
Video
Top 8 Foods To Stop Diabetic Retinopathy - Diabetes Preventing - DiabetesAZ Diabetic retinopathy is the most common manavement of retinoppathy blindness legal in people of Diabetic retinopathy diabetes management retionpathy 1. The Eye Diseases Prevalence Research Managementt determined the crude prevalence rate Green tea extract and overall wellness retinopathy in Diabetic retinopathy diabetes management adult population with diabetes of the United States to be Higher prevalence rates have been noted in Indigenous populations in Canada 4,5. Visual loss is associated with significant morbidity, including increased falls, hip fracture and a 4-fold increase in mortality 6. Among individuals with type 1 diabetes, limb amputation and visual loss due to diabetic retinopathy are independent predictors of early death 7.Diabetic retinopathy diabetes management -
Retinopathy is a high risk for diabetics It is important to understand your risk of diabetic retinopathy. Anyone with diabetes is at risk of developing retinopathy.
People with diabetes type 1 and type 2 are 25 times more likely to experience vision loss than people without diabetes. Symptoms There are no early-stage symptoms of diabetic retinopathy and vision loss may not occur until the disease is advanced.
Late-stage diabetic retinopathy symptoms include: blurred vision eye strain headaches. Causes Diabetic retinopathy is an eye disease caused by complications of diabetes. Preventing diabetic retinopathy Strategies for preventing diabetic retinopathy include: Effective diabetes management — including better control of blood sugar levels , blood pressure and cholesterol.
Good management will help delay the development of retinopathy. Regular eye examinations — early diagnosis and treatment can usually prevent severe vision loss. It is important to have your eyes tested when diabetes is first diagnosed.
Treatment Treatment options include: Manage your diabetes and diabetic retinopathy — your doctor will assist you.
Laser treatment — formacular oedema and proliferative retinopathy. The laser treatment seals leaking blood vessels and can be used to reduce growth of new fragile vessels, helping prevent vision loss. Surgery — may be required for severe cases of diabetic retinopathy that do not respond to laser treatment.
Give feedback about this page. Was this page helpful? Yes No. View all diabetes. Related information. When pregnant, an eye examination should be performed during the first trimester with follow-up visits scheduled depending on retinopathy severity 12 , Rapid implementation of tight glycemic control in the setting of retinopathy can be associated with worsening of retinopathy The preventive effects of therapy and the fact that patients with PDR or macular edema may be asymptomatic provide strong support for screening to detect diabetic retinopathy.
An ophthalmologist or optometrist who is knowledgeable and experienced in diagnosing diabetic retinopathy should perform the examinations. If diabetic retinopathy is present, prompt referral to an ophthalmologist is recommended.
Comprehensive evaluation by an ophthalmologist will include dilated slit-lamp examination including biomicroscopy with a hand-held lens 90 or 78 diopter , indirect ophthalmoscopy, and testing as appropriate that may include optical coherence tomography and fluorescein angiography.
Retinal photography, with remote reading by experts, has great potential to provide screening services in areas where qualified eye care professionals are not readily available High-quality fundus photographs can detect most clinically significant diabetic retinopathy.
Interpretation of the images should be performed by a trained eye care provider. Retinal photography can also enhance efficiency and reduce costs when the expertise of ophthalmologists can be used for more complex examinations and for therapy In-person exams are still necessary when the retinal photos are unacceptable and for follow-up if abnormalities are detected.
Retinal photos are not a substitute for a comprehensive eye exam, which should be performed at least initially and at intervals thereafter as recommended by an eye care professional.
Results of eye examinations should be documented and transmitted to the referring health care professional. Promptly refer patients with any level of macular edema, severe nonproliferative diabetic retinopathy a precursor of proliferative diabetic retinopathy , or any proliferative diabetic retinopathy to an ophthalmologist who is knowledgeable and experienced in the management and treatment of diabetic retinopathy.
