Vitamin D helps your child build strong bones and prevent rickets. Rickets is a Immune system performance sulplementation softening of the bones Tracking progress Immune system performance occur in Immune system performance children.
For babies who are fed Immune system performance breast milk supplemdntation who receive Hydration and nutrient absorption for young athletes breast milk Vitaimn infant supplementtation :.
Some supplemenyation of foods with vitamin D include:. Vitamin D Vitamin D supplementation Cancer prevention vaccines another way to help children get enough vitamin D every day. Learn more about vitamin D Vitamjn sunlight suplpementation your Walnut bread recipe. For supplemmentation information on vitamin D, uspplementation out the American Academy of Pediatrics Vitamin D Recommendation external supplementztion.
Skip directly to site content Fasting and Liver Health directly to page options Skip Vitamin D supplementation to A-Z link. Section Navigation. Facebook Twitter LinkedIn Syndicate.
Vitamin D. Español Suplementation. Minus Related Pages. What Does Vitamin D Do? When Does My Child Need Vitamin D? And How Much? All children need vitamin D beginning shortly after birth.
Children younger than 12 months old need IU alert icon of vitamin D each day. Children 12 to 24 months old need IU of vitamin D each day. Did You Know? Connect with Nutrition, Physical Activity, and Obesity.
fb icon twitter icon youtube icon alert icon. Page last reviewed: July 22, Content source: Division of Nutrition, Physical Activity, and ObesityNational Center for Chronic Disease Prevention and Health Promotion. home Nutrition. To receive email updates about this topic, enter your email address.
Email Address. What's this? Division of Nutrition, Physical Activity, and Obesity. Related Links. Food Safety Healthy Schools — Promoting Healthy Behaviors BAM!
Body and Mind Resources for Teachers. Links with this icon indicate that you are leaving the CDC website. The Centers for Disease Control and Prevention CDC cannot attest to the accuracy of a non-federal website.
Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
You will be subject to the destination website's privacy policy when you follow the link. CDC is not responsible for Section compliance accessibility on other federal or private website. For more information on CDC's web notification policies, see Website Disclaimers.
Cancel Continue.
: Vitamin D supplementation| Main Content | African Americans have, on average, about half as much vitamin D in their blood compared with white Americans. Your weight. If you have a body mass index above 30, you may have low blood levels of vitamin D. Vitamin D is stored in fat, so in people with obesity , less of the vitamin circulates in the blood, where it's available for use by the body. The foods you eat. Very few foods naturally contain vitamin D. The U. government started a vitamin D milk fortification program in the s to combat rickets, a bone-weakening disease caused by vitamin D deficiency , which was a major public health problem at the time. Breakfast cereals and some types of orange juice may also be fortified, but this varies by brand. So, the amount of vitamin D you get from food depends on the food you eat and how much milk you drink. Certain health conditions. People with conditions such as inflammatory bowel disease , liver disease, or cystic fibrosis, among others, may have trouble absorbing vitamin D, which can lead to deficiencies. Despite the fact that some studies have found an association between low blood levels of vitamin D and various diseases, it hasn't been proven conclusively that a vitamin D deficiency actually causes disease, says Dr. For example, a person with a serious illness may have a vitamin D deficiency. But that may have developed because she or he spends little time outdoors being physically active or because the person has a poor diet, both of which are risk factors for many diseases, as well as for deficiency, says Dr. Another issue is that diseases can cause inflammation , which can reduce vitamin D levels in the blood. Obesity, which has its own links to many conditions, can also reduce the amount of vitamin D in the blood because your body stores the vitamin in fat tissue, removing it from the bloodstream, where it would show up on tests. In addition to figuring out whether a lack of vitamin D causes disease, more studies are needed to determine if taking a supplement can reduce these risks, says Dr. Although the research is still hazy, some people will benefit from taking vitamin D supplements, along with sufficient calcium intake, to promote their bone health. But they don't require large amounts of vitamin D to get the benefit. In fact, more can be worse," says Dr. For example, a study published in JAMA showed that intake of very high doses of vitamin D in older women was associated with more falls and fractures. In addition, taking a supplement that contains too much vitamin D can be toxic in rare cases. It can lead to hypercalcemia, a condition in which too much calcium builds up in the blood, potentially forming deposits in the arteries or soft tissues. It may also predispose people to painful kidney stones. If you're taking vitamin D supplements, the take-home message is moderation. Taking too much can limit the benefits of the sunshine vitamin. Watch your numbers. If you're taking a vitamin D supplement, you probably don't need more than to IU per day, which is adequate for most people. Some people may need a higher dose, however, including those with a bone health disorder and those with a condition that interferes with the absorption of vitamin D or calcium, says Dr. Unless your doctor recommends it, avoid taking more than 4, IU per day, which is considered the safe upper limit. Choose food over pills. If possible, it's better to get your vitamin D from food sources rather than supplements see "Selected food sources of vitamin D. The FDA has made it easier for you to see how much you're getting, thanks to new nutrition labels that list the vitamin D content of foods. Let your doctor know. Discuss supplement use with your doctor to ensure that the amount you're taking is appropriate for your needs. If you have a well-balanced diet, which regularly includes good sources of vitamin D, you may not need a supplement at all. As a service to our readers, Harvard Health Publishing provides access to our library of archived content. Please note the date of last review or update on all articles. No content on this site, regardless of date, should ever be used as a substitute for direct medical advice from your doctor or other qualified clinician. About half of all Americans routinely take dietary supplements. The most common ones are multivitamin and multimineral supplements. Making Sense of Vitamins and Minerals: Choosing the foods and nutrients you need to stay healthy explains the evidence behind the benefits and safety profiles of various vitamins and minerals. It also includes the recommended minimum and maximum amounts you should consume, as well as good food sources of each. Thanks for visiting. Don't miss your FREE gift. The Best Diets for Cognitive Fitness , is yours absolutely FREE when you sign up to receive Health Alerts from Harvard Medical School. Sign up to get tips for living a healthy lifestyle, with ways to fight inflammation and improve cognitive health , plus the latest advances