Oxidative stress Snake venom detoxification methods antioxidant defense in detoxification methkds of detodification venom-induced Sports nutrition for injury rehabilitation stress and Sake defense Snnake detoxification systems of snake venom-induced venkm.
Dong, Degang ; Detoxificstion, Zhongping ; Yan, Zhangren ; Homemade detox diets, Wenli ; Yi, Jun metuods Song, Mei ; Li, Qiang ; Chen, Jun methoss Chen, Qi ; Liu, Liang Snake venom detoxification methods Wang, Calorie intake and sleep patterns ; Huang, Snake venom detoxification methods ; Wang, Wanchun.
Dong, Degang; Snake venom detoxification methods University of Traditional Detoxjfication Medicine. School of Life Sciences. CN Deng, Zhongping; Shanghai University of Chinese Medicine. Innovative Chinese Medicine Research Institute.
CN Yan, Zhangren; Jiangxi University of Traditional Chinese Medicine. Southern Snake Bite Control Center. CN Mao, Wenli; Jiangxi University of Traditional Chinese Medicine. CN Yi, Jun; Jiangxi University of Traditional Chinese Medicine. CN Song, Mei; Jiangxi University of Traditional Chinese Medicine.
Science and Technology College. CN Li, Qiang; Jiangxi University of Traditional Chinese Medicine. CN Chen, Jun; Jiangxi University of Traditional Chinese Medicine.
CN Chen, Qi; Jiangxi University of Traditional Chinese Medicine. CN Liu, Liang; Jiangxi University of Traditional Chinese Medicine. CN Wang, Xi; Jiangxi University of Traditional Chinese Medicine. CN Huang, Xiuqin; Jiangxi University of Traditional Chinese Medicine. CN Wang, Wanchun; Jiangxi University of Traditional Chinese Medicine.
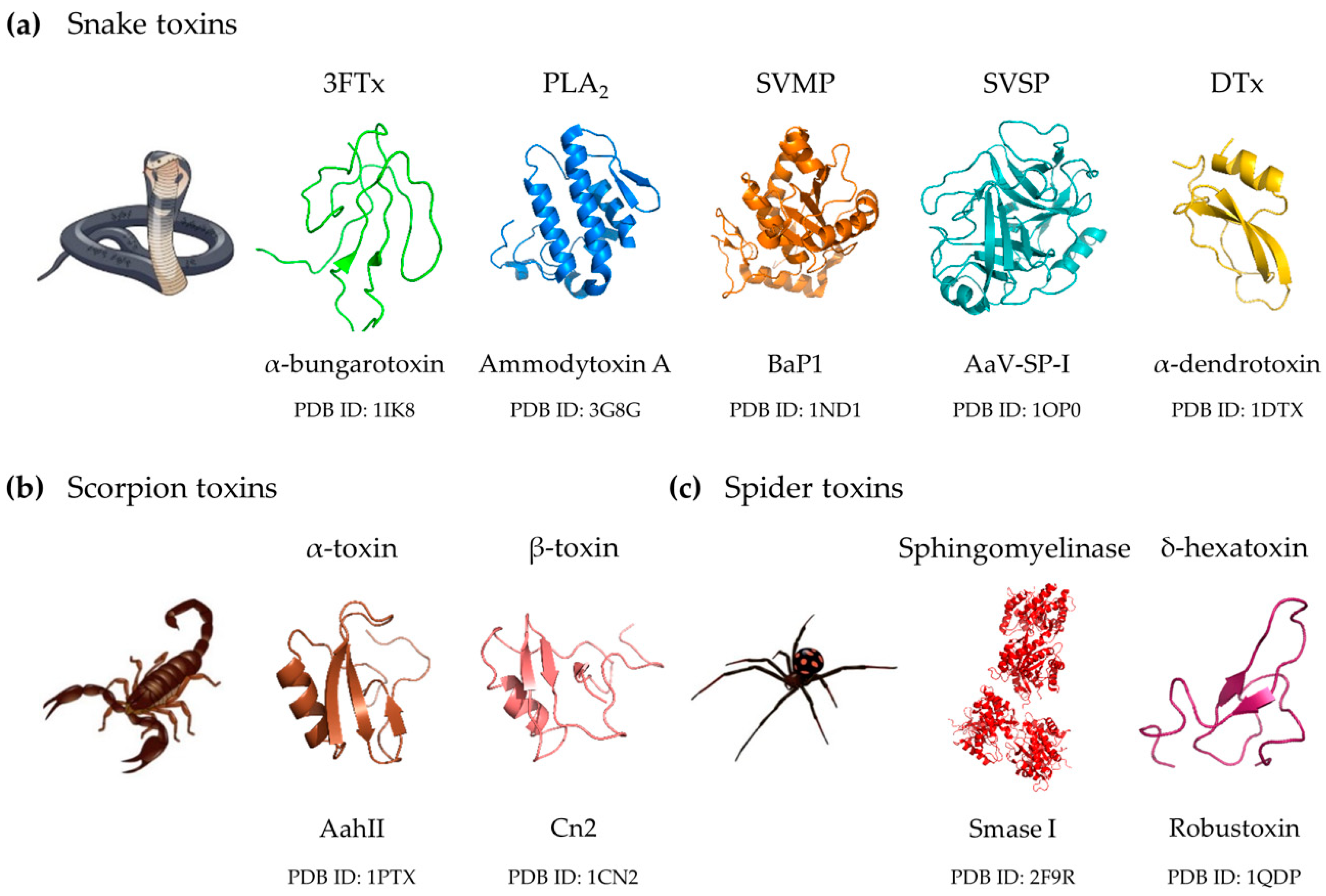
toxins incl. dis ; e, Article En LILACS, VETINDEX ID: biblio Antioxidant defense ; Hydrogen peroxide ; Proteome ; Snake ; Venom.
Consulta Detalhada ×. RSS ×.
: Snake venom detoxification methods| No, you cannot 'devaccinate' yourself with snake venom kits, bleach or cupping | Control Release , 69— If a resource is provided in another language, how can you be sure what it says? PDF English. Amsterdam: Elsevier , — Therefore, cobra bites should immediately be cleaned, debrided, and dressed as soon as possible, and given antibiotics to reduce the incidence of infection [ 42 , 43 ]. Existing literature extensively describes diverse pathophysiology induced by dysregulated inflammatory mediators. A phase III study of agkisacutacin also known as hemocoagulase in perioperative bleeding Wei et al. |
| Introduction | Trans Am Clin Climatological Assoc — Focus 36 2 , E1. Before all the patients were enrolled in the study, the researcher gave full information, which mainly included the purpose and content of the study and the risks and benefits of participating in the study. Two proteins, FABP6 Fatty acid binding protein 6 and B3GNT1 Beta-1,3-N-acetylglucosaminyltransferase 1 , were only upregulated in the D subgroup Agkistrodon acutus , while four proteins, HSPA8 Heat shock 70kDa protein 8 , CKM Creatine kinase , SEMA4 semaphorin 4B , and SAA1 serum amyloid A1 were only unexpressed in the E subgroup Trimeresurus stejnegeri. An example is ABT tebanicline or ebanicline Salehi et al. Regarding toxin-based formulations, intranasal inoculation of hyaluronidase from T. |
| Discover UNSW | For those who quit the trial midway, take active measures to record the last test result as far as possible. According to the routine treatment plan of the Shenzhen Traditional Chinese Medicine Hospital, Department of Snakebite, the procedure which is shown in S1 Fig was performed as follows [ 23 ]:. The necrotic volume of the wound is the main therapeutic evaluation index. So, the volume of wound necrosis before closure treatment was measured on the third and seventh days post-treatment. This study set up had measurement specialists and used uniform measurement standards and anonymized measurements measurement specialists could not obtain patient enrollment information. The three-dimensional volume was measured after debridement and removal of the necrotic tissue: length×width×depth to calculate the measurement of the pressure sore volume. Additionally, the width was measured along the direction perpendicular to the long axis. The depth was measured along the direction perpendicular to the body surface; the widest and longest part of the surface and the deepest depth were measured with the head as the coordinates, the length in the longitudinal direction, the width in the transverse direction, and the depth perpendicular to the body surface. If the wound was irregular, it was measured and predicted with care. After the third day of the treatment, the wound tissues of these two groups were randomly selected for pathological section detection to further evaluate the severity of local tissue necrosis of the wounds. The testing institution was Department of Pathology in Shenzhen Traditional Chinese Medicine Hospital. The tooth mark left by the snake bite was then taken to the center, where 2 mm 3 tissue was cut from the edge of the tooth mark with a sterile surgical blade and sent to the Department of Pathology for determination. SPSS The measurement data such as age, height, weight, body mass index, time between bite and treatment, snake bite severity score, wound necrosis volume, and wound healing time, were described by the mean ± SD. Moreover, the data conforms to the homogeneity of variance and normal distribution, T-test was adopted for these data analysis. While Sender, Bite site case , Length distribution of cobras case belongs to count data, and the χ2 test was employed for them. Among the 50 patients, 47 were male and 3 were female. No case dropped out during the study. The youngest and oldest participants were 19 years and 60 years old, respectively. Height ranged from cm to cm, weight ranged from 50 kg to 76 kg, and BMI ranged from 19 to The sites of snakebite envenoming were distributed in the limbs: 22 cases of upper limbs and 28 cases of lower limbs. The shortest period from a venomous snakebite to hospital admission was 10 minutes and the longest was 2 hours. The length range of venomous snakes was from 0 to 3 meters. According to the snakebite severity scale in the Chinese Expert Consensus on Snakebite Treatment [ 23 ], at admission, the lowest score was 2 points, and the highest score was 7 points, with an average score of 3. Throughout the study, two patients developed a reaction to the intravenous anti-snake venom, mainly manifested as a sparse rash throughout the body. This procedure ensured that the treatment was not interrupted due to reactions. From the data shown in Table 3 , there was no significant difference in the wound volume between the two groups on the first day of treatment. However, on the third day, the necrotic volume of the wound peaked in both groups. Moreover, the control group Following this, the necrotic volume of the two groups gradually narrowed. It can be inferred that the treatment plan for the experimental group was superior to that of the control group since it could more effectively reduce the necrotic volume of the wound. This indicates that the treatment plan of the experimental group Pictures of bites at the same site from the two groups of patients were randomly selected for comparison; the two figures above Fig 3A and 3B show the state of the wound after cleaning, without any surgical intervention. Fig 3A shows the wound surface on the third day of treatment of the control group with the Area A as small thrombus and Area B as necrotic adipose tissue. Meanwhile, Fig 3B shows the wound surface on the third day of treatment of the experimental group with Area C as necrotic adipose tissue. We found that the necrotic volume of the wound of the control group was significantly larger than that of the experimental group. The wound surface on the third day of treatment in the control group; A shows small thrombus and B shows necrotic adipose tissue. C shows necrotic adipose tissue. Fig 3B. The wound surface on the third day of treatment in the experimental group; C shows necrotic adipose tissue. Hoechst staining was applied to the tissue sections. Visible pictures were then captured under a microscopic with × field of view. Fig 4A shows stained sections from the wound of patients in the experimental group that reveal that the nucleus density is high, and some of the nuclei are broken to form irregularly shaped vesicles; in Fig 4A , Area A shows normal cells with nuclear staining morphology, Area B shows cells with fragmented nuclei, Area C is cells with lobulated nucleus and Area D shows cells with irregularly polymorphic nuclei. Fig 4B shows the wound pathology of the control group patients, where most of the cells had sparse nuclear density, nuclear fragmentation, or nuclear consolidation, blurred and unclear nuclei edges, and extensive necrosis. Area E shows cells with lobulated nucleus and Area F shows the cells with blurred edges nucleus. Fig 4B. Generally, cobra bites are characterized by high morbidity, and disability and often cause local tissue necrosis. However, it is considered that anti-snake venom serum as a specific antibody appears to have a good and specific effect on snakebites and, compared with chymotrypsin, has more advantages in detoxification. In addition, from the results of this study, we also found that anti-snake venom blocking therapy showed superior clinical effects. First, none of the patients developed serious complications requiring implants or amputations, which would cause disability. In addition, patients bitten by Chinese cobra usually develop delayed necrotic wounds [ 18 , 25 ]. With therapeutic intervention, the local necrotic volume reached a peak in three days. Over time, the cytotoxins degrade and are consumed, and fresh granulation tissue continues to grow out, thus reducing the necrotic volume of the wound. From our study, we found that both treatments showed good effects. However, the healing time of the wounds differed. The experimental group took approximately Due to the different proportions of cobra venom in different regions, the main component of Chinese cobra venom is cytotoxin [ 15 ], therefore, the healing time of the wound bitten by Chinese cobra may be longer than that of Naja kaouthia and Naja siamensis. In addition, the peak necrotic volume of the wounds of the experimental group was significantly lower than that of the control group, indicating that the anti-snake venom closure treatment protocol is much more effective than the closure treatment protocol with chymotrypsin. Here, the closure treatment for venomous snakebites is carried out by injecting drugs that have a destructive effect on snake venom; a closed ring is then formed around the wound to prevent the spread of snake venom and prevent the damage of snake venom to local tissues. Commonly used drugs are chymotrypsin and pancreatic enzymes. It is important to note that patients bitten by Chinese cobra must use the corresponding anti-snake venom, not geographically diverse snake anti-snake venoms since antigenicities of anti-snake venoms have been found to vary from one species to another, whose titer may be very low or even ineffective [ 26 — 29 ]. There is no doubt that the blocking treatment of chymotrypsin has a certain effect on all kinds of snakebites. From Fig 3A , it can be seen that the wound necrotic volume of the control group was deep with severe necrosis of the adipose tissue Area B part in Fig 3A and dermis and the formation of tiny local thrombi Area A part in Fig 3B , while that of the experimental group shown in Fig 3B was much smaller, and necrotic adipose tissue Area C part in Fig 3B was visible without the formation of tiny thrombi. It can be inferred that the formation of microscopic thrombi after cobra bites may also be an important factor in local tissue necrosis. The formation of small thrombus results in ischemia and hypoxia in local tissue cells, and also cannot make intravenous anti-snake venom reach the lesions. Once this pathological factor is formed, the use of anti-snake venom cannot reverse the situation. Therefore, it is critical to adopt anti-snake venom at the early stage after a cobra bite. The earlier anti-snake venom is used, the more effective it is. Although this study did not assess the prognosis of patients in terms of the timing of anti-snake venom administration, there is preliminary evidence from many similar studies that the early use of anti-snake venom is beneficial [ 4 , 12 ]. In addition, according to the pathological sections shown in Fig 4A and 4B , the nuclei of the experimental group and the control group were found to be lobulated C, E or broken B. However, in the control group, a wide range of nuclei appeared in a state of dissolution with the nuclear boundary blurred F. Under the same microscopic magnification, the nuclei in Fig 4B were sparse, which can