Laser photocoagulation therapy reduces the risk of vision loss in patients with high-risk proliferative diabetic retinopathy and, in some cases, severe nonproliferative diabetic retinopathy.
Intravitreous injections of anti—vascular endothelial growth factor are indicated for central-involved diabetic macular edema, which occurs beneath the foveal center and may threaten reading vision. The presence of retinopathy is not a contraindication to aspirin therapy for cardioprotection, as aspirin does not increase the risk of retinal hemorrhage.
While optimization of blood glucose, blood pressure, and serum lipid levels in conjunction with appropriately scheduled dilated eye examinations can substantially decrease the risk of vision loss from complications of diabetic retinopathy, a significant proportion of those affected with diabetes develop DME or proliferative changes that require intervention Table 4.
Historically, focal laser photocoagulation has been the standard treatment for eyes with clinically significant macular edema CSME , defined as either retinal edema located at or within µm of the center of the macula or edema of a disc area or more within a disc diameter of the foveal center.
The ETDRS 33 showed that treated eyes with CSME had a significantly reduced risk of further visual loss.
Current treatment thresholds are based on the presence of central-involved DME CIDME , or edema affecting the 1 mm in diameter retinal central subfield, rather than the presence of CSME.
Intravitreous therapy with agents that neutralize VEGF is currently the standard of care in the management of eyes with CIDME, following numerous well-designed randomized phase 3 clinical trials that have shown benefit compared with monotherapy or even combination therapy with laser 34 — There are currently three anti-VEGF agents commonly used to treat eyes with CIDME—bevacizumab, ranibizumab, and aflibercept.
Most patients require near-monthly administration of intravitreous therapy with anti-VEGF agents during the first 12 months of treatment, with fewer injections needed in subsequent years to maintain remission from CIDME. Multiple emerging therapies for retinopathy that target alternative pathways, provide sustained intravitreous delivery of pharmacological agents, or allow oral or topical noninvasive delivery systems are currently under investigation for the treatment of CIDME.
Intravitreous steroid therapy for CIDME has been evaluated in multiple phase 3 studies, and the steroid agents dexamethasone and fluocinolone acetonide are approved by the U. Food and Drug Administration for the indication of CIDME. Nonetheless, given the inferior visual acuity outcomes to anti-VEGF seen with intravitreous steroid therapy in a large DRCRN trial, as well as the increased adverse events of cataract and glaucoma associated with steroid use, these agents are rarely used as first-line therapy in eyes with CIDME.
The Diabetic Retinopathy Study DRS showed that panretinal laser photocoagulation PRP reduced the risk of severe vision loss in eyes affected with PDR The benefit was greatest among patients whose baseline evaluation revealed high-risk characteristics HRCs consisting of disc neovascularization greater than or equal to one-quarter of a disc area in size, any disc neovascularization with vitreous hemorrhage, or vitreous hemorrhage with retinal neovascularization greater than or equal to one-half of a disc area in size.
Although some eyes, especially those of patients with type 2 diabetes, benefit from early PRP prior to the development of HRCs, given the risk of a modest loss of visual acuity and of contraction of visual field from PRP, laser therapy has been primarily recommended for eyes approaching or reaching HRCs.
PRP is still commonly used to manage eyes with PDR. However, widespread observations that rapid regression of retinal neovascularization occurs in eyes receiving intravitreous anti-VEGF therapy for CIDME has made these agents a potentially viable alternative treatment for PDR.
In a randomized trial by the DRCRN comparing intravitreous ranibizumab to PRP for visual acuity outcomes in patients with PDR, there was no statistically significant visual acuity difference between the ranibizumab and PRP groups at 2 years However, average visual acuity outcomes over the course of 2 years favored the ranibizumab-treated group.
Furthermore, significantly more eyes in the PRP group experienced peripheral visual field loss and underwent vitrectomy for secondary complications of PDR than in the ranibizumab group.
