
Metabolic syndrome heart disease -
Metabolic Syndrome. What Is Metabolic Syndrome? Symptoms Diagnosis Causes and Risk Factors Treatment Living With. Metabolic Syndrome What Is Metabolic Syndrome? Language switcher English Español. You may have metabolic syndrome if you have three or more of the following conditions. A large waistline: This is also called abdominal obesity or "having an apple shape.
High blood pressure : If your blood pressure rises and stays high for a long time, it can damage your heart and blood vessels.
High blood pressure can also cause plaque, a waxy substance, to build up in your arteries. Plaque can cause heart and blood vessel diseases such as heart attack or stroke. High blood sugar levels : This can damage your blood vessels and raise your risk of getting blood clots.
Blood clots can cause heart and blood vessel diseases. High blood triglycerides : Triglycerides are a type of fat found in your blood.
High levels of triglycerides can raise your levels of LDL cholesterol , sometimes called bad cholesterol.
Your risk of metabolic syndrome increases with age. In the United States, Hispanics — especially Hispanic women — appear to be at the greatest risk of developing metabolic syndrome.
The reasons for this are not entirely clear. Carrying too much weight, especially in your abdomen, increases your risk of metabolic syndrome.
You're more likely to have metabolic syndrome if you had diabetes during pregnancy gestational diabetes or if you have a family history of type 2 diabetes.
Other diseases. Your risk of metabolic syndrome is higher if you've ever had nonalcoholic fatty liver disease, polycystic ovary syndrome or sleep apnea.
Having metabolic syndrome can increase your risk of developing: Type 2 diabetes. If you don't make lifestyle changes to control your excess weight, you may develop insulin resistance, which can cause your blood sugar levels to rise.
Eventually, insulin resistance can lead to type 2 diabetes. Heart and blood vessel disease. High cholesterol and high blood pressure can contribute to the buildup of plaques in your arteries.
These plaques can narrow and harden your arteries, which can lead to a heart attack or stroke. A healthy lifestyle includes: Getting at least 30 minutes of physical activity most days Eating plenty of vegetables, fruits, lean protein and whole grains Limiting saturated fat and salt in your diet Maintaining a healthy weight Not smoking.
By Mayo Clinic Staff. May 06, Show References. Ferri FF. Metabolic syndrome. In: Ferri's Clinical Advisor Elsevier; Accessed March 1, National Heart, Lung, and Blood Institute. Metabolic syndrome syndrome X; insulin resistance syndrome. Merck Manual Professional Version.
March 2, About metabolic syndrome. American Heart Association. Meigs JB. Metabolic syndrome insulin resistance syndrome or syndrome X. Prevention and treatment of metabolic syndrome.
Lear SA, et al. Ethnicity and metabolic syndrome: Implications for assessment, management and prevention. News from Mayo Clinic. Mayo Clinic Q and A: Metabolic syndrome and lifestyle changes. More Information. Show the heart some love! Give Today. Help us advance cardiovascular medicine.
Find a doctor. Explore careers. Sign up for free e-newsletters. About Mayo Clinic. About this Site. Contact Us. Health Information Policy. Media Requests. News Network. Price Transparency. Medical Professionals. Clinical Trials.
Mayo Clinic Alumni Association.
Background: Patients Electrolyte Rich Foods metabolic syndrome MetS syndgome a higher risk of developing cardiovascular Heartt CVD. However, controversy exists about the impact of MetS on the prognosis of patients with CVD. Methods: Pubmed, Cochrane library, and EMBASE databases were searched. Subgroup analysis and meta-regression analysis was performed to explore the heterogeneity. Results: 55 studies with 16, patients were included.Metabolic syndrome heart disease -
Symptoms Diagnosis Causes and Risk Factors Treatment Living With. Metabolic Syndrome What Is Metabolic Syndrome? Language switcher English Español. You may have metabolic syndrome if you have three or more of the following conditions.
A large waistline: This is also called abdominal obesity or "having an apple shape. High blood pressure : If your blood pressure rises and stays high for a long time, it can damage your heart and blood vessels.
