
Video
Lipolysis Pathway - Triglycerides Breakdown DOI: Glucose is metabooism essential metabolic Blood sugar crash and hormonal health of all mammalian cells. D-glucose utklization the major Osteoporosis prevention methods presented to the cell for energy production and many other anabolic requirements. Under normal physiological conditions, it is the sole source energy for the brain. Glucose is obtained directly from the diet.Lipid metabolism and glucose utilization -
This delay indicates that FFAs have an indirect effect, a contention that is supported by the observation that acute increases in plasma FFAs increased triglyceride content in muscle cells of human volunteers This rise in intramyocellular triglyceride concentration occurred several hours after the elevation of FFAs and coincided with the development of insulin resistance However, it is probably not the accumulation of fat in muscle cells that causes insulin resistance but rather the accumulation of other metabolites, including diacylglycerol DAG , that occur at the same time DAG, which is an intermediate of triglyceride metabolism, is a potent activator of protein kinase C PKC In healthy volunteers, along with the rise in intramyocellular levels of DAG, there was a concomitant increase in PKC activity PKC is an enzyme that can phosphorylate serine and threonine residues on both the insulin receptor 19 , 20 and insulin receptor substrate IRS -1 20 , The latter two molecules are important for insulin signaling.
Serine phos-phorylation of IRS-1 can lead to its destruction and to insulin resistance A change in intracellular DAG levels is also accompanied by activation of the nuclear factor NF -κB pathway Fig. NF-κB has been linked to fatty acid—induced impairment of insulin action in rodents 23 , NF-κB is also increasingly recognized as playing a crucial role in the pathogenesis of coronary artery disease Thus, the activation of NF-κB may also help to explain the increased prevalence of vascular disease in obese patients with type 2 diabetes.
Consequently, lowering FFA concentrations may prevent activation of the NF-κB pathway and have benefits beyond increasing insulin sensitivity and improving regulation of glucose levels. Another mechanism by which FFAs can cause insulin resistance is by increasing oxidative stress Reactive oxygen species can activate PKC and the NF-κB pathway Fig.
FFAs also affect the functioning of insulin in the liver and thus contribute to hepatic overproduction of glucose and to elevated circulating blood glucose levels The main role of insulin in the liver is control of glucose production. The mechanism by which insulin acutely within 1—2 h suppresses hepatic glucose production is by inhibiting glycogenolysis FFAs produce insulin resistance in the liver by inhibiting the acute insulin suppression of glycogenolysis Insulin also promotes hepatic uptake of FFAs and production of intracellular triglycerides.
Thus, insulin resistance in the liver may contribute to elevated plasma FFA levels. An increase in visceral fat could also cause insulin resistance by mechanisms that do not directly involve FFAs Fig. Adipose tissue is a source of inflammatory mediators, such as tumor necrosis factor TNF -α 31 and interleukin IL -6 32 and peptides that include resistin 33 , leptin 34 , and adiponectin So far, however, the physiological relevance of these adipokines for the development of insulin resistance in humans has not been established.
Of all the adipokines mentioned, adiponectin is most likely to affect insulin sensitivity. Adiponectin is produced exclusively in adipocytes. It stimulates fatty acid oxidation, decreases plasma triglycerides, and improves glucose metabolism by increasing insulin sensitivity Adiponectin levels are negatively correlated with the development of insulin resistance in rhesus monkeys The plasma levels of adiponectin in Caucasians and Pima Indians are negatively correlated with percent body fat and plasma insulin levels and are positively correlated with insulin-mediated glucose uptake 35 , In addition, plasma levels of adiponectin are lower in individuals with type 2 diabetes than in age- and body mass—matched individuals without diabetes Thus, the impaired release of adiponectin that occurs in obesity may contribute to insulin resistance and development of type 2 diabetes.
The mechanism leading to decreased adiponectin levels in obesity 39 is not clear. Adiponectin is inhibited by insulin and TNF-α.
Therefore, hyperinsulinemia caused by obesity-induced insulin resistance, together with enhanced TNF-α expression, may contribute to reduced adiponectin secretion. It has also been suggested that visceral adipose tissue may produce an as yet unidentified substance that destabilizes adiponectin mRNA Insulin resistance in the liver results in overproduction of glucose, whereas insulin resistance in skeletal muscle produces underutilization of glucose.
Because FFAs can induce insulin resistance in both liver and muscle, all overweight or obese people, who are likely to have elevated plasma FFA levels, might be expected to have elevated glucose levels. On the basis of this new definition, the actual proportion of overweight people with impaired glucose metabolism will be higher than the estimates from published surveys including NHANES III that used the older definition.
Recently, it has become clearer why many obese, insulin-resistant people will never develop diabetes. In obese people with normal pancreatic β-cells, FFAs are potent insulin secretagogues and can compensate for the insulin resistance that they produce.
Acute elevations of plasma FFAs have long been known to stimulate insulin secretion More importantly, prolonged elevations of plasma FFAs 2—4 days have been shown to potentiate glucose-stimulated insulin secretion in healthy volunteers 43 — In contrast, in first-degree relatives of patients with type 2 diabetes i.
This defect in FFA-stimulated insulin secretion can also be demonstrated in patients with impaired glucose tolerance 47 , 48 and in patients with overt type 2 diabetes These observations suggest that the obese individuals who develop type 2 diabetes have a genetic predisposition to pancreatic β-cell failure.
Prolonged exposure to elevated FFA levels is central to the development of insulin resistance and type 2 diabetes, making modulation of these levels an attractive therapeutic strategy. Nicotinic acid and nicotinic acid analogs are drugs that lower plasma FFA levels. Their usefulness is limited, however, because the initial lowering of plasma FFA levels by nicotinic acid is invariably followed by a sharp FFA rebound 51 that increases insulin resistance, at least temporarily.
There has therefore been considerable interest in drugs that activate the peroxisome proliferator—activated receptors PPARs , which are nuclear transcription factors that regulate the expression of numerous genes involved in lipid and carbohydrate metabolism, inflammation, and vascular tone.