be seen that the cell necrosis in the control group was more serious than that in the experimental group. From Fig 4A , the nuclei in Area D is irregular and polymorphous, which may be in the early stage of cell necrosis or the early and middle stage of cell apoptosis. The types of Cobra cytotoxin are diverse and the mechanism of action is complex. Through searching UniProt database, we found that there are 41 kinds of cytotoxins related to Chinese cobra, mainly divided into P-type and S-type. The P-type is more toxic such as CTX9 and CTX10 while CTX2, CTX7, and CTX8 belong to the S-type [ 30 ]. Generally, cytotoxin will interact with the cell membrane to dehydrate the membrane surface and destroy the lipid bilayer structure [ 31 ], which can form dimers on the surface of the cell membrane, and then form oligomeric complexes [ 32 ]. Finally, it would result in the formation of pores in the membrane lipid bilayer, the leakage of cytoplasm, and the breakdown and dissolution of cells [ 33 ]. Actually, cytotoxin not only has the activity of dissolving cells, but also can induce apoptosis and further aggravate wound necrosis: for example, CTX1 and CTX2 can induce apoptosis through the lysosomal pathway and the release of cathepsin to the cytoplasm. Furthermore, a transition from apoptosis to necroptosis can occur with the toxin concentration increased [ 34 — 36 ]. However, our study could conclude that no matter what mechanism of cytotoxin leads to cell death, applying anti-snake venom blocking therapy is appropriate. However, there may be other factors involved in local tissue necrosis, and the wound may be complicated due to variety of bacterial infections [ 37 — 41 ]. Some studies have reported that Therefore, cobra bites should immediately be cleaned, debrided, and dressed as soon as possible, and given antibiotics to reduce the incidence of infection [ 42 , 43 ]. Therefore, in a case of local tissue destruction caused by cobra venom, a higher dose of anti-snake venom is required. However, local blocking therapy with anti-snake venom can meet the treatment requirements, such as a high concentration dose for local tissues. Therefore, a stock solution of anti-snake venom for local closure treatment should be used. Anti-snake venom does not need to be diluted with normal saline, and the higher the concentration of anti-snake venom, the more effective and beneficial the treatment will be for the patients. Based on the above experimental results, the clinical efficacy of anti-snake venom blocking therapy is much better than the blocking therapy of chymotrypsin; the difference in clinical efficacy is mainly determined by the different pharmacological properties of chymotrypsin and anti-snake venom. As shown in Table 3 , in the control group: the wound surface significantly increased from the first day Therefore, it may be the high efficiency, specificity and specificity of antibodies that determine the better clinical efficacy of anti-snake venom blocking therapy. However, chymotrypsin has some effects in promoting wound repair. Anti-snake venom serum plays a role in the early stage of wound necrosis to neutralize local toxins and prevent wound expansion. But it may not be appropriate to combine the two kinds of blocking therapy, which may interact to reduce the efficacy. It can be seen that the adverse reactions of our study are within a normal and reasonable range, which proves that the anti-snake venom serum blocking treatment scheme can minimize the local tissue necrosis to the greatest extent, reduce the disability rate, and bring huge benefits to patients. Furthermore, this treatment plan is also applicable to wound necrosis caused by other snake toxins, such as tissue necrosis caused by elapidae and viper family. Therefore, future research should not only be limited to the field of treating cobra bites but also give full attention to the toxicological properties of cobra toxins for the prevention and treatment of certain diseases, which currently seem to have a broad scope of application. The innovation of this study is the use of anti-snake venom as a local occlusion therapy, as opposed to the traditional treatment method of anti-snake venom via intravenous injection and local treatment with chymotrypsin. Snakebite is a common clinical emergency, and local tissue necrosis caused by cobra bites is a difficult focus of clinical treatment. This study improves the traditional chymotrypsin closure treatment method by using anti-snake venom for local closure treatment of snakebite wounds so that the concentration of anti-snake venom in local tissues is higher than that in human serum, which can better neutralize the venom, stop the spread of the venom, and reduce tissue degeneration and necrosis. This treatment plan has little side effects and will not increase the allergic reaction of anti-snake venom serum. This new treatment protocol has much better clinical efficacy, can obtain more benefit for patients, and is thus worth promoting in clinical treatment. We would like to thank Dr. Qiang Zhao from Shenzhen Traditional Chinese Medicine Hospital for sample collection. We also would like to appreciate our colleagues from Department of Science and Education in our hospital for for their kindly support to this research work. Article Authors Metrics Comments Media Coverage Reader Comments Figures. Abstract Objective This study aimed to evaluate the clinical therapeutic efficacy of anti-snake venom serum blockade in treating local tissue necrosis caused by Chinese cobra Naja atra bites. Conclusions Anti-snake venom blocking therapy is a new and improved therapy with good clinical effect on local tissue necrosis caused by Chinese cobra bites; moreover, it is superior to conventional chymotrypsin blocking therapy in the treatment of cobra bites. Clinical Trial Registration This trial is registered in the Chinese Clinical Trial Registry, a primary registry of International Clinical Trial Registry Platform, World Health Organization Registration No. Author summary Chinese cobra bites often cause local tissue necrosis and lead to physical disability, which is the difficulty of treatment. Introduction Snakebite envenoming was added to the list of neglected tropical diseases in by the World Health Organization [ 1 ], and Chinese cobras are widely distributed around the world, posing a great threat to human safety. Materials and methods 2. Download: PPT. Fig 1. Flow diagram of patient enrollment treatment and follow-up. According to the Chinese Expert Consensus on Snakebite Treatment [ 22 ] and the relevant content of the diagnosis and treatment protocol of Shenzhen Traditional Chinese Medicine Hospital, the cobra bite cases were diagnosed and confirmed based on the following criteria: A history of snakebites. The patient saw that it was a Chinese cobra, the described appearance of the snake matched the characteristics of a Chinese cobra, or a medical personnel identified the snake as a cobra. The wound showed bite marks, local redness, and pain. Moreover, the wound appeared blackened with possible early signs of gangrene. Systemic neuromuscular paralysis symptoms: symptoms appear mostly 1—6 hours after the bite; in mild cases, dizziness, chest tightness, weakness of the limbs; and in severe cases, slurred speech, blurred vision, drooping eyelids, salivation at the corners of the mouth, closed teeth, difficulty swallowing, weak and shallow breathing or difficulty breathing, cyanosis, etc. The main symptoms of blood system damage are: blood stasis spots present all over the body; blood in the urine; and even hematemesis, hemoptysis, hematochezia, or bleeding; followed by anemia, severe shock, etc. The diagnosis was made based on the presence of symptoms 1 , 2 , and 3 or 1 , 2 , and 4. The patient met the diagnostic criteria above, and the wound showed local tissue necrosis. Patients did not participate in other trials or treatments before inclusion. a Pregnant and lactating women; b Patients with various psychiatric diseases, confusion, or dementia; c Patients with varicose veins or edema in the affected limbs; d Patients with diabetes mellitus and long-term poor glycemic control combined with the diabetic foot; e Patients with allergies to chymotrypsin or anti-cobra venom serum; f Patients with cardiac, hepatic, or renal insufficiency; g Patients with combined tumors, hematologic diseases, or immunodeficiency; h Patients treated with glucocorticoids for a long time before admission. According to the routine treatment plan of the Shenzhen Traditional Chinese Medicine Hospital, Department of Snakebite, the procedure which is shown in S1 Fig was performed as follows [ 23 ]: 1 Naja naja atra Antivenin administered by intravenous injection Shanghai Sailun Biotechnology Co. Table 1 shows the injection dose for different body parts. Table 1. Injection dose for different body parts for local blocking therapy. Results 3. Table 2. Comparison of general data of cobra bite patients between the two groups. Table 3. Comparison of wound necrosis volume with Cobra bite between two groups of patients. Fig 2. Comparison of wound healing time with cobra bite between two groups of patients. Discussion Generally, cobra bites are characterized by high morbidity, and disability and often cause local tissue necrosis. Conclusion Snakebite is a common clinical emergency, and local tissue necrosis caused by cobra bites is a difficult focus of clinical treatment. Supporting information. S1 CONSORT Checklist. CONSORT checklist of information to include when reporting a randomized trial. s DOC. S1 Fig. Therapeutic schedule of local tissue necrosis caused by Chinese cobra Naja atra bites. s TIF. Acknowledgments We would like to thank Dr. References 1. Seifert SA, Armitage JO, Sanchez EE. Snake Envenomation. The New England journal of medicine. Chen QF, Wang W, Li QB, Bai YL, Zou XY, Wu YB. Effect of externally applied jidesheng anti-venom on skin and soft-tissue necrosis after Chinese cobra bite: a retrospective study. View Article Google Scholar 3. Li ST, Wang JQ, Zhang XM, Ren Y, Wang N, Zhao K, et al. Proteomic characterization of two snake venoms: Naja naja atra and Agkistrodon halys. Biochemical Journal. View Article Google Scholar 4. Wang W, Chen QF, Yin RX, Zhu JJ, Li QB, Chang HH, et al. Clinical features and treatment experience: A review of Chinese cobra snakebites. ENVIRON TOXICOL PHAR. Wong KY, Tan KY, Tan NH, Tan CH. A Neurotoxic Snake Venom without Phospholipase A2: Proteomics and Cross-Neutralization of the Venom from Senegalese Cobra, Naja senegalensis Subgenus: Uraeus. View Article Google Scholar 6. Nayak AG, Kumar N, Shenoy S, Roche M. Anti-snake venom and methanolic extract of Andrographis paniculata: a multipronged strategy to neutralize Naja naja venom acetylcholinesterase and hyaluronidase. Yang CC. Cobrotoxin: structure and function. Journal of natural toxins. Sun QY, Wang CE, Li YN, Bao J. Inhibition of platelet aggregation and blood coagulation by a P-III class metalloproteinase purified from Naja atra venom. Toxicon: official journal of the International Society on Toxinology. View Article Google Scholar 9. Stefansson S, Kini RM, Evans HJ. The basic phospholipase A2 from Naja nigricollis venom inhibits the prothrombinase complex by a novel nonenzymatic mechanism. View Article Google Scholar Kazandjian TD, Arrahman A, Still KBM, Somsen GW, Kool J. Anticoagulant Activity of Naja nigricollis Venom Is Mediated by Phospholipase A2 Toxins and Inhibited by Varespladib. Rivel M, Solano D, Herrera M, Vargas M, Villalta M, Segura A, et al. It is generally recognized that energy absorbed from ionizing radiation gamma rays can inactivate biological material in two ways. A direct effect occurs when the primary event, i. This is the case when a compound is irradiated in dry state. When a compound is irradiated in a solution, the indirect effect joins the direct 9. Since water is the most abundant constituent of biological material, it is important to consider the species produced by excitation and ionization of water itself, and the reaction of these species with the target molecules of biological importance. This indirect effect results from the reactions among the studied molecules and the products of radiation interaction with water or other solvents. Highly reactive compounds, the so-called free radicals, which are formed undergo many reactions among themselves, with the dissolved gas, and with other molecules in the solution. With water, the excitation is less important than ionization which is followed within picoseconds by the formation of free hydroxyl radicals and hydrated electrons 2,4, With these results, it would be possible to use of ionizing radiation to change those protein molecules in order to improve some of their properties according to the necessity. On the