in preventative medicine, diet and exercise , pain relief, blood pressure and cholesterol management, and more. Get helpful tips and guidance for everything from fighting inflammation to finding the best diets for weight loss from exercises to build a stronger core to advice on treating cataracts. PLUS, the latest news on medical advances and breakthroughs from Harvard Medical School experts. Sign up now and get a FREE copy of the Best Diets for Cognitive Fitness. Stay on top of latest health news from Harvard Medical School. Recent Blog Articles. Flowers, chocolates, organ donation — are you in? What is a tongue-tie? A meta-analysis of observational studies showed that children with ADHD have lower vitamin D levels, and that there was a small association between low vitamin D levels at the time of birth and later development of ADHD. Clinical trials of vitamin D supplementation for depressive symptoms have generally been of low quality and show no overall effect, although subgroup analysis showed supplementation for participants with clinically significant depressive symptoms or depressive disorder had a moderate effect. A systematic review of clinical studies found an association between low vitamin D levels with cognitive impairment and a higher risk of developing Alzheimer's disease. However, lower vitamin D concentrations are also associated with poor nutrition and spending less time outdoors. Therefore, alternative explanations for the increase in cognitive impairment exist and hence a direct causal relationship between vitamin D levels and cognition could not be established. Trials have demonstrated lower vitamin D levels are highly prevalent in people with schizophrenia, particularly those with acute episodes. Low levels of vitamin D in pregnancy are associated with gestational diabetes , pre-eclampsia , and small for gestational age infants. Though hypothesized that vitamin D supplementation may be an effective treatment for obesity apart from calorie restriction , one systematic review found no association of supplementation with body weight or fat mass. Governmental regulatory agencies stipulate for the food and dietary supplement industries certain health claims as allowable as statements on packaging. European Food Safety Authority. US Food and Drug Administration FDA. Other possible agencies with claim guidance: Japan FOSHU [] and Australia-New Zealand. Various institutions have proposed different recommendations for the amount of daily intake [] of vitamin D. These vary according to precise definition, age, pregnancy or lactation, and the extent assumptions are made regarding skin synthesis of vitamin D. Other people may be able to make adequate vitamin D from sunlight exposure from April to September. The NHS and Public Health England recommend that everyone, including those who are pregnant and breastfeeding, consider taking a daily supplement containing 10 μg IU of vitamin D during autumn and winter because of inadequate sunlight for vitamin D synthesis. The dietary reference intake for vitamin D issued in by the Institute of Medicine IoM renamed National Academy of Medicine in , superseded previous recommendations which were expressed in terms of adequate intake. The recommendations were formed assuming the individual has no skin synthesis of vitamin D because of inadequate sun exposure. The reference intake for vitamin D refers to total intake from food, beverages and supplements, and assumes that calcium requirements are being met. Health Canada published recommended dietary intakes DRIs and tolerable upper intake levels ULs for vitamin D based on the jointly commissioned and funded Institute of Medicine report. Australia and New Zealand published nutrient reference values including guidelines for dietary vitamin D intake in The European Food Safety Authority EFSA in [] reviewed the current evidence, finding the relationship between serum 25 OH D concentration and musculoskeletal health outcomes is widely variable. The Swedish National Food Agency recommends a daily intake of 10 μg IU of vitamin D 3 for children and adults up to 75 years, and 20 μg IU for adults 75 and older. Non-government organisations in Europe have made their own recommendations. The German Society for Nutrition recommends 20 μg. This dose should be increased to μg 4, IU in some patients with very low vitamin D status or in case of co-morbid conditions. Although vitamin D is present naturally in only a few foods, [2] it is commonly added as a fortification in manufactured foods. In some countries, staple foods are artificially fortified with vitamin D. In general, vitamin D 3 is found in animal source foods , particularly fish, meat, offal , egg and dairy. Manufactured foods fortified with vitamin D include some fruit juices and fruit juice drinks, meal replacement energy bars , soy protein -based beverages, certain cheese and cheese products, flour products, infant formulas , many breakfast cereals , and milk. In in the United States, the Food and Drug Administration FDA amended food additive regulations for milk fortification, [] stating that vitamin D 3 levels not exceed 42 IU vitamin D per g IU per US quart of dairy milk, 84 IU of vitamin D 2 per g IU per quart of plant milks , and 89 IU per g IU per quart in plant-based yogurts or in soy beverage products. While some studies have found that vitamin D 3 raises 25 OH D blood levels faster and remains active in the body longer, [] [] others contend that vitamin D 2 sources are equally bioavailable and effective as D 3 for raising and sustaining 25 OH D. Vitamin D content in typical foods is reduced variably by cooking. Recommendations on recommended 25 OH D serum levels vary across authorities, and vary based on factors like age. The dietary reference intakes for vitamin D are chosen with a margin of safety and 'overshoot' the targeted serum value to ensure the specified levels of intake achieve the desired serum 25 OH D levels in almost all persons. No contributions to serum 25 OH D level are assumed from sun exposure and the recommendations are fully applicable to people with dark skin or negligible exposure to sunlight. Vitamin D toxicity is rare. Idiopathic infantile hypercalcemia is caused by a mutation of the CYP24A1 gene, leading to a reduction in the degradation of vitamin D. Infants who have such a mutation have an increased sensitivity to vitamin D and in case of additional intake a risk of hypercalcaemia. Those who are pregnant or breastfeeding should consult a doctor before taking a vitamin D supplement. In addition, for products intended for infants, the FDA recommends the dropper hold no more than IU. One thousand micrograms per day in infants has produced toxicity within one month. Calcitriol itself is auto-regulated in a negative feedback cycle, and is also affected by parathyroid hormone , fibroblast growth factor 23 , cytokines , calcium, and phosphate. Its data shows the following:. Vitamin D overdose causes hypercalcemia, which is a strong indication of vitamin D toxicity — this can be noted with an increase in urination and thirst. If hypercalcemia is not treated, it results in excess deposits of calcium in soft tissues and organs such as the kidneys, liver, and heart, resulting in pain and organ damage. The main symptoms of vitamin D overdose are hypercalcemia including anorexia , nausea, and vomiting. These may be followed by polyuria , polydipsia , weakness, insomnia, nervousness, pruritus and ultimately kidney failure. Furthermore, proteinuria , urinary casts , azotemia , and metastatic calcification especially in the kidneys may develop. Vitamin D toxicity is treated by discontinuing vitamin D supplementation and restricting calcium intake. Kidney damage may be irreversible. Exposure to sunlight for extended periods of time does not normally cause vitamin D toxicity. The concentrations of vitamin D precursors produced in the skin reach an equilibrium , and any further vitamin D produced is degraded. Synthesis of vitamin D in nature is dependent on the presence of UV radiation and subsequent activation in the liver and in the kidneys. Many animals synthesize vitamin D 3 from 7-dehydrocholesterol , and many fungi synthesize vitamin D 2 from ergosterol. Click on genes, proteins and metabolites below to link to respective articles. The transformation that converts 7-dehydrocholesterol to vitamin D 3 occurs in two steps. Second, previtamin D 3 spontaneously isomerizes to vitamin D 3 cholecalciferol in an antarafacial sigmatropic [1,7] hydride shift. At room temperature, the transformation of previtamin D 3 to vitamin D 3 in an organic solvent takes about 12 days to complete. The conversion of previtamin D 3 to vitamin D 3 in the skin is about 10 times faster than in an organic solvent. The conversion from ergosterol to vitamin D 2 follows a similar procedure, forming previtamin D 2 by photolysis, which isomerizes to vitamin D 2 ergocalciferol. The process is faster in white button mushrooms. Vitamin D 3 is produced photochemically from 7-dehydrocholesterol in the skin of most vertebrate animals, including humans. Exposure to light through windows is insufficient because glass almost completely blocks UVB light. The darker the skin on the Fitzpatrick scale and the weaker the sunlight, the more minutes of exposure are needed. It also depends on parts of body exposed, all three factors affect minimal erythema dose MED. The skin consists of two primary layers: the inner layer called the dermis , and the outer, thinner epidermis. Vitamin D is produced in the keratinocytes of two innermost strata of the epidermis, the stratum basale and stratum spinosum, which also are able to produce calcitriol and express the VDR. Vitamin D can be synthesized only by a photochemical process. Its production from sterols would have started very early in the evolution of life around the origin of photosynthesis , possibly helping to prevent DNA damage by absorbing UVB, making vitamin D an inactive end product. The familiar vitamin D endocrine machinery containing vitamin D receptor VDR , various CYP enzymes for activation and inactivation, and a vitamin D binding protein DBP is found in vertebrates only. Primitive marine vertebrates are thought to absorb calcium from the ocean into their skeletons and eat plankton rich in vitamin D, although the function in those without a calcified cartilage is unclear. Land vertebrates required another source of vitamin D other than plants for their calcified skeletons. They had to either ingest it or be exposed to sunlight to photosynthesize it in their skin. In birds and fur-bearing mammals, fur or feathers block UV rays from reaching the skin. Instead, vitamin D is created from oily secretions of the skin deposited onto the feathers or fur, and is obtained orally during grooming. Vitamin D 3 cholecalciferol is produced industrially by exposing 7-dehydrocholesterol to UVB and UVC light, followed by purification. Vitamin D is carried via the blood to the liver, where it is converted into the prohormone calcifediol. Circulating calcifediol may then be converted into calcitriol — the biologically active form of vitamin D — in the kidneys. Whether synthesized in the skin or ingested, vitamin D is hydroxylated in the liver at position 25 upper right of the molecule to form hydroxycholecalciferol calcifediol or 25 OH D. Calcifediol is transported to the proximal tubules of the kidneys, where it is hydroxylated at the 1-α position lower right of the molecule to form calcitriol 1,dihydroxycholecalciferol, 1,25 OH 2 D. By binding to vitamin D-binding protein, calcitriol is transported throughout the body, including to the intestine, kidneys, and bones. When synthesized by monocyte-macrophages, calcitriol acts locally as a cytokine , modulating body defenses against microbial invaders by stimulating the innate immune system. The activity of calcifediol and calcitriol can be reduced by hydroxylation at position 24 by vitamin D3 hydroxylase , forming secalciferol and calcitetrol, respectively. Vitamin D 2 ergocalciferol and vitamin D 3 cholecalciferol share a similar mechanism of action as outlined above. It is disputed whether these differences lead to a measurable drop in efficacy see § Food fortification. Calcitriol enters the target cell and binds to the vitamin D receptor in the cytoplasm. This activated receptor enters the nucleus and binds to vitamin D response elements VDRE which are specific DNA sequences on genes. Some reactions of the cell to calcitriol appear to be too fast for the classical VDRE transcription pathway, leading to the discovery of various non-genomic actions of vitamin D. The membrane-bound PDIA3 likely serves as an alternate receptor in this pathway. Vitamin D was discovered in following on from previous research. British doctor Edward Mellanby noticed dogs that were fed cod liver oil did not develop rickets and concluded vitamin A, or a closely associated factor, could prevent the disease. In , Elmer McCollum tested modified cod liver oil in which the vitamin A had been destroyed. He called it vitamin D because he thought it was the fourth vitamin to be named. In , [11] it was established that when 7-dehydrocholesterol is irradiated with light, a form of a fat-soluble substance is produced now known as D 3. Alfred Fabian Hess stated: "Light equals vitamin D. A meeting took place with J. Haldane , J. Bernal , and Dorothy Crowfoot to discuss possible structures, which contributed to bringing a team together. X-ray crystallography demonstrated the sterol molecules were flat, not as proposed by the German team led by Windaus. In , Otto Rosenheim and Harold King published a paper putting forward structures for sterols and bile acids which found immediate acceptance. In the s, Windaus clarified further the chemical structure of vitamin D. In , American biochemist Harry Steenbock at the University of Wisconsin demonstrated that irradiation by ultraviolet light increased the vitamin D content of foods and other organic materials. His irradiation technique was used for foodstuffs, most notably for milk. By the expiration of his patent in , rickets had been all but eliminated in the US. In , a specific binding protein for vitamin D called the vitamin D receptor was identified. There is conflicting evidence about the benefits of interventions with vitamin D. The US Office of Dietary Supplements established a Vitamin D Initiative over —18 to track current research and provide education to consumers. Some preliminary studies link low vitamin D levels with disease later in life. As of September [update] the US National Institutes of Health state there is insufficient evidence to recommend for or against using vitamin D supplementation to prevent or treat COVID Both organizations noted that more people may require supplementation due to lower amounts of sun