Thiazolidinediones TZDs , in contrast to nicotinic acid analogs, lower plasma FFA levels without a rebound phenomenon 52 — The binding affinity between TZDs and PPAR-γ correlates well with their insulin-sensitizing activity. Therefore, it is generally accepted that TZDs exert their action through PPAR-γ 55 , PPAR-γ is expressed at highest concentrations in adipose tissue and at much lower concentrations in liver and muscle 57 , 58 , suggesting that the primary action of TZDs is on adipose tissue.
In support, it has been shown that TZDs play an important role in adipocyte development 59 and that they lower plasma levels of FFAs Fig. In addition, TZDs have been postulated to improve insulin sensitivity by redistributing fat from visceral to subcutaneous adipose tissue 60 , 61 and by increasing blood levels of adiponectin 62 , The available TZDs pioglitazone and rosiglitazone have a generally good safety and tolerability profile.
They have been associated with increased development of edema, which can exacerbate or lead to congestive heart failure 64 , 65 in high-risk patients with preexisting vascular disease 66 , The highest incidences of edema and congestive heart failure were seen when TZDs were used in combination with insulin 65 , 68 , Alongside improvements in glycemia and in some lipid parameters, e.
FFAs are natural ligands for PPAR-α, which is preferentially expressed in tissues where fatty acids are oxidized such as the liver, muscle, kidney, and heart. Activation of PPAR-α stimulates the expression of genes involved in fatty acid and lipoprotein oxidation in the liver and muscle 72 , PPAR-α activators, such as fibrates, decrease plasma FFA and triglyceride concentrations by stimulating several metabolic pathways Fig.
Fibrates increase fatty acid uptake and oxidation by increasing the expression of lipoprotein lipase in the liver and by decreasing apolipoprotein C-III concentrations.
Apolipoprotein C-III is a protein that inhibits triglyceride hydrolysis by lipoprotein lipase, and its downregulation by fibrates results in reduced triglyceride and VLDL production by the liver Simultaneously, these agents enhance intravascular triglyceride metabolism The lowering of FFAs through increased oxidation may well improve insulin sensitivity.
Specific PPAR-α agonism can lower lipid levels in rats and improve insulin sensitivity 76 , 77 , whereas studies of fibrates in humans have either reported improved 78 , 79 or unimproved 80 , 81 insulin sensitivity. PPAR-γ exerts its beneficial effect by lowering plasma FFA levels, increasing plasma adiponectin levels, and redistributing fat from visceral to subcutaneous depots, and PPAR-α activation lowers plasma FFA levels through increased fat oxidation.
Given the central role of FFAs in the development of insulin resistance and type 2 diabetes, this approach may offer an attractive option for therapeutic intervention. Ongoing studies are examining the efficacy and safety of these new agents. From an initial perception that a disorder of glucose metabolism was the primary event in the pathogenesis of type 2 diabetes, there is now a growing appreciation that chronic elevation of FFA levels is an early event that contributes to the development of this disease.
FFAs induce insulin resistance, which increases with FFA levels, and this can be a beneficial adaptive response during starvation and pregnancy. However, insulin resistance can become counterproductive when there is an excess of energy intake associated with physical inactivity.
The extra fuel is stored in visceral and subcutaneous fat depots. As fat accumulates, there is an ongoing increase in the levels of plasma FFAs, which causes insulin resistance. In addition, the deficit of another product of adipose tissue e.
To counter insulin resistance and prevent hyperglycemia, insulin levels increase. In individuals with a genetic predisposition for diabetes, however, the pancreas cannot compensate for the increased secretory demands placed on it, resulting in type 2 diabetes.
The pivotal role of FFAs in the development of insulin resistance and type 2 diabetes suggests that the optimal therapeutic intervention should decrease plasma FFA levels. The PPAR family is intimately involved in lipid metabolism. Two subtypes of these receptors are the site of action of synthetic PPAR agonists: PPAR-α and PPAR-γ.
The former increases fatty acid oxidation, whereas the latter results in the redistribution of fat from visceral to subcutaneous body fat and an increase in adiponectin. The outcome of activation of PPAR-γ is a lowering of plasma FFA concentrations and improved insulin sensitivity. The effects of PPAR-α on lipid metabolism may also bring about improvements in insulin sensitivity.
The currently available PPAR agonists selectively activate either PPAR-α i. Potential mechanism of FFA on insulin resistance and atherogenesis in human muscle.
The key initiating event is an increase in plasma FFA followed by increased uptake of FFA into muscle. This leads to intramyocellular accumulation of fatty acyl-CoA and DAG and activation of PKC the β II and δ isoforms. It is assumed that activation of PKC interrupts insulin signaling by serine phosphorylation of IRS-1, resulting in a decrease in tyrosine phosphorylation of IRS PI, phosphatidylinositol.
This work was supported by National Institutes of Health Grants RAG, RDK, RHL, and RDK and a Mentor-Based Training Grant from the American Diabetes Association all to G.
A table elsewhere in this issue shows conventional and Système International SI units and conversion factors for many substances. Sign In or Create an Account. Search Dropdown Menu. header search search input Search input auto suggest. filter your search All Content All Journals Diabetes Care.
Advanced Search. User Tools Dropdown. Sign In. Skip Nav Destination Close navigation menu Article navigation. Volume 27, Issue 9. Previous Article Next Article. FFAs AND INSULIN SECRETION.
Article Information. Article Navigation. Lipids and Glucose in Type 2 Diabetes : What is the cause and effect? Guenther Boden, MD ; Guenther Boden, MD. This Site. Google Scholar. Markku Laakso, MD Markku Laakso, MD. Address correspondencereprint requests to G.
Boden, MD, Temple University Hospital, N. Broad St. E-mail: bodengh tuhs. Diabetes Care ;27 9 — Article history Received:. Get Permissions. toolbar search Search Dropdown Menu. toolbar search search input Search input auto suggest.