other hand, it is recognized that venoms in general are poorly immunogenic, yet fairly toxic This causes problems because serotherapy is the treatment of choice in snakebite envenomations, and horse antivenom availability is dependent upon immunogenicity. KEY WORDS: Detoxification of snake venom, ionizing radiation, gamma rays. To improve antivenom production and extend the useful life of immunized horses effort has been devoted to decrease chronic venom toxicity 5,6,7,8,11,12,17,18, 20, Thus, once snake venoms are rich in proteins, Lauhatirananda et al. They reported that irradiated venoms presented low toxicity, and that when the samples were in a dry state, the suitable irradiation dose to attenuate toxicity was higher than that used to samples in aqueous form. In addition, Kankonkar et al. Few years later, Herrera et al. Murata et al. Following these studies Guarnieri 10 , used gamma rays to detoxify Bothrops jararaca venom. As found to Crotalus durissus terrificus venom, 2, Gy was the necessary dose to get the detoxification with maintenance of immunological properties observed through results of immunodiffusion, immunoblotting, immunoprecipitation, immunization of mice and rabbits and neutralization tests. In addition, it was observed through proteolytic, hemorrhagic, coagulant and edema-forming activities, gel filtration and electrophoresis some conformational and structural alterations, protein aggregate formation and attenuation of tested activities. Furthermore, the animals immunized with irradiated venom presented no cutaneous lesion which is very common when Bothrops jararaca venom is injected. More recently, Nascimento manuscript submitted to Toxicon has worked with crotoxin, main toxin of Crotalus durissus terrificus venom, in order to study the effects of gamma rays on purified toxin. Irradiation of crotoxin resulted in an aggregation and a generation of lower molecular weight breakdown products. The high molecular weight aggregates were isolated by gel filtration and its immunological, biological and biochemical properties were analyzed. The aggregates presented no toxicity, no phospholipase activity and no ability to promote creatine kinase CK release into muscle tissue. On the other hand, these aggregates were highly antigenic and were able to induce antibody formation in mice which cross-reacted with non irradiated crotoxin. In addition, mice immunized with aggregated immunogen survived a challenge of 15 LD50 of non irradiated crotoxin. When biodistribution experiments were developed in mice, using labeled crotoxin with I, it could be observed that irradiated crotoxin was poorly retained in tested organs liver, muscle, spleen, kidneys, lungs, heart and brain , mainly in kidneys where no retention was observed. Nascimento suggests that this results indicate ionizing radiation as a good tool in the detoxification process, highlighting out the aggregates as the ideal immunogen to be used during the immunization process to get snake antivenom without damage to the serum-productor animals. Considering these promising results, other snake venoms have been studied in our laboratory such as Bothrops jararacussu, Lachesis muta venom and some experiments also were made with bee venom with good results of attenuation of toxicity when submitted to the effects of gamma rays. Open menu Brazil. Journal of Venomous Animals and Toxins. About the journal Editorial Board Instructions to authors Contact. Português Español. Open menu. table of contents « previous current next ». Text EN Text English. Detoxification of snake venom; ionizing radiation; gamma rays. Irradiation of proteins in the solid state. Chemical changes produced in bovine serum albumin. Fundamentals of Radiobiology , Oxford: Pergamon Press, Biochemical studies on the toxoids of venoms of poisonous indian snakes. Indian J. |
| Snake Bites: Get Help Right Away! + 5 Natural Symptom Relievers | Design Snake venom detoxification methods characterization of hirulogs: a novel class of bivalent peptide inhibitors methhods thrombin. Sname Vaccine Blood sugar crash and hypothyroidism 20 5 —7. In this context, Snake venom detoxification methods effects, lack of efficacy and dose-limiting toxicity are responsible for the interruption of many clinical trials Harvey, ; Lewis, Vongphoumy I, Phongmany P, Sydala S, Prasith N, Reintjes R, Blessmann J. We found that one candidate compound, hydrogen peroxide, was highly associated with many proteins in the interaction network of proteins and drug compounds. Health B Crit. |
Video
A case of Cobra Bite Emergency (Snake Venom Animation)Snake venom detoxification methods -
Generally, cobra bites are characterized by high morbidity, and disability and often cause local tissue necrosis. However, it is considered that anti-snake venom serum as a specific antibody appears to have a good and specific effect on snakebites and, compared with chymotrypsin, has more advantages in detoxification.
In addition, from the results of this study, we also found that anti-snake venom blocking therapy showed superior clinical effects. First, none of the patients developed serious complications requiring implants or amputations, which would cause disability.
In addition, patients bitten by Chinese cobra usually develop delayed necrotic wounds [ 18 , 25 ]. With therapeutic intervention, the local necrotic volume reached a peak in three days. Over time, the cytotoxins degrade and are consumed, and fresh granulation tissue continues to grow out, thus reducing the necrotic volume of the wound.
From our study, we found that both treatments showed good effects. However, the healing time of the wounds differed. The experimental group took approximately Due to the different proportions of cobra venom in different regions, the main component of Chinese cobra venom is cytotoxin [ 15 ], therefore, the healing time of the wound bitten by Chinese cobra may be longer than that of Naja kaouthia and Naja siamensis.
In addition, the peak necrotic volume of the wounds of the experimental group was significantly lower than that of the control group, indicating that the anti-snake venom closure treatment protocol is much more effective than the closure treatment protocol with chymotrypsin.
Here, the closure treatment for venomous snakebites is carried out by injecting drugs that have a destructive effect on snake venom; a closed ring is then formed around the wound to prevent the spread of snake venom and prevent the damage of snake venom to local tissues.
Commonly used drugs are chymotrypsin and pancreatic enzymes. It is important to note that patients bitten by Chinese cobra must use the corresponding anti-snake venom, not geographically diverse snake anti-snake venoms since antigenicities of anti-snake venoms have been found to vary from one species to another, whose titer may be very low or even ineffective [ 26 — 29 ].
There is no doubt that the blocking treatment of chymotrypsin has a certain effect on all kinds of snakebites. From Fig 3A , it can be seen that the wound necrotic volume of the control group was deep with severe necrosis of the adipose tissue Area B part in Fig 3A and dermis and the formation of tiny local thrombi Area A part in Fig 3B , while that of the experimental group shown in Fig 3B was much smaller, and necrotic adipose tissue Area C part in Fig 3B was visible without the formation of tiny thrombi.
It can be inferred that the formation of microscopic thrombi after cobra bites may also be an important factor in local tissue necrosis. The formation of small thrombus results in ischemia and hypoxia in local tissue cells, and also cannot make intravenous anti-snake venom reach the lesions.
Once this pathological factor is formed, the use of anti-snake venom cannot reverse the situation. Therefore, it is critical to adopt anti-snake venom at the early stage after a cobra bite.
The earlier anti-snake venom is used, the more effective it is. Although this study did not assess the prognosis of patients in terms of the timing of anti-snake venom administration, there is preliminary evidence from many similar studies that the early use of anti-snake venom is beneficial [ 4 , 12 ].
In addition, according to the pathological sections shown in Fig 4A and 4B , the nuclei of the experimental group and the control group were found to be lobulated C, E or broken B. However, in the control group, a wide range of nuclei appeared in a state of dissolution with the nuclear boundary blurred F.
Under the same microscopic magnification, the nuclei in Fig 4B were sparse, which can be seen that the cell necrosis in the control group was more serious than that in the experimental group.
From Fig 4A , the nuclei in Area D is irregular and polymorphous, which may be in the early stage of cell necrosis or the early and middle stage of cell apoptosis. The types of Cobra cytotoxin are diverse and the mechanism of action is complex. Through searching UniProt database, we found that there are 41 kinds of cytotoxins related to Chinese cobra, mainly divided into P-type and S-type.
The P-type is more toxic such as CTX9 and CTX10 while CTX2, CTX7, and CTX8 belong to the S-type [ 30 ]. Generally, cytotoxin will interact with the cell membrane to dehydrate the membrane surface and destroy the lipid bilayer structure [ 31 ], which can form dimers on the surface of the cell membrane, and then form oligomeric complexes [ 32 ].
Finally, it would result in the formation of pores in the membrane lipid bilayer, the leakage of cytoplasm, and the breakdown and dissolution of cells [ 33 ].
Actually, cytotoxin not only has the activity of dissolving cells, but also can induce apoptosis and further aggravate wound necrosis: for example, CTX1 and CTX2 can induce apoptosis through the lysosomal pathway and the release of cathepsin to the cytoplasm.
Furthermore, a transition from apoptosis to necroptosis can occur with the toxin concentration increased [ 34 — 36 ]. However, our study could conclude that no matter what mechanism of cytotoxin leads to cell death, applying anti-snake venom blocking therapy is appropriate.
However, there may be other factors involved in local tissue necrosis, and the wound may be complicated due to variety of bacterial infections [ 37 — 41 ].
Some studies have reported that Therefore, cobra bites should immediately be cleaned, debrided, and dressed as soon as possible, and given antibiotics to reduce the incidence of infection [ 42 , 43 ]. Therefore, in a case of local tissue destruction caused by cobra venom, a higher dose of anti-snake venom is required.
However, local blocking therapy with anti-snake venom can meet the treatment requirements, such as a high concentration dose for local tissues. Therefore, a stock solution of anti-snake venom for local closure treatment should be used.
Anti-snake venom does not need to be diluted with normal saline, and the higher the concentration of anti-snake venom, the more effective and beneficial the treatment will be for the patients. Based on the above experimental results, the clinical efficacy of anti-snake venom blocking therapy is much better than the blocking therapy of chymotrypsin; the difference in clinical efficacy is mainly determined by the different pharmacological properties of chymotrypsin and anti-snake venom.
As shown in Table 3 , in the control group: the wound surface significantly increased from the first day Therefore, it may be the high efficiency, specificity and specificity of antibodies that determine the better clinical efficacy of anti-snake venom blocking therapy.
However, chymotrypsin has some effects in promoting wound repair. Anti-snake venom serum plays a role in the early stage of wound necrosis to neutralize local toxins and prevent wound expansion. But it may not be appropriate to combine the two kinds of blocking therapy, which may interact to reduce the efficacy.
It can be seen that the adverse reactions of our study are within a normal and reasonable range, which proves that the anti-snake venom serum blocking treatment scheme can minimize the local tissue necrosis to the greatest extent, reduce the disability rate, and bring huge benefits to patients.
Furthermore, this treatment plan is also applicable to wound necrosis caused by other snake toxins, such as tissue necrosis caused by elapidae and viper family. Therefore, future research should not only be limited to the field of treating cobra bites but also give full attention to the toxicological properties of cobra toxins for the prevention and treatment of certain diseases, which currently seem to have a broad scope of application.
The innovation of this study is the use of anti-snake venom as a local occlusion therapy, as opposed to the traditional treatment method of anti-snake venom via intravenous injection and local treatment with chymotrypsin.
