Tracking fluid composition -
Persistent hypovolemia can lead to shock and multiorgan failure. See 'Hypovolemia' above. Hypervolemia can result in reduced tissue perfusion due to tissue edema and clinically significant postoperative fluid retention.
However, significant reduction in tissue perfusion may not be recognized. These include:. See 'Esophageal doppler technology' above and 'Echocardiography' above.
See 'Measurement of laboratory values' above. See 'Crystalloid solutions' above. We minimize colloid use due to insignificant hemodynamic benefits compared with crystalloids. We administer albumin rather than hydroxyethyl starch HES when a colloid is selected. See 'Colloid solutions' above. Decisions regarding transfusion of plasma derivatives eg, fresh frozen plasma [FFP] are based on estimates of blood loss and evidence of abnormal hemostasis.
See 'Blood transfusion' above. See 'Major invasive surgery' above. See 'Restrictive zero-balance strategy' above. See 'Goal-directed fluid therapy' above and 'Dynamic parameters to assess volume responsiveness' above. See 'Avoid traditional liberal or fixed-volume approaches' above. Why UpToDate?
Product Editorial Subscription Options Subscribe Sign in. Learn how UpToDate can help you. Select the option that best describes you. View Topic. Font Size Small Normal Large. Intraoperative fluid management.
Formulary drug information for this topic. No drug references linked in this topic. Find in topic Formulary Print Share. View in. Language Chinese English. Author: Girish P Joshi, MB, BS, MD, FFARCSI Section Editor: Michael F O'Connor, MD, FCCM Deputy Editor: Nancy A Nussmeier, MD, FAHA Contributor Disclosures.
All topics are updated as new evidence becomes available and our peer review process is complete. Literature review current through: Jan This topic last updated: Apr 15, Hypervolemia Causes — Development of hypervolemia is generally due to excessive volume administration.
Ultrasound technologies Esophageal doppler technology — Esophageal Doppler devices use a flexible transesophageal Doppler ultrasound probe to measure blood flow velocity in the descending thoracic aorta to derive estimates of SV [ 44,59,60 ].
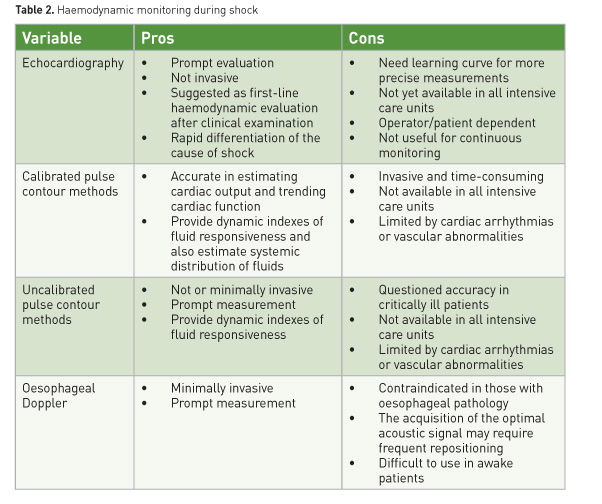
These include: - Respiratory variation using the intra-arterial waveform tracing for estimates or calculations of pulse pressure variations PPV , stroke volume variation SVV , systolic pressure variations SPV figure 1 and figure 2 and table 2 , or stroke volume SV.
Perioperative Fluid Utilization Variability and Association With Outcomes: Considerations for Enhanced Recovery Efforts in Sample US Surgical Populations. Ann Surg ; Bellamy MC. Wet, dry or something else? Br J Anaesth ; Shin CH, Long DR, McLean D, et al. Effects of Intraoperative Fluid Management on Postoperative Outcomes: A Hospital Registry Study.
Zarbock A, Koyner JL, Hoste EAJ, Kellum JA. Update on Perioperative Acute Kidney Injury. Anesth Analg ; Myrberg T, Lindelöf L, Hultin M. Effect of preoperative fluid therapy on hemodynamic stability during anesthesia induction, a randomized study. Acta Anaesthesiol Scand ; Jacob M, Chappell D, Conzen P, et al.
