Thinking of going gluten-free? If you are, you have plenty of company. Gluten-free diet and gut health and enthusiasm around but diets continues to grow lGuten-free. You can find plenty of books, diet experts, and Measuring body composition supporting the Gluten-free diet and gut health.
But does it really improve your health or sense of well-being? Or Gluten-fre it just be yut widely amplified ugt fad? Gluten is a protein found in Muscle building nutrition grains, including wheat, barley, and rye.
It's common Understanding Ac levels foods such didt bread, pasta, pizza, and Gluten-free. Gluten provides Gluten-fred essential nutrients. People with celiac diiet have an immune reaction that heslth triggered by eating gluten. They develop inflammation Gluten-free diet and gut health damage in their intestinal tracts and other parts abd the Gluten-free when they eat foods dier gluten.
If wnd do have celiac Gluten-free diet and gut health, a Gluten-fres diet is necessary to ahd the inflammation and the symptoms. Grocery stores and restaurants routinely offer gluten-free options die rival conventional foods in taste and quality; in diwt past, it was much harder to maintain a gluten-free diet.
As mentioned, people with celiac guh avoid Gluten-frer and maintain much better health heallth they follow a gluten-free diet. For them, a gluten-free diet is nothing Tailored meal plans of essential.
Glutrn-free then Gluten-free diet and gut health are people described as gluten-sensitive. Their tests for celiac healyh are negative nadyet whenever they heath food containing gluten, they experience symptoms like bloating Gluten-ftee, diarrhea, diett crampy abdominal pain.
One cause is wheat Dietary supplement slimming pills, a helth that can be diagnosed by skin testing. But healtg many others, the diagnosis remains uncertain. Some have begun calling this non-celiac gluten hypersensitivity, a poorly defined condition about which we have much to learn.
Avoiding gluten makes sense for people with celiac disease, wheat allergy, or those who feel unwell whenever they consume gluten.
There is no compelling evidence that a gluten-free diet will improve health or prevent disease if you don't have celiac disease and can eat gluten without trouble.
Of course, future research could change this. We may someday learn that at least some people without celiac disease or symptoms of intestinal disease are better off avoiding gluten. Before you buy into the gluten-free life, buyer beware!
While many people think gluten-free diets are more nutritious and contain more minerals and vitamins than conventional foods, the opposite is often true. Gluten-free foods are commonly less fortified with folic acid, iron, and other nutrients than regular foods containing gluten.
And gluten-free foods tend to have less fiber and more sugar and fat. Several studies have found a trend toward weight gain and obesity among those who follow a gluten-free diet including those with celiac disease. Meanwhile, gluten-free foods tend to be more expensive than conventional foods.
It reminds me of the organic food option: People are often willing to pay much higher prices for foods they think are healthier. The problem is that there is little or no proof that these foods are actually better for you. If you feel well and have no digestive symptoms, enjoy your good health!
And stop worrying so much about gluten. But if you have symptoms that might be related to gluten, or any significant and unexplained symptoms, talk to your doctor. Symptoms of celiac disease or gluten sensitivity include.
There are reliable tests to diagnose celiac disease. These include genetic tests, blood tests that detect certain antibodies, and intestinal biopsies. The results can help you understand which, if any, foods you should avoid. You may learn that you can eat anything you like. You may learn that it's lactose the sugar in milknot gluten, that's causing you trouble.
Or you may turn out to have another common condition that's unrelated to gluten, such as Crohn's disease, an ulcer, or irritable bowel syndrome.
We are undoubtedly in a time of heightened gluten awareness. Is that a good thing? It is if you have celiac disease. I think it's a major step forward that people who truly need to avoid gluten can do so more easily than in the past, as more gluten-free foods are now available and labels more clearly identify foods containing gluten.
But the dangers of gluten have probably been overstated — and oversold. Don't be swayed by an elite athlete or influencer to restrict your diet when there's no medical reason to do so. It's up to you and your doctor — not a celebrity or a book author — to take care of your health.