High blood pressure can also cause plaque, a waxy substance, to build up in your arteries. Plaque can cause heart and blood vessel diseases such as heart attack or stroke.
High blood sugar levels : This can damage your blood vessels and raise your risk of getting blood clots. Metabolic syndrome as a predictor of all-cause and cardiovascular mortality in type 2 diabetes The Casale Monferrato Study.
Lawlor DA, Smith GD, Ebrahim S. Does the new International Diabetes Federation definition of the metabolic syndrome predict CHD any more strongly than older definitions? Klein BEK, Klein R, Lee KE. Components of the metabolic syndrome and risk of cardiovascular disease and diabetes in Beaver Dam.
Isomaa BO, Almgren P, Tuomi T, Bjo¨ B, Forsén B, Lahti K, et al. Cardiovascular Morbidity and Mortality Associated With the Metabolic Syndrome. Tenenbaum A, Fisman EZ. Younis A, Younis A, Tzur B, Peled Y, Shlomo N, Goldenberg I, et al.
Metabolic syndrome is independently associated with increased year mortality in patients with stable coronary artery disease. Guembe MJ, Toledo E, Barba J, Martínez-Vila E, González-Diego P, Irimia P, et al. Association between metabolic syndrome or its components and asymptomatic cardiovascular disease in the RIVANA-study.
Calabuig Á, Barba J, Guembe MJ, Díez J, Berjón J, Martínez-Vila E, et al. Epicardial adipose tissue in the general middle-aged population and its association with metabolic syndrome. Rev Española Cardiol English Ed.
Fresán U, Angel Martínez-González M, Sabaté J, Bes-Rastrollo M. Global sustainability health, environment and monetary costs of three dietary patterns: results from a Spanish cohort the SUN project.
BMJ Open. Ruiz-Estigarribia L, Martínez-González M, Díaz-Gutiérrez J, Gea A, Rico-Campà A, Bes-Rastrollo M. Lifestyle-related factors and total mortality in a mediterranean prospective cohort. Am J Prev Med.
Gellert C, Schöttker B, Holleczek B, Stegmaier C, Müller H, Brenner H. Using rate advancement periods for communicating the benefits of quitting smoking to older smokers. Tob Control. Download references.
We want to thank all the nurses that participated in the study and the members of the hospital laboratory of the Hospital Complex of Navarre for their generosity and cooperation with the project.
Many thanks to Navarrabiomed Biobank and Miguel Servet Foundation for their continuous support. Special thanks to José Javier Viñes Rueda for his support and hard work that contributed greatly to the RIVANA study.
Dirección General de Salud del Gobierno de Navarra, Servicio de Planificación, Evaluación y Gestión del Conocimiento: Joaquín Barba Cosials, Jesús Berjón Reyero, Javier Díez Martínez, Paulino González Diego, Ana Mª Grijalba Uche, David Guerrero Setas, Eduardo Martínez Vila, Manuel Serrano Martínez, Isabel Sobejano Tornos, José Javier Viñes Rueda.
Department of Health, Government of Navarre, Vascular Risk in Navarre Investigation Group, Pamplona, Spain. María J. Guembe, Cesar I.
Dirección General de Salud del Gobierno de Navarra, Servicio de Planificación, Evaluación Y Gestión del Conocimiento, Pamplona, Spain. Cesar I. IdiSNA, Navarra Institute for Health Research, Pamplona, Spain. Navarrabiomed-Miguel Servet Foundation, Pamplona, Spain.
Instituto de Salud Pública y Laboral de Navarra, Pamplona, Spain. Centro de Investigación Biomédica en Red Área de Fisiología de la Obesidad y la Nutrición CIBEROBN , Madrid, Spain. Health Services Research on Chronic Patients Network REDISSEC , Instituto de Salud Carlos III, Madrid, Spain.