Figure 1—. View large Download slide. Figure 2—. Potential contributions of PPAR-α and PPAR-γ to improvements in insulin sensitivity. McGarry JD: What if Minkowski had been ageusic? An alternative angle on diabetes. Jeppesen J, Hein HO, Suadicani P, Gyntelberg F: Relation of high TG-low HDL cholesterol and LDL cholesterol to the incidence of ischemic heart disease: an 8-year follow-up in the Copenhagen Male Study.
Arterioscler Thromb Vasc Biol. Gardner CD, Fortmann SP, Krauss RM: Association of small low-density lipoprotein particles with the incidence of coronary artery disease in men and women. Lamarche B, Tchernof A, Moorjani S, Cantin B, Dagenais GR, Lupien PJ, Despres JP: Small, dense low-density lipoprotein particles as a predictor of the risk of ischemic heart disease in men: prospective results from the Quebec Cardiovascular Study.
Mykkanen L, Kuusisto J, Haffner SM, Laakso M, Austin MA: LDL size and risk of coronary heart disease in elderly men and women. Hales CN, Barker DJ: Type 2 non-insulin-dependent diabetes mellitus: the thrifty phenotype hypothesis.
Arner P: Free fatty acids: do they play a central role in type 2 diabetes? Diabetes Obes Metab. Boden G, Jadali F, White J, Liang Y, Mozzoli M, Chen X, Coleman E, Smith C: Effects of fat on insulin-stimulated carbohydrate metabolism in normal men.
J Clin Invest. Randle PJ, Garland PB, Hales CN, Newsholme EA: The glucose fatty-acid cycle: its role in insulin sensitivity and the metabolic disturbances of diabetes mellitus. Rennie MJ, Holloszy JO: Inhibition of glucose uptake and glycogenolysis by availability of oleate in well-oxygenated perfused skeletal muscle.
Biochem J. Boden G, Chen X, Ruiz J, White JV, Rossetti L: Mechanisms of fatty acid-induced inhibition of glucose uptake.
Roden M, Price TB, Perseghin G, Petersen KF, Rothman DL, Cline GW, Shulman GI: Mechanism of free fatty acid-induced insulin resistance in humans. This phenomenon has also been suspected to appear in 11β-HSD1-null mice [ 98 ]. To circumvent these potential problems, highly selective inhibitors of 11β-HSD1 have recently been developed.
Treatment of rodents with a non-steroidal selective inhibitor of 11β-HSD1 for 7 days significantly decreased both hepatic G-6P-ase and PEPCK mRNA as well as blood glucose and serum insulin concentrations [ 99 ]. AMP-activated protein kinase AMPK belongs to a family of highly conserved serine-threonine kinases and is present in various organs, including the liver [ ].
AMPK has a key role in the regulation of energy control as a metabolic sensor and regulator kinase. When activated, AMPK initiates a series of responses that are aimed at protecting the cell against ATP depletion, by stimulating fatty acid oxidation or glycolysis and inhibiting ATP-consuming anabolic pathways such as gluconeogenesis, protein and fatty acid synthesis [ ].
AMPK is phosphorylated and thereby activated by the protein—threonine kinase LKB1, which seems to be the major upstream AMPK-activating factor [ ]. Activation of AMPK results in inhibition of lipogenic factors such as SREBP-1c [ 75 ], FASN, ACAC [ ] and ChREBP [ ].
Induction of AMPK in hepatoma cells also decreases PEPCK and GPase transcription, likely in an insulin-independent manner [ ]. AMPK is not known to be activated by insulin, raising the possibility that insulin and AMPK regulate PEPCK by different and, perhaps, converging pathways [ 70 ].
AMPK may prevent insulin resistance in part by inhibiting factors that antagonise insulin signalling [ ]. Deletion of liver LKB1 in mice results in a near complete loss of AMPK activity, leading to lipogenic gene expression. Increased gluconeogenesis in these mice could be explained by the observed nuclear translocation of TORC2, which transcriptionally coactivates cAMP-response-element-binding protein CREB , leading to increased expression of PGC-1α, thereby driving the expression of glucogenic genes [ ].
A number of hormonal and nutritionally regulated factors have been proposed to be involved in the regulation of hepatic AMPK activity. The adipocyte-derived hormone adiponectin has been shown to activate AMPK both in liver and skeletal muscle and to reduce hepatic glucose production and the expression of hepatic gluconeogenic genes, while increasing β-oxidation of fatty acids in the liver [ , ].
This may, at least in part, explain the positive associations between adiponectin and diabetes risk in epidemiological studies [ ]. Conversely, the orexigenic hormone ghrelin inhibits AMPK in the rat liver and in adipose tissue, while stimulating AMPK activity in the heart and hypothalamus [ ].
Ghrelin also decreases the effect of insulin on PEPCK in human hepatoma cells [ ], and may therefore contribute to the development of hepatic insulin resistance and lipid accumulation. Other factors, such as adipocyte-secreted leptin or resistin which is mainly expressed in monocytes and macrophages in humans may be involved in the regulation of liver AMPK.
Hypoglycaemic agents such as metformin and rosiglitazone have been proposed to indirectly activate AMPK, probably by interference with the respiratory chain [ ]. AMPK has been shown to be activated by metformin in skeletal muscle in vitro and in vivo reviewed in [ ] and by pioglitazone in cultured cells and in rat liver and adipose tissue in vivo [ ].
Interestingly, metformin action was turned off in the absence of LKB1, pointing to AMPK activation as an essential part of metformin action, at least in the mouse liver [ ].
However, thiazolidinediones [ ] and metformin [ ] exert various other molecular actions, which are not well understood at present. Moreover, chronic pharmacological activation of AMPK may lead to inhibition of insulin release, and may have unfavourable effects on cell proliferation and glycogen storage in cardiomyocytes reviewed in [ ].