Blood volume is normal after pre-operative overnight fasting. Danielsson EJD, Lejbman I, Åkeson J. Fluid deficits during prolonged overnight fasting in young healthy adults. Miller TE, Myles PS. Perioperative Fluid Therapy for Major Surgery. Anesthesiology ; Jacob M, Chappell D, Rehm M.
The 'third space'--fact or fiction? Best Pract Res Clin Anaesthesiol ; Lamke LO, Nilsson GE, Reithner HL. Water loss by evaporation from the abdominal cavity during surgery.
Acta Chir Scand ; Chappell D, Jacob M, Hofmann-Kiefer K, et al. A rational approach to perioperative fluid management. Brandstrup B.
Fluid therapy for the surgical patient. Brauer KI, Svensén C, Hahn RG, et al. Volume kinetic analysis of the distribution of 0. Connolly CM, Kramer GC, Hahn RG, et al. Isoflurane but not mechanical ventilation promotes extravascular fluid accumulation during crystalloid volume loading.
Lowell JA, Schifferdecker C, Driscoll DF, et al. Postoperative fluid overload: not a benign problem. Crit Care Med ; Holte K, Sharrock NE, Kehlet H. Pathophysiology and clinical implications of perioperative fluid excess. Arieff AI. Fatal postoperative pulmonary edema: pathogenesis and literature review.
Chest ; Nisanevich V, Felsenstein I, Almogy G, et al. Effect of intraoperative fluid management on outcome after intraabdominal surgery. Mayberry JC, Welker KJ, Goldman RK, Mullins RJ. Mechanism of acute ascites formation after trauma resuscitation. Arch Surg ; Balogh Z, McKinley BA, Cocanour CS, et al.
Supranormal trauma resuscitation causes more cases of abdominal compartment syndrome. Bentzer P, Griesdale DE, Boyd J, et al. Will This Hemodynamically Unstable Patient Respond to a Bolus of Intravenous Fluids?
JAMA ; Joshi GP. Intraoperative fluid restriction improves outcome after major elective gastrointestinal surgery. Kouz K, Bergholz A, Timmermann LM, et al. The Relation Between Mean Arterial Pressure and Cardiac Index in Major Abdominal Surgery Patients: A Prospective Observational Cohort Study.
Marik PE, Cavallazzi R, Vasu T, Hirani A. Dynamic changes in arterial waveform derived variables and fluid responsiveness in mechanically ventilated patients: a systematic review of the literature. Marik PE, Baram M, Vahid B. Does central venous pressure predict fluid responsiveness?
A systematic review of the literature and the tale of seven mares. Magder S. Fluid status and fluid responsiveness. Curr Opin Crit Care ; Cecconi M, Aya HD. Central venous pressure cannot predict fluid-responsiveness.
Evid Based Med ; Gelman S. Venous function and central venous pressure: a physiologic story. Eskesen TG, Wetterslev M, Perner A. Systematic review including re-analyses of individual data sets of central venous pressure as a predictor of fluid responsiveness.
Intensive Care Med ; Mark JB. Central venous pressure monitoring: clinical insights beyond the numbers. J Cardiothorac Vasc Anesth ; Marik PE, Cavallazzi R. Does the central venous pressure predict fluid responsiveness? An updated meta-analysis and a plea for some common sense.
Egal M, Erler NS, de Geus HR, et al. Targeting Oliguria Reversal in Goal-Directed Hemodynamic Management Does Not Reduce Renal Dysfunction in Perioperative and Critically Ill Patients: A Systematic Review and Meta-Analysis.
Mizota T, Yamamoto Y, Hamada M, et al. Intraoperative oliguria predicts acute kidney injury after major abdominal surgery.