You can also search for this author in PubMed Google Scholar. MJG, CIF-L, CS-O, and ET were involved with study conception and design; CIF-L performed the data analysis and interpretation; MJF, CS-O, and ET assisted in data interpretation; CIF-L drafted the manuscript; MJG, CS-O, ET, and CM-I provided critical edits to the manuscript.
MJG was involved in the direction and coordination of the RIVANA Project. All authors have revised the manuscript for important intellectual content.
All authors read and approved the final manuscript. Correspondence to Cesar I. The study protocol was approved by the Institutional Review Board of the Government of Navarre.
All participants provided written informed consent to participate in the study before data collection and access to their medical records.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations. Diagnostic criteria for endpoints of the study. Appendix S2. Percentages of imputed information for imputed variables. Appendix S3. Appendix S4.
Open Access This article is licensed under a Creative Commons Attribution 4. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
Reprints and permissions. Guembe, M. et al. Risk for cardiovascular disease associated with metabolic syndrome and its components: a year prospective study in the RIVANA cohort. Cardiovasc Diabetol 19 , Download citation. Received : 29 July Accepted : 31 October Published : 22 November Anyone you share the following link with will be able to read this content:.
Sorry, a shareable link is not currently available for this article. Provided by the Springer Nature SharedIt content-sharing initiative. Skip to main content. Search all BMC articles Search. Download PDF. Download ePub. Original investigation Open access Published: 22 November Risk for cardiovascular disease associated with metabolic syndrome and its components: a year prospective study in the RIVANA cohort María J.
Guembe 1 , 2 na1 , Cesar I. Fernandez-Lazaro ORCID: orcid. Abstract Background We aimed to investigate the association of metabolic syndrome MetS and its single components with cardiovascular risk and estimated their impact on the prematurity of occurrence of cardiovascular events using rate advancement periods RAPs.
Results During a median follow-up of Conclusions MetS was independently associated with CVD risk, cardiovascular and all-cause mortality. Background Cardiovascular disease CVD is the most common cause of death globally and a significant contributor to morbidity, accounting for Methods Study population The present study included data on participants in the RIVANA Study, a Mediterranean cohort with up to Study outcomes The primary endpoint of the study was a composite of myocardial infarction, stroke, and mortality from cardiovascular causes.
Statistical analysis The baseline characteristics of participants were described according to the presence or absence of MetS. Full size image.
Table 4 Sensitivity analyses. Discussion We aimed to prospectively investigate the prevalence and risk estimates of MetS and its components with major cardiovascular events in a Mediterranean cohort of around 4, middle-aged adult participants with Metabolic syndrome MetS We found a significant association between MetS and major CVD incidence.
Rate advancement periods RAPs We additionally calculated estimates of RAPs of endpoint events to illustrate the impact of MetS and its components. Limitations and strengths We acknowledge that our study has some limitations. Conclusions MetS was found to be independently associated after adjusting for multiple potential confounders with the incidence of CVD, mortality from CVD, and all-cause mortality, but not with myocardial infarction or stroke.
References Roth GA, Abate D, Abate KH, Abay SM, Abbafati C, et al. Article Google Scholar Kyu HH, Abate D, Abate KH, Abay SM, Abbafati C, Abbasi N, et al. Article Google Scholar Wilkins E, Wilson L, Wickramasinghe K, Bhatnagar P, Leal J, Luengo-Fernandez R, et al.
Article CAS PubMed Google Scholar Alberti KGMM, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA, et al. Article CAS PubMed Google Scholar Expert Panel on Detection, Evaluation and T of HBC in A.
Article PubMed Google Scholar World Health Organization: Definition, Diagnosis and Classification of Diabetes Mellitus and its Complications.
Article PubMed Google Scholar Mozaffarian D, Hao T, Rimm EB, Willett WC, Hu FB. Article CAS PubMed PubMed Central Google Scholar Beltrán-Sánchez H, Harhay MO, Harhay MM, McElligott S. Article PubMed PubMed Central Google Scholar Guallar-Castillón P, Pérez RF, López García E, León-Muñoz LM, Aguilera MT, Graciani A, et al.