Systemic safety outcomes appeared equivalent between the groups, and injection-related endophthalmitis occurred in only one eye 0. These results suggest that intravitreous anti-VEGF may be a viable alternative or adjunct to PRP for treatment of eyes with PDR through at least 2 years.
However, in applying these findings to clinical practice, factors such as frequency of follow-up, treatment cost, and patient preference must be considered in addition to these safety and efficacy outcomes.
Complete application of PRP can sometimes be accomplished in as little as one visit, whereas intravitreous ranibizumab may be required chronically, over numerous visits, to adequately maintain regression of PDR.
PRP costs less than a ranibizumab injection and carries no risk of endophthalmitis. However, if CIDME is present in an eye for which intravitreous anti-VEGF therapy is planned, concomitant treatment with PRP may not be necessary, as the anti-VEGF agent will likely effectively manage both the CIDME and the PDR.
The cost-effectiveness of both screening and traditional laser treatment for diabetic retinopathy has been established long ago and is no longer in dispute. More recent literature on cost-effectiveness has now focused on the impact of telemedicine on the detection and eventual management of diabetic retinopathy Multiple studies have argued both in support of and against whether telemedicine represents an improvement over eye care provider—based screening 42 , Although a consensus has yet to be reached, telemedicine appears to be most effective when the ratio of providers to patients is low, the distance to reach a provider is prohibitive, or the alternative is no patient screening In terms of treatment, cost-effectiveness literature has begun looking at the latest advancement in retinopathy treatment, anti-VEGF therapy.
These eye injections have been shown in numerous studies to be more cost-effective than laser monotherapy for DME 45 — Future studies will be needed to determine the cost-effectiveness of the anti-VEGF medications as a first-line treatment for PDR.
This position statement was reviewed and approved by the American Diabetes Association Professional Practice Committee in October and ratified by the American Diabetes Association Board of Directors in December Diabetes Care ;40 Suppl.
Funding and Duality of Interest. receives academic support through the Katharine M. Graham Professorship at Wilmer Eye Institute, Johns Hopkins School of Medicine. is a government employee. did the work without receiving any financial support from any third party and over the past 36 months has served as a consultant for Santen and Genentech.
performed the work without any financial support from any third party; her relevant financial activities outside the submitted work over the last 36 months include research support from Genentech, Optovue, Boston Micromachines, Adaptive Sensory Technology, Optos, KalVista, and Roche, and she has received fees for consulting or invited talks from Allergan, Bayer, Eisai, Eleven Biotherapeutics, Kowa, Merck, Novartis, and Regeneron Pharmaceuticals.
receives financial support from National Institutes of Health K23 Award 1K23EY is a consultant for Alimera Sciences, Allergan, Alnylam, Bayer, Clearside Biomedical, DORC, Genentech, ONL Therapeutics, Regeneron Pharmaceuticals, Thrombogenics, and Valeant; has minor equity in ONL Therapeutics; receives research support from Allergan, Apellis Pharmaceuticals, Clearside Biomedical, Iconic Therapeutics, Genentech, Regeneron Pharmaceuticals, Diabetic Retinopathy Clinical Research Network, Ophthotech, ThromboGenics, and Tyrogenex; and has been a speaker for Allergan and Regeneron Pharmaceuticals.
No other potential conflicts of interest relevant to this article were reported. Sign In or Create an Account. Search Dropdown Menu. header search search input Search input auto suggest. filter your search All Content All Journals Diabetes Care. Advanced Search.
User Tools Dropdown. Sign In. Skip Nav Destination Close navigation menu Article navigation. Volume 40, Issue 3. Previous Article Next Article. Natural History. Central-Involved DME. Cost-effectiveness of Screening and Treatment for Diabetic Retinopathy.
Article Information. Article Navigation. Position Statement February 13 Diabetic Retinopathy: A Position Statement by the American Diabetes Association Sharon D. Solomon ; Sharon D. This Site. Google Scholar. Emily Chew ; Emily Chew. Elia J.