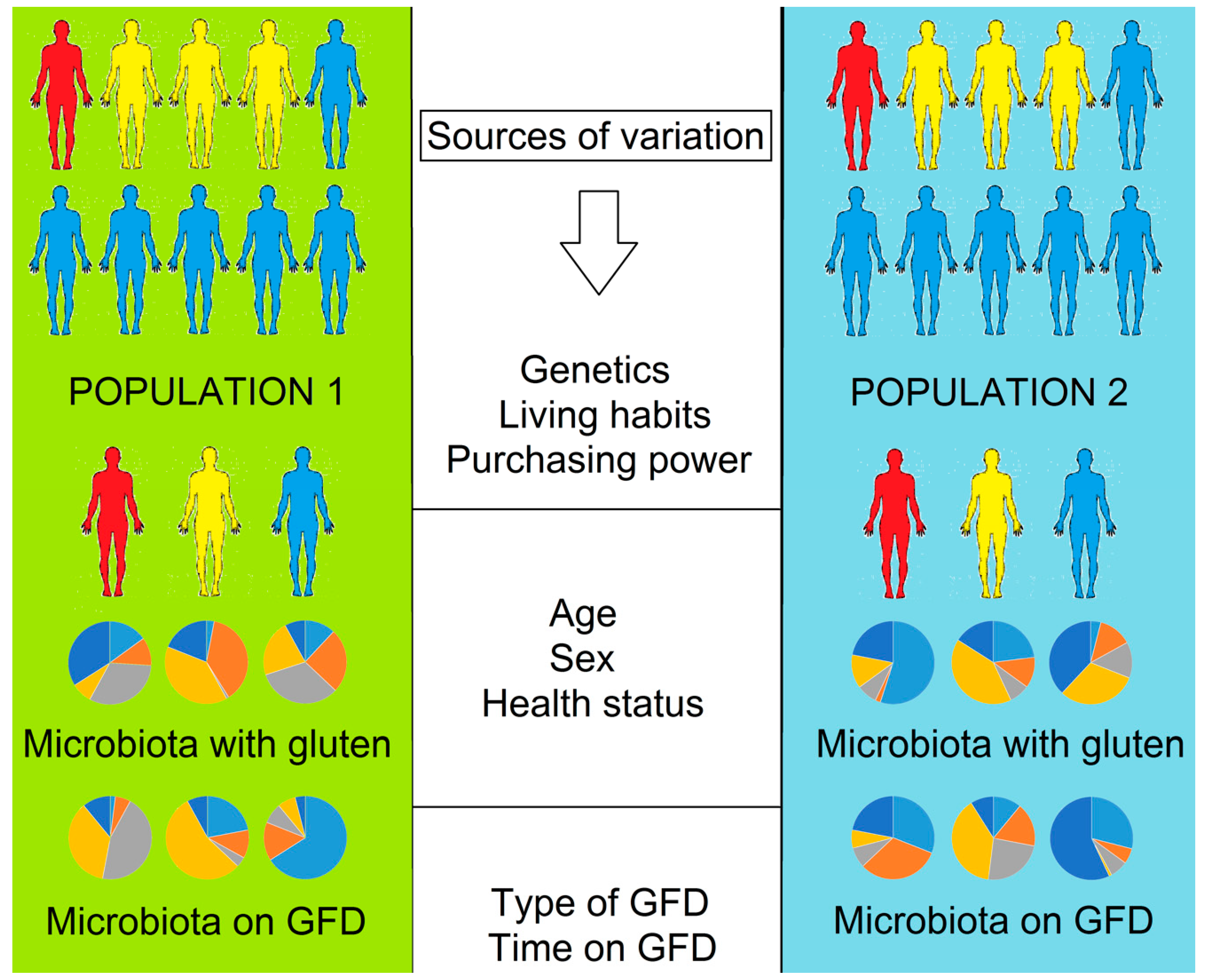
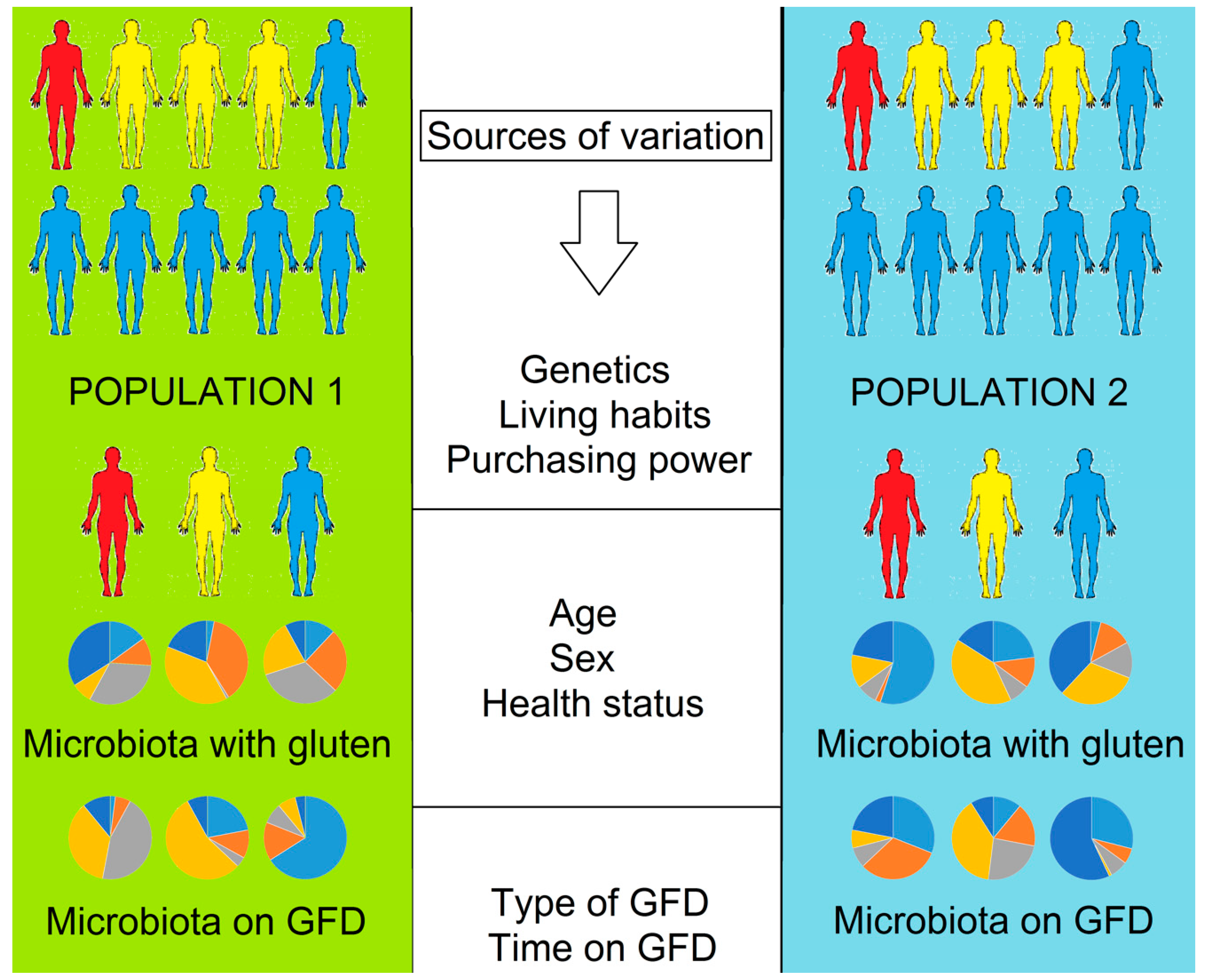
: Gluten-free diet and gut health| Helpful Links | In general, gluten has often been swerved in the past as it has the potential to cause inflammation. Research found that having a leaky gut can contribute from everything to over-activation of the immune system to chronic inflammation. It is important to note here that, that being said, there is no one-size-fits-all approach when it comes to nutrition and, indeed, gluten. There is nothing inherently wrong with gluten and the majority of the population eat it day-to-day without suffering from ill side effects. It's in a lot of the foods we eat - bread, pasta, cereals and more. That being said, going gluten free is an absolute must for those with coeliac disease, shares Chamon. Did you know? Grains such as wheat are unfortunately some of the crops that are most heavily affected by the use of pesticides such as glyphosate, shares the expert. As above, it may be a trigger for digestive symptoms such as bloating and diarrhoea. Fun fact: wheat is a source of prebiotic fibre, which is the main source of food for our beneficial gut bacteria. It's completely up to you and your body type, but there is nothing innately "bad" with gluten and you certainly shouldn't ever avoid food groups for the sake of it. For those without a diagnosis of Coeliac Disease or wheat allergy it may be worth consulting with a qualified nutritionist before jumping into a gluten free diet. Celebrity news, beauty, fashion advice, and fascinating features, delivered straight to your inbox! Ally Head is Marie Claire UK's Senior Health, Sustainability, and Relationships Editor, nine-time marathoner, and Boston Qualifying runner. She's won a BSME for her sustainability work, regularly hosts panels and presents for events like the Sustainability Awards, and saw nine million total impressions on the January Wellness Issue she oversaw. The research on this topic is expanding rapidly, and alterations in the microbiome have been correlated to conditions such as obesity , inflammatory bowel disease , other autoimmune diseases , and cancer. The information resulting from microbiome research is changing the practice of medicine. Several studies have reported imbalances in the microbiome in people with celiac disease, and another showed the bacteria we have might affect what symptoms we display. This may explain why some celiac patients experience headaches, while others have joint pain; the type of bacteria they have in their intestine may be playing a role. The Finnish study mentioned earlier found less bacterial diversity fewer different types of bacteria and an imbalance in certain types of bacteria in celiac patients with persistent symptoms. The bacterial make-up of people with ongoing symptoms resembled that of untreated celiac patients. The microbiome stays relatively stable in healthy people, but when illness or antibiotics upset the balance, the microbiome is altered. Most studies with probiotics and celiac disease have been done in animals. Studies show that probiotics can decrease inflammation when gluten exposure occurs. Human studies are needed, and the best type of probiotic is yet to be identified, but the results thus far are