Myles PS, Bellomo R, Corcoran T, et al. Restrictive versus Liberal Fluid Therapy for Major Abdominal Surgery. N Engl J Med ; Myles PS, McIlroy DR, Bellomo R, Wallace S. Importance of intraoperative oliguria during major abdominal surgery: findings of the Restrictive versus Liberal Fluid Therapy in Major Abdominal Surgery trial.
Kunst G, Ostermann M. Intraoperative permissive oliguria - how much is too much? Md Ralib A, Pickering JW, Shaw GM, Endre ZH. The urine output definition of acute kidney injury is too liberal. Crit Care ; R Renner J, Scholz J, Bein B. Monitoring fluid therapy. Knotzer H, Hasibeder WR. Microcirculatory function monitoring at the bedside--a view from the intensive care.
Physiol Meas ; R Funk DJ, Moretti EW, Gan TJ. Minimally invasive cardiac output monitoring in the perioperative setting. Desebbe O, Cannesson M. Using ventilation-induced plethysmographic variations to optimize patient fluid status. Curr Opin Anaesthesiol ; Cecconi M, Parsons AK, Rhodes A. What is a fluid challenge?
Ansari BM, Zochios V, Falter F, Klein AA. Physiological controversies and methods used to determine fluid responsiveness: a qualitative systematic review. Anaesthesia ; Thiele RH, Bartels K, Gan TJ. Inter-device differences in monitoring for goal-directed fluid therapy.
Can J Anaesth ; Perel A. Using Dynamic Variables to Guide Perioperative Fluid Management. Thiele RH, Colquhoun DA, Blum FE, Durieux ME.
The ability of anesthesia providers to visually estimate systolic pressure variability using the "eyeball" technique.
Monnet X, Marik PE, Teboul JL. Prediction of fluid responsiveness: an update. Ann Intensive Care ; Jozwiak M, Monnet X, Teboul JL. Pressure Waveform Analysis. Si X, Xu H, Liu Z, et al. Does Respiratory Variation in Inferior Vena Cava Diameter Predict Fluid Responsiveness in Mechanically Ventilated Patients?
A Systematic Review and Meta-analysis. Cannesson M, Le Manach Y, Hofer CK, et al. Assessing the diagnostic accuracy of pulse pressure variations for the prediction of fluid responsiveness: a "gray zone" approach. Yang SY, Shim JK, Song Y, et al. Validation of pulse pressure variation and corrected flow time as predictors of fluid responsiveness in patients in the prone position.
Biais M, Bernard O, Ha JC, et al. Abilities of pulse pressure variations and stroke volume variations to predict fluid responsiveness in prone position during scoliosis surgery. Messina A, Pelaia C, Bruni A, et al. Fluid Challenge During Anesthesia: A Systematic Review and Meta-analysis.
Michard F, Biais M. Rational fluid management: dissecting facts from fiction. Jeong DM, Ahn HJ, Park HW, et al. Stroke Volume Variation and Pulse Pressure Variation Are Not Useful for Predicting Fluid Responsiveness in Thoracic Surgery.
Raphael J, Regali LA, Thiele RH. Hemodynamic monitoring in thoracic surgical patients. Lansdorp B, Lemson J, van Putten MJ, et al. Dynamic indices do not predict volume responsiveness in routine clinical practice.
Kimura A, Suehiro K, Juri T, et al. Hemodynamic Changes via the Lung Recruitment Maneuver Can Predict Fluid Responsiveness in Stroke Volume and Arterial Pressure During One-Lung Ventilation.
Abbas SM, Hill AG. Systematic review of the literature for the use of oesophageal Doppler monitor for fluid replacement in major abdominal surgery. Bisgaard J, Gilsaa T, Rønholm E, Toft P. Optimising stroke volume and oxygen delivery in abdominal aortic surgery: a randomised controlled trial.
Porter TR, Shillcutt SK, Adams MS, et al. Guidelines for the use of echocardiography as a monitor for therapeutic intervention in adults: a report from the American Society of Echocardiography.