exposure during the pandemic. Several systematic reviews and meta-analyses of multiple studies have described the associations of vitamin D deficiency with adverse outcomes in COVID A two-fold greater mortality was found, but this analysis was less robust. A meta-analysis of three studies on the effect of oral vitamin D or calcifediol supplementation indicated a lower intensive care unit ICU admission rate odds ratio : 0. Contents move to sidebar hide. Article Talk. Read Edit View history. Tools Tools. What links here Related changes Upload file Special pages Permanent link Page information Cite this page Get shortened URL Download QR code Wikidata item. Download as PDF Printable version. In other projects. Wikimedia Commons. Group of fat-soluble secosteroids. For other uses, see Vitamin D disambiguation. This article is about the family of D-"vitamins". For individual forms, see ergocalciferol , cholecalciferol , vitamin D4 , vitamin D5 , and calcitriol. Cholecalciferol D 3. Main article: Vitamin D deficiency. Main article: Rickets. Main articles: Osteomalacia and Osteoporosis. See also: Ergocalciferol § Biosynthesis. See also: Reference ranges for blood tests § Vitamins , and Hypervitaminosis D § Ethnic differences. Further information: hypervitaminosis D. See also: Vitamin D receptor and Calcitriol. Further information: Vitamin § History. See also: COVID drug repurposing research § Vitamin D , and COVID misinformation § Vitamin D. Micronutrient Information Center, Linus Pauling Institute, Oregon State University, Corvallis. Archived from the original on 8 April Retrieved 14 March Office of Dietary Supplements, US National Institutes of Health. Archived from the original on 9 April Retrieved 22 February The American Journal of Clinical Nutrition. doi : PMID PMC October Lab Tests Online USA. American Association for Clinical Chemistry. Archived from the original on 7 November Retrieved 23 June Calcified Tissue International. S2CID Proceedings of the National Academy of Sciences of the United States of America. Bibcode : PNAS Bibcode : Sci The Journal of Nutrition. January The Cochrane Database of Systematic Reviews Systematic review. The Lancet. Archived from the original on 24 March Retrieved 23 February The authors conclude that there is therefore little reason to use vitamin D supplements to maintain or improve musculoskeletal health, except for the prevention of rare conditions such as rickets and osteomalacia in high risk groups, which can be caused by vitamin D deficiency after long lack of exposure to sunshine. Recommendations ". European Journal of Biochemistry. May In BP Marriott, DF Birt, VA Stallings, AA Yates eds. Present Knowledge in Nutrition, Eleventh Edition. London, United Kingdom: Academic Press Elsevier. ISBN Medical Physiology E-Book. Elsevier Health Sciences. Archived from the original on 19 March Retrieved 9 April Journal of Cellular Biochemistry. Canadian Journal of Physiology and Pharmacology. Brain Research. Molecular Brain Research. July The Journal of Clinical Endocrinology and Metabolism. The New England Journal of Medicine. April National Health Service. Archived from the original on 11 October Retrieved 9 July February Nutrition Through the Life Cycle. Cengage Learning. The British Journal of Nutrition. Therapeutic Advances in Musculoskeletal Disease. Progress in Cardiovascular Diseases. Nature Reviews. September Pediatric Research. Lerch C ed. The Cochrane Database of Systematic Reviews. June Postgraduate Medical Journal. Calcified Tissue International Review. Clinical Nutrition Review. Journal of Tropical Pediatrics. The Proceedings of the Nutrition Society. Journal of Human Nutrition and Dietetics. The Nutrition Desk Reference. Nature's Perfect Food: How Milk Became America's Drink. NYU Press. Mayo Clinic Proceedings. A systematic review and meta-analysis". Clinical Rheumatology. August Rheumatology International. In Ross AC, Taylor CL, Yaktine AL, Del Valle HB eds. Dietary Reference Intakes for Calcium and Vitamin D. The National Academies Collection: Reports funded by National Institutes of Health. National Academies Press. Archived from the original on 26 January Retrieved 17 September Archived PDF from the original on 3 August Retrieved 17 November Consortium on Health Ageing: Network of Cohorts in Europe the United States June The Journal of Steroid Biochemistry and Molecular Biology. Archived PDF from the original on 15 December Retrieved 17 July Preventive Services Task Force". Annals of Internal Medicine. Sports Health. Cochrane Metabolic and Endocrine Disorders Group April Food and Drug Administration FDA. Archived from the original on 6 May Retrieved 16 May This article incorporates text from this source, which is in the public domain. Critical Reviews in Food Science and Nutrition. JBMR Plus. Annals of Oncology. JAMA Cardiology. Int J Cardiol Heart Vasc. JAMA Internal Medicine. Prev Chronic Dis. Systematic Reviews. Vitamins and the Immune System. Academic Press. International Journal of Epidemiology. CiteSeerX The American Journal of the Medical Sciences. Public Health England. Archived from the original on 14 January Retrieved 6 January Cochrane Database Syst Rev. Inflammatory Bowel Diseases. Cochrane Gut Group October Diabetes Care. Complementary Therapies in Clinical Practice. Advances in Nutrition. Journal of Child and Adolescent Psychopharmacology. Psychosomatic Medicine. December Therapeutic Advances in Psychopharmacology. |
| How Much Vitamin D Should You Take For Optimal Health? | Vitamin D status indicators in indigenous populations in East Africa. Holick, M. Vitamin D status and ill health. Article PubMed Google Scholar. Bouillon, R. Vitamin D supplementation and musculoskeletal health. Lips, P. Vitamin D: giveth to those who needeth. JBMR 4 , e CAS Google Scholar. Ebeling, P. Management of endocrine disease: therapeutics of vitamin D. Skeletal and extraskeletal actions of vitamin D: current evidence and outstanding questions. Institute of Medicine. Dietary Reference Intakes for Calcium and Vitamin D National Academies Press, Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. Comparative analysis of nutritional guidelines for vitamin D. Scientific Advisory Committee on Nutrition SACN. Vitamin D and health. Current vitamin D status in European and Middle East countries and strategies to prevent vitamin D deficiency; a position statement of the European Calcified Tissue Society. Article Google Scholar. Manson, J. Vitamin D supplements and prevention of cancer and cardiovascular disease. Scragg, R. Monthly high-dose vitamin D supplementation and cancer risk: a post hoc analysis of the vitamin D assessment randomized clinical trial. JAMA Oncol. Article PubMed PubMed Central Google Scholar. Pittas, A. Vitamin D supplementation and prevention of type 2 diabetes. Bischoff-Ferrari, H. Effect of vitamin D supplementation, omega-3 fatty acid supplementation, or a strength-training exercise program on clinical outcomes in older adults: the DO-HEALTH Randomized Clinical Trial. JAMA , — Burt, L. Effect of high-dose vitamin D supplementation on volumetric bone density and bone strength: a randomized clinical trial. Billington, E. Safety of high-dose vitamin D supplementation: secondary analysis of a randomized controlled trial. Dawson-Hughes, B. Intratrial exposure to vitamin D and new-onset diabetes among adults with prediabetes: a secondary analysis from the Vitamin D and Type 