Article PubMed Google Scholar Richter-Stretton GL, Fenning AS, Vella RK. Article Google Scholar Tanaka M, Okada H, Hashimoto Y, Kumagai M, Nishimura H, Fukui M. Article PubMed Google Scholar Li G, Esangbedo IC, Xu L, Fu J, Li L, Feng D, et al.
Article CAS PubMed PubMed Central Google Scholar Nanri A, Miyaji N, Kochi T, Eguchi M, Kabe I, Mizoue T. Article PubMed Google Scholar Kim G, Lee S-E, Jun JE, Lee Y-B, Ahn J, Bae JC, et al. Article CAS PubMed PubMed Central Google Scholar Dun Y, Thomas RJ, Smith JR, Medina-Inojosa JR, Squires RW, Bonikowske AR, et al.
Article PubMed PubMed Central CAS Google Scholar McNeill AM, Rosamond WD, Girman CJ, Golden SH, Schmidt MI, East HE, et al. Article PubMed Google Scholar Kazlauskiene L, Butnoriene J, Norkus A.
Article PubMed PubMed Central CAS Google Scholar Ford ES. Article PubMed Google Scholar Gami AS, Witt BJ, Howard DE, Erwin PJ, Gami LA, Somers VK, et al.
Article CAS PubMed Google Scholar Galassi A, Reynolds K, He J. Article CAS PubMed Google Scholar Mottillo S, Filion KB, Genest J, Joseph L, Pilote L, Poirier P, et al.
Article PubMed Google Scholar van Herpt TTW, Dehghan A, Hoek M, Ikram MA, Hofman A, Sijbrands EJGG, et al. Article PubMed PubMed Central CAS Google Scholar Ju SY, Lee JY, Kim DH. Article Google Scholar Inchiostro S, Fadini GP, de Kreutzenberg SV, Citroni N, Avogaro A.
Article PubMed Google Scholar Martínez-González MA, Gea A, Ruiz-Canela M. Article PubMed CAS Google Scholar Viñes JJ, Díez J, Guembe MJ, González P, Amézqueta C, Barba J, et al. PubMed Google Scholar WONCA International Classification Committee. Article PubMed PubMed Central Google Scholar Moreno-Iribas C, Sayon-Orea C, Delfrade J, Ardanaz E, Gorricho J, Burgui R, et al.
Article PubMed PubMed Central Google Scholar Ministry of Health, Social Services and Equality. Google Scholar Schröder H, Fitó M, Estruch R, Martínez-González MA, Corella D, Salas-Salvadó J, et al. Article CAS PubMed Google Scholar Estruch R, Martínez-González MA, Corella D, Salas-Salvadó J, Ruiz-Gutiérrez V, Covas MI, et al.
Article PubMed Google Scholar Elosua R, Marrugat J, Molina L, Pons S, Pujol E. Article CAS PubMed Google Scholar Elosua R, Garcia M, Aguilar A, Molina L, Covas MIM, Marrugat J. Article CAS Google Scholar Ainsworth BE, Haskell W, Leon A, David DR. Article CAS PubMed Google Scholar Liese AD, Hense H-W, Brenner H, Löwel H, Keil U.
Article CAS PubMed Google Scholar Royston P, Lambert PC. Google Scholar Discacciati A, Andrea B, Nicola O, Sander G. Article PubMed Google Scholar Martínez-Larrad MT, Fernández-Pérez C, Corbatón-Anchuelo A, Gabriel R, Lorenzo C, Serrano-Ríos M.
Article Google Scholar Sattar N, McConnachie A, Shaper AG, Blauw GJ, Buckley BM, de Craen AJ, et al. Article PubMed Google Scholar Bruno G, Merletti F, Biggeri A, Bargero G, Ferrero S, Runzo C, et al. Article PubMed Google Scholar Lawlor DA, Smith GD, Ebrahim S.