promising. Diversity in the gut means you have a lot of different types of gut bacteria. The diversity of gut bacteria is a good thing. Effective treatments to make the microbiome more healthy and diverse are in development. Until then, here are things you can do to optimize it on your own. This is exciting news for people with celiac disease or any autoimmune disorder. If we can learn to optimize and balance the microbiome and follow a gluten-free diet if you have celiac disease , symptoms may be decreased or alleviated. If we can change the microbiome with targeted probiotics or even fecal transplants , the potential for optimal health is improved. Since a correlation is also found between bacterial imbalance and autoimmune diseases , balancing and optimizing the microbiome may also decrease the risk of other autoimmune diseases, such as thyroid disease, which affects over 20 million people in the US alone. And perhaps by modulating the microbiome, we can even decrease the risk of cancer. The possibilities are exciting! Amy Burkhart is a doctor M. and Registered Dietitian R. Consuming more naturally-occurring gluten-free foods, such as fruits, vegetables, legumes, certain whole grains, fish, dairy, and meat, is the best way to cut out gluten, get plenty of vitamins and minerals, and avoid sneaky branding. As with any medical condition, it is always best to seek assistance from a qualified medical professional if you are experiencing symptoms that are causing you difficulty. If you need a gastroenterologist in Southern Indiana, or in the Louisville or Lexington Kentucky-area, contact Gastroenterology Health Partners today for more information or to schedule an appointment. Is The Gluten-Free Diet Right For You? You might also like Prevent Colorectal Cancer: Get Screened. William Evans Discusses Pancreatitis. Irritable Bowel Syndrome — Signs and Symptoms. Whitney Jones Discusses Colorectal Cancer. John Horlander Explains a Colonoscopy. When It Comes To Early-Onset Colorectal Cancer, More Awareness Is Needed. |
| Subscribe for updates, exclusive promotions, and more. | However, in general, it could be hypothesized that these bacteria benefit from a change in available substrates as a result from the change in diet, which could in turn result in altered metabolite production and related gastrointestinal complaints. Download citation. Natl Acad. All individuals gave written informed consent before participating in the study. Consuming more naturally-occurring gluten-free foods, such as fruits, vegetables, legumes, certain whole grains, fish, dairy, and meat, is the best way to cut out gluten, get plenty of vitamins and minerals, and avoid sneaky branding. |
| Does Gluten Cause Leaky Gut Syndrome? | The study was supported by the Innovation Fund Denmark grant no. Similarly, a previous study reported that production of pro-inflammatory cytokines by peripheral blood mononuclear cells stimulated with faecal water was reduced after a GFD This is because gluten-free products cost manufacturers more money to make. Cereal Sci. Article CAS PubMed Google Scholar May A, Abeln S, Crielaard W, Heringa J, Brandt BW. |