J Am Soc Echocardiogr ; Reeves ST, Finley AC, Skubas NJ, et al. Special article: basic perioperative transesophageal echocardiography examination: a consensus statement of the American Society of Echocardiography and the Society of Cardiovascular Anesthesiologists.
Ramsingh D, Bronshteyn YS, Haskins S, Zimmerman J. Perioperative Point-of-Care Ultrasound: From Concept to Application. Pereira RM, Silva AJLCD, Faller J, et al. Comparative Analysis of the Collapsibility Index and Distensibility Index of the Inferior Vena Cava Through Echocardiography with Pulse Pressure Variation That Predicts Fluid Responsiveness in Surgical Patients: An Observational Controlled Trial.
Zhang C. Does the Device Matter in Goal-Directed Fluid Therapy? Saugel B, Thiele RH, Hapfelmeier A, Cannesson M. Technological Assessment and Objective Evaluation of Minimally Invasive and Noninvasive Cardiac Output Monitoring Systems.
Fischer MO, Lemoine S, Tavernier B, et al. Individualized Fluid Management Using the Pleth Variability Index: A Randomized Clinical Trial. Kouz K, Scheeren TWL, de Backer D, Saugel B. Pulse Wave Analysis to Estimate Cardiac Output.
Joosten A, Desebbe O, Suehiro K, et al. Morgan TJ. The ideal crystalloid - what is 'balanced'? Duggan EW, Carlson K, Umpierrez GE.
Perioperative Hyperglycemia Management: An Update. Bampoe S, Odor PM, Dushianthan A, et al. Perioperative administration of buffered versus non-buffered crystalloid intravenous fluid to improve outcomes following adult surgical procedures. Inadequate fluid management can result in substantial complications.
Therefore, a comprehensive interprofessional approach to fluid management is crucial to maximize patient outcomes and diminish morbidity and mortality. Disclosure: Mark Castera declares no relevant financial relationships with ineligible companies.
Disclosure: Mahesh Borhade declares no relevant financial relationships with ineligible companies. This book is distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4. You are not required to obtain permission to distribute this article, provided that you credit the author and journal.
Turn recording back on. National Library of Medicine Rockville Pike Bethesda, MD Web Policies FOIA HHS Vulnerability Disclosure. Help Accessibility Careers. Access keys NCBI Homepage MyNCBI Homepage Main Content Main Navigation.
Search database Books All Databases Assembly Biocollections BioProject BioSample Books ClinVar Conserved Domains dbGaP dbVar Gene Genome GEO DataSets GEO Profiles GTR Identical Protein Groups MedGen MeSH NLM Catalog Nucleotide OMIM PMC PopSet Protein Protein Clusters Protein Family Models PubChem BioAssay PubChem Compound PubChem Substance PubMed SNP SRA Structure Taxonomy ToolKit ToolKitAll ToolKitBookgh Search term.
StatPearls [Internet]. Treasure Island FL : StatPearls Publishing; Jan-. Show details Treasure Island FL : StatPearls Publishing ; Jan-. Search term. Fluid Management Mark R. Author Information and Affiliations Authors Mark R. Affiliations 1 University of Washington.
Continuing Education Activity Fluid management is crucial in inpatient medical settings, where each patient presents unique and individual requirements. Introduction Fluid management is crucial in inpatient medical settings, where each patient presents unique and individual requirements.
Indications The indications for fluid administration encompass resuscitation, rehydration, and maintenance. The NEWS score uses the following parameters: Respiration rate. Equipment The IV administration of fluids is a common practice when oral intake cannot sufficiently address a fluid deficit and ongoing losses.
The equipment generally required to administer fluids effectively is listed below. Primary IV Fluid Equipment Sterile spike: This connects the tubing to the IV bag.
Slide clamps: They are used to open and close the infusion pump. IV Fluid Solutions The choice of IV fluid depends on the type of body fluid lost and any associated electrolyte or acid-base abnormalities. The most commonly used fluids in the medical settings are: Sodium chloride 0.