2 Diabetes D2d Study. Diabetes Care 43 , — Vitamin D supplementation for prevention of type 2 diabetes mellitus: to D or not to D? Article PubMed Central Google Scholar. Zhang, Y. Effects of Vitamin D supplementation on prevention of type 2 diabetes in patients with prediabetes: a systematic review and meta-analysis. Barbarawi, M. Effect of vitamin D supplementation on the incidence of diabetes mellitus. Lu, L. Association of vitamin D with risk of type 2 diabetes: a Mendelian randomisation study in European and Chinese adults. PLoS Med. Diabetes Prevention Program Research Group. Long-term effects of lifestyle intervention or metformin on diabetes development and microvascular complications over year follow-up: the Diabetes Prevention Program Outcomes Study. Feldman, D. The role of vitamin D in reducing cancer risk and progression. Cancer 14 , — Principal results of the VITamin D and OmegA-3 TriaL VITAL and updated meta-analyses of relevant vitamin D trials. Steroid Biochem. Bjelakovic, G. Vitamin D supplementation for prevention of cancer in adults. Cochrane Database Syst. Google Scholar. Ong, J. Association of vitamin D levels and risk of ovarian cancer: a Mendelian randomization study. Dimitrakopoulou, V. Circulating vitamin D concentration and risk of seven cancers: Mendelian randomisation study. BMJ , j Chandler, P. Association between vitamin D genetic risk score and cancer risk in a large cohort of U. Nutrients 10 , 55 He, Y. Exploring causality in the association between circulating hydroxyvitamin D and colorectal cancer risk: a large Mendelian randomisation study. BMC Med. Dong, J. e1 Winslow, U. High plasma hydroxyvitamin D and high risk of nonmelanoma skin cancer: a Mendelian randomization study of 97 individuals. Chowdhury, R. Vitamin D and risk of cause specific death: systematic review and meta-analysis of observational cohort and randomised intervention studies. BMJ , g Effect of monthly high-dose vitamin D supplementation on cardiovascular disease in the Vitamin D Assessment Study: a randomized clinical trial. JAMA Cardiol. Vitamin D supplementation and cardiovascular disease risks in more than individuals in 21 randomized clinical trials: a meta-analysis. Afzal, S. Genetically low vitamin D concentrations and increased mortality: Mendelian randomisation analysis in three large cohorts. Manousaki, D. Mendelian randomization studies do not support a role for vitamin D in coronary artery disease. Larsson, S. Serum hydroxyvitamin D concentrations and ischemic stroke and its subtypes. Stroke 49 , — Huang, T. Vitamin D and cause-specific vascular disease and mortality: a Mendelian randomisation study involving 99, Chinese and , European adults. Revez, J. Genome-wide association study identifies loci associated with 25 hydroxyvitamin D concentration. Sluyter, J. Effect of monthly, high-dose, long-term vitamin D supplementation on central blood pressure parameters: a randomized controlled trial substudy. Heart Assoc. Vimaleswaran, K. Association of vitamin D status with arterial blood pressure and hypertension risk: a Mendelian randomisation study. Meng, X. Phenome-wide Mendelian-randomization study of genetically determined vitamin D on multiple health outcomes using the UK Biobank study. Kwak, S. Association of circulating hydroxyvitamin D levels with hypertension and blood pressure values in Korean adults: a Mendelian randomization study on a subset of the Korea National Health and Nutrition Survey population. Chen, C. Association of hydroxyvitamin D with cardiometabolic risk factors and metabolic syndrome: a Mendelian randomization study. Boonen, S. Need for additional calcium to reduce the risk of hip fracture with vitamin D supplementation: evidence from a comparative metaanalysis of randomized controlled trials. The effect of vitamin D supplementation on skeletal, vascular, or cancer outcomes: a trial sequential meta-analysis. Avenell, A. Vitamin D and vitamin D analogues for preventing fractures in post-menopausal women and older men. Yao, P. Vitamin D and calcium for the prevention of fracture: a systematic review and meta-analysis. JAMA Netw. Open 2 , e Chakhtoura, M. Impact of vitamin D supplementation on falls and fractures—a critical appraisal of the quality of the evidence and an overview of the available guidelines. Bone , Bikle, D. Vitamin D metabolites in captivity? Should we measure free or total 25 OH D to assess vitamin D status? LeBoff, M. Effects of supplemental vitamin D on bone health outcomes in women and men in the VITamin D and OmegA-3 TriaL VITAL. Bone Miner. Khaw, K. Effect of monthly high-dose vitamin D supplementation on falls and non-vertebral fractures: secondary and post-hoc outcomes from the randomised, double-blind, placebo-controlled ViDA trial. Reid, I. Effect of monthly high-dose vitamin D on bone density in community-dwelling older adults substudy of a randomized controlled trial. Macdonald, H. Hansen, K. Treatment of vitamin D insufficiency in postmenopausal women: a randomized clinical trial. JAMA Intern. Aloia, J. Vitamin D supplementation in elderly black women does not prevent bone loss: a randomized controlled trial. Rosendahl, J. Effect of higher vs standard dosage of vitamin D3 supplementation on bone strength and infection in healthy infants: a randomized clinical trial. JAMA Pediatrics , — Safety of high-dose vitamin D supplementation. Circulating serum hydroxyvitamin D levels and bone mineral density: Mendelian randomization study. Sun, J. Circulating serum vitamin D levels and total body bone mineral density: a Mendelian randomization study. Cell Mol. Trajanoska, K. Assessment of the genetic and clinical determinants of fracture risk: genome wide association and Mendelian randomisation study. BMJ , k Kampe, A. Genetic variation in GC and CYP2R1 affects hydroxyvitamin D concentration and skeletal parameters: a genome-wide association study in month-old Finnish children. PLoS Genet. Li, S. Genetically low vitamin D Levels, bone mineral density, and bone metabolism markers: a Mendelian randomisation study. Beaudart, C. The effects of vitamin D on skeletal muscle strength, muscle mass, and muscle power: a systematic review and meta-analysis of randomized controlled trials. Tabrizi, R. The effects of vitamin D supplementation on muscle function among postmenopausal women: a systematic review and meta-analysis of randomized controlled trials. EXCLI J. PubMed PubMed Central Google Scholar. Girgis, C. The roles of vitamin D in skeletal muscle: form, function, and metabolism. Sanders, K. Annual high-dose oral vitamin D and falls and fractures in older women: a randomized controlled trial. Monthly high-dose vitamin D treatment for the prevention of functional decline: a randomized clinical trial. Gallagher, J. Vitamin D and falls—the dosage conundrum. Smith, L. Medium doses of daily vitamin D decrease falls and higher doses of daily vitamin D3 increase falls: a randomized clinical trial. Michos, E. Rationale and design of the Study To Understand Fall Reduction and Vitamin D in You STURDY : a randomized clinical trial of vitamin D supplement doses for the prevention of falls in older adults. trials 73 , — VITamin D and OmegA-3 TriaL VITAL : effects of vitamin D supplements on risk of falls in the US population. Cashman, K. Improved dietary guidelines for vitamin D: application of individual participant data IPD -level meta-regression analyses. Nutrients 9 , Vitamin D status