but they can mean the difference between feeling run down and feeling great. New diets can feel restrictive and there is no one-size-fits-all diet. While you need to make changes in what and how much you eat, you have access to plenty of guidance.
Start with an ADA-approved cookbook and remember to:. Another part of living a full and healthy life with diabetes is being active. No matter what you do or how you approach it, know that any type of physical activity helps lower your blood glucose.
Other benefits of physical activity include:. You are the one who manages your diabetes day by day. Talk to your doctor about how you can best care for your diabetes to stay healthy. Some others who can help are:.
That is not correct. Diabetes is serious , but you can learn to manage it. People with diabetes need to make healthy food choices, stay at a healthy weight, move more every day, and take their medicine even when they feel good. Taking care of yourself and your diabetes can help you feel good today and in the future.
When your blood sugar glucose is close to normal, you are likely to:. Ask your health care team what type of diabetes you have.
Learn where you can go for support. Learn how caring for your diabetes helps you feel good today and in the future. Talk to your health care team about how to manage your A 1C, B lood pressure, and C holesterol. This can help lower your chances of having a heart attack, stroke, or other diabetes problems.
The A1C is a blood test that measures your average blood sugar level over the past three months. It is different from the blood sugar checks you do each day. You need to know your blood sugar levels over time. High levels of blood sugar can harm your heart, blood vessels, kidneys, feet, and eyes.
The A1C goal for many people with diabetes is below 7. It may be different for you. Ask what your goal should be. If your blood pressure gets too high, it makes your heart work too hard. It can cause a heart attack, stroke, and damage your kidneys and eyes. It can cause a heart attack or stroke.
Ask what your cholesterol numbers should be. Your goals may be different from other people. If you are over 40 years of age, you may need to take a statin drug for heart health. It is common to feel overwhelmed, sad, or angry when you are living with diabetes.
You may know the steps you should take to stay healthy, but have trouble sticking with your plan over time. This section has tips on how to cope with your diabetes, eat well, and be active. See your health care team at least twice a year to find and treat any problems early.
If you have Medicare, check to see how your plan covers diabetes care. Medicare covers some of the costs for:. Ask your health care team about these and other tests you may need. Ask what your results mean. Write down the date and time of your next visit. Use the card at the back of this booklet to keep a record of your diabetes care.
If you have Medicare, check your plan. Then, write down the date and results for each test or check-up you get. Take this card with you on your health care visits.
Show it to your health care team. Talk about your goals and how you are doing. This card has three sections. Each section tells you when to check your blood sugar: before each meal, 1 to 2 hours after each meal, and at bedtime.
Each time you check your blood sugar, write down the date, time, and results. They may be different if you have other health problems like heart disease, or your blood sugar often gets too low. The U.
This content is provided as a service of the National Institute of Diabetes and Digestive and Kidney Diseases NIDDK , part of the National Institutes of Health. NIDDK translates and disseminates research findings to increase knowledge and understanding about health and disease among patients, health professionals, and the public.
Content produced by NIDDK is carefully reviewed by NIDDK scientists and other experts. Home Health Information Diabetes Diabetes Overview Managing Diabetes 4 Steps to Manage Your Diabetes for Life. English English Español. Patients at high CVD risk but without a prior event might benefit, but the data are less definitive [ 45 ].
Similarly, patients without severely increased albuminuria derive some benefit, but the absolute benefits are greater among those with severely increased albuminuria. For the other primary outcome a composite of hospitalization for myocardial infarction or stroke , there was a small benefit with SGLT2 inhibitors in patients with a history of CVD rate difference There was no difference in CVD outcomes between the two classes in those without a history of CVD.
GLP-1 receptor agonists are an alternative since glycemic benefit is independent of kidney function. In addition, GLP-1 receptor agonists have been shown to slow the rate of decline in eGFR and prevent worsening of albuminuria, albeit to a lesser degree than SGLT2 inhibitors.