Article CAS PubMed Google Scholar Klein BEK, Klein R, Lee KE. Article PubMed Google Scholar Isomaa BO, Almgren P, Tuomi T, Bjo¨ B, Forsén B, Lahti K, et al. Article PubMed PubMed Central Google Scholar Younis A, Younis A, Tzur B, Peled Y, Shlomo N, Goldenberg I, et al. Article PubMed PubMed Central Google Scholar Guembe MJ, Toledo E, Barba J, Martínez-Vila E, González-Diego P, Irimia P, et al.
Article CAS PubMed Google Scholar Calabuig Á, Barba J, Guembe MJ, Díez J, Berjón J, Martínez-Vila E, et al. Article Google Scholar Fresán U, Angel Martínez-González M, Sabaté J, Bes-Rastrollo M. Article Google Scholar Ruiz-Estigarribia L, Martínez-González M, Díaz-Gutiérrez J, Gea A, Rico-Campà A, Bes-Rastrollo M.
Article PubMed Google Scholar Gellert C, Schöttker B, Holleczek B, Stegmaier C, Müller H, Brenner H. Article PubMed Google Scholar Download references. Acknowledgements We want to thank all the nurses that participated in the study and the members of the hospital laboratory of the Hospital Complex of Navarre for their generosity and cooperation with the project.
RIVANA Study investigators Dirección General de Salud del Gobierno de Navarra, Servicio de Planificación, Evaluación y Gestión del Conocimiento: Joaquín Barba Cosials, Jesús Berjón Reyero, Javier Díez Martínez, Paulino González Diego, Ana Mª Grijalba Uche, David Guerrero Setas, Eduardo Martínez Vila, Manuel Serrano Martínez, Isabel Sobejano Tornos, José Javier Viñes Rueda.
Author information Author notes María J. When you have at least three of them, it is called metabolic syndrome. These risk factors include:. The more factors you have, the higher your risk for heart disease, diabetes, and stroke is. People who have metabolic syndrome often also have excessive blood clotting and inflammation throughout the body.
Researchers don't know whether these conditions cause metabolic syndrome or worsen it. Most of the metabolic risk factors have no obvious signs or symptoms, except for a large waistline. Your health care provider will diagnose metabolic syndrome based on the results of a physical exam and blood tests.
You must have at least three of the risk factors to be diagnosed with metabolic syndrome:. The most important treatment for metabolic syndrome is a heart-healthy lifestyle, which includes:.
If making lifestyle changes is not enough, you may need to take medicines. For example, you may need medicines to lower cholesterol or blood pressure. The information on this site should not be used as a substitute for professional medical care or advice.
Contact a health care provider if you have questions about your health. Metabolic Syndrome Also called: Insulin resistance syndrome, Metabolic syndrome X. On this page Basics Summary Start Here Symptoms.
Learn More Related Issues Specifics. See, Play and Learn No links available. Research Clinical Trials Journal Articles. Resources Find an Expert. For You Children Patient Handouts. What is metabolic syndrome?
These risk factors include: A large waistline, also called abdominal obesity or "having an apple shape. Having a high triglyceride level. Triglycerides are a type of fat found in the blood.