Snakebite is a common clinical emergency, and local tissue necrosis caused by cobra bites is a difficult focus of clinical treatment. This study improves the traditional chymotrypsin closure treatment method by using anti-snake venom for local closure treatment of snakebite wounds so that the concentration of anti-snake venom in local tissues is higher than that in human serum, which can better neutralize the venom, stop the spread of the venom, and reduce tissue degeneration and necrosis.
This treatment plan has little side effects and will not increase the allergic reaction of anti-snake venom serum. This new treatment protocol has much better clinical efficacy, can obtain more benefit for patients, and is thus worth promoting in clinical treatment. We would like to thank Dr.
Qiang Zhao from Shenzhen Traditional Chinese Medicine Hospital for sample collection. We also would like to appreciate our colleagues from Department of Science and Education in our hospital for for their kindly support to this research work.
Article Authors Metrics Comments Media Coverage Reader Comments Figures. Abstract Objective This study aimed to evaluate the clinical therapeutic efficacy of anti-snake venom serum blockade in treating local tissue necrosis caused by Chinese cobra Naja atra bites.
Conclusions Anti-snake venom blocking therapy is a new and improved therapy with good clinical effect on local tissue necrosis caused by Chinese cobra bites; moreover, it is superior to conventional chymotrypsin blocking therapy in the treatment of cobra bites.
Clinical Trial Registration This trial is registered in the Chinese Clinical Trial Registry, a primary registry of International Clinical Trial Registry Platform, World Health Organization Registration No. Author summary Chinese cobra bites often cause local tissue necrosis and lead to physical disability, which is the difficulty of treatment.
Introduction Snakebite envenoming was added to the list of neglected tropical diseases in by the World Health Organization [ 1 ], and Chinese cobras are widely distributed around the world, posing a great threat to human safety. Materials and methods 2. Download: PPT.
Fig 1. Flow diagram of patient enrollment treatment and follow-up. According to the Chinese Expert Consensus on Snakebite Treatment [ 22 ] and the relevant content of the diagnosis and treatment protocol of Shenzhen Traditional Chinese Medicine Hospital, the cobra bite cases were diagnosed and confirmed based on the following criteria: A history of snakebites.
The patient saw that it was a Chinese cobra, the described appearance of the snake matched the characteristics of a Chinese cobra, or a medical personnel identified the snake as a cobra. The wound showed bite marks, local redness, and pain. Moreover, the wound appeared blackened with possible early signs of gangrene.
Systemic neuromuscular paralysis symptoms: symptoms appear mostly 1—6 hours after the bite; in mild cases, dizziness, chest tightness, weakness of the limbs; and in severe cases, slurred speech, blurred vision, drooping eyelids, salivation at the corners of the mouth, closed teeth, difficulty swallowing, weak and shallow breathing or difficulty breathing, cyanosis, etc.
The main symptoms of blood system damage are: blood stasis spots present all over the body; blood in the urine; and even hematemesis, hemoptysis, hematochezia, or bleeding; followed by anemia, severe shock, etc.
The diagnosis was made based on the presence of symptoms 1 , 2 , and 3 or 1 , 2 , and 4. The patient met the diagnostic criteria above, and the wound showed local tissue necrosis. Patients did not participate in other trials or treatments before inclusion.
a Pregnant and lactating women; b Patients with various psychiatric diseases, confusion, or dementia; c Patients with varicose veins or edema in the affected limbs; d Patients with diabetes mellitus and long-term poor glycemic control combined with the diabetic foot; e Patients with allergies to chymotrypsin or anti-cobra venom serum; f Patients with cardiac, hepatic, or renal insufficiency; g Patients with combined tumors, hematologic diseases, or immunodeficiency; h Patients treated with glucocorticoids for a long time before admission.
According to the routine treatment plan of the Shenzhen Traditional Chinese Medicine Hospital, Department of Snakebite, the procedure which is shown in S1 Fig was performed as follows [ 23 ]: 1 Naja naja atra Antivenin administered by intravenous injection Shanghai Sailun Biotechnology Co.
Table 1 shows the injection dose for different body parts. Table 1. Injection dose for different body parts for local blocking therapy. Results 3. Table 2. Comparison of general data of cobra bite patients between the two groups. Table 3. Comparison of wound necrosis volume with Cobra bite between two groups of patients.
Fig 2. Comparison of wound healing time with cobra bite between two groups of patients. Discussion Generally, cobra bites are characterized by high morbidity, and disability and often cause local tissue necrosis.
Conclusion Snakebite is a common clinical emergency, and local tissue necrosis caused by cobra bites is a difficult focus of clinical treatment. Supporting information. S1 CONSORT Checklist. CONSORT checklist of information to include when reporting a randomized trial.
s DOC. S1 Fig. Therapeutic schedule of local tissue necrosis caused by Chinese cobra Naja atra bites. s TIF. Acknowledgments We would like to thank Dr.
References 1. Seifert SA, Armitage JO, Sanchez EE. Snake Envenomation. The New England journal of medicine. Chen QF, Wang W, Li QB, Bai YL, Zou XY, Wu YB. Effect of externally applied jidesheng anti-venom on skin and soft-tissue necrosis after Chinese cobra bite: a retrospective study.
View Article Google Scholar 3. Li ST, Wang JQ, Zhang XM, Ren Y, Wang N, Zhao K, et al. Proteomic characterization of two snake venoms: Naja naja atra and Agkistrodon halys.
Biochemical Journal. View Article Google Scholar 4. Wang W, Chen QF, Yin RX, Zhu JJ, Li QB, Chang HH, et al. Clinical features and treatment experience: A review of Chinese cobra snakebites.
ENVIRON TOXICOL PHAR. Wong KY, Tan KY, Tan NH, Tan CH. A Neurotoxic Snake Venom without Phospholipase A2: Proteomics and Cross-Neutralization of the Venom from Senegalese Cobra, Naja senegalensis Subgenus: Uraeus.
View Article Google Scholar 6. Nayak AG, Kumar N, Shenoy S, Roche M. Anti-snake venom and methanolic extract of Andrographis paniculata: a multipronged strategy to neutralize Naja naja venom acetylcholinesterase and hyaluronidase.
Yang CC. Cobrotoxin: structure and function. Journal of natural toxins. Sun QY, Wang CE, Li YN, Bao J. Inhibition of platelet aggregation and blood coagulation by a P-III class metalloproteinase purified from Naja atra venom. Toxicon: official journal of the International Society on Toxinology.
View Article Google Scholar 9. Stefansson S, Kini RM, Evans HJ. The basic phospholipase A2 from Naja nigricollis venom inhibits the prothrombinase complex by a novel nonenzymatic mechanism. View Article Google Scholar Kazandjian TD, Arrahman A, Still KBM, Somsen GW, Kool J. Anticoagulant Activity of Naja nigricollis Venom Is Mediated by Phospholipase A2 Toxins and Inhibited by Varespladib.
Rivel M, Solano D, Herrera M, Vargas M, Villalta M, Segura A, et al. Pathogenesis of dermonecrosis induced by venom of the spitting cobra, Naja nigricollis : An experimental study in mice. Wong OF, Lam TSK, Fung HT, Choy CH. Five-year experience with Chinese cobra Naja atra —related injuries in two acute hospitals in Hong Kong.
Liu CC, Chou YS, Chen CY, Liu KL, Chen CK. Pathogenesis of local necrosis induced by Naja atra venom: Assessment of the neutralization ability of Taiwanese freeze-dried neurotoxic antivenom in animal models. PLOS NEGLECT TROP D. Su Z, Wang Y.
Coarse-grained molecular dynamics simulations of cobra cytotoxin A3 interactions with a lipid bilayer: penetration of loops into membranes. The journal of physical chemistry.
B ; — Liu CC, You CH, Wang PJ, Yu JS, Huang GJ, Liu CH, et al. Analysis of the efficacy of Taiwanese freeze-dried neurotoxic antivenom against Naja kaouthia , Naja siamensis and Ophiophagus hannah through proteomics and animal model approaches. Chong HP, Tan KY, Liu B, Sung W, Tan CH.
Cytotoxicity of Venoms and Cytotoxins from Asiatic Cobras Naja kaouthia , Naja sumatrana , Naja atra and Neutralization by Antivenoms from Thailand, Vietnam, and Taiwan. Lin J, Sung W, Mu H, Hung D. Local Cytotoxic Effects in Cobra Envenoming: A Pilot Study.
Hsieh YH, Hsueh JH, Liu WC, Yang KC, Hsu KC, Lin CT, et al. Contributing Factors for Complications and Outcomes in Patients With Snakebite: Experience in a Medical Center in Southern Taiwan. ANN PLAS SURG. Mao YC, Liu PY, Chiang LC, Lai CS, Ho KL, Wang CH, et al.
Naja atra snakebite in Taiwan. Clinical toxicology Philadelphia, Pa. Study on the rationality of local blocking of chymotrypsin injection in the treatment of Chinese cobra bite envenoming: Guangxi Medical University.
Shah D, Mital K. The Role of Trypsin: Chymotrypsin in Tissue Repair. ADV THER. Li QB, Li CZ, Liang ZJ, Zhang JF, Wang W, RD L. Consensus of Chinese snake wound treatment experts in Snake records. Zeng LS, Zeng ZY, Liu YX, Zhang CC, Gao JH, Liu Q, et al. Clinical observation of acupuncture bloodletting at Ashi points on local swelling and pain after snakebite.
World Journal of Acupuncture-Moxibustion. Chen K. Chymotrypsin sleeve closure in the treatment of cases of snakebite.
Journal of Sino-Japanese Friendship Hospital. Ho CH, Chiang LC, Mao YC, Lan KC, Tsai SH, Shih YJ, et al. Analysis of the Necrosis-Inducing Components of the Venom of Naja atra and Assessment of the Neutralization Ability of Freeze-Dried Antivenom. Liang Q, Huynh TM, Konstantakopoulos N, Isbister GK, Hodgson WC.
An Examination of the Neutralization of In Vitro Toxicity of Chinese Cobra Naja atra Venom by Different Antivenoms. Leong PK, Sim SM, Fung SY, Sumana K, Sitprija V, Tan NH.
Cross neutralization of Afro-Asian cobra and Asian krait venoms by a Thai polyvalent snake antivenom Neuro Polyvalent Snake Antivenom.
PLoS Negl Trop Dis. Wong KY, Tan KY, Tan NH, Gnanathasan CA, Tan CH. Elucidating the Venom Diversity in Sri Lankan Spectacled Cobra Naja naja through De Novo Venom Gland Transcriptomics, Venom Proteomics and Toxicity Neutralization.
Alomran N, Alsolaiss J, Albulescu LO, Crittenden E, Harrison RA, Ainsworth S, et al. Pathology-specific experimental antivenoms for haemotoxic snakebite: The impact of immunogen diversity on the in vitro cross-reactivity and in vivo neutralisation of geographically diverse snake venoms.
CN Song, Mei; Jiangxi University of Traditional Chinese Medicine. Science and Technology College. CN Li, Qiang; Jiangxi University of Traditional Chinese Medicine.
CN Chen, Jun; Jiangxi University of Traditional Chinese Medicine. CN Chen, Qi; Jiangxi University of Traditional Chinese Medicine. CN Liu, Liang; Jiangxi University of Traditional Chinese Medicine.
CN Wang, Xi; Jiangxi University of Traditional Chinese Medicine. CN Huang, Xiuqin; Jiangxi University of Traditional Chinese Medicine.
CN Wang, Wanchun; Jiangxi University of Traditional Chinese Medicine. toxins incl. dis ; e, Article En LILACS, VETINDEX ID: biblio
Snake venom detoxification methods is generally recognized that energy absorbed from ionizing radiation gamma rays Snake venom detoxification methods inactivate Natural metabolic enhancer material in venon ways. A direct methode occurs when the primary event, i. This is the case when Snake venom detoxification methods compound is irradiated in veenom state. When a compound is irradiated in a solution, the indirect effect joins the direct 9. Since water is the most abundant constituent of biological material, it is important to consider the species produced by excitation and ionization of water itself, and the reaction of these species with the target molecules of biological importance. This indirect effect results from the reactions among the studied molecules and the products of radiation interaction with water or other solvents. Venoms are complex mixtures Blood sugar control for energy toxic compounds delivered by bite or sting. In humans, Snakee consequences of Emotion regulation techniques range from self-limiting to Snake venom detoxification methods. Critical host mrthods against envenomation comprises innate and venoom immune strategies Snake venom detoxification methods towards venom detection, Snake venom detoxification methods, detoxification, and symptom resolution. In some instances, venoms mediate immune dysregulation that contributes to symptom severity. This review details the involvement of immune cell subtypes and mediators, particularly of the dermis, in host resistance and venom-induced immunopathology. We further discuss established venom-associated immunopathology, including allergy and systemic inflammation, and investigate Irukandji syndrome as a potential systemic inflammatory response. Finally, this review characterises venom-derived compounds as a source of immune modulating drugs for treatment of disease.Snake venom detoxification methods -
The emergency treatment of snakebites is based primarily on clinical practice guidelines, some of which lack scientific study. Furthermore, our understanding of the relationship between Compound Chinese Medicine and the effects of multiple components is still in its infancy [ 17 Sun K, Fan J, Han J.