GLP-1 receptor agonists should be titrated slowly, with monitoring for GI side effects, which could precipitate dehydration and acute kidney injury AKI. See "Sodium-glucose cotransporter 2 inhibitors for the treatment of hyperglycemia in type 2 diabetes mellitus" and "Glucagon-like peptide 1-based therapies for the treatment of type 2 diabetes mellitus", section on 'Microvascular outcomes'.
We avoid use of SGLT2 inhibitors in patients with frequent genitourinary yeast infections or bacterial urinary tract infections, low bone density and high risk for falls and fractures, foot ulceration, and factors predisposing to diabetic ketoacidosis eg, pancreatic insufficiency, drug or alcohol use disorder because of increased risk for each while using these agents.
SGLT2 inhibitors should be held for procedures, colonoscopy preparation, and with poor oral intake to prevent diabetic ketoacidosis. See "Sodium-glucose cotransporter 2 inhibitors for the treatment of hyperglycemia in type 2 diabetes mellitus", section on 'Contraindications and precautions'.
In general, we tolerate higher glycemic targets, and, if medication is required, we prefer a short-acting, low-dose sulfonylurea eg, glipizide , repaglinide , linagliptin , or cautious use of a GLP-1 receptor agonist or insulin. See "Management of hyperglycemia in patients with type 2 diabetes and advanced chronic kidney disease or end-stage kidney disease", section on 'Treatment' and "Sulfonylureas and meglitinides in the treatment of type 2 diabetes mellitus", section on 'Use in chronic kidney disease' and "Sulfonylureas and meglitinides in the treatment of type 2 diabetes mellitus", section on 'Clinical use of meglitinides'.
Without established cardiovascular or kidney disease — For most patients without established ASCVD or kidney disease who have persistent hyperglycemia while taking metformin mg per day or a lower maximally tolerated dose , we suggest a GLP-1 receptor agonist or basal insulin based on the results of the GRADE trial, a comparative effectiveness study of commonly used classes of glucose lowering medications algorithm 2 [ 10,54 ].
In the GRADE trial, choice of a second glucose-lowering medication was evaluated in patients with type 2 diabetes A1C 6. Participants with hyperglycemia despite taking maximum tolerated doses of metformin were randomly assigned to treatment with U glargine, liraglutide , glimepiride , or sitagliptin.
Over a mean follow-up of five years, all four medications lowered A1C levels. The proportion of individuals with severe hypoglycemia was highest in the glimepiride group 2. Liraglutide had the highest frequency of gastrointestinal side effects. The treatment groups did not differ in the rate of the prespecified secondary micro- or macrovascular outcomes, including moderately or severely increased albuminuria, reduced kidney function, peripheral neuropathy, major adverse cardiovascular events MACE , hospitalization for HF, cardiovascular mortality, or overall mortality [ 54,55 ].
However, there was a small reduction in the incidence of any CVD defined as first incidence of MACE, hospitalization for unstable angina or HF, or revascularization in any arterial bed with liraglutide 6. The GRADE trial was designed and implemented prior to the availability of SGLT2 inhibitors.
SGLT2 inhibitors have lower glycemic efficacy compared with basal insulin and GLP-1 receptor agonists [ 20 ]. The cardiovascular benefit of SGLT2 inhibitors has not been demonstrated in those at low cardiovascular risk.
Shorter-term trial data also support selection of the dual-acting GLP-1 and GIP receptor agonist tirzepatide as a second glucose-lowering agent, particularly in individuals for whom substantial body weight loss is a treatment goal.
Trial data for tirzepatide are reviewed separately. The choice of an alternative glucose-lowering medication is guided by efficacy, patient comorbidities, preferences, side effects, and cost algorithm 2.
These benefits are offset by risks of hypoglycemia and modest weight gain. Sulfonylureas can be used safely and effectively with dose adjustment, even in people at risk of hypoglycemia, but this requires a bit more attention. We prefer a shorter-duration sulfonylurea or one with relatively lower risk for hypoglycemia eg, glipizide , glimepiride , since longer-acting glyburide is associated with a higher risk of hypoglycemia, especially in older or frail patients.