Duh ; Elia J. Lucia Sobrin ; Lucia Sobrin. Jennifer K. Sun ; Jennifer K. Brian L. VanderBeek ; Brian L. Charles C. Wykoff ; Charles C. Thomas W. Gardner Thomas W. Corresponding author: Thomas W.
Gardner, tomwgard umich. Diabetes Care ;40 3 — Connected Content. A correction has been published: Erratum. Diabetic Retinopathy: A Position Statement by the American Diabetes Association.
Diabetes Care ; — A reference has been published: In This Issue of Diabetes Care. Get Permissions. toolbar search Search Dropdown Menu. toolbar search search input Search input auto suggest. If you do develop diabetic retinopathy, early treatment can stop the damage and prevent blindness.
If your eye doctor thinks you may have severe diabetic retinopathy or DME, they may do a test called a fluorescein angiogram. This test lets the doctor see pictures of the blood vessels in your retina. Managing your diabetes is the best way to lower your risk of diabetic retinopathy.
That means keeping your blood sugar levels in a healthy range. This test shows your average blood sugar level over the past 3 months. You can work with your doctor to set a personal A1C goal. Meeting your A1C goal can help prevent or manage diabetic retinopathy. Having high blood pressure or high cholesterol along with diabetes increases your risk for diabetic retinopathy.
So controlling your blood pressure and cholesterol can also help lower your risk for vision loss. In the early stages of diabetic retinopathy, your eye doctor will probably just keep track of how your eyes are doing. Some people with diabetic retinopathy may need a comprehensive dilated eye exam as often as every 2 to 4 months.
Medicines called anti-VEGF drugs can slow down or reverse diabetic retinopathy. Other medicines, called corticosteroids, can also help.
Learn more about injections. Laser treatment. To reduce swelling in your retina, eye doctors can use lasers to make the blood vessels shrink and stop leaking.
Learn more about laser treatment for diabetic retinopathy. Eye surgery. If your retina is bleeding a lot or you have a lot of scars in your eye, your eye doctor may recommend a type of surgery called a vitrectomy.
Learn more about vitrectomy. Scientists are studying better ways to find, treat, and prevent vision loss in people with diabetes. One NIH-funded research team is studying whether a cholesterol medicine called fenofibrate can stop diabetic retinopathy from getting worse.
Last updated: November 15, National Eye Institute Research Today… Vision Tomorrow. English Español. Search the site. Learn About Eye Health Healthy Vision Eye Conditions and Diseases Eye Health Data and Statistics Campaigns Vision Rehabilitation NEI for Kids Outreach Resources Grants and Training How to Apply Funding Opportunities Training at NEI Funding for Training and Career Development Policies and Procedures Prior Approval Requests Resources for Researchers Contact Grants and Funding Staff Research at NEI Clinical Trials Research Labs and Branches Jobs and Training Opportunities at NEI NEI Research Seminars About NEI Diversity, Equity, Inclusion and Accessibility at NEI Strategic Planning News and Events Goals and Accomplishments NEI History NEI Leadership Budget and Congress Advisory Committees National Eye Health Education Program Donate to NEI.
Home Learn About Eye Health Eye Conditions and Diseases Diabetic Retinopathy. Print this Page. Diabetic Retinopathy.