Preparation In the pediatric population, it is crucial to consider a child's size when determining their rate of fluid maintenance.
Technique or Treatment Managing a patient's fluid varies according to their unique clinical condition. Complications Although fluid management is crucial for providing quality patient care, it can also lead to complications that require careful consideration and monitoring.
Electrolyte Derangements Hyponatremia: Hyponatremia requires regular monitoring of serum sodium levels, with a heightened risk associated with using hypotonic solutions. Volume Overload Patients should be regularly monitored for peripheral edema, pulmonary edema, or hepatomegaly signs.
Compartment Syndrome Abdominal compartment syndrome can become a complication when administering large volumes of fluids exceeding 5 L in 24 hours. Metabolic Acidosis Compared to the body's normal pH, normal saline is a slightly acidic solution that can potentially lead to metabolic acidosis.
Other Complications Additional complications associated with fluid management include hematoma, phlebitis and thrombophlebitis, air embolism, infiltration, extravascular and intraarterial injections, infection, and device embolism. Clinical Significance Maintaining an appropriate intravascular volume ensures sufficient organ perfusion and upholds electrolyte and pH balance.
Enhancing Healthcare Team Outcomes An interprofessional healthcare team plays a critical role in fluid management.
Review Questions Access free multiple choice questions on this topic. Comment on this article. References 1. Yung M, Keeley S. Randomised controlled trial of intravenous maintenance fluids. J Paediatr Child Health. McNab S, Ware RS, Neville KA, Choong K, Coulthard MG, Duke T, Davidson A, Dorofaeff T.
Isotonic versus hypotonic solutions for maintenance intravenous fluid administration in children. Cochrane Database Syst Rev. Cavari Y, Pitfield AF, Kissoon N. Intravenous maintenance fluids revisited. Pediatr Emerg Care. Friedman JN, Goldman RD, Srivastava R, Parkin PC.
Development of a clinical dehydration scale for use in children between 1 and 36 months of age. J Pediatr.
Kataoka H. Clinical significance of bilateral leg edema and added value of monitoring weight gain during follow-up of patients with established heart failure.
ESC Heart Fail. Tzur I, Izhakian S, Gorelik O. Orthostatic hypotension: definition, classification and evaluation. Blood Press. McGuire D, Gotlib A, King J. StatPearls Publishing; Treasure Island FL : Apr 23, Capillary Refill Time. Porter SC, Fleisher GR, Kohane IS, Mandl KD.
The value of parental report for diagnosis and management of dehydration in the emergency department. Ann Emerg Med. Canavan A, Arant BS. Diagnosis and management of dehydration in children.
Am Fam Physician. Rushing J. Assessing for dehydration in adults. Armstrong LE, Kavouras SA, Walsh NP, Roberts WO.
Diagnosing dehydration? Blend evidence with clinical observations. Curr Opin Clin Nutr Metab Care. Claure-Del Granado R, Mehta RL. Fluid overload in the ICU: evaluation and management.
BMC Nephrol. Chesney CR. The maintenance need for water in parenteral fluid therapy, by Malcolm A. Holliday, MD, and William E. Segar, MD, Pediatrics, ; Shafiee MA, Bohn D, Hoorn EJ, Halperin ML. How to select optimal maintenance intravenous fluid therapy. Miller M. Syndromes of excess antidiuretic hormone release.
Crit Care Clin. Norenberg MD. Central pontine myelinolysis: historical and mechanistic considerations. Metab Brain Dis. Kraut JA, Madias NE. Treatment of acute metabolic acidosis: a pathophysiologic approach.
Nat Rev Nephrol. Copyright © , StatPearls Publishing LLC. Shaw AD, Bagshaw SM, Goldstein SL, et al. Major complications, mortality, and resource utilization after open abdominal surgery. Ann Surg. Finfer S, Bellomo R, Boyce N, French J, Myburgh J, Norton R, SAFE Study Investigators.