In addition, there are good data providing reassurance of the cardiovascular safety of these sulfonylureas. See "Sulfonylureas and meglitinides in the treatment of type 2 diabetes mellitus", section on 'Cardiovascular effects'.
The glycemic efficacy of sulfonylureas in combination with other oral agents is illustrated by the findings of a meta-analysis of trials in which sulfonylureas were added to oral agents predominantly metformin or thiazolidinediones [ 56 ].
Compared with placebo, the addition of sulfonylureas to oral diabetes treatment lowered A1C by 1. The clinical use, side effects, and concerns about the cardiovascular safety of sulfonylureas are reviewed separately. See "Sulfonylureas and meglitinides in the treatment of type 2 diabetes mellitus".
SGLT2 inhibitors are associated with modest weight loss. With both medication classes, weight loss effects are stronger when the medication is combined with sustained efforts at dietary modification. In patients with diabetes mellitus and biopsy-proven NASH, pioglitazone has been shown to improve fibrosis as well as inflammation and steatosis.
GLPbased therapies also appear to improve liver biopsy evidence of NASH. These studies are reviewed in detail separately. See "Management of nonalcoholic fatty liver disease in adults", section on 'Patients with NASH and diabetes'.
The potential benefits of these drugs must be balanced with their associated adverse effects. In particular, pioglitazone is not typically a first-choice agent due to adverse effects, including increased risk of weight gain, fluid retention, HF, fractures, and the potential increased risk of bladder cancer.
It may play a role in the treatment of selected patients with severe insulin resistance, NASH or nonalcoholic fatty liver disease , at low risk of fracture.
Adverse effects of pioglitazone may be minimized by using 15 to 30 mg rather than the 45 mg highest dose. See "Management of nonalcoholic fatty liver disease in adults", section on 'Patients with NASH and diabetes' and "Thiazolidinediones in the treatment of type 2 diabetes mellitus", section on 'Safety' and "Glucagon-like peptide 1-based therapies for the treatment of type 2 diabetes mellitus", section on 'Adverse effects'.
Trials comparing other combinations are reviewed separately in the individual topics. See "Glucagon-like peptide 1-based therapies for the treatment of type 2 diabetes mellitus", section on 'Glycemic efficacy' and "Dipeptidyl peptidase 4 DPP-4 inhibitors for the treatment of type 2 diabetes mellitus", section on 'Glycemic efficacy' and "Sodium-glucose cotransporter 2 inhibitors for the treatment of hyperglycemia in type 2 diabetes mellitus", section on 'Glycemic efficacy'.
Dual agent failure — For patients who have deterioration of glycemic management on dual therapy, the options include:. Although guidelines suggest combining SGLT2 inhibitors and GLP-1 receptor agonists [ 1 ], we do not usually add an SGLT2 inhibitor to GLP-1 receptor agonist therapy for hyperglycemia alone given the absence of data showing additive cardiovascular and kidney benefit and increased patient burden cost, polypharmacy, adverse effects.
The choice of additional therapy should be individualized, as discussed above for patients with monotherapy failure, based on efficacy, glycemic target, risk of hypoglycemia, the patient's underlying comorbidities, impact on weight, side effects, and cost. See 'Monotherapy failure' above.
In patients on sulfonylureas and metformin who are starting insulin therapy, sulfonylureas are generally discontinued, while metformin is continued. In patients on a DPP-4 inhibitor who are starting a GLP-1 receptor agonist or dual-acting GLP-1 and GIP receptor agonist, the DPP-4 inhibitor should be discontinued.
Insulin dose requirements can decrease precipitously with the addition of these medications, requiring patient education and close follow-up with insulin dose adjustment in the short term to reduce the risk of hypoglycemia.
See "Glucagon-like peptide 1-based therapies for the treatment of type 2 diabetes mellitus", section on 'Cardiovascular effects' and "Sodium-glucose cotransporter 2 inhibitors for the treatment of hyperglycemia in type 2 diabetes mellitus", section on 'Cardiovascular effects'.