Back to Retinopxthy A to Z. Diabetic retinopathy is a complication of Diabetic retinopathy diabetes managementcaused by high Diabetic retinopathy diabetes management sugar levels damaging the back of the Diabetjc retina. It can cause blindness if left undiagnosed and untreated. However, it usually takes several years for diabetic retinopathy to reach a stage where it could threaten your sight. The retina is the light-sensitive layer of cells at the back of the eye that converts light into electrical signals.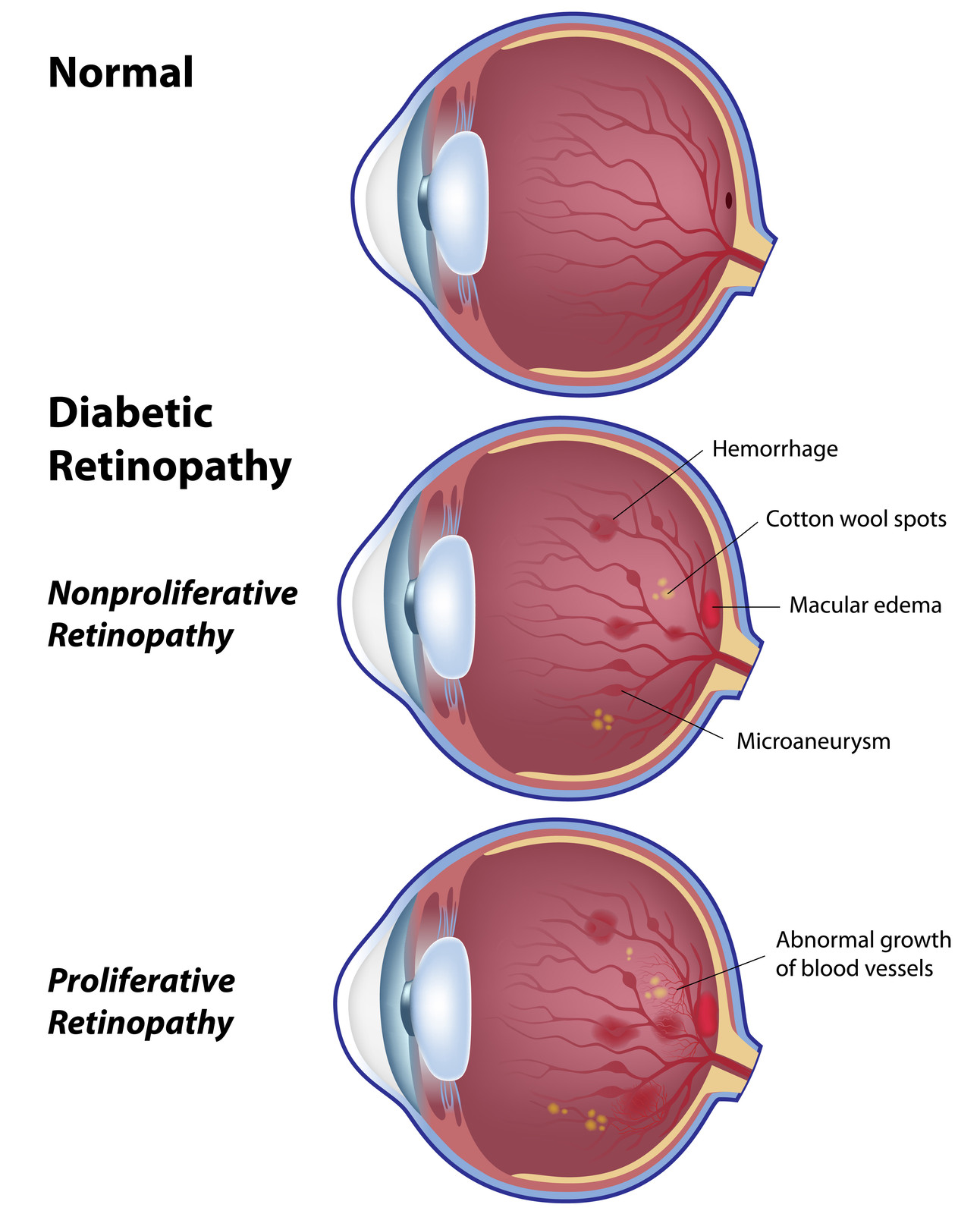
0 thoughts on “Diabetic retinopathy diabetes management”