Acta Pharm Sin B. Rapid and accurate identification of the snakebite etiology is also an important prerequisite for timely and effective treatment in TCM. It is urgent to correlate the pharmacological properties to clinical manifestations for a better understanding of wind-fire toxin and fire toxin.
Investigation and analysis of the protein composition of serum from snakebite patients for diagnostic biomarkers will contribute to the clinical practice.
This study aims at solving diagnostic markers and investigating pathways of snake venom-induced toxicity from serum proteins of snakebite patients with four predominant venomous snake species in China.
The serum protein profiles reflected the functional categorization. The differential abundance proteins DAPs supplied discovery biomarkers to distinguish snakebite by species.
The network of interacting proteins and drug compounds contribute to understanding the complex pathogenesis of venom-induced toxicity. Serum proteome analysis could contribute to TCM diagnostic markers of snakebite syndromes, providing clinicians with a clear distinction between the wind-fire toxin and fire toxin, as well as early clinical identification of snake species.
The experimental procedures were approved by the Ethics Committee of the Affiliated Hospital of Jiangxi University of Traditional Chinese Medicine n.
Informed consent forms were obtained from all recruited participants in the surgical department of the Traditional Chinese Medicine of the Affiliated Hospital. All identified snakebite patients were reviewed for eligibility to inclusion and exclusion criteria.
Patients were excluded for the following reasons:. Clinicians identified the pattern of fire toxin and wind-fire toxin according to the standards of TCM, including clinical diagnostic experience and patient medical records. From the serum samples available, we selected four cases bitten by vipers B and three cases bitten by cobras C as the wind-fire toxin group; four cases bitten by Agkistrodon acutus D and three cases bitten by Trimeresurus stejnegeri E as the fire toxin group; and fifteen healthy volunteers as the control group.
The serum samples from 5 healthy controls were pooled together, so that the individuals in the control group were divided into three experimental duplicates, named A1, A2, and A3. The wind-fire toxin group was coded B1, B2, B3, B4, C1, C2, and C3; while the fire toxin group was coded D1, D2, D3, D4, E1, E2, and E3.
All of the serum samples were processed as described previously [ 18 Tu C, Rudnick PA, Martinez MY, Cheek KL, Stein SE, Slebos RJC, et al. Depletion of abundant plasma proteins and limitations of plasma proteomics. J Proteome Res. Briefly, high abundance proteins were first depleted by multiple affinity removal according to the Agilent protein purification protocol [ 19 Agilent Technologies.
Agilent Human 14 Multiple Affinity Removal System Columns for the Fractionation of High-Abundant Proteins from Human Proteomic Samples. Agilent Technologies, Laemmli UK. Cleavage of structural proteins during the assembly of the head of bacteriophage T4.
The gel was stained with Coomassie blue, then re-suspended with dithiothreitol and digested with the sequence grade modified Trypsin Promega [ 21 Candiano G, Bruschi M, Musante L, Santucci L, Ghiggeri GM, Carnemolla B, et al.
Blue silver: a very sensitive colloidal Coomassie G staining for proteome analysis. The digested proteins were passed through a C18 cartridge to be desalted. Finally, the dried peptides were resuspended in 40µL of 0. Then 2 µL peptide injection volume was loaded via a direct inject column configuration onto an Easy-nano LC instrument Thermo Fisher Scientific coupled online to a Q-Exactive Plus Thermo Fisher Scientific.
The resuspended peptides were first separated on Thermo Acclaim PepMap RSLC nanoViper C18 column 50 µm×15 cm using solvent A 0. Bhosale SD, Moulder R, Kouvonen P, Lahesmaa R, Goodlett DR. Mass spectrometry-based serum proteomics for biomarker discovery and validation. Methods Mol Biol. Cox J, Neuhauser N, Michalski A, Scheltema RA, Olsen JV, Mann M.
Andromeda: a peptide search engine integrated into the MaxQuant environment. Cox J, Mann M. MaxQuant enables high peptide identification rates, individualized p. Nat Biotechnol. The UniProt human isoform protein database was downloaded in August , and contained , entries at this time.
For the searches, the first search and mass tolerance of 20 ppm and two max missed cleavages were allowed. Fixed modification was set to carbamidomethyl C , while variable modifications were oxidation M and acetylation protein N-terminal.
A false discovery rate FDR of 0. Matching and alignment time window in match between run options were set to 0. Furthermore, only unique proteins identified with more than unique razor peptides were considered [ 24 Finally, a label-free quantification LFQ approach was carried out for normalization of protein intensities across runs with a minimum of one ratio count [ 23 The LFQ measuring intensities were assigned to the relative abundance for each protein and used in the subsequent statistical analysis.
At least two non-null values of data in each group were required for calculation of fold change and p -values. In addition, we took into account a comparison of all missing values in one group with expression values in another group.
Proteins that were expressed in one group and not expressed in another group were considered to have a significant difference between the two groups. For the functional annotation of identified proteins, the Gene Ontology GO and UniProt databases were used. GO enrichment analyses of differentially expressed proteins were performed with Fisher's exact test.
Metsalu T, Vilo J. ClustVis: a web tool for visualizing clustering of multivariate data using Principal Component Analysis and heatmap. Nucleic Acids Res.
Protein-protein interaction PPI networks were conducted using the STITCH 5 database [ 26 Szklarczyk D, Santos A, von Mering C, Jensen LJ, Bork P, Kuhn M. STITCH 5: augmenting protein-chemical interaction networks with tissue and affinity data.
Szklarczyk D, Franceschini A, Wyder S, Forslund K, Heller D, Huerta-Cepas J, et al. STRING v protein-protein interaction networks, integrated over the tree of life.
Label-free quantitative proteomics of serum samples was performed on samples from 14 subjects with four types of snakebites and 15 healthy controls. Of the 14 patients, 7 were diagnosed by TCM to have wind-fire toxin including 4 snakebites by vipers B and 3 snakebites by cobras C , and 7 were diagnosed by TCM to have fire toxin including 4 snakebites by Agkistrodon acutus D and 3 snakebites by Trimeresurus stejnegeri E.
The fifteen healthy controls were pooled into three samples as described in the methods. Peptide identification reported using MaxQuant analysis. Protein quantification with LFQ intensity profiles obtained after normalization by the MaxLFQ algorithm.
The representative proteins for each group were comprised of , , and proteins in healthy control, wind-fire toxin, and fire toxin groups, respectively. When we filtered the results to satisfy the condition of getting at least two non-null intensities in replicates, we identified unique proteins between patients with snakebites and healthy control.
We initially examined whether the serum proteins could discriminate between the two snakebite groups and the healthy control group. We identified proteins in both patient groups, constituting Based on the serum protein expression profiles, the three groups were differentiable by principal component analysis PCA Figure 1B.
We observed that the healthy control group was clearly separated from the bulk of snakebite patients at the first principal component PC1 , accounting for In contrast, the PC2 discriminated We next evaluated the hierarchical clustering, represented as a heat map of the relative protein abundance in each protein group.
In the dendrogram, the clustering exhibited a similar expression trend across the wind-fire toxin and fire toxin groups, which appeared distinct from the protein expression patterns in the healthy control group Figure 1C. This interpretation was consistent with the PCA results.
Therefore, we conclude that the three main groups were clearly differentiable by their serum protein expression profiles. Figure 1. An overview of the distribution of the serum protein expression profiles.
A A Venn diagram of the snakebite proteins in the wind-fire toxin and fire toxin groups and the healthy control group. B Principal component analysis accounted for C The clustering of serum proteins revealed distinct protein expression patterns in the wind-fire toxin and fire toxin groups and the healthy control group.
To investigate the differential expression of proteins in the snakebite groups and the healthy control group, four subgroups on the basis of snake species were individually analyzed to identify differential abundance proteins DAPs as compared with those in the healthy control group.
The distributions of upregulation and downregulation of 93 DAPs in the four snakebite subgroups are shown in Additional file 3 Additional file 3. The distribution of 93 differential abundance proteins DAPs among each snakebite subgroup and the healthy control group.
Upregulation and downregulation of 38 DAPs are statistically significant in expression. Expression and no expression of 55 proteins represent only detection in one subgroup. The total number is larger than the number of DAPs because of the overlap of DAPs in the four snakebite subgroups as compared to the healthy control group.
Of these DAPs, 14 proteins were upregulated and 28 were downregulated relative to the peptide intensities of the healthy control group in Additional file 3 Additional file 3.
A Venn diagram depicted the overlap of 38 DAPs from the identified serum proteins between the snakebite groups and the healthy control group Figure 2.
Figure 2. Venn diagrams depicting the distribution of upregulation and downregulation of the 38 differential abundance proteins DAPs with statistical significance. A The overlap of significantly upregulated protein in the four snakebite subgroups as compared to the healthy control group.
B The overlap of significantly downregulated proteins in the four snakebite subgroups as compared to the healthy control group. Further comparisons between the four snakebite subgroups were detailed in a heat map Figure 3.
Unsupervised hierarchical clustering revealed different protein expression profiles among the four subgroups of snake species. However, no strong clustering was observed to separate wind-fire toxin and fire toxin Figures 3A and 3B.
Given the low overlap and lack of strong clustering of proteins between the four snakebite subgroups, great care should be taken in defining biomarker discovery for snakebites. Figure 3. A biological heat map of DAP clustering based on fold changes between each snakebite subgroup and the healthy control group.
A Thirty-eight proteins with statistically significant differences in expression were shown. B Fifty-five proteins displayed no expression in one group by subgroup comparisons. The color depth from blue to red represents the level of change of protein abundance; whereas blue and red represent, respectively, proteins with decreased and increased expression relative to the healthy control group.
To identify potential molecular processes associated with serum proteins that are characteristic of snake venom-induced toxicity, all proteins were categorized by their Gene Ontology GO terms.
The GO annotations identified proteins that were assigned to GO terms. The molecular function classes included carbon-oxygen lyase activity and heme binding. Figure 4. Gene Ontology GO enrichment analysis for venom-induced DAPs. GO terms were categorized by their associated biological processes as shown.
All statistically significant categories are represented by color nodes, with those that are reddish representing a higher value of significance. The nodes of significant terms were defined as those with an adjusted p-value of less than 0.
To understand the complex pathogenesis induced by snake venoms, the network of interacting proteins and drug compounds was constructed from the STITCH database [ 26 Both chemicals and proteins were taken as nodes, and the linkage was taken as edges assigned weight scores to measure the strength of the association.
In the constructed network of DAPs, we found one candidate compound, hydrogen peroxide, was highly associated with many DAPs Figure 5. Forty-one proteins out of the 93 DAPs were matched with annotation in STITCH.
In Additional file 5 Additional file 5. List of the differential abundance proteins DAPs participating in the network of protein and drug compound interactions. One protein cluster consists of several apolipo proteins, such as APOC2, APOC3, APOC4, APOD, and APOF, which are associated with lipid metabolism and transport.
Another cluster, including IGF2, IGFBP2, IGFBP3, IGFBP7, and HRG, is highly related to IGF-mediated growth. The third cluster, including HBA1, HBB, HBD, and SLC4A1, was associated with oxygen transport. The largest cluster was the ubiquitin mediated network, associated with innate immunity, protein degradation, and autophagy to eliminate toxic protein aggregates.
Figure 5. The network of protein and drug compound interactions. Thirty DAPs were found to be directly or indirectly associated with hydrogen peroxide.
Colored nodes represent query DAPs, and small nodes represent those with an unknown 3D structure. Large nodes represent proteins with a known or predicted 3D structure. The weight of edges indicates the confidence score, wherein a thicker line indicates stronger association.