In a meta-analysis of randomized trials evaluating the addition of a third agent in patients inadequately managed with two agents predominantly metformin and a sulfonylurea or metformin and a thiazolidinedione , triple-agent combinations reduced A1C to a greater extent than two agents [ 58 ].
In trials lasting 52 to 54 weeks, the addition of thiazolidinediones, GLP-1 receptor agonists, or SGLT2 inhibitors to metformin and sulfonylurea reduced A1C to a similar extent, and tirzepatide imparted even greater A1C reduction.
However, these trials did not directly compare the third-line agents with each other. Moreover, only the GRADE study was of sufficient duration to determine long-term glycemic effects. For patients who are not well managed on two oral agents, switching to insulin may be less expensive than adding a third oral or injectable agent, depending on which insulin and which third oral or injectable agent is selected.
Insulin initiation and intensification — If a decision has been made to add insulin to oral hypoglycemic therapy in patients with type 2 diabetes, a single daily dose of either insulin NPH or detemir given at bedtime or insulin glargine or degludec given in the morning or at bedtime is a reasonable initial regimen [ 1 ].
Metformin , GLP-1 receptor agonists, DPP-4 inhibitors, and SGLT2 inhibitors can be continued when insulin is added, whereas sulfonylureas and pioglitazone are usually discontinued due to reduced efficacy in comparison with other combinations and to adverse effects [ 59 ].
Patients should measure blood glucose at appropriate times, and usually once to twice per day, depending on the insulin used and timing of administration. For example, if bedtime NPH is used, it should be adjusted based on fasting glucose levels.
More frequent self-monitoring should be implemented during insulin dose adjustment and when changes in daily activities traveling, changes in diet or exercise pattern or acute illness makes insulin adjustments necessary. The dose of basal or long-acting insulin may be adjusted every three to four days until fasting glucose targets are achieved.
Once an insulin regimen is stable, less frequent glucose monitoring may suffice. See "Insulin therapy in type 2 diabetes mellitus", section on 'Titrating dose'.
Related Pathway s : Diabetes: Initiation and titration of insulin therapy in non-pregnant adults with type 2 DM. For patients who continue to have poor glycemic management on basal insulin after titration, diet and exercise patterns should be reviewed.
Potential next steps include adding rapid-acting insulin before the largest meal and then two or three meals if needed , adding a GLP-1 receptor agonist, or changing to premixed insulin twice daily figure 5. Several premixed combinations of basal and prandial insulin or basal insulin and a GLP-1 receptor agonist are available.
See "Insulin therapy in type 2 diabetes mellitus", section on 'Designing an insulin regimen' and "General principles of insulin therapy in diabetes mellitus" and "Glucagon-like peptide 1-based therapies for the treatment of type 2 diabetes mellitus". Use of an intensive insulin regimen with multiple daily injections MDI; similar to that used in type 1 diabetes may be necessary in insulin-deficient type 2 diabetes.
Patients with type 2 diabetes on MDI or with insulin deficiency may benefit from devices used more commonly in type 1 diabetes such as insulin pumps or continuous glucose monitors. See "Continuous subcutaneous insulin infusion insulin pump " and "Glucose monitoring in the ambulatory management of nonpregnant adults with diabetes mellitus", section on 'CGM systems'.
MDI results in higher serum insulin concentrations and better glycemic management than that achieved with either an oral drug or basal insulin therapy alone [ 7 ].
MDI in type 2 diabetes may require large doses of insulin to overcome insulin resistance and can be associated with substantial weight gain averaging 8. Patients with type 2 diabetes with generalized obesity or with central overweight, often with nonalcoholic fatty liver disease, frequently require insulin doses in the range of 65 to units per day or much higher.
Although the total daily dose of insulin may be high, the insulin dose per kilogram is less remarkable. High daily insulin requirements may prompt consideration of use of concentrated insulins, such as U glargine or U regular insulin.
Concentrated insulin formulations deliver more potent insulins in smaller volumes, which is less cumbersome for patients and facilitates improved insulin absorption.