| Does Gluten Cause Leaky Gut Syndrome? | In this study we found a stronger effect of diet on the imputed KEGG pathways than on the taxonomic level. So, although the changes in the overall microbiome were moderate, there were more profound effects on the pathway activities of the microbiome. The strength of our study lies in our analysis of the microbiome at multiple time points for the same individuals. We identified that the inter-individual variability is the strongest determinant of sample variability, suggesting that in healthy individuals the gut microbiome is stable, even with short-term changes in the habitual diet. We did not observe differences in the downstream effect of GFD in relation to high or low richness, which contradicts previous observations [ 50 ]. The study by David et al. This profound short-term diet effect was not observed in our study when changing from a gluten-containing to a gluten-free diet. Induced by the diet change, David et al. These results suggest that changing the main energy source meat vs. plant has a more profound effect on the microbiome than changing the carbohydrate source gluten. Although De Palma et al. Further, it is possible that changes in nutritional intake other than those driven by gluten exclusion might influence microbiome changes. For our selection of blood and stool biomarkers, we observed no significant associations with the diet change. All the selected biomarkers are markers of inflammation or metabolic changes and remained in the normal range in all our participants, with a high proportion of the values of blood inflammatory markers being below the detection limit. Overall, we conclude that a GFD and its downstream effects on the microbiome do not cause major inflammatory or metabolic changes in gut function in healthy participants. We have identified eight taxa and 21 bacterial pathways associated with a change from a habitual diet to a GFD in healthy individuals. We conclude that the effect of gluten intake on the microbiota is less pronounced than that seen for a shift from a meat-based diet to a vegetarian diet or vice versa. However, a GFD diet clearly influences the abundance of several species, in particular those involved specifically in carbohydrate and starch metabolism. Our study illustrates that variations in diet could confound the results of microbiome analysis in relation to disease phenotypes, so dietary variations should be carefully considered and reported in such studies. The short-term GFD did not influence the levels of inflammatory gut biomarkers in healthy individuals. Further research is needed to assess the impact of a GFD on inflammatory and metabolic changes in gut function in individuals with gastrointestinal conditions such as IBS and gluten-related disorders. This GFD study followed the sampling protocol of the LifeLines-DEEP study, which was approved by the ethics committee of the University Medical Centre Groningen and conform the Declaration of Helsinki, document no. All participants signed their informed consent prior to study enrolment. Sollid LM. Coeliac disease: dissecting a complex inflammatory disorder. Nat Rev Immunol. Article CAS PubMed Google Scholar. Sapone A, Bai JC, Ciacci C, Dolinsek J, Green PH, Hadjivassiliou M, et al. Spectrum of gluten-related disorders: consensus on new nomenclature and classification. BMC Med. Article PubMed PubMed Central Google