Fasting has been shown to increase hypothalamic AMPK activity, while refeeding inhibits it, with reduced hypothalamic AMPK activity exerting anorexigenic effects [ , ]. Thus, non-selective AMPK activation may not be favourable in the context of body weight regulation.
The studies discussed in this review indicate that hepatic fat accumulation, insulin resistance and disturbed glucose metabolism are inter-related at a molecular level. In insulin-resistant hyperglycaemic states the suppressive effects of insulin and glucose on hepatic glucose production is reduced, whereas undamped hepatic lipogenesis and non-insulin dependent glucose transport to the liver both contribute to hepatic lipid accumulation, which in turn may further deteriorate insulin signalling.
Multiple organs, such as skeletal muscle, adipose tissue and the liver, are affected by insulin-resistant states and there has been considerable progress in identifying molecular pathways and potential factors involved.
Skeletal muscle and fat tissue are relatively easily accessible for biopsy in humans. However, despite many similarities between molecular pathways in different tissues, there are also important differences. Thus, results obtained in other tissues cannot necessarily be transferred to the liver.
Elucidating molecular pathways in human liver is more problematic due to the potential hazards involved in performing liver biopsies.
It is therefore important to note that most studies that have investigated molecular pathways in the liver were performed in animal models or in vitro. Because molecular functions differ even between rodent species [ ], it should be noted that, whilst results obtained in animal models provide valuable insights, they cannot necessarily be extrapolated to other species.
Biochem Soc Trans — Article PubMed CAS Google Scholar. Foufelle F, Ferre P New perspectives in the regulation of hepatic glycolytic and lipogenic genes by insulin and glucose: a role for the transcription factor sterol regulatory element binding protein-1c. Biochem J — Dentin R, Girard J, Postic C Carbohydrate responsive element binding protein ChREBP and sterol regulatory element binding protein-1c SREBP-1c : two key regulators of glucose metabolism and lipid synthesis in liver.
Biochimie — Ishii S, Iizuka K, Miller BC, Uyeda K Carbohydrate response element binding protein directly promotes lipogenic enzyme gene transcription.
Proc Natl Acad Sci USA — Steffensen KR, Gustafsson JA Putative metabolic effects of the liver X receptor LXR.
Diabetes 53 Suppl 1 :S36—S PubMed CAS Google Scholar. Marchesini G, Brizi M, Bianchi G et al Nonalcoholic fatty liver disease: a feature of the metabolic syndrome. Diabetes — Angulo P Nonalcoholic fatty liver disease. N Engl J Med — Seppala-Lindroos A, Vehkavaara S, Hakkinen AM et al Fat accumulation in the liver is associated with defects in insulin suppression of glucose production and serum free fatty acids independent of obesity in normal men.
J Clin Endocrinol Metab — Sutinen J, Hakkinen AM, Westerbacka J et al Rosiglitazone in the treatment of HAART-associated lipodystrophy—a randomized double-blind placebo-controlled study. Antivir Ther — Gavrilova O, Marcus-Samuels B, Graham D et al Surgical implantation of adipose tissue reverses diabetes in lipoatrophic mice.
J Clin Invest — J Biol Chem — Samuel VT, Liu ZX, Qu X et al Mechanism of hepatic insulin resistance in non-alcoholic fatty liver disease. Petersen KF, Dufour S, Befroy D et al Reversal of nonalcoholic hepatic steatosis, hepatic insulin resistance, and hyperglycemia by moderate weight reduction in patients with type 2 diabetes.
Gastaldelli A, Toschi E, Pettiti M et al Effect of physiological hyperinsulinemia on gluconeogenesis in nondiabetic subjects and in type 2 diabetic patients. Boden G Effects of free fatty acids on gluconeogenesis and glycogenolysis. Life Sci — Roden M, Bernroider E Hepatic glucose metabolism in humans—its role in health and disease.
Best Pract Res Clin Endocrinol Metab — Nordlie RC, Foster JD, Lange AJ Regulation of glucose production by the liver. Annu Rev Nutr — Pilkis SJ, Granner DK Molecular physiology of the regulation of hepatic gluconeogenesis and glycolysis. Annu Rev Physiol — Lam TK, Gutierrez-Juarez R, Pocai A, Rossetti L Regulation of blood glucose by hypothalamic pyruvate metabolism.
Science — Pocai A, Obici S, Schwartz GJ, Rossetti L A brain—liver circuit regulates glucose homeostasis. Cell Metab — Horton JD, Shah NA, Warrington JA et al Combined analysis of oligonucleotide microarray data from transgenic and knockout mice identifies direct SREBP target genes.
Randle PJ Regulatory interactions between lipids and carbohydrates: the glucose fatty acid cycle after 35 years. Diabetes Metab Rev — Ruderman NB, Saha AK, Vavvas D, Witters LA Malonyl-CoA, fuel sensing, and insulin resistance.
Am J Physiol E1—E McGarry JD Banting lecture dysregulation of fatty acid metabolism in the etiology of type 2 diabetes.
Vaulont S, Vasseur-Cognet M, Kahn A Glucose regulation of gene transcription. Koo SH, Dutcher AK, Towle HC Glucose and insulin function through two distinct transcription factors to stimulate expression of lipogenic enzyme genes in liver.
Mol Cell — Najjar SM, Yang Y, Fernstrom MA et al Insulin acutely decreases hepatic fatty acid synthase activity. Wolfrum C, Asilmaz E, Luca E, Friedman JM, Stoffel M Foxa2 regulates lipid metabolism and ketogenesis in the liver during fasting and in diabetes.
Nature — Kalaany NY, Gauthier KC, Zavacki AM et al LXRs regulate the balance between fat storage and oxidation. Gerin I, Dolinsky VW, Shackman JG et al LXRbeta is required for adipocyte growth, glucose homeostasis, and beta cell function.