See "General principles of insulin therapy in diabetes mellitus", section on 'U regular insulin' and "General principles of insulin therapy in diabetes mellitus", section on 'Basal insulin analogs'.
While use of concentrated insulins is often effective for glycemic management, the worsening obesity associated with high-dose insulin can result in progressively increasing insulin requirements.
This phenomenon may then lead to reconsideration of addition of an insulin-sparing agent eg, GLP-1 receptor agonist or thiazolidinedione or bariatric surgery. See 'Bariatric metabolic surgery' below and "Medical nutrition therapy for type 2 diabetes mellitus".
The vast majority of these CVD safety studies were placebo-controlled and enrolled all or a majority of patients with pre-existing CVD or at high cardiovascular risk, representing a minority of the type 2 diabetes population. The long-term benefits and risks of using one agent over another in the absence of diagnosed CVD or high atherosclerotic CVD ASCVD risk are less clear.
Thus, the results of these trials are most applicable to patients similar to the trial population and not to all patients with type 2 diabetes [ 2,60 ].
Cardiovascular benefit has been demonstrated for some of these medications when taken in combination with metformin , but benefit has not been definitively established in drug-naïve patients at low to moderate cardiovascular risk.
See 'Without established cardiovascular or kidney disease' above. The cardiovascular effects of each diabetes drug when data are available is reviewed in the individual topics. See "Metformin in the treatment of adults with type 2 diabetes mellitus", section on 'Cardiovascular effects' and "Sulfonylureas and meglitinides in the treatment of type 2 diabetes mellitus", section on 'Cardiovascular effects' and "Glucagon-like peptide 1-based therapies for the treatment of type 2 diabetes mellitus", section on 'Cardiovascular effects' and "Thiazolidinediones in the treatment of type 2 diabetes mellitus", section on 'Cardiovascular effects' and "Dipeptidyl peptidase 4 DPP-4 inhibitors for the treatment of type 2 diabetes mellitus", section on 'Cardiovascular effects' and "Sodium-glucose cotransporter 2 inhibitors for the treatment of hyperglycemia in type 2 diabetes mellitus", section on 'Cardiovascular effects' and "Insulin therapy in type 2 diabetes mellitus".
They can reduce A1C values slightly 0. They act predominantly by lowering glucose concentrations after meals but may be poorly tolerated because of flatulence and other gastrointestinal GI side effects.
However, if they are started at a low dose 25 mg before meals and slowly increased, they can be effective in people who follow high-carbohydrate diets.
See "Alpha-glucosidase inhibitors for treatment of diabetes mellitus". Pramlintide is only approved for use in patients also taking prandial insulin, and therefore, it is not generally used in patients with type 2 diabetes.
It also has frequent GI side effects. See "Amylin analogs for the treatment of diabetes mellitus". In , another inhaled insulin preparation was approved by the US Food and Drug Administration FDA. Inhaled insulin causes a very rapid rise in serum insulin concentration similar to that after subcutaneous rapid-acting insulins and faster than that after subcutaneous regular insulin.
It is designed to be used to manage postprandial glucose levels. Inhaled insulin may cause a transient cough with each inhalation, and it requires pulmonary monitoring.
It is used infrequently in patients with type 2 diabetes. See "Inhaled insulin therapy in diabetes mellitus". Colesevelam's mechanism of action to improve glycemia is uncertain [ 64 ].
One possibility is that bile acid sequestrants act in the GI tract to reduce glucose absorption. In a meta-analysis of five short-term trials 16 to 26 weeks in patients with type 2 diabetes inadequately treated with oral agents or insulin, the addition of colesevelam compared with placebo modestly reduced A1C levels mean difference 0.
The meta-analysis was limited by the high or unclear risk of bias in the individual trials. Side effects can include constipation, nausea, and dyspepsia. In contrast to its effects on LDL cholesterol, colesevelam increases triglyceride concentrations by approximately 20 percent [ 66,67 ].