Scholar. Catassi C, Bai JC, Bonaz B, Bouma G, Calabrò A, Carroccio A, et al. Non-celiac gluten sensitivity: the new frontier of gluten related disorders. A controlled trial of gluten-free diet in patients with irritable bowel syndrome-diarrhea: effects on bowel frequency and intestinal function. Collado MC, Donat E, Ribes-Koninckx C, Calabuig M, Sanz Y. Specific duodenal and faecal bacterial groups associated with paediatric coeliac disease. J Clin Pathol. Di Cagno R, Rizzello CG, Gagliardi F, Ricciuti P, Ndagijimana M, Francavilla R, et al. Different fecal microbiotas and volatile organic compounds in treated and untreated children with celiac disease. Appl Environ Microbiol. Nistal E, Caminero A, Vivas S, de Morales JMR, de Miera LES, Rodríguez-Aparicio LB, et al. Differences in faecal bacteria populations and faecal bacteria metabolism in healthy adults and celiac disease patients. De Palma G, Nadal I, Collado MC, Sanz Y. Effects of a gluten-free diet on gut microbiota and immune function in healthy adult human subjects. Br J Nutr. Article PubMed Google Scholar. David LA, Maurice CF, Carmody RN, Gootenberg DB, Button JE, Wolfe BE, et al. Diet rapidly and reproducibly alters the human gut microbiome. Article CAS PubMed PubMed Central Google Scholar. Tigchelaar EF, Zhernakova A, Dekens JAM, Hermes G, Baranska A, Mujagic Z, et al. An Introduction to LifeLines DEEP: Study Design and Baseline Characteristics. Cold Spring Harbor Labs J. Baranska A, Tigchelaar E, Smolinska A, Dallinga JW, Moonen EJC, Dekens JAM, et al. Profile of volatile organic compounds in exhaled breath changes as a result of gluten-free diet. J Breath Res. Caporaso JG, Kuczynski J, Stombaugh J, Bittinger K, Bushman FD, Costello EK. QIIME allows analysis of high-throughput community sequencing data. Nat Methods. Edgar RC. Search and clustering orders of magnitude faster than BLAST. DeSantis TZ, Hugenholtz P, Larsen N, Rojas M, Brodie EL, Keller K, et al. Greengenes, a chimera-checked 16S rRNA gene database and workbench compatible with ARB. Brandt BW, Bonder MJ, Huse SM, Zaura E. TaxMan: a server to trim rRNA reference databases and inspect taxonomic coverage. Nucleic Acids Res. Bonder MJ, Abeln S, Zaura E, Brandt BW. Comparing clustering and pre-processing in taxonomy analysis. May A, Abeln S, Crielaard W, Heringa J, Brandt BW. Unraveling the outcome of 16S rDNA-based taxonomy analysis through mock data and simulations. Ding T, Schloss PD. Dynamics and associations of microbial community types across the human body. Langille MGI, Zaneveld J, Caporaso JG, McDonald D, Knights D, Reyes J, et al. Predictive functional profiling of microbial communities using 16S rRNA marker gene sequences. Nat Biotechnol. Abubucker S, Segata N, Goll J, Schubert AM, Izard J, Cantarel BL, et al. Metabolic reconstruction for metagenomic data and its application to the human microbiome. PLoS Comput Biol. Tickle T, Waldron L, Yiren Lu, Huttenhower C. Multivariate association of microbial communities with rich metadata in high-dimensional studies. In progress. Google Scholar. R Development Core Team RFFSC. R: A Language and Environment for Statistical Computing. R Foundation for Statistical Computing. Vienna: R Development; Dabney A, Storey JD, qvalue Tutorial PRS, Install R, Packages