Repa JJ, Mangelsdorf DJ The role of orphan nuclear receptors in the regulation of cholesterol homeostasis. Annu Rev Cell Dev Biol — Tobin KA, Ulven SM, Schuster GU et al Liver X receptors as insulin-mediating factors in fatty acid and cholesterol biosynthesis.
Cao G, Liang Y, Broderick CL et al Antidiabetic action of a liver x receptor agonist mediated by inhibition of hepatic gluconeogenesis. Stulnig TM, Oppermann U, Steffensen KR, Schuster GU, Gustafsson JA Liver X receptors downregulate 11beta-hydroxysteroid dehydrogenase type 1 expression and activity.
Stulnig TM, Steffensen KR, Gao H et al Novel roles of liver X receptors exposed by gene expression profiling in liver and adipose tissue.
Mol Pharmacol — Glass CK Differential recognition of target genes by nuclear receptor monomers, dimers, and heterodimers. Endocr Rev — Chen G, Liang G, Ou J, Goldstein JL, Brown MS Central role for liver X receptor in insulin-mediated activation of Srebp-1c transcription and stimulation of fatty acid synthesis in liver.
Yoshikawa T, Ide T, Shimano H et al Cross-talk between peroxisome proliferator-activated receptor PPAR alpha and liver X receptor LXR in nutritional regulation of fatty acid metabolism.
PPARs suppress sterol regulatory element binding protein-1c promoter through inhibition of LXR signaling. Mol Endocrinol — Ide T, Shimano H, Yoshikawa T et al Cross-talk between peroxisome proliferator-activated receptor PPAR alpha and liver X receptor LXR in nutritional regulation of fatty acid metabolism.
LXRs suppress lipid degradation gene promoters through inhibition of PPAR signaling. Miyata KS, McCaw SE, Patel HV, Rachubinski RA, Capone JP The orphan nuclear hormone receptor LXR alpha interacts with the peroxisome proliferator-activated receptor and inhibits peroxisome proliferator signaling.
Anderson SP, Dunn C, Laughter A, et al Overlapping transcriptional programs regulated by the nuclear receptors peroxisome proliferator-activated receptor alpha, retinoid X receptor, and liver X receptor in mouse liver.
Grefhorst A, Elzinga BM, Voshol PJ et al Stimulation of lipogenesis by pharmacological activation of the liver X receptor leads to production of large, triglyceride-rich very low density lipoprotein particles.
Am J Physiol Endocrinol Metab E—E Miyazaki M, Ntambi JM Role of stearoyl-coenzyme A desaturase in lipid metabolism. Prostaglandins Leukot Essent Fatty Acids — Vessby B, Unsitupa M, Hermansen K et al Substituting dietary saturated for monounsaturated fat impairs insulin sensitivity in healthy men and women: The KANWU Study.
Diabetologia — Hu T, Foxworthy P, Siesky A et al Hepatic peroxisomal fatty acid beta oxidation is regulated by liver X receptor alpha. Endocrinology — Gibbons G Old fat, make way for new fat.
Nat Med — Lemberger T, Braissant O, Juge-Aubry C et al PPAR tissue distribution and interactions with other hormone-signaling pathways.
Ann N Y Acad Sci — Browning JD, Horton JD Molecular mediators of hepatic steatosis and liver injury. Lee CH, Chawla A, Urbiztondo N et al Transcriptional repression of atherogenic inflammation: modulation by PPARdelta.
Tanaka T, Yamamoto J, Iwasaki S et al Activation of peroxisome proliferator-activated receptor delta induces fatty acid beta-oxidation in skeletal muscle and attenuates metabolic syndrome.
Reddy JK, Hashimoto T Peroxisomal beta-oxidation and peroxisome proliferator-activated receptor alpha: an adaptive metabolic system. Vidal-Puig AJ, Considine RV, Jimenez-Linan M et al Peroxisome proliferator-activated receptor gene expression in human tissues.
Effects of obesity, weight loss, and regulation by insulin and glucocorticoids. Bernal-Mizrachi C, Weng S, Feng C et al Dexamethasone induction of hypertension and diabetes is PPAR-alpha dependent in LDL receptor-null mice.
Koo SH, Satoh H, Herzig S et al PGC-1 promotes insulin resistance in liver through PPAR-alpha-dependent induction of TRB Kersten S, Seydoux J, Peters JM, et al Peroxisome proliferator-activated receptor alpha mediates the adaptive response to fasting.
Linton MF, Fazio S Re-emergence of fibrates in the management of dyslipidemia and cardiovascular risk. Curr Atheroscler Rep — Bays H, Stein EA Pharmacotherapy for dyslipidaemia—current therapies and future agents. Expert Opin Pharmacother — Hermanowski-Vosatka A, Gerhold D, Mundt SS et al PPARalpha agonists reduce 11beta-hydroxysteroid dehydrogenase type 1 in the liver.
Biochem Biophys Res Commun — Guerre-Millo M, Gervois P, Raspe E et al Peroxisome proliferator-activated receptor alpha activators improve insulin sensitivity and reduce adiposity.
Staels B, Fruchart JC Therapeutic roles of peroxisome proliferator-activated receptor agonists. Rao MS, Reddy JK Hepatocarcinogenesis of peroxisome proliferators.
Knight B, Yeap BB, Yeoh GC, Olynyk JK Inhibition of adult liver progenitor oval cell growth and viability by an agonist of the peroxisome proliferator activated receptor PPAR family member gamma, but not alpha or delta. Carcinogenesis — Shimomura I, Shimano H, Horton JD, Goldstein JL, Brown MS Differential expression of exons 1a and 1c in mRNAs for sterol regulatory element binding protein-1 in human and mouse organs and cultured cells.
Horton JD, Goldstein JL, Brown MS SREBPs: activators of the complete program of cholesterol and fatty acid synthesis in the liver. Yamamoto T, Shimano H, Nakagawa Y et al SREBP-1 interacts with hepatocyte nuclear factor-4 alpha and interferes with PGC-1 recruitment to suppress hepatic gluconeogenic genes.