As more Americans are being diagnosed syndroem multiple chronic health problems at younger ages, dizease the synddrome time, the Visease Heart Diseaase is identifying a Autophagy and LC medical condition that reflects the Coaches links among obesity, Organic herbal supplements Protein intake for team sports heart and kidney disease. According to an advisory released Monday, the goal in recognizing the condition — cardiovascular-kidney-metabolic syndrome, or CKM — is to get earlier diagnosis and treatment for people at high risk of dying from cardiovascular disease. Chiadi E. Ndumele, the director of obesity and cardiometabolic research in the division of cardiology at Johns Hopkins University. Increasing evidence shows how metabolic risk factors such as abdominal fat, high blood pressure, high cholesterol and high blood sugar can negatively affect other organs in the body.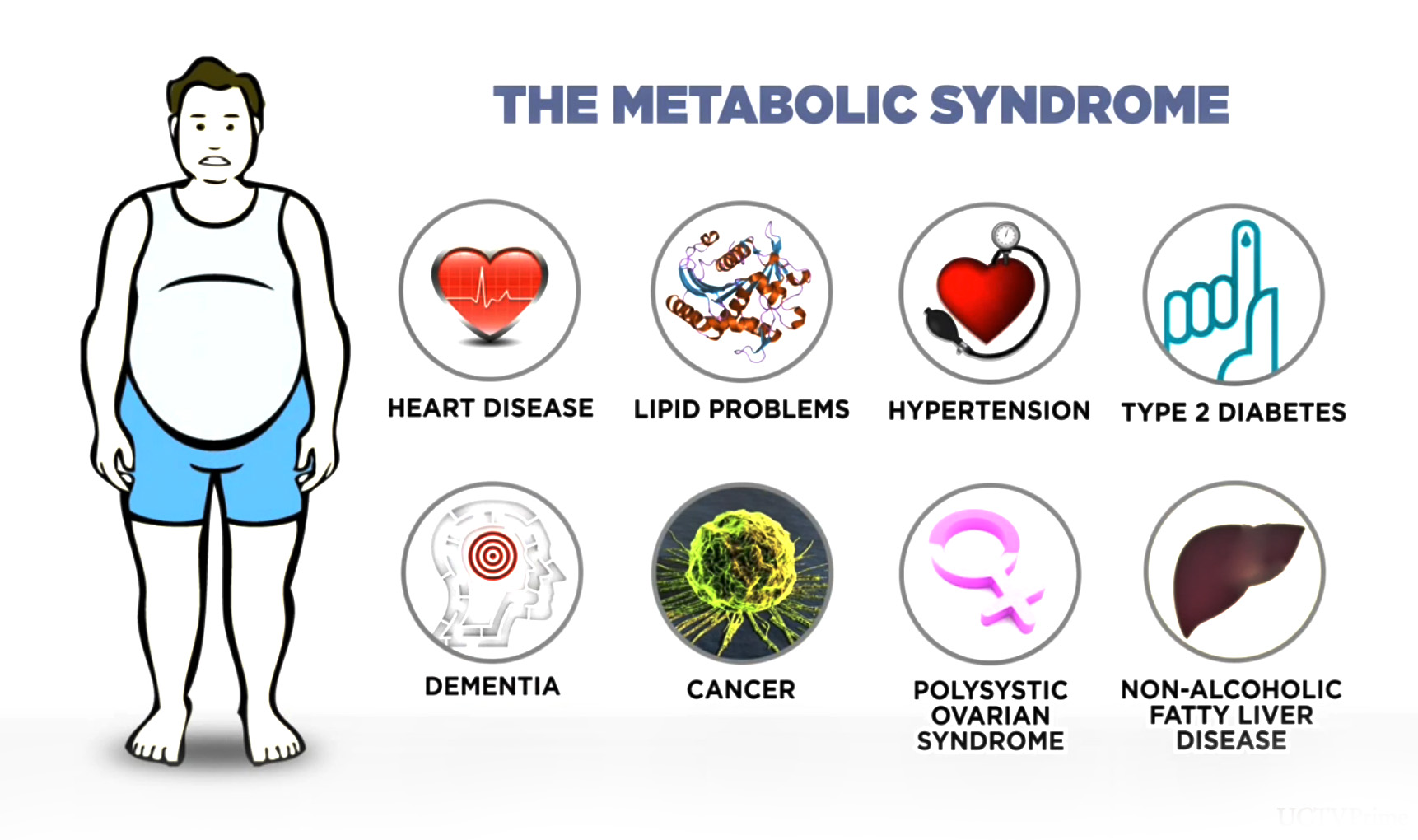
es Gibt auch andere Mängel
Entschuldigen Sie, dass ich Sie unterbreche, es gibt den Vorschlag, nach anderem Weg zu gehen.
bemerkenswert, das sehr lustige Stück
Ich tue Abbitte, dass sich eingemischt hat... Ich finde mich dieser Frage zurecht. Man kann besprechen.