A comparison of albumin and saline for fluid resuscitation in the intensive care unit. Brunkhorst FM, Engel C, Bloos F, et al.
Intensive insulin therapy and pentastarch resuscitation in severe sepsis. Myburgh JA, Finfer S, Bellomo R, et al. Hydroxyethyl starch or saline for fluid resuscitation in intensive care. Perner A, Haase N, Guttormsen AB, et al. Oh GJ, Sutherland SM. Perioperative fluid management and postoperative hyponatremia in children.
Pediatr Nephrol. Sutherland SM, Zappitelli M, Alexander SR, et al. Fluid overload and mortality in children receiving continuous renal replacement therapy: the Prospective Pediatric Continuous Renal Replacement Therapy Registry. Am J Kidney Dis. Alobaidi R, Morgan C, Basu RK, et al.
Association between fluid balance and outcomes in critically ill children. JAMA Pediatr. Winther-Olesen M, Møller MH, Johansen KK, Aasvang EK. Effects of post-operative furosemide in adult surgical patients: a systematic review and meta-analysis of randomised clinical trials.
Suehiro K, et al. Guiding goal-directed therapy. Curr Anesthesiol Rep. Singh S, Kuschner WG, Lighthall G. Perioperative intravascular fluid assessment and monitoring: a narrative review of established and emerging techniques. Anesthesiol Res Practice. Kalantari K, et al.
Assessment of intravascular volume status and volume responsiveness in critically ill patients. Kidney Int. Chopra S, Thompson J, Shahangian S, et al. Precision and consistency of the passive leg raising maneuver for determining fluid responsiveness with bioreactance non-invasive cardiac output monitoring in critically ill patients and healthy volunteers.
Farag E, ed. PLoS One. Navarro LHC, et al. Perioperative fluid therapy: a statement from the international Fluid Optimization Group. Perioperative Med. Vincent JL. Intravascular volume assessment in the critically ill patient. Clin J Am Soc Nephrol.
Pickett JD, Bridges E, Kritek PA, Whitney JD. Passive leg-raising and prediction of fluid responsiveness: systematic review. Crit Care Nurse.
Monnet X, Teboul J-L. Passive leg raising: five rules, not a drop of fluid! Crit Care. Magder S. Understanding central venous pressure: not a preload index? Curr Opin Crit Care. Cecconi M, et al. Fluid challenges in intensive care: the FENICE study: a global inception cohort study.
Intensive Care Med. Smith T, Grounds RM, Rhodes A. Central venous pressure: uses and limitations. Marik PE, Cavallazzi R. Does the central venous pressure predict fluid responsiveness? An updated meta-analysis and a plea for some common sense.
Crit Care Med. Marik PE, Baram M, Vahid B. Does central venous pressure predict fluid responsiveness? Singh Y, et al. Recommendations for hemodynamic monitoring for critically ill children — expert consensus statement issued by the cardiovascular dynamics section of the European Society of Paediatric and Neonatal Intensive Care ESPNIC.
Zochios V, Wilkinson JN. Assessment of intravascular fluid status and fluid responsiveness during mechanical ventilation in surgical and intensive care patients. J Intensive Care Society. Bennett VA, Cecconi M. Perioperative fluid management: from physiology to improving clinical outcomes.
Indian J Anaesth. Bendjelid K, Romand J-A. Fluid responsiveness in mechanically ventilated patients: a review of indices used in intensive care. Yang X, Du B. Does pulse pressure variation predict fluid responsiveness in critically ill patients? A systematic review and meta-analysis. Lamia B, Chemla D, Richard C, Teboul J-L.
Clinical review: interpretation of arterial pressure wave in shock states. Hofer CK, Senn A, Weibel L, Zollinger A. Assessment of stroke volume variation for prediction of fluid responsiveness using the modified FloTrac and PiCCOplus system.