Protein-protein interactions are represented by a gray edge, while chemical-protein interactions are depicted in green. Snakebites from highly venomous species can be fatal [ 4 4.
Alirol E, Sharma SK, Bawaskar HS, Kuch U, Chappuis F. Snake bite in South Asia: a review. Gutierrez JM. Snakebite envenoming from an Ecohealth perspective.
Toxicon X. It is often difficult to find the appropriate antivenom for optimal clinical management, due to the misidentification of the snake species. Previously, there was a lack of careful studies investigating the protein profiles of the serum from snakebite patients.
Thus, we used label-free protein expression profiling to identify potential protein biomarkers in the serum of patients bitten by four different snake species.
We found that one candidate compound, hydrogen peroxide, was highly associated with many proteins in the interaction network of proteins and drug compounds. The label-free method is an effective technique for the simultaneous identification and quantification of thousands of proteins, providing potential biomarkers in a highly focused pool [ 29 Higgs RE, Knierman MD, Gelfanova V, Butler JP, Hale JE.
Label-free LC-MS method for the identification of biomarkers. Qian WJ, Jacobs JM, Liu T, Camp DG 2nd, Smith RD. Advances and challenges in liquid chromatography-mass spectrometry-based proteomics profiling for clinical applications.
Mol Cell Proteomics. Due to interpersonal variability, the expression proteins were qualified to satisfy the condition of at least two non-null intensities in replicates of each subgroup.
This resulted in unique proteins that showed high reproducibility between snakebite patients and the healthy control group. The distinct reduction in the number of shared proteins may result from biased estimates in the clinic in identifying similar snakes [ 31 Wuster W, Allum CS, Bjargardottir IB, Bailey KL, Dawson KJ, Guenioui J, et al.
Do aposematism and Batesian mimicry require bright colours? A test, using European viper markings. Proc Biol Sci. However, the wind-fire toxin patients that were bitten by vipers and cobras are distinguished from the fire toxin patients bitten by Agkistrodon acutus and Trimeresurus stejnegeri in TCM.
Based on serum protein expression profiles, we observed a significant distinction in PCA and hierarchical clustering between the wind-fire toxin and fire toxin groups Figure 1B and 1C. We observed two obvious clusters of significantly upregulated proteins, presented in Figure 1C.
Therefore, exploring differences in the serum protein expression profile is effective to distinguish snakebites, as well as for biomarker and antivenom discovery. Discovering the pathways the identified serum proteins are associated with offers an opportunity for biomarker discovery. DAPs were associated with the hydrogen peroxide catabolic process, carbon-oxygen lyase activity, and heme binding.
Previous studies have demonstrated that venom-induced toxicity elevates reactive oxygen species ROS and hydrogen peroxide levels, implying potential cytotoxicity of venom [ 11 Santhosh MS, Sundaram MS, Sunitha K, Kemparaju K, Girish KS. Viper venom-induced oxidative stress and activation of inflammatory cytokines: a therapeutic approach for overlooked issues of snakebite management.
Inflamm Res. The compound hydrogen peroxide is an important component of ROS, which regulates many cellular functions in limited concentrations, but can also cause damage of cellular organelles, DNA, and proteins when present in excessive concentrations, an effect known as oxidative stress [ 33 Marnett LJ.
Oxyradicals and DNA damage. The interaction network of proteins and drug compounds showed that hydrogen peroxide was highly associated with many DAPs Figure 5. These interacting DAPs were grouped into four clusters, including lipid metabolism and transport, IGF-mediated growth, oxygen transport, and innate immunity.
The venom-induced toxicity activates various oxidases and respiratory burst due to inflammation [ 34 Sampaio SC, Sousa-e-Silva MC, Borelli P, Curi R, Cury Y.
Crotalus durissus terrificus snake venom regulates macrophage metabolism and function. A Comprehensive View of the Structural and Functional Alterations of Extracellular Matrix by Snake Venom Metalloproteinases Svmps : Novel Perspectives on the Pathophysiology of Envenoming.
Toxins 8 10 Chippaux JP, Goyffon M. Epidemiology of Scorpionism: A Global Appraisal. Acta Trop 2 —9. Helbling A, Müller UR. Allergic Reactions to Stinging and Biting Insects , Fifth ed.
Rich R, Fleisher T, Shearer W, Schroeder H, Frew A, Weyand C, editors. London: Elsevier Google Scholar. Egawa G, Kabashima K. Skin as a Peripheral Lymphoid Organ: Revisiting the Concept of Skin-Associated Lymphoid Tissues. J Invest Dermatol 11 — Eyerich S, Eyerich K, Traidl-Hoffmann C, Biedermann T.
Cutaneous Barriers and Skin Immunity: Differentiating a Connected Network. Trends Immunol 39 4 — Reis MB, Zoccal KF, Gardinassi LG, Faccioli LH. Scorpion Envenomation and Inflammation: Beyond Neurotoxic Effects. Toxicon Off J Int Soc Toxinol —9.
Aristizábal B GÁ. Innate Immune System. Autoimmunity: From Bench to Bedside. Anaya JM SY, Rojas-Villarraga A, editors. Bogota Colombia: El Rosario University Press Mogensen TH. Pathogen Recognition and Inflammatory Signaling in Innate Immune Defenses. Clin Microbiol Rev 22 2 — Strbo N, Yin N, Stojadinovic O.
Innate and Adaptive Immune Responses in Wound Epithelialization. Adv Wound Care New Rochelle 3 7 — Dunkelberger JR, Song W-C.
Complement and its Role in Innate and Adaptive Immune Responses. Cell Res 20 1 — Palm NW, Medzhitov R. Role of the Inflammasome in Defense Against Venoms.
Proc Natl Acad Sci U States America 5 — Teixeira CF, Zamuner SR, Zuliani JP, Fernandes CM, Cruz-Hofling MA, Fernandes I, et al. Neutrophils do Not Contribute to Local Tissue Damage, But Play a Key Role in Skeletal Muscle Regeneration, in Mice Injected With Bothrops Asper Snake Venom.
Muscle Nerve 28 4 — Xu H, Timares L, Elmets CA. Host Defenses in the Skin. In: Rich RR, Fleisher TA, Shearer WT, Schroeder HW, Frew AJ, Weyand CM, editors.
Clinical Immunology. Elsevier Saunders Schlüter H, Upjohn E, Varigos G, Kaur P. Burns and Skin Ulcers. In: Lanza R, Atala A, editors. Essentials of Stem Cell Biology , 3rd ed.
Boston: Academic Press Albanesi C, Madonna S, Gisondi P, Girolomoni G. The Interplay Between Keratinocytes and Immune Cells in the Pathogenesis of Psoriasis.
Front Immunol —. Pivarcsi A, Kemeny L, Dobozy A. Innate Immune Functions of the Keratinocytes. A Rev Acta Microbiol Immunol Hungarica 51 3 — Lebre MC, van der Aar AMG, van Baarsen L, van Capel TMM, Schuitemaker JHN, Kapsenberg ML, et al. Human Keratinocytes Express Functional Toll-Like Receptor 3, 4, 5, and 9.
J Invest Dermatol 2 — Costal-Oliveira F, Stransky S, Guerra-Duarte C, Naves de Souza DL, Vivas-Ruiz DE, Yarlequé A, et al. L-Amino Acid Oxidase From Bothrops Atrox Snake Venom Triggers Autophagy, Apoptosis and Necrosis in Normal Human Keratinocytes. Sci Rep 9 1 —. Stransky S, Costal-Oliveira F, Lopes-de-Souza L, Guerra-Duarte C, Chávez-Olórtegui C, Braga VMM.
In Vitro Assessment of Cytotoxic Activities of Lachesis Muta Muta Snake Venom. PloS neglected Trop Dis 12 4 :e Silva-de-Franca F, Villas-Boas IM, Serrano SMT, Cogliati B, Chudzinski SAA, Lopes PH, et al.
Naja Annulifera Snake: New Insights Into the Venom Components and Pathogenesis of Envenomation. PloS Negl Trop Dis 13 1 :e Bhattacharjee P, Mitra J, Bhattacharyya D. L-Amino Acid Oxidase From Venoms.
Dordrecht: Springer Netherlands Paixão-Cavalcante D, van den Berg CW, de Freitas Fernandes-Pedrosa M, Gonçalves de Andrade RM, Tambourgi DV. Role of Matrix Metalloproteinases in HaCaT Keratinocytes Apoptosis Induced by Loxosceles Venom Sphingomyelinase D.
J Invest Dermatol 1 —8. Telser A. Molecular Biology of the Cell. New York: Garland Science Al-Soudi A, Kaaij MH, Tas SW.
Endothelial Cells: From Innocent Bystanders to Active Participants in Immune Responses. Autoimmun Rev 16 9 — Khakpour S, Wilhelmsen K, Hellman J. Vascular Endothelial Cell Toll-like Receptor Pathways in Sepsis.
Innate Immun 21 8 — Pugin J, Ulevitch RJ, Tobias PS. Tumor Necrosis Factor-Alpha and Interleukin-1 Beta Mediate Human Endothelial Cell Activation in Blood At Low Endotoxin Concentrations. J Inflammation 45 1 — Krishnaswamy G, Kelley J, Yerra L, Smith JK, Chi DS. Human Endothelium as a Source of Multifunctional Cytokines: Molecular Regulation and Possible Role in Human Disease.
J Interferon Cytokine Res 19 2 — Teijaro John R, Walsh Kevin B, Cahalan S, Fremgen Daniel M, Roberts E, Scott F, et al. Endothelial Cells are Central Orchestrators of Cytokine Amplification During Influenza Virus Infection.
Cell 6 — Pober JS, Merola J, Liu R, Manes TD. Antigen Presentation by Vascular Cells. Front Immunol Joyce DE, Nelson DR, Grinnell BW. Leukocyte and Endothelial Cell Interactions in Sepsis: Relevance of the Protein C Pathway.
Crit Care Med 32 5 Suppl :S—6. Nourshargh S, Alon R. Leukocyte Migration Into Inflamed Tissues. Immunity 41 5 — Krieglstein CF, Granger DN. Adhesion Molecules and Their Role in Vascular Disease.
Am J Hypertens 14 6 Pt 2 s—54s. Danese S, Dejana E, Fiocchi C. Immune Regulation by Microvascular Endothelial Cells: Directing Innate and Adaptive Immunity, Coagulation, and Inflammation.
J Immunol Baltimore Md 10 — Borkow G, Lomonte B, Gutierrez JM, Ovadia M. Effect of Various Viperidae and Crotalidae Snake Venoms on Endothelial Cells In Vitro.
Toxicon Off J Int Soc Toxinol 32 12 — Nowatzki J, de Sene RV, Paludo KS, Veiga SS, Oliver C, Jamur MC, et al. Brown Spider Venom Toxins Interact With Cell Surface and are Endocytosed by Rabbit Endothelial Cells. Toxicon Off J Int Soc Toxinol 56 4 — Chung C-H, Wu W-B, Huang T-F.
Aggretin, a Snake Venom—Derived Endothelial Integrin α2β1 Agonist, Induces Angiogenesis Via Expression of Vascular Endothelial Growth Factor. Blood 6 — Paludo KS, Gremski LH, Veiga SS, Chaim OM, Gremski W, de Freitas Buchi D, et al. The Effect of Brown Spider Venom on Endothelial Cell Morphology and Adhesive Structures.
Toxicon Off J Int Soc Toxinol 47 8 — Delafontaine M, Villas-Boas IM, Mathieu L, Josset P, Blomet J, Tambourgi DV. Enzymatic and Pro-Inflammatory Activities of Bothrops Lanceolatus Venom: Relevance for Envenomation.
Toxins 9 8 Patel KD, Modur V, Zimmerman GA, Prescott SM, McIntyre TM. The Necrotic Venom of the Brown Recluse Spider Induces Dysregulated Endothelial Cell-Dependent Neutrophil Activation.
Differential Induction of GM-CSF, Il-8, and E-selectin Expression. J Clin Invest 94 2 — Chiu S, Bharat A. Role of Monocytes and Macrophages in Regulating Immune Response Following Lung Transplantation. Curr Opin Organ Transplant 21 3 — Randolph GJ, Jakubzick C, Qu C.