IB, Packages UB, Vignettes P, Cloud AMI, Team C. Q-value estimation for false discovery rate control. Tibble JA, Sigthorsson G, Foster R, Scott D, Fagerhol MK, Roseth A, et al. High prevalence of NSAID enteropathy as shown by a simple faecal test. Joshi S, Lewis SJ, Creanor S, Ayling RM. Age-related faecal calprotectin, lactoferrin and tumour M2-PK concentrations in healthy volunteers. Ann Clin Biochem. Maheshwari A, Lu W, Lacson A, Barleycorn AA, Nolan S, Christensen RD, et al. Effects of interleukin-8 on the developing human intestine. Harder J, Bartels J, Christophers E, Schröder JM. A peptide antibiotic from human skin. Langhorst J, Junge A, Rueffer A, Wehkamp J, Foell D, Michalsen A, et al. Elevated human beta-defensin-2 levels indicate an activation of the innate immune system in patients with irritable bowel syndrome. Am J Gastroenterol. El-Salhy M, Lomholt-Beck B, Hausken T. Chromogranin A as a possible tool in the diagnosis of irritable bowel syndrome. Scand J Gastroenterol. Sidhu R, Drew K, McAlindon ME, Lobo AJ, Sanders DS. Elevated serum chromogranin A in irritable bowel syndrome IBS and inflammatory bowel disease IBD : a shared model for pathogenesis? Inflamm Bowel Dis. Ohman L, Stridsberg M, Isaksson S, Jerlstad P, Simrén M. Altered levels of fecal chromogranins and secretogranins in IBS: relevance for pathophysiology and symptoms? Hamer HM, Jonkers D, Venema K, Vanhoutvin S, Troost FJ, Brummer R-J. Review article: the role of butyrate on colonic function. Aliment Pharmacol Ther. Windmueller HG, Spaeth AE. Source and fate of circulating citrulline. Am J Physiol. CAS PubMed Google Scholar. Crenn P, Messing B, Cynober L. Citrulline as a biomarker of intestinal failure due to enterocyte mass reduction. Clin Nutr. Le Chatelier E, Nielsen T, Qin J, Prifti E, Hildebrand F, Falony G, et al. Richness of human gut microbiome correlates with metabolic markers. Brock M, Maerker C, Schütz A, Völker U, Buckel W. Oxidation of propionate to pyruvate in Escherichia coli: Involvement of methylcitrate dehydratase and aconitase. Eur J Biochem. Kang D-W, Park JG, Ilhan ZE, Wallstrom G, LaBaer J, Adams JB, et al. Reduced incidence of prevotella and other fermenters in intestinal microflora of autistic children. PLoS One. Gevers D, Kugathasan S, Denson LA, Vázquez-Baeza Y, Van Treuren W, Ren B, et al. Cell Host Microbe. Haberman Y, Tickle TL, Dexheimer PJ, Kim M, Tang D, Karns R, et al. Pediatric Crohn disease patients exhibit specific ileal transcriptome and microbiome signature. J Clin Invest. Shukla R, Ghoshal U, Dhole TN, Ghoshal UC. Fecal microbiota in patients with irritable bowel syndrome compared with healthy controls using real-time polymerase chain reaction: an evidence of dysbiosis. Dig Dis Sci. Ze X, Duncan SH, Louis P, Flint HJ. Ruminococcus bromii is a keystone species for the degradation of resistant starch in the human colon. ISME J. Walker AW, Ince J, Duncan SH, Webster LM, Holtrop G, Ze X, et al. Dominant and diet-responsive groups of bacteria within the human colonic microbiota. Rajilić-Stojanović M. Function of the microbiota. Best Pract Res Clin Gastroenterol. Aziz I, Trott N, Briggs R, North JR, Hadjivassiliou M, Sanders DS. Clin Gastroenterol Hepatol. doi: Tigchelaar EF, Bonder MJ, Jankipersadsing SA, Fu