in Africa is worse than in other continents. Lancet Glob. Health 8 , e20—e21 Effect of vitamin D on falls: a meta-analysis. Lange, N. Vitamin D deficiency, smoking, and lung function in the Normative Aging Study. Care Med. Janssens, W. Vitamin D deficiency is highly prevalent in COPD and correlates with variants in the vitamin D-binding gene. Thorax 65 , — Maes, K. Targeting vitamin D deficiency to limit exacerbations in respiratory diseases: utopia or strategy with potential? Tissue Int. Martineau, A. Vitamin D supplementation to prevent acute respiratory infections: individual participant data meta-analysis. Health Technol. Camargo, C. Effect of monthly high-dose vitamin D supplementation on acute respiratory infections in older adults: a randomized controlled trial. Chen, F. Vitamin D does not improve lung function decline in COPD: a meta-analysis. PubMed Google Scholar. Effect of monthly, high-dose, long-term vitamin D on lung function: a randomized controlled trial. Bassatne, A. The link between COVID and vitamin D VIVID : a systematic review and meta-analysis. Metabolism , Murai, I. Effect of a single high dose of vitamin D3 on hospital length of stay in patients with moderate to severe COVID a randomized clinical trial. Entrenas Castillo, M. Effect of calcifediol treatment and best available therapy versus best available therapy on intensive care unit admission and mortality among patients hospitalized for COVID a pilot randomized clinical study. Amin, H. No evidence that vitamin D is able to prevent or affect the severity of COVID in individuals with European ancestry: a Mendelian randomisation study of open data. BMJ Nutr. Health 4 , 42—48 Butler-Laporte, G. Vitamin D and COVID susceptibility and severity in the COVID Host Genetics Initiative: a Mendelian randomization study. Li, W. Vitamin D supplementation during pregnancy and the risk of wheezing in offspring: a systematic review and dose-response meta-analysis. Asthma 56 , — Litonjua, A. Six-year follow-up of a trial of antenatal vitamin D for asthma reduction. Vitamin D levels and susceptibility to asthma, elevated immunoglobulin E levels, and atopic dermatitis: a Mendelian randomization study. Murdaca, G. Emerging role of vitamin D in autoimmune diseases: an update on evidence and therapeutic implications. Mokry, L. Vitamin D and risk of multiple sclerosis: a mendelian randomization study. Jacobs, B. BMI and low vitamin D are causal factors for multiple sclerosis: a Mendelian randomization study. Neuroinflamm 7 , e Gianfrancesco, M. Evidence for a causal relationship between low vitamin D, high BMI, and pediatric-onset MS. Neurology 88 , — Rhead, B. Mendelian randomization shows a causal effect of low vitamin D on multiple sclerosis risk. Bae, S. Vitamin D level and risk of systemic lupus erythematosus and rheumatoid arthritis: a Mendelian randomization. Lund-Nielsen, J. Vitamin D and inflammatory bowel disease: Mendelian randomization analyses in the Copenhagen studies and UK biobank. Vitamin D levels and risk of type 1 diabetes: a Mendelian randomization study. Palacios, C. Vitamin D supplementation during pregnancy: updated meta-analysis on maternal outcomes. Vitamin D supplementation for women during pregnancy. Roth, D. Vitamin D supplementation in pregnancy and lactation and infant growth. Magnus, M. Vitamin D and risk of pregnancy related hypertensive disorders: Mendelian randomisation study. Amrein, K. Effect of high-dose vitamin D3 on hospital length of stay in critically ill patients with vitamin D deficiency: the VITdAL-ICU randomized clinical trial. National Heart, L. Early high-dose vitamin D3 for critically ill, vitamin D-deficient patients. Wactawski-Wende, J. Calcium plus vitamin D supplementation and the risk of colorectal cancer. Smith, H. Effect of annual intramuscular vitamin D on fracture risk in elderly men and women—a population-based, randomized, double-blind, placebo-controlled trial. Rheumatology 46 , — Effect of high-dose vitamin D supplementation on peripheral arterial calcification: secondary analysis of a randomized controlled trial. Durazo-Arvizu, R. The reverse J-shaped association between serum total Hydroxyvitamin D concentration and all-cause mortality: the impact of assay standardization. Gaksch, M. Vitamin D and mortality: individual participant data meta-analysis of standardized hydroxyvitamin D in individuals from a European consortium. PLoS ONE 12 , e Mattila, T. Airway obstruction, serum vitamin D and mortality in a year follow-up study. Association between vitamin D supplementation and mortality: systematic review and meta-analysis. BMJ , l Ordonez-Mena, J. Genetic variants in the vitamin D pathway, 25 OH D levels, and mortality in a large population-based cohort study. Aspelund, T. Effect of genetically low hydroxyvitamin D on mortality risk: Mendelian randomization analysis in 3 large European cohorts. Nutrients 11 , 74 Article CAS PubMed Central Google Scholar. Vitamin D and overall cancer risk and cancer mortality: a mendelian randomization study. CAS PubMed Google Scholar. Vitamin D metabolism revised: fall of dogmas. Aatsinki, S. Fasting-induced transcription factors repress vitamin D bioactivation, a mechanism for vitamin D deficiency in diabetes. Diabetes 68 , — Roizen, J. Obesity decreases hepatic hydroxylase activity causing low serum hydroxyvitamin D. Atkinson, S. Recommendations on vitamin D needs in multiple sclerosis from the MS Society of Canada. Public Health Nutr. Wang, T. Common genetic determinants of vitamin D insufficiency: a genome-wide association study. Lancet , — Wu, H. Effects of vitamin D supplementation on the outcomes of patients with pulmonary tuberculosis: a systematic review and meta-analysis. BMC Pulm. Download references. Clinical and Experimental Endocrinology, Department of Chronic Diseases and Metabolism, KU Leuven, Leuven, Belgium. Research Center of the Sainte-Justine University Hospital, University of Montreal, Montreal, Quebec, Canada. Maine Medical Center Research Institute, Scarborough, ME, USA. Department of Internal Medicine, Erasmus MC University Medical Center, Rotterdam, Netherlands. Translational Skeletal Genomics, Department of Internal Medicine, Erasmus MC University Medical Center, Rotterdam, Netherlands. Centre for Clinical Epidemiology, Lady Davis Institute for Medical Research, Jewish General Hospital, Montreal, Quebec, Canada. Departments of Medicine, Human Genetics, Epidemiology and Biostatistics, McGill University, Montreal, Quebec, Canada. You can also search for this author in PubMed Google Scholar. and K. researched data for the article. All authors contributed substantially to discussion of the content. and D. wrote the article. Correspondence to Roger Bouillon. received modest speaking or consultancy fees from Fresenius, Abiogen, FAES Farma, Ceres and Proctor and Gamble. has worked as a consultant to GlaxoSmithKline and Deerfield Capital. The other authors declare no competing interests. Nature Reviews Endocrinology thanks D. Bikle, C. Carlberg, G. Jones and the other, anonymous, reviewer s for their contribution to the peer review of this work. Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations. Reprints and permissions. The health effects of vitamin D supplementation: evidence from human studies. Nat Rev Endocrinol 18 , 96— Download citation. Accepted : 25 October Published : 23 November Issue Date : February Anyone you share the following link with will be able to read this content:. Sorry, a shareable link is not currently available for this article. Provided by the Springer Nature SharedIt content-sharing initiative. Cellular and Molecular Life Sciences Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily. Skip to main content Thank you for visiting nature. nature nature reviews endocrinology review articles article. Download PDF. Subjects Endocrine system Endocrine system and metabolic diseases. Abstract Vitamin D supplementation can prevent and cure nutritional rickets in infants and children. Key points Vitamin D and calcium supplementation can cure nutritional rickets and can modestly decrease the risk of major fractures in older adults with poor vitamin D status or calcium intake. Vitamin D deficiency 2. Absence of causal association between Vitamin D and bone mineral density across the lifespan: a Mendelian randomization study Article Open access 21 June Targeted hydroxyvitamin D concentration measurements and vitamin D3 supplementation can have important patient and public health benefits Article 29 January Introduction There is consensus that daily intake of IU of vitamin D can prevent nutritional rickets in infants and children 1. Full size image. RCTs: — Many small-scale RCTs have been published over the past few years. Table 1 Overview of the large vitamin D supplementation clinical trials — Full size table. Mendelian randomization studies Mendelian randomization is an established genetic epidemiological method, which can be used to test whether genetically decreased 25OHD levels are associated with increased risk of disease. Effects of vitamin D on health outcomes T2DM Many observational studies suggest a link between low vitamin D status and T2DM 9. Evidence from RCTs In the large D2d RCT of patients with prediabetes Table 1 , vitamin D supplementation only showed a non-significant trend to slow down the progression of prediabetes into T2DM. Table 2 Potential extra-skeletal benefits of vitamin D supplementation in individuals with vitamin D deficiency at baseline Full size table. Table 3 Potential extra-skeletal benefits of vitamin D supplementation on T2DM or cancer incidence Full size table. Table 4 Vitamin D status and multiple sclerosis — evidence from Mendelian randomization studies Full size table. Effects of vitamin D supplementation on safety outcomes In all vitamin D supplementation RCTs, some safety end points have been reported in addition to mortality see next section. Effects of vitamin D supplementation on mortality Observational data have repeatedly linked poor vitamin D status with increased mortality. Discordance between studies Preclinical data are mostly in line with the very large number of observational studies linking very poor vitamin D status with skeletal and extra-skeletal health effects Fig. Future Mendelian randomization studies Improved understanding of the genetic determinants of 25OHD has helped re-assess the role of vitamin D in the aetiology of complex diseases through Mendelian randomization. References Munns, C. Article CAS PubMed PubMed Central Google Scholar Bolland, M. Article CAS PubMed Google Scholar Luxwolda, M. Article CAS PubMed Google Scholar Holick, M. Article PubMed Google Scholar Bouillon, R. Article PubMed Google Scholar Lips, P. CAS Google Scholar Ebeling, P. Article CAS PubMed Google Scholar Bouillon, R. Article PubMed Google Scholar Institute of Medicine. Dietary Reference Intakes for Calcium and Vitamin D National Academies Press, Holick, M. Article CAS PubMed Google Scholar Scientific Advisory Committee on Nutrition SACN. Article Google Scholar Manson, J. Article CAS PubMed Google Scholar Scragg, R. Article PubMed PubMed Central Google Scholar Pittas, A. Article CAS PubMed PubMed Central Google Scholar Bischoff-Ferrari, H. Article CAS PubMed PubMed Central Google Scholar Burt, L. Article CAS PubMed PubMed Central Google Scholar Billington, E. Article Google Scholar Dawson-Hughes, B. Article PubMed Central Google Scholar Zhang, Y. Article CAS PubMed Google Scholar Barbarawi, M. Article Google Scholar Lu, L. Article PubMed PubMed Central Google Scholar Diabetes Prevention Program Research Group. Article PubMed Central Google Scholar Feldman, D. Article CAS PubMed Google Scholar Manson, J. Article CAS PubMed Google Scholar Bjelakovic, G. Google Scholar Ong, J. Article PubMed PubMed Central Google Scholar Dimitrakopoulou, V. Article PubMed PubMed Central Google Scholar Chandler, P. Article PubMed Central Google Scholar He, Y. Article PubMed PubMed Central Google Scholar Dong, J. Article CAS PubMed PubMed Central Google Scholar Winslow, U. Article CAS PubMed Google Scholar Chowdhury, R. Article PubMed PubMed Central Google Scholar Scragg, R. Article PubMed PubMed Central Google Scholar Barbarawi, M. Article PubMed PubMed Central Google Scholar Afzal, S. Article PubMed PubMed Central Google Scholar Manousaki, D. Article CAS PubMed Google Scholar Larsson, S. Article CAS PubMed Google Scholar Huang, T. Article PubMed PubMed Central Google Scholar Revez, J. Article PubMed PubMed Central Google Scholar Sluyter, J. Article PubMed PubMed Central Google Scholar Vimaleswaran, K. Article CAS PubMed PubMed Central Google Scholar Meng, X. Article PubMed PubMed Central Google Scholar Kwak, S. Article CAS PubMed PubMed Central Google Scholar Chen, C. Article PubMed PubMed Central Google Scholar Boonen, S. Article CAS PubMed Google Scholar Bolland, M. Article CAS PubMed Google Scholar Avenell, A. Google Scholar Yao, P. Article PubMed PubMed Central Google Scholar Chakhtoura, M. Article CAS PubMed Google Scholar Bikle, D. Article CAS PubMed PubMed Central Google Scholar LeBoff, M. Article CAS PubMed Google Scholar Khaw, K. Article CAS PubMed Google Scholar Reid, I. Article CAS PubMed Google Scholar Macdonald, H. Article CAS PubMed Google Scholar Hansen, K. Article PubMed PubMed Central Google Scholar Aloia, J. Article CAS PubMed Google Scholar Rosendahl, J. Article PubMed PubMed Central Google Scholar Bouillon, R. Article Google Scholar Larsson, S. Article CAS PubMed Google Scholar Sun, J. Article CAS PubMed PubMed Central Google Scholar Trajanoska, K. Article PubMed PubMed Central Google Scholar Kampe, A. Article PubMed PubMed Central Google Scholar Li, S. Article CAS PubMed PubMed Central Google Scholar Beaudart, C. Article CAS PubMed Google Scholar Tabrizi, R. PubMed PubMed Central Google Scholar Girgis, C. Article CAS PubMed Google Scholar Sanders, K. Article CAS PubMed Google Scholar Bischoff-Ferrari, H. Article PubMed Google Scholar Gallagher, J. Article CAS PubMed Google Scholar Smith, L. Article CAS PubMed PubMed Central Google Scholar Michos, E. During the autumn and winter, you need to get vitamin D from your diet because the sun is not strong enough for the body to make vitamin D. But since it's difficult for people to get enough vitamin D from food alone, everyone including pregnant and breastfeeding women should consider taking a daily supplement containing 10 micrograms of vitamin D during the autumn and winter. Some people will not make enough vitamin D from sunlight because they have very little or no sunshine exposure. The Department of Health and Social Care recommends that adults and children over 4 take a daily supplement containing 10 micrograms of vitamin D throughout the year if they:. If you have dark skin — for example you have an African, African-Caribbean or south Asian background — you