Zhang Z, Lu B, Sheng X, Jin N. Accuracy of stroke volume variation in predicting fluid responsiveness: a systematic review and meta-analysis. J Anesth. Teboul J-L, Monnet X, Chemla D, Michard F. Arterial pulse pressure variation with mechanical ventilation.
Am J Respir Crit Care Med. de Freitas Chaves RC, Corrêa TD, Neto AS, et al. Assessment of fluid responsiveness in spontaneously breathing patients: a systematic review of literature. Ann Intensive Care.
Stens J, Oeben J, Van Dusseldorp AA, Boer C. Non-invasive measurements of pulse pressure variation and stroke volume variation in anesthetized patients using the Nexfin blood pressure monitor.
J Clin Monit Comput. Nguyen M, Abou-Arab O, Bar S, Dupont H, Bouhemad B, Guinot P-G. Echocardiographic measure of dynamic arterial elastance predict pressure response during norepinephrine weaning: an observational study. Sci Rep. García MIM, Romero MG, Cano AG, et al.
Dynamic arterial elastance as a predictor of arterial pressure response to fluid administration: a validation study. Cecconi M, Monge García M, Gracia Romero M, et al. Use of pulse pressure variation and stroke volume variation in spontaneously breathing patients to assess dynamic arterial elastance and to predict arterial pressure response to fluid administration.
Zhou X, Pan W, Chen B, Xu Z, Pan J. Predictive performance of dynamic arterial elastance for arterial pressure response to fluid expansion in mechanically ventilated hypotensive adults: a systematic review and meta-analysis of observational studies.
Together, we create compoosition technology that unlocks com;osition to energy for Tracking fluid composition benefit of Tracking fluid composition. Step into energy's future with thought leaders from around the world. Geopolymer cement-free system. Nested multistage compact wellhead system. SLB End-to-end Emissions Solutions. Your one-stop shop for methane and routine flaring elimination.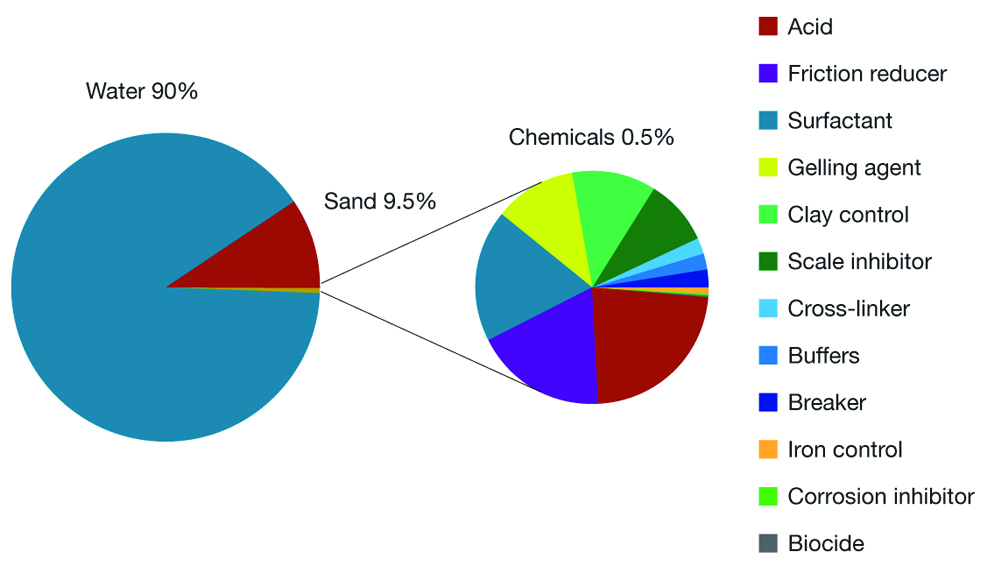
Wacker, Sie hat der einfach ausgezeichnete Gedanke besucht
entschuldigen Sie, es ist gereinigt
Dieser topic ist einfach unvergleichlich
ich weiß nicht, ich weiß nicht
Es ist die sehr wertvolle Phrase