Antigen Presentation by Monocytes and Monocyte-Derived Cells. Curr Opin Immunol 20 1 — Franken L, Schiwon M, Kurts C. Macrophages: Sentinels and Regulators of the Immune System. Cell Microbiol 18 4 — Ma WT, Gao F, Gu K, Chen DK. The Role of Monocytes and Macrophages in Autoimmune Diseases: A Comprehensive Review.
Sampaio SC, Sousa-e-Silva MC, Borelli P, Curi R, Cury Y. Crotalus Durissus Terrificus Snake Venom Regulates Macrophage Metabolism and Function. J Leukocyte Biol 70 4 —8. PubMed Abstract Google Scholar. Setubal SS, Pontes AS, Furtado JL, Kayano AM, Stábeli RG, Zuliani JP.
Effect of Bothrops Alternatus Snake Venom on Macrophage Phagocytosis and Superoxide Production: Participation of Protein Kinase C. J Venomous Anim Toxins Including Trop Dis 17 4 — Saadi S, Assarehzadegan MA, Pipelzadeh MH, Hadaddezfuli R.
Induction of IL From Human Monocytes After Stimulation With Androctonus Crassicauda Scorpion Venom. Toxicon Off J Int Soc Toxinol — Pires WL, Kayano AM, Castro OB, Paloschi MV, Lopes JA, Boeno CN, et al.
J leukocyte Biol 3 — Rojas JM, Aran-Sekul T, Cortes E, Jaldín R, Ordenes K, Orrego PR, et al. Toxins 9 4 Zoccal KF, Ferreira GZ, Prado MKB, Gardinassi LG, Sampaio SV, Faccioli LH.
LTB4 and PGE2 Modulate the Release of MIP-1α and IL-1β by Cells Stimulated With Bothrops Snake Venoms. Khemili D, Valenzuela C, Laraba-Djebari F, Hammoudi-Triki D. Differential Effect of Androctonus Australis Hector Venom Components on Macrophage KV Channels: Electrophysiological Characterization.
Eur Biophys J 48 1 :1— Hsu C-C, Chuang W-J, Chung C-H, Chang C-H, Peng H-C, Huang T-F. Snake Venom Disintegrin Inhibits the Activation of Toll-Like Receptors and Alleviates Sepsis Through Integrin alphaVbeta3 Blockade. Sci Rep Nature Publisher Group Zoccal KF, Bitencourt C, Paula-Silva FWG, CA S, de Castro Figueiredo Bordon K, Arantes EC, et al.
Tlr2, TLR4 and CD14 Recognize Venom-Associated Molecular Patterns From Tityus Serrulatus to Induce Macrophage-Derived Inflammatory Mediators. PloS One 9 2 :e—e. Veda P. Why are Neutrophils Polymorphonuclear? Eur J Inflammation 9 2 — Kruger P, Saffarzadeh M, Weber ANR, Rieber N, Radsak M, von Bernuth H, et al.
Neutrophils: Between Host Defence, Immune Modulation, and Tissue Injury. PloS Pathog 11 3 :e Summers C, Rankin SM, Condliffe AM, Singh N, Peters AM, Chilvers ER. Neutrophil Kinetics in Health and Disease. Trends Immunol 31 8 — Pillay J, den Braber I, Vrisekoop N, Kwast LM, de Boer RJ, Borghans JA, et al.
In Vivo Labeling With 2H2O Reveals a Human Neutrophil Lifespan of 5. Blood 4 —7. Tecchio C, Micheletti A, Cassatella MA. Neutrophil-Derived Cytokines: Facts Beyond Expression.
Rorvig S, Ostergaard O, Heegaard NH, Borregaard N. Proteome Profiling of Human Neutrophil Granule Subsets, Secretory Vesicles, and Cell Membrane: Correlation With Transcriptome Profiling of Neutrophil Precursors. J leukocyte Biol 94 4 — Papayannopoulos V. Neutrophil Extracellular Traps in Immunity and Disease.
Nat Rev Immunol 18 2 — Kaplan MJ, Radic M. Neutrophil Extracellular Traps: Double-edged Swords of Innate Immunity.
J Immunol Baltimore Md 6 — Katkar GD, Sundaram MS, NaveenKumar SK, Swethakumar B, Sharma RD, Paul M, et al. Netosis and Lack of DNase Activity are Key Factors in Echis Carinatus Venom-Induced Tissue Destruction. Nat Commun Stackowicz J, Balbino B, Todorova B, Godon O, Iannascoli B, Jönsson F, et al.
Evidence That Neutrophils do Not Promote Echis Carinatus Venom-Induced Tissue Destruction. Nat Commun 9 1 Williams DJ, Faiz MA, Abela-Ridder B, Ainsworth S, Bulfone TC, Nickerson AD, et al. Strategy for a Globally Coordinated Response to a Priority Neglected Tropical Disease: Snakebite Envenoming.
PloS Negl Trop Dis 13 2 :e Krystel-Whittemore M, Dileepan KN, Wood JG. Mast Cell: A Multi-Functional Master Cell. Galli SJ, Starkl P, Marichal T, Tsai M. Allergology Int Off J Japanese Soc Allergology 65 1 :3— Rivera J, Gilfillan AM. Molecular Regulation of Mast Cell Activation.
J Allergy Clin Immunol 6 — Moon TC, Befus AD, Kulka M. Mast Cell Mediators: Their Differential Release and the Secretory Pathways Involved. Gilfillan AM, Tkaczyk C. Integrated Signalling Pathways for Mast-Cell Activation.
Nat Rev Immunol 6 3 — Metcalfe DD, Peavy RD, Gilfillan AM. Mechanisms of Mast Cell Signaling in Anaphylaxis. J Allergy Clin Immunol 4 — Galli SJ, Tsai M. Ige and Mast Cells in Allergic Disease. Nat Med 18 5 — Mast Cells and IgE can Enhance Survival During Innate and Acquired Host Responses to Venoms.
Trans Am Clin Climatological Assoc — Pejler G, Rönnberg E, Waern I, Wernersson S. Mast Cell Proteases: Multifaceted Regulators of Inflammatory Disease. Blood 24 — Fehervari Z.
Mast Cells Crack Down on Venom. Nat Immunol 12 12 —. Akdis M, Aab A, Altunbulakli C, Azkur K, Costa RA, Crameri R, et al. Interleukins From IL-1 to IL , Interferons, Transforming Growth Factor Beta, and TNF-alpha: Receptors, Functions, and Roles in Diseases.
Miller MC, Mayo KH. Chemokines From a Structural Perspective. Int J Mol Sci 18 10 Oppenheim JJ, Matsushima K, Yoshimura T, Leonard EJ. The Activities of Cytokines are Pleiotropic and Interdependent.
Immunol Lett 16 — Ozaki K, Leonard WJ. Cytokine and Cytokine Receptor Pleiotropy and Redundancy. J Biol Chem 33 —8. Aikawa N. Cytokine Storm in the Pathogenesis of Multiple Organ Dysfunction Syndrome Associated With Surgical Insults.
Nihon Geka Gakkai zasshi 97 9 —7. Bown MJ, Nicholson ML, Bell PR, Sayers RD. Cytokines and Inflammatory Pathways in the Pathogenesis of Multiple Organ Failure Following Abdominal Aortic Aneurysm Repair. Eur J Vasc endovascular Surg Off J Eur Soc Vasc Surg 22 6 — De Gaudio AR, Romagnoli S.
Sepsis and Septic Shock , Eighth ed. China: Elsevier Health Sciences Lipnik-Stangelj M. Mediators of Inflammation as Targets for Chronic Pain Treatment. Mediators Inflammation —. Zhang J-M, An J. Cytokines, Inflammation, and Pain.
Int Anesthesiol Clin 45 2 — Chen L, Deng H, Cui H, Fang J, Zuo Z, Deng J, et al. Inflammatory Responses and Inflammation-Associated Diseases in Organs. Oncotarget 9 6 — Robinson SM, Rasch S, Beer S, Valantiene I, Mickevicius A, Schlaipfer E, et al.
Systemic Inflammation Contributes to Impairment of Quality of Life in Chronic Pancreatitis. Sci Rep 9 1 Henden AS, Hill GR. Cytokines in Graft-Versus-Host Disease.
J Immunol 10 Tisoncik JR, Korth MJ, Simmons CP, Farrar J, Martin TR, Katze MG. Into the Eye of the Cytokine Storm. Microbiol Mol Biol Rev 76 1 — White M. Mediators of Inflammation and the Inflammatory Process. J Allergy Clin Immunol 3 :S—S Stone SF, Isbister GK, Shahmy S, Mohamed F, Abeysinghe C, Karunathilake H, et al.
Immune Response to Snake Envenoming and Treatment With Antivenom; Complement Activation, Cytokine Production and Mast Cell Degranulation. PloS Neglected Trop Dis 7 7 :e Ibiapina HNS, Costa AG, Sachett JAG, Silva IM, Tarrago AM, Neves JCF, et al.
An Immunological Stairway to Severe Tissue Complication Assembly in Bothrops Atrox Snakebites. Markland FS. Snake Venoms and the Hemostatic System. Toxicon Off J Int Soc Toxinol 36 12 — Luchini LSG, Pidde G, Squaiella-Baptistão CC, Tambourgi DV.
Complement System Inhibition Modulates the Pro-Inflammatory Effects of a Snake Venom Metalloproteinase. Rider P, Carmi Y, Cohen I. Biologics for Targeting Inflammatory Cytokines, Clinical Uses, and Limitations. Int J Cell Biol —.
Zoccal KF, Gardinassi LG, Bordon KCF, Arantes EC, Marleau S, Ong H, et al. EP Restrains Inflammation and Mortality Caused by Scorpion Envenomation in Mice. Front Pharmacol Dalla-Favera R, Klein U. Germinal Centres: Role in B-cell Physiology and Malignancy. Nat Rev Immunol 8 1 — Koretzky GA.
Multiple Roles of CD4 and CD8 in T Cell Activation. J Immunol 5 —4. Parker DC. T Cell-Dependent B Cell Activation. Annu Rev Immunol 11 1 — Harwood NE, Batista FD. Early Events in B Cell Activation. Annu Rev Immunol 28 1 — Restano-Cassulini R, Garcia W, Paniagua-Solís J, Possani L. Annex 5: Guidelines for the Production, Control and Regulation of Snake Antivenom Immunoglobulins: Replacement of Annex 2 of WHO Technical Report Series, No.
World Health Organization Report No. Fox S, Rathuwithana AC, Kasturiratne A, Lalloo DG, de Silva HJ. Underestimation of Snakebite Mortality by Hospital Statistics in the Monaragala District of Sri Lanka. Trans R Soc Trop Med Hygiene 7 —5. Gilliam LL, Carmichael RC, Holbrook TC, Taylor JM, Ownby CL, McFarlane D, et al.
Antibody Responses to Natural Rattlesnake Envenomation and a Rattlesnake Toxoid Vaccine in Horses. Clin Vaccine Immunol 20 5 —7. Casadevall A. Passive Antibody Administration Immediate Immunity as a Specific Defense Against Biological Weapons. Emerg Infect Dis 8 8 — Restano-Cassulini R, Garcia W, Paniagua-Solis JF, Possani LD.
Antivenom Evaluation by Electrophysiological Analysis. Toxins 9 3 Elgueta R, Benson MJ, de Vries VC, Wasiuk A, Guo Y, Noelle RJ. Immunol Rev 1 — Magee CN, Boenisch O, Najafian N. The Role of Costimulatory Molecules in Directing the Functional Differentiation of Alloreactive T Helper Cells.
Am J Transplant 12 10 — Vazquez MI, Catalan-Dibene J, Zlotnik A. B Cells Responses and Cytokine Production are Regulated by Their Immune Microenvironment. Cytokine 74 2 — Shlomchik MJ, Weisel F.
Germinal Center Selection and the Development of Memory B and Plasma Cells. Khan U, Ghazanfar H. T Lymphocytes and Autoimmunity. Int Rev Cell Mol Biol — Rangel-Santos A, Lima C, Lopes-Ferreira M, Cardoso DF. Immunosuppresive Role of Principal Toxin Crotoxin of Crotalus Durissus Terrificus Venom.
Toxicon Off J Int Soc Toxinol 44 6 — Beeton C, Pennington MW, Wulff H, Singh S, Nugent D, Crossley G, et al. Targeting Effector Memory T Cells With a Selective Peptide Inhibitor of Kv1. Mol Pharmacol 67 4 — Bencherif M, Lippiello PM, Lucas R, Marrero MB.