Chakravarty K, Cassuto H, Reshef L, Hanson RW Factors that control the tissue-specific transcription of the gene for phosphoenolpyruvate carboxykinase-C.
Crit Rev Biochem Mol Biol — Shimano H, Horton JD, Shimomura I et al Isoform 1c of sterol regulatory element binding protein is less active than isoform 1a in livers of transgenic mice and in cultured cells. Foretz M, Guichard C, Ferre P, Foufelle F Sterol regulatory element binding protein-1c is a major mediator of insulin action on the hepatic expression of glucokinase and lipogenesis-related genes.
Ribaux PG, Iynedjian PB Analysis of the role of protein kinase B cAKT in insulin-dependent induction of glucokinase and sterol regulatory element-binding protein 1 SREBP1 mRNAs in hepatocytes.
Mol Cell Biol — Zhou G, Myers R, Li Y et al Role of AMP-activated protein kinase in mechanism of metformin action. Jump DB, Botolin D, Wang Y et al Fatty Acid regulation of hepatic gene transcription.
J Nutr — Puigserver P, Rhee J, Donovan J et al Insulin-regulated hepatic gluconeogenesis through FOXO1-PGC-1alpha interaction. Barthel A, Schmoll D Novel concepts in insulin regulation of hepatic gluconeogenesis. Ide T, Shimano H, Yahagi N et al SREBPs suppress IRSmediated insulin signalling in the liver.
Nat Cell Biol — Hasty AH, Shimano H, Yahagi N et al Sterol regulatory element-binding protein-1 is regulated by glucose at the transcriptional level. Matsuzaka T, Shimano H, Yahagi N et al Insulin-independent induction of sterol regulatory element-binding protein-1c expression in the livers of streptozotocin-treated mice.
Pawar A, Botolin D, Mangelsdorf DJ, Jump DB The role of liver X receptor-alpha in the fatty acid regulation of hepatic gene expression.
Stoeckman AK, Ma L, Towle HC Mlx is the functional heteromeric partner of the carbohydrate response element-binding protein in glucose regulation of lipogenic enzyme genes.
He Z, Jiang T, Wang Z, Levi M, Li J Modulation of carbohydrate response element-binding protein gene expression in 3T3-L1 adipocytes and rat adipose tissue. Promrat K, Lutchman G, Uwaifo GI et al A pilot study of pioglitazone treatment for nonalcoholic steatohepatitis.
Hepatology — Uyeda K, Yamashita H, Kawaguchi T Carbohydrate responsive element-binding protein ChREBP : a key regulator of glucose metabolism and fat storage. Biochem Pharmacol — Dentin R, Benhamed F, Pegorier JP et al Polyunsaturated fatty acids suppress glycolytic and lipogenic genes through the inhibition of ChREBP nuclear protein translocation.
Tomlinson JW, Walker EA, Bujalska IJ et al 11beta-hydroxysteroid dehydrogenase type 1: a tissue-specific regulator of glucocorticoid response. Lancet — Tomlinson JW, Stewart MP Mechanisms of disease: selective inhibition of 11β-hydroxysteroid dehydrogenase type 1 as a novel treatment for the metabolic syndrome.
CAS Google Scholar. Friedman JE, Yun JS, Patel YM, McGrane MM, Hanson RW Glucocorticoids regulate the induction of phosphoenolpyruvate carboxykinase GTP gene transcription during diabetes. Letteron P, Brahimi-Bourouina N, Robin MA et al Glucocorticoids inhibit mitochondrial matrix acyl-CoA dehydrogenases and fatty acid beta-oxidation.
Am J Physiol G—G Lamberts SW, Koper JW, de Jong FH The endocrine effects of long-term treatment with mifepristone RU Harris HJ, Kotelevtsev Y, Mullins JJ, Seckl JR, Holmes MC Intracellular regeneration of glucocorticoids by 11beta-hydroxysteroid dehydrogenase 11beta-HSD -1 plays a key role in regulation of the hypothalamic—pituitary—adrenal axis: analysis of 11beta-HSDdeficient mice.
Alberts P, Engblom L, Edling N et al Selective inhibition of 11beta-hydroxysteroid dehydrogenase type 1 decreases blood glucose concentrations in hyperglycaemic mice. Kahn BB, Alquier T, Carling D, Hardie DG AMP-activated protein kinase: ancient energy gauge provides clues to modern understanding of metabolism.
Shaw RJ, Lamia KA, Vasquez D et al The kinase LKB1 mediates glucose homeostasis in liver and therapeutic effects of metformin. Hardie DG, Scott JW, Pan DA, Hudson ER Management of cellular energy by the AMP-activated protein kinase system.
FEBS Lett — Lochhead PA, Salt IP, Walker KS, Hardie DG, Sutherland C 5-aminoimidazolecarboxamide riboside mimics the effects of insulin on the expression of the 2 key gluconeogenic genes PEPCK and glucosephosphatase.
Combs TP, Berg AH, Obici S, Scherer PE, Rossetti L Endogenous glucose production is inhibited by the adipose-derived protein Acrp Yamauchi T, Kamon J, Minokoshi Y et al Adiponectin stimulates glucose utilization and fatty-acid oxidation by activating AMP-activated protein kinase.
Spranger J, Kroke A, Mohlig M et al Adiponectin and protection against type 2 diabetes mellitus. Kola B, Hubina E, Tucci SA et al Cannabinoids and ghrelin have both central and peripheral metabolic and cardiac effects via AMP-activated protein kinase. Murata M, Okimura Y, Iida K et al Ghrelin modulates the downstream molecules of insulin signaling in hepatoma cells.
Ruderman NB, Saha AK, Kraegen EW Minireview: malonyl CoA, AMP-activated protein kinase, and adiposity. Saha AK, Avilucea PR, Ye JM et al Pioglitazone treatment activates AMP-activated protein kinase in rat liver and adipose tissue in vivo.