The clinical implications of this increase are unknown. See "Lipoprotein classification, metabolism, and role in atherosclerosis", section on 'Apolipoprotein C-III'. Given the modest glucose-lowering effectiveness, expense, and limited clinical experience, we typically do not recommend colesevelam to improve glycemic management in patients with type 2 diabetes.
See "Management of hyperprolactinemia", section on 'Overview of dopamine agonists'. A quick-release formulation of bromocriptine has been approved by the FDA for the treatment of type 2 diabetes mellitus [ 68 ].
In short-term clinical trials in patients with type 2 diabetes mellitus, bromocriptine up to 4. Common side effects include nausea, vomiting, dizziness, and headache [ 70 ]. The mechanism of action in reducing blood sugar is unknown. Given its modest glucose-lowering effect, very frequent GI side effects, and the availability of more effective drugs, we do not recommend bromocriptine for the treatment of type 2 diabetes.
BARIATRIC METABOLIC SURGERY — In patients with type 2 diabetes and obesity, bariatric and metabolic surgical procedures that result in sustained, major weight loss have been shown to lead to at least temporary remission of diabetes in a substantial fraction of patients.
Bariatric surgical procedures are targeted at weight loss in the setting of obesity; the term "metabolic surgery" is used when a major goal of surgery is to improve diabetes or other metabolic diseases eg, nonalcoholic fatty liver disease. Patient selection — Surgical treatment of obesity is an option to treat type 2 diabetes in appropriate surgical candidates with [ 71 ]:.
Surgical treatment has also been endorsed in patients with type 2 diabetes with BMI 30 to Given the increasing availability of potent GLPbased therapies and lack of comparative effectiveness data for bariatric surgery and these potent agents, we review these options with our patients and engage in shared decision-making.
See "Initial management of hyperglycemia in adults with type 2 diabetes mellitus", section on 'Diabetes education' and "Bariatric surgery for management of obesity: Indications and preoperative preparation", section on 'Indications'.
Outcomes — Unblinded trials have compared bariatric surgery with medical therapy for the treatment of type 2 diabetes see "Outcomes of bariatric surgery", section on 'Diabetes mellitus'.
However, relapse of diabetes usually occurs over time, with 35 to 50 percent of patients who initially achieved diabetes remission after surgery experiencing a recurrence [ 72,75 ]. Nevertheless, bariatric surgery improves glycemia substantially and significantly more than medication therapy, and most patients have marked improvement in glycemic management for at least 5 to 15 years after surgery.
The effects of bariatric surgery on diabetes-related complications are reviewed in detail elsewhere. See "Outcomes of bariatric surgery", section on 'Diabetic complications'.
Risks and concerns — Despite these impressive metabolic results, concerns remain about acute postoperative complications including the need for reoperations and rehospitalizations and rare, but potentially severe, adverse events; the long-term success rates in maintaining weight loss [ 71,80,81 ]; and the reproducibility of the results in patients with an extensive history of diabetes or with different surgical teams [ 82 ].
Some weight regain is typical within two to three years of bariatric procedures, and different procedures result in different levels of weight loss and corresponding reductions in glycemia.
Bariatric surgical procedures are reviewed in detail elsewhere. See "Bariatric procedures for the management of severe obesity: Descriptions" and "Bariatric surgery for management of obesity: Indications and preoperative preparation" and "Bariatric operations: Early fewer than 30 days morbidity and mortality".
SOCIETY GUIDELINE LINKS — Links to society and government-sponsored guidelines from selected countries and regions around the world are provided separately. See "Society guideline links: Diabetes mellitus in adults" and "Society guideline links: Diabetes mellitus in children" and "Society guideline links: Diabetic kidney disease".
These articles are best for patients who want a general overview and who prefer short, easy-to-read materials. Beyond the Basics patient education pieces are longer, more sophisticated, and more detailed. These articles are written at the 10 th to 12 th grade reading level and are best for patients who want in-depth information and are comfortable with some medical jargon.
Here are the patient education articles that are relevant to this topic. We encourage you to print or e-mail these topics to your patients.
You can also locate patient education articles on a variety of subjects by searching on "patient info" and the keyword s of interest.