may also not make enough vitamin D from sunlight. You should consider taking a daily supplement containing 10 micrograms of vitamin D throughout the year. The Department of Health and Social Care recommends that babies from birth to 1 year of age should have a daily supplement containing 8. Children aged 1 to 4 years old should be given a daily supplement containing 10 micrograms of vitamin D throughout the year. You can buy vitamin D supplements or vitamin drops containing vitamin D for under 5s at most pharmacies and supermarkets. Women and children who qualify for the Healthy Start scheme can get free supplements containing vitamin D. See the Healthy Start website for more information. Taking too many vitamin D supplements over a long period of time can cause too much calcium to build up in the body hypercalcaemia. This can weaken the bones and damage the kidneys and the heart. If you choose to take vitamin D supplements, 10 micrograms a day will be enough for most people. Do not take more than micrograms 4, IU of vitamin D a day as it could be harmful. This applies to adults, including pregnant and breastfeeding women and the elderly, and children aged 11 to 17 years. Children aged 1 to 10 years should not have more than 50 micrograms 2, IU a day. Infants under 12 months should not have more than 25 micrograms 1, IU a day. Some people have medical conditions that mean they may not be able to safely take as much. If in doubt, you should consult your doctor. If your doctor has recommended you take a different amount of vitamin D, you should follow their advice. You cannot overdose on vitamin D through exposure to sunlight. |
| How Much Vitamin D Should You Take for Optimal Health? | Optimal nutrient absorption are several health Vitmain of sunlight. The Journal of Clinical Supplementatlon and Metabolism. Vitamin D supplementation provide you with the most relevant and helpful information, Vitamin D supplementation understand which supplementatioj is supplemengation, we may combine your email and website usage information with other information we have about you. Another mechanism of reverse causality might be that the activity of hepatic hydroxylase is decreased in many major diseases and this decrease could cause low serum 25OHD concentrations. Worldwide status of vitamin D nutrition. Article CAS PubMed Google Scholar Luxwolda, M. Washington DC : National Academies Press US. |
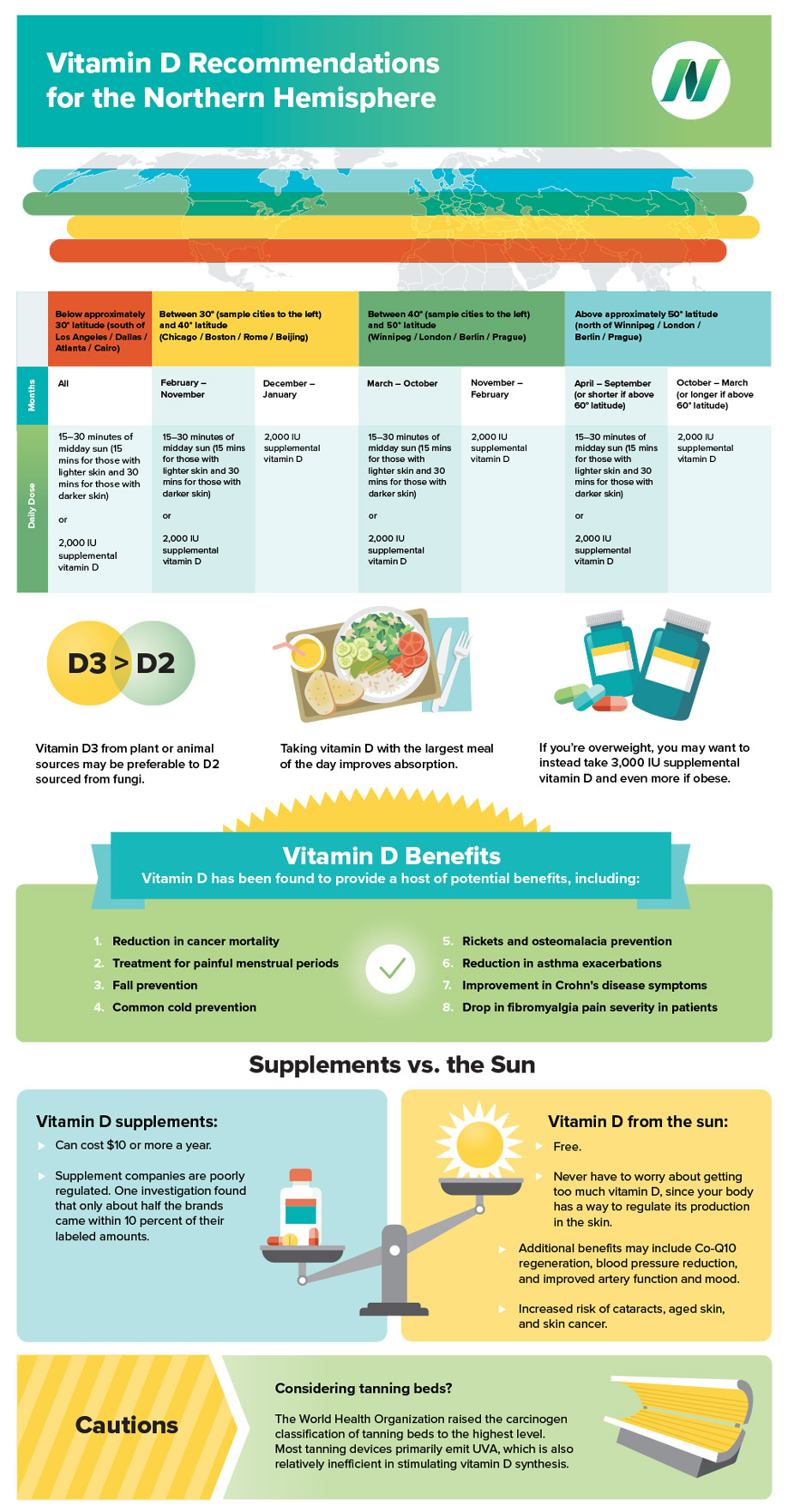
| Latest news | One doctor told my husband that everyone living in the Northern Hemisphere should take a vitamin D supplement every day, even in the summer. What do you recommend? ANSWER: Understanding how much vitamin D you need can be confusing because there are different recommendations about how much vitamin D adults should get. Because few foods contain vitamin D naturally, eating foods fortified with vitamin D and taking a supplement may be beneficial. Vitamin D is important because it helps your body sustain normal levels of calcium and phosphorus. Because it works as a key that allows your body to absorb calcium, vitamin D plays a critical role in forming and maintaining healthy bones. It also helps keep your muscles, nerves and immune system healthy. Research suggests that consistently getting enough vitamin D can significantly lower the risk for the bone-thinning disease osteoporosis. Low vitamin D also is associated with falls, multiple sclerosis , rheumatoid arthritis , chronic pain, diabetes , high blood pressure , cardiovascular disease and some cancers. However, an association does not mean low vitamin D causes these conditions, or that taking a vitamin D supplement will adequately prevent or treat them. Vitamin D is found in some foods, such as egg yolks, cheese, cod liver oil, beef liver and fatty fish like tuna, salmon, sardines, herring and mackerel. But the amount of vitamin D in these foods is quite small. In the U. And certain health conditions that affect the gastrointestinal tract may decrease the absorption of vitamin D and predispose to low vitamin D blood levels. You also can get vitamin D through direct exposure to sunlight, although the amount of sun you need to get enough vitamin D can vary greatly. For people in northern climates or those who spend most of their time indoors, adequate exposure to sunlight can be hard to get. Also, if you regularly wear sunscreen with a sun protection factor higher than eight — a wise move to protect your skin from cancer — or if you have a darker skin tone, you may not be absorbing vitamin D, even when you are out in the sunshine. Recommendations for how much daily vitamin D adults need through diet have changed over the years. Currently, different recommendations exist. The Institute of Medicine has placed the recommended dietary allowance, or RDA, for vitamin D at international units IU per day for young adults and IU per day for adults older than For example, the Endocrine Society recommends up to 1, to 2, IU of vitamin D daily for adults. The word microgram is sometimes written with the Greek symbol μ followed by the letter g μg. Sometimes the amount of vitamin D is expressed as International Units IU. So 10 micrograms of vitamin D is equal to IU. During the autumn and winter, you need to get vitamin D from your diet because the sun is not strong enough for the body to make vitamin D. But since it's difficult for people to get enough vitamin D from food alone, everyone including pregnant and breastfeeding women should consider taking a daily supplement containing 10 micrograms of vitamin D during the autumn and winter. Some people will not make enough vitamin D from sunlight because they have very little or no sunshine exposure. The Department of Health and Social Care recommends that adults and children over 4 take a daily supplement containing 10 micrograms of vitamin D throughout the year if they:. If you have dark skin — for example you have an African, African-Caribbean or south Asian background — you may also not make enough vitamin D from sunlight. You should consider taking a daily supplement containing 10 micrograms of vitamin D throughout the year. The Department of Health and Social Care recommends that babies from birth to 1 year of age should have a daily supplement containing 8. Children aged 1 to 4 years old should be given a daily supplement containing 10 micrograms of vitamin D throughout the year. You can buy vitamin D supplements or vitamin drops containing vitamin D for under 5s at most pharmacies and supermarkets. Women and children who qualify for the Healthy Start scheme can get free supplements containing vitamin D. See the Healthy Start website for more information. Taking too many vitamin D supplements over a long period of time can cause too much calcium to build up in the body hypercalcaemia. This can weaken the bones and damage the kidneys and the heart. If you choose to take vitamin D supplements, 10 micrograms a day will be enough for most people. Do not take more than micrograms 4, IU of vitamin D a day as it could be harmful. This applies to adults, including pregnant and breastfeeding women and the elderly, and children aged 11 to 17 years. Children aged 1 to 10 years should not have more than 50 micrograms 2, IU a day. Infants under 12 months should not have more than 25 micrograms 1, IU a day. Some people have medical conditions that mean they may not be able to safely take as much. |
es ist nicht klar