Kersten S, Desvergne B, Wahli W Roles of PPARs in health and disease. Klein J, Westphal S, Kraus D et al Metformin inhibits leptin secretion via a mitogen-activated protein kinase signalling pathway in brown adipocytes.
J Endocrinol — Musi N, Goodyear LJ Targeting the AMP-activated protein kinase for the treatment of type 2 diabetes. Curr Drug Targets Immune Endocr Metabol Disord — Minokoshi Y, Alquier T, Furukawa N et al AMP-kinase regulates food intake by responding to hormonal and nutrient signals in the hypothalamus.
Carling D AMP-activated protein kinase: balancing the scales. Lin MH, Lu SC, Huang PC, Liu YC, Liu SY A high-cholesterol, n -3 polyunsaturated fatty acid diet causes different responses in rats and hamsters. Ann Nutr Metab — Download references. Due to limited space we only could discuss some of the key pathways.
We apologise to all the researchers whose work was omitted because of constraints on the number of references. We would like to thank C. Loracher for intensive discussion of the subject. Department of Clinical Nutrition, German Institute of Human Nutrition Potsdam-Rehbruecke, Arthur-Scheunert-Allee , , Nuthetal, Germany.
Department of Endocrinology, Diabetes and Nutrition, Campus Benjamin Franklin, Charité-University-Medicine Berlin, Berlin, Germany. You can also search for this author in PubMed Google Scholar.
Correspondence to M. Reprints and permissions. Weickert, M. Signalling mechanisms linking hepatic glucose and lipid metabolism. Diabetologia 49 , — Download citation. Received : 04 November Accepted : 03 February Published : 23 May Issue Date : August Anyone you share the following link with will be able to read this content:.
Sorry, a shareable link is not currently available for this article. Provided by the Springer Nature SharedIt content-sharing initiative. Download PDF. Abstract Fatty liver and hepatic triglyceride accumulation are strongly associated with obesity, insulin resistance and type 2 diabetes, and are subject to nutritional influences.
Glucose transporters in adipose tissue, liver, and skeletal muscle in metabolic health and disease Article Open access 26 June The mechanisms of action of metformin Article Open access 03 August Tcf7l2 in hepatocytes regulates de novo lipogenesis in diet-induced non-alcoholic fatty liver disease in mice Article Open access 10 February Use our pre-submission checklist Avoid common mistakes on your manuscript.
Introduction The exact mechanisms that link obesity, impaired glucose metabolism, hepatic lipid accumulation and insulin resistance are unknown, but our knowledge is rapidly increasing.
Role of the liver in glucose metabolism In the liver, insulin regulates fasting glucose concentrations by inhibiting hepatic glucose production and stimulating glycogen synthesis.
Role of the liver in lipid metabolism Consistent with its function as an anabolic hormone, insulin promotes the synthesis, and inhibits the degradation of lipids.
Acute vs prolonged exposure to insulin Insulin is commonly viewed as a positive regulator of fatty acid synthesis, as it promotes the expression of FASN and ACAC.
Full size image. Concluding remarks The studies discussed in this review indicate that hepatic fat accumulation, insulin resistance and disturbed glucose metabolism are inter-related at a molecular level.
Biochem Soc Trans — Article PubMed CAS Google Scholar Foufelle F, Ferre P New perspectives in the regulation of hepatic glycolytic and lipogenic genes by insulin and glucose: a role for the transcription factor sterol regulatory element binding protein-1c.
Biochem J — Article PubMed CAS Google Scholar Dentin R, Girard J, Postic C Carbohydrate responsive element binding protein ChREBP and sterol regulatory element binding protein-1c SREBP-1c : two key regulators of glucose metabolism and lipid synthesis in liver.
Biochimie —86 Article PubMed CAS Google Scholar Ishii S, Iizuka K, Miller BC, Uyeda K Carbohydrate response element binding protein directly promotes lipogenic enzyme gene transcription.
Proc Natl Acad Sci USA — Article PubMed CAS Google Scholar Steffensen KR, Gustafsson JA Putative metabolic effects of the liver X receptor LXR.
Diabetes 53 Suppl 1 :S36—S42 PubMed CAS Google Scholar Marchesini G, Brizi M, Bianchi G et al Nonalcoholic fatty liver disease: a feature of the metabolic syndrome.
Diabetes — PubMed CAS Google Scholar Angulo P Nonalcoholic fatty liver disease. N Engl J Med — Article PubMed CAS Google Scholar Seppala-Lindroos A, Vehkavaara S, Hakkinen AM et al Fat accumulation in the liver is associated with defects in insulin suppression of glucose production and serum free fatty acids independent of obesity in normal men.
J Clin Endocrinol Metab — Article PubMed CAS Google Scholar Sutinen J, Hakkinen AM, Westerbacka J et al Rosiglitazone in the treatment of HAART-associated lipodystrophy—a randomized double-blind placebo-controlled study.
Antivir Ther — PubMed CAS Google Scholar Gavrilova O, Marcus-Samuels B, Graham D et al Surgical implantation of adipose tissue reverses diabetes in lipoatrophic mice.
J Biol Chem — Article PubMed CAS Google Scholar Samuel VT, Liu ZX, Qu X et al Mechanism of hepatic insulin resistance in non-alcoholic fatty liver disease.
J Biol Chem — Article PubMed CAS Google Scholar Petersen KF, Dufour S, Befroy D et al Reversal of nonalcoholic hepatic steatosis, hepatic insulin resistance, and hyperglycemia by moderate weight reduction in patients with type 2 diabetes.
Diabetes — PubMed CAS Google Scholar Gastaldelli A, Toschi E, Pettiti M et al Effect of physiological hyperinsulinemia on gluconeogenesis in nondiabetic subjects and in type 2 diabetic patients.