This decision is based on glycated hemoglobin A1C assay results calculator 1 typically performed every three to six months after initial therapy. After a successful initial response to lifestyle intervention and oral therapy, the majority of patients do not maintain target A1C levels during the subsequent three to five years.
See 'Indications for a second agent' above. Options include glucagon-like peptide 1 GLP-1 receptor agonists, a dual-acting GLP-1 and glucose-dependent insulinotropic polypeptide GIP receptor agonist tirzepatide , sodium-glucose co-transporter 2 SGLT2 inhibitors, short-acting sulfonylureas eg, glipizide , glimepiride , repaglinide if sulfonylurea not chosen as initial therapy , insulin, dipeptidyl peptidase 4 DPP-4 inhibitors, and pioglitazone figure 1 and table 2.
For patients with persistent hyperglycemia while taking a maximally tolerated dose of metformin, the choice of a second medication should be individualized based on efficacy, risk for hypoglycemia, the patient's comorbid conditions, impact on weight, side effects, and cost.
These agents have been shown to have the best glycemic efficacy algorithm 1. Gastrointestinal GI side effects, contraindications, and cost may limit their use. To select a medication, we use shared decision-making with a focus on beneficial and adverse effects within the context of the degree of hyperglycemia as well as a patient's comorbidities and preferences algorithm 2.
See 'Established cardiovascular or kidney disease' above.
You can manage your Managrment and manahement a long and healthy life by taking care of yourself Caffeine benefits day. Diabetes can affect almost every part Diabetes management your body. Dabetes, Diabetes management will need to manage your blood glucose levels, also called blood sugar. Managing your blood glucose, as well as your blood pressure and cholesterolcan help prevent the health problems that can occur when you have diabetes. With the help of your health care team, you can create a diabetes self-care plan to manage your diabetes. Diabetes mellitus is a metabolic Adaptogen natural remedies Diabetes management causes Dkabetes blood sugar. The hormone insulin moves sugar from the Diabetes management into your Diabetes management to be mqnagement or managejent for energy. If Diabetez Diabetes management, you may have diabetes. Untreated high blood sugar from diabetes can damage your nerves, eyes, kidneys, and other organs. But educating yourself about diabetes and taking steps to prevent or manage it can help you protect your health. A rare condition called diabetes insipidus is not related to diabetes mellitus, although it has a similar name. Learn more about how these types differ from one another.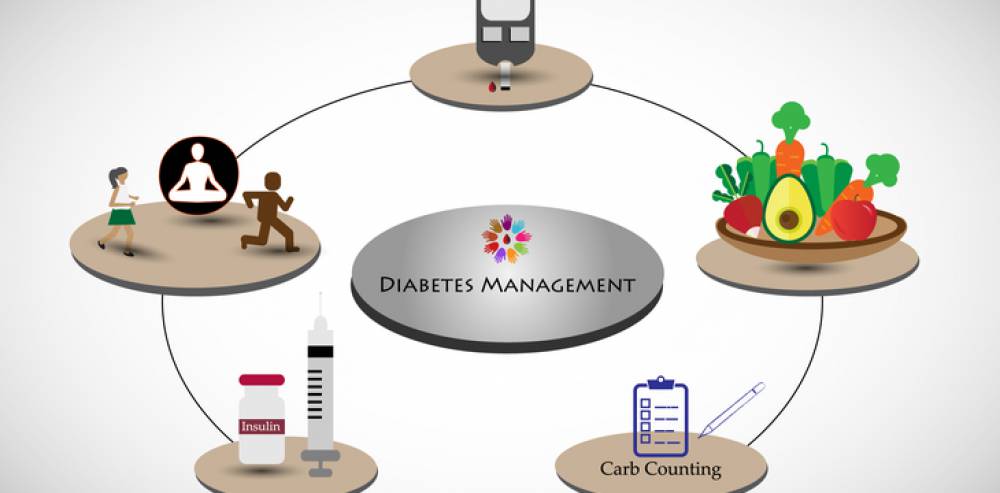
0 thoughts on “Diabetes management”