J, Wijmenga C, Zhernakova A. Gut microbiota composition associated with stool consistency. Maukonen J, Kolho K-L, Paasela M, Honkanen J, Klemetti P, Vaarala O, et al. Altered fecal microbiota in paediatric inflammatory bowel disease. J Crohns Colitis. Chen W, Liu F, Ling Z, Tong X, Xiang C. Human intestinal lumen and mucosa-associated microbiota in patients with colorectal cancer. In the review, gluten-free foods were on average found to be lower in protein and dietary fibre, but higher in fat and salt compared to their equivalent gluten-containing products. Although, in somewhat good news, there does seem to be a growing trend towards increasing the fibre content of these products. quinoa grains. We also see this first hand at The Gut Health Clinic. Even when following a strict gluten-free diet, several studies have still reported people with coeliac disease are at a higher risk of micronutrient deficiencies. Taken together, making an effort to maximise key nutrients in a gluten-free diet is super important for not only helping to restore the diversity of the GM and remember, having a more diverse GM is linked with better health outcomes , but also to get enough micronutrients. Here are our top tips to help you follow a nutrient dense gluten-free diet for those with coeliac disease:. There are so many naturally gluten-free grains that are more accessible now than ever before quinoa, gluten-free oats, corn, buckwheat, amaranth, teff, wild rice etc. Your gut will thank you! Fill up on fibre. Aim for 30g of fibre a day from all 6 different plant-based food groups. Eat lots of variety — the more, the merrier. Tuck into a full range of food groups, across fruit, vegetables, potatoes, nuts, seeds, beans, pulses, herbs and spices, fish, eggs, fermented dairy and lean meats. Gibson, P. Gluten Causes Gastrointestinal Symptoms in Subjects Without Celiac Disease: A Double-Blind Randomized Placebo-Controlled Trial. The American Journal of Gastroenterology, 3 , Campbell SC, Wisniewski PJ, Noji M, McGuinness LR, Häggblom MM, Lightfoot SA, et al. The Effect of Diet and Exercise on Intestinal Integrity and Microbial Diversity in Mice. PLoS ONE 11 3. Rachel Allen is a writer at Hyperbiotics who's absolutely obsessed with learning about how our bodies work. She's fascinated by the latest research on bacteria and the role they play in health, and loves to help others learn about how probiotics can help the body get back in balance. For more ideas on how you can benefit from the power of probiotics and live healthier days, be sure to subscribe to our newsletter. To learn more about how a healthy microbiome can enrich your life, subscribe to our newsletter. Item added to your cart. Check out Continue shopping. So, what does that actually mean for you? Your gut on gluten, according to science: Many studies have been done on the effects of gluten on gut health, including one that found that mice who were fed a gluten-free diet had significantly more of several types of important gut bacteria than those who were fed a diet containing gluten. Learn to love your microbes. Move in ways that make you feel good. Experiment with your eating. Get your doctor in the game. Give your gut a boost with a probiotic. All pretty doable, right? |
Ich verstehe etwas nicht