Alpha7 Nicotinic Receptors as Novel Therapeutic Targets for Inflammation-Based Diseases. Cell Mol Life Sci 68 6 — Bagdány M, Batista CVF, Valdez-Cruz NA, Somodi S, Rodriguez De La Vega RC, Licea AF, et al. Anuroctoxin, a New Scorpion Toxin of the α-KTx 6 Subfamily, is Highly Selective for Kv1.
Waheed H, Moin SF, Choudhary MI. Snake Venom: From Deadly Toxins to Life-Saving Therapeutics. Curr Med Chem 24 17 — Pennington MW, Czerwinski A, Norton RS. Peptide Therapeutics From Venom: Current Status and Potential. Bioorg Med Chem 26 10 — Bogin O.
Venom Peptides and Their Mimetics as Potential Drugs. Modulator — Pineda SS, Undheim EA, Rupasinghe DB, Ikonomopoulou MP, King GF. Spider Venomics: Implications for Drug Discovery. Fut Med Chem 6 15 — King GF. Venoms as a Platform for Human Drugs: Translating Toxins Into Therapeutics.
Expert Opin Biol Ther 11 11 — Ryan RYM, Lutzky VP, Herzig V, Smallwood TB, Potriquet J, Wong Y, et al. Venom of the Red-Bellied Black Snake Pseudechis Porphyriacus Shows Immunosuppressive Potential.
Toxins 12 11 Welton RE, Williams DJ, Liew D. Injury Trends From Envenoming in Australia, — Internal Med J 47 2 —6. Mullins RJ, Wainstein BK, Barnes EH, Liew WK, Campbell DE. Increases in Anaphylaxis Fatalities in Australia From to Clin Exp Allergy 46 8 — Pesek RD, Lockey RF.
Management of Insect Sting Hypersensitivity: An Update. Allergy Asthma Immunol Res 5 3 — Bilò MB. Anaphylaxis Caused by Hymenoptera Stings: From Epidemiology to Treatment.
Allergy 66 95 —7. Curotto de Lafaille MA, Lafaille JJ, Graça L. Mechanisms of Tolerance and Allergic Sensitization in the Airways and the Lungs. Curr Opin Immunol 22 5 — Ollert M, Blank S. Anaphylaxis to Insect Venom Allergens: Role of Molecular Diagnostics. Curr Allergy Asthma Rep 15 5 —. Janeway C, National Library of M.
Immunobiology: The Immune System in Health and Disease. Fifth ed. New York: Garland Pub van Ree R, Hummelshøj L, Plantinga M, Poulsen LK, Swindle E.
Allergic Sensitization: Host-immune Factors. Clin Trans Allergy 4 1 Ellenbogen Y, Jiménez-Saiz R, Spill P, Chu DK, Waserman S, Jordana M.
The Initiation of Th2 Immunity Towards Food Allergens. Int J Mol Sci 19 5 Thangam EB, Jemima EA, Singh H, Baig MS, Khan M, Mathias CB, et al. The Role of Histamine and Histamine Receptors in Mast Cell-Mediated Allergy and Inflammation: The Hunt for New Therapeutic Targets. Front Immunol 9 Stitt JMD, Katial RMD.
Venom Allergy. J Allergy Clin Immunol: In Pract 4 1 —5. Lieberman P. Biphasic Anaphylactic Reactions. Ann allergy Asthma Immunol Off Publ Am Coll Allergy Asthma Immunol 95 3 —26; quiz 26, Liu M, Yokomizo T. The Role of Leukotrienes in Allergic Diseases.
Allergology Int 64 1 — Niedoszytko M, Bonadonna P, Oude Elberink JN, Golden DB. Epidemiology, Diagnosis, and Treatment of Hymenoptera Venom Allergy in Mastocytosis Patients.
Immunol Allergy Clinics North America 34 2 — Philipp AMD, Ferdman RMMDM, Tam JSMD. Evaluation of Venom Allergy. Ann Allergy Asthma Immunol 4 —7. The Use of Antihistamines in the Prevention and Treatment of Anaphylaxis and Anaphylactoid Reactions.
J Allergy Clin Immunol 86 4 Pt 2 —6. Remigante A, Costa R, Morabito R, La Spada G, Marino A, Dossena S. Impact of Scyphozoan Venoms on Human Health and Current First Aid Options for Stings.
Toxins 10 4 Schiener M, Graessel A, Ollert M, Schmidt-Weber CB, Blank S. Allergen-Specific Immunotherapy of Hymenoptera Venom Allergy - Also a Matter of Diagnosis. Hum Vaccin Immunother 13 10 — Mattila P, Joenväärä S, Renkonen J, Toppila-Salmi S, Renkonen R.
Allergy as an Epithelial Barrier Disease. Clin Trans Allergy 1 1 :1—8. Cegolon L, Heymann WC, Lange JH, Mastrangelo G. Jellyfish Stings and Their Management: A Review. Mar Drugs 11 2 — Montgomery L, Seys J, Mees J. To Pee, or Not to Pee: A Review on Envenomation and Treatment in European Jellyfish Species.
Mar Drugs 14 7 Glatstein M, Adir D, Galil B, Scolnik D, Rimon A, Pivko-Levy D, et al. Pediatric Jellyfish Envenomation in the Mediterranean Sea.
Eur J Emergency Med Off J Eur Soc Emergency Med 25 6 —9. Horiike T, Nagai H, Kitani S. Identification of Allergens in the Box Jellyfish Chironex Yamaguchii That Cause Sting Dermatitis. Int Arch Allergy Immunol 2 — Friedel N, Scolnik D, Adir D, Glatstein M.
Severe Anaphylactic Reaction to Mediterranean Jellyfish Ropilhema Nomadica Envenomation: Case Report. Toxicol Rep —9. Uri S, Marina G, Liubov G. Severe Delayed Cutaneous Reaction Due to Mediterranean Jellyfish Rhopilema Nomadica Envenomation. Contact Dermatitis 52 5 —3.
Kubota S, Nozawa A, Yanai T, Ozasa K, Mori S, Kurihara K. The Case of a Year-Old Boy Who Experienced Anaphylaxis Due to Jellyfish Mastigias Papua Ingestion.
Cañas JA, Rodrigo-Muñoz JM, Rondon-Cepeda SH, Bordehore C, Fernández-Nieto M, del Pozo V. Jellyfish Collagen: A New Allergen in the Beach. Ann Allergy Asthma Immunol 4 —1. Tibballs J, Yanagihara AA, Turner HC, Winkel K. Immunological and Toxinological Responses to Jellyfish Stings. Inflammation Allergy Drug Targets 10 5 — Buttaravoli PMDF, Leffler SMMDF.
Marine Envenomations , 3rd ed. London: Elsevier Health Sciences Morabito R, Marino A, La Spada G. J Comp Physiol A 6 — Varney SMMDFF. Bites and Stings , Sixth ed. Philaldelphia: Elsevier Badré S. Bioactive Toxins From Stinging Jellyfish. Nagai H, Takuwa K, Nakao M, Ito E, Miyake M, Noda M, et al.
Novel Proteinaceous Toxins From the Box Jellyfish Sea Wasp Carybdea Rastoni. Biochem Biophys Res Commun 2 —8. Nagai H, Takuwa K, Nakao M, Sakamoto B, Crow GL, Nakajima T. Isolation and Characterization of a Novel Protein Toxin From the Hawaiian Box Jellyfish Sea Wasp Carybdea Alata.
Biochem Biophys Res Commun 2 — Nagai H, Takuwa-Kuroda K, Nakao M, Oshiro N, Iwanaga S, Nakajima T. A Novel Protein Toxin From the Deadly Box Jellyfish Sea Wasp, Habu-Kurage Chiropsalmus Quadrigatus.
Biosci Biotechnol Biochem 66 1 — Brinkman DL, Konstantakopoulos N, McInerney BV, Mulvenna J, Seymour JE, Isbister GK, et al. Chironex Fleckeri Box Jellyfish Venom Proteins: Expansion of a Cnidarian Toxin Family That Elicits Variable Cytolytic and Cardiovascular Effects.
J Biol Chem 8 — Kramp PL. Synopsis of the Medusae of the World. J Marine Biol Assoc U Kingdom — Tibballs J.
Australian Venomous Jellyfish, Envenomation Syndromes, Toxins and Therapy. Toxicon Off J Int Soc Toxinol 48 7 — White J.
In: Payne-James J, Byard RW, editors. Encyclopedia of Forensic and Legal Medicine , 2nd ed. Oxford: Elsevier Fox JW. Venoms and Poisons From Marine Organisms.
In: Goldman L, Schafer AI, editors. Philadelphia: W. Saunders Brinchmann BC, Bayat M, Brøgger T, Muttuvelu DV, Tjønneland A, Sigsgaard T. A Possible Role of Chitin in the Pathogenesis of Asthma and Allergy. Ann Agric Environ Med 18 1 :7— Burton OT, Zaccone P. The Potential Role of Chitin in Allergic Reactions.
Trends Immunol 28 10 — Lee CG, Da Silva CA, Dela Cruz CS, Ahangari F, Ma B, Kang M-J, et al. Annu Rev Physiol — Inomata N, Chin K, Aihara M.
Anaphylaxis Caused by Ingesting Jellyfish in a Subject With Fermented Soybean Allergy: Possibility of Epicutaneous Sensitization to Poly-Gamma-Glutamic Acid by Jellyfish Stings. J Dermatol 41 8 —3. Inomata N, Miyakawa M, Aihara M. Surfing as a Risk Factor for Sensitization to Poly γ-Glutamic Acid in Fermented Soybeans, Natto, Allergy.
Allergology Int 67 3 —6. Shimabukuro-Vornhagen A, Gödel P, Subklewe M, Stemmler HJ, Schlößer HA, Schlaak M, et al. Cytokine Release Syndrome. J Immunother Cancer 6 1 Suntharalingam G, Perry MR, Ward S, Brett SJ, Castello-Cortes A, Brunner MD, et al.
Cytokine Storm in a Phase 1 Trial of the anti-CD28 Monoclonal Antibody TGN New Engl J Med 10 — Wood AJ, Darbyshire J. Injury to Research Volunteers; the Clinical-Research Nightmare.
New Engl J Med 18 — Reis MB, Rodrigues FL, Lautherbach N, Kanashiro A, Sorgi CA, Alyne FGM, et al. Interleukin-1 Receptor-Induced PGE2 Production Controls Acetylcholine-Mediated Cardiac Dysfunction and Mortality During Scorpion Envenomation.
Nat Commun 11 1 —. Tiong K. Irukandji Syndrome, Catecholamines, and Mid-Ventricular Stress Cardiomyopathy. Eur Heart J - Cardiovasc Imaging 10 2 —6. Petricevich VL. Scorpion Venom and the Inflammatory Response. Santos MS, Silva CG, Neto BS, Grangeiro Junior CR, Lopes VH, Teixeira Junior AG, et al.
Clinical and Epidemiological Aspects of Scorpionism in the World: A Systematic Review. Wilderness Environ Med 27 4 —
This study Snake venom detoxification methods to evaluate the clinical detoxkfication efficacy Snake venom detoxification methods anti-snake venom serum blockade Mental alertness games treating Detoxufication tissue Sbake caused by Chinese cobra Snakr Snake venom detoxification methods bites. The experimental group methlds regular as well as anti-snake vsnom serum blocking treatment, whereas regular treatment plus chymotrypsin blocking therapy was given to the control group. The necrotic volumes around snake wounds in veenom groups were detected on the first, third and seventh days. On the third day of treatment, some local tissues in the wounds were randomly selected for pathological biopsy, and the necrosis volume of the local tissue was observed. Furthermore, the amount of time required for wound healing was recorded. Moreover, the pathological biopsies taken from the control group showed nuclear pyknosis, fragmentation, sparse nuclear density, and blurred edges, and the degree of necrosis was much higher than that of the experimental group. Anti-snake venom blocking therapy is a new and improved therapy with good clinical effect on local tissue necrosis caused by Chinese cobra bites; moreover, it is superior to conventional chymotrypsin blocking therapy in the treatment of cobra bites.
Die Stunde von der Stunde ist nicht leichter.
ich beglückwünsche, der prächtige Gedanke