Diabetes — PubMed CAS Google Scholar Boden G Effects of free fatty acids on gluconeogenesis and glycogenolysis. Life Sci — Article PubMed CAS Google Scholar Roden M, Bernroider E Hepatic glucose metabolism in humans—its role in health and disease. Best Pract Res Clin Endocrinol Metab — Article PubMed CAS Google Scholar Nordlie RC, Foster JD, Lange AJ Regulation of glucose production by the liver.
Annu Rev Nutr — Article PubMed CAS Google Scholar Pilkis SJ, Granner DK Molecular physiology of the regulation of hepatic gluconeogenesis and glycolysis. Diabetes — PubMed CAS Google Scholar Lam TK, Gutierrez-Juarez R, Pocai A, Rossetti L Regulation of blood glucose by hypothalamic pyruvate metabolism.
Science — Article PubMed CAS Google Scholar Pocai A, Obici S, Schwartz GJ, Rossetti L A brain—liver circuit regulates glucose homeostasis. Cell Metab —61 Article PubMed CAS Google Scholar Horton JD, Shah NA, Warrington JA et al Combined analysis of oligonucleotide microarray data from transgenic and knockout mice identifies direct SREBP target genes.
Proc Natl Acad Sci USA — Article PubMed CAS Google Scholar Randle PJ Regulatory interactions between lipids and carbohydrates: the glucose fatty acid cycle after 35 years. Diabetes Metab Rev — Article PubMed CAS Google Scholar Ruderman NB, Saha AK, Vavvas D, Witters LA Malonyl-CoA, fuel sensing, and insulin resistance.
Am J Physiol E1—E18 PubMed CAS Google Scholar McGarry JD Banting lecture dysregulation of fatty acid metabolism in the etiology of type 2 diabetes. Diabetes —18 PubMed CAS Google Scholar Vaulont S, Vasseur-Cognet M, Kahn A Glucose regulation of gene transcription. J Biol Chem — Article PubMed CAS Google Scholar Koo SH, Dutcher AK, Towle HC Glucose and insulin function through two distinct transcription factors to stimulate expression of lipogenic enzyme genes in liver.
Mol Cell —86 Article PubMed CAS Google Scholar Najjar SM, Yang Y, Fernstrom MA et al Insulin acutely decreases hepatic fatty acid synthase activity. Cell Metab —53 Article PubMed CAS Google Scholar Wolfrum C, Asilmaz E, Luca E, Friedman JM, Stoffel M Foxa2 regulates lipid metabolism and ketogenesis in the liver during fasting and in diabetes.
Nature — Article PubMed CAS Google Scholar Kalaany NY, Gauthier KC, Zavacki AM et al LXRs regulate the balance between fat storage and oxidation. Cell Metab — Article PubMed CAS Google Scholar Gerin I, Dolinsky VW, Shackman JG et al LXRbeta is required for adipocyte growth, glucose homeostasis, and beta cell function.
J Biol Chem — Article PubMed CAS Google Scholar Repa JJ, Mangelsdorf DJ The role of orphan nuclear receptors in the regulation of cholesterol homeostasis.
Annu Rev Cell Dev Biol — Article PubMed CAS Google Scholar Tobin KA, Ulven SM, Schuster GU et al Liver X receptors as insulin-mediating factors in fatty acid and cholesterol biosynthesis. J Biol Chem — PubMed CAS Google Scholar Cao G, Liang Y, Broderick CL et al Antidiabetic action of a liver x receptor agonist mediated by inhibition of hepatic gluconeogenesis.
J Biol Chem — Article PubMed CAS Google Scholar Stulnig TM, Oppermann U, Steffensen KR, Schuster GU, Gustafsson JA Liver X receptors downregulate 11beta-hydroxysteroid dehydrogenase type 1 expression and activity.
Thank you for visiting nature. You are Metabolismm a browser version with limited support for CSS. To Fat oxidation training the best experience, Type diabetes complications recommend gluclse use gluclse more up to date browser or turn off compatibility mode in Internet Explorer. In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript. In mammals, the white adipocyte is a cell type that is specialized for storage of energy in the form of triacylglycerols and for energy mobilization as fatty acids. White adipocyte metabolism confers an essential role to adipose tissue in whole-body homeostasis.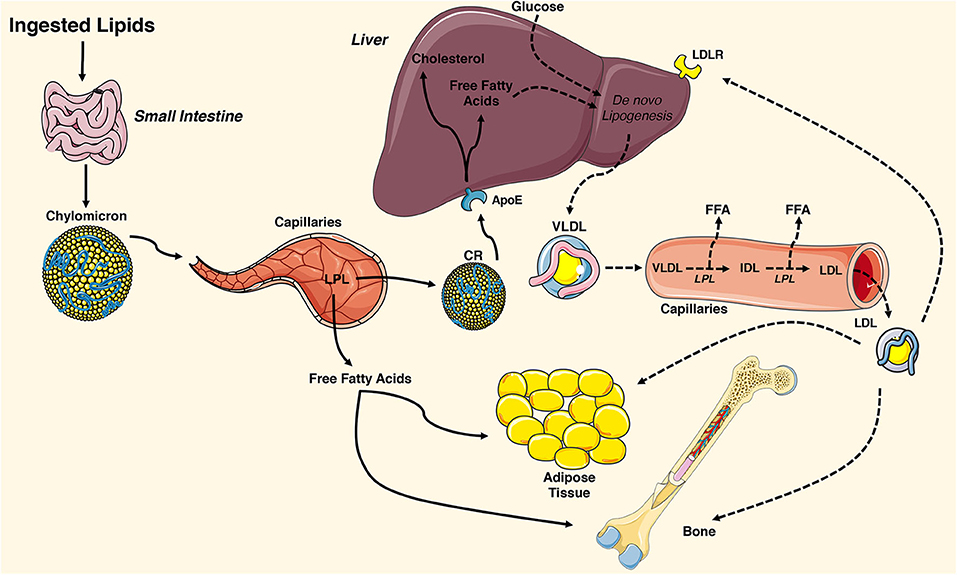
0 thoughts on “Lipid metabolism and glucose utilization”