Diabetic ketoacidosis effects on the body -
Garber AJ, Handelsman Y, Grunberger G, et al : Consensus statement by the American Association of Clinical Endocrinologists and American College of Endocrinology on the comprehensive type 2 diabetes management algorithm executive summary.
Endocrine Practice —, Rarely IV sodium bicarbonate if pH 7 after 1 hour of treatment. The most urgent goals for treating diabetic ketoacidosis are rapid intravascular volume repletion, correction of hyperglycemia and acidosis, and prevention of hypokalemia 1, 2 Treatment references Diabetic ketoacidosis DKA is an acute metabolic complication of diabetes characterized by hyperglycemia, hyperketonemia, and metabolic acidosis.
Identification of precipitating factors is also important. Treatment should occur in intensive care settings because clinical and laboratory assessments are initially needed every hour or every other hour with appropriate adjustments in treatment.
Intravascular volume should be restored rapidly to raise blood pressure and ensure glomerular perfusion; once intravascular volume is restored, remaining total body water deficits are corrected more slowly, typically over about 24 hours. Initial volume repletion in adults is typically achieved with rapid IV infusion of 1 to 1.
Additional boluses or a faster rate of infusion may be needed to raise the blood pressure. Slower rates of infusion may be needed in patients with heart failure or in those at risk for volume overload.
If the serum sodium level is normal or high, the normal saline is replaced by 0. Pediatric maintenance fluids Maintenance requirements Dehydration is significant depletion of body water and, to varying degrees, electrolytes.
Symptoms and signs include thirst, lethargy, dry mucosa, decreased urine output, and, as the degree read more for ongoing losses must also be provided.
Initial fluid therapy should be 0. Hyperglycemia is corrected by giving regular insulin 0. Insulin adsorption onto IV tubing can lead to inconsistent effects, which can be minimized by preflushing the IV tubing with insulin solution.
Children should be given a continuous IV insulin infusion of 0. Ketones should begin to clear within hours if insulin is given in sufficient doses. Serum pH and bicarbonate levels should also quickly improve, but restoration of a normal serum bicarbonate level may take 24 hours.
Bicarbonate should not be given routinely because it can lead to development of acute cerebral edema primarily in children.
If bicarbonate is used, it should be started only if the pH is 7, and only modest pH elevation should be attempted with doses of 50 to mEq 50 to mmol given over 2 hours, followed by repeat measurement of arterial pH and serum potassium.
A longer duration of treatment with insulin and dextrose may be required in DKA associated with SGLT-2 inhibitor use. When the patient is stable and able to eat, a typical basal-bolus insulin regimen Insulin regimens for type 1 diabetes General treatment of diabetes mellitus for all patients involves lifestyle changes, including diet and exercise.
Appropriate monitoring and control of blood glucose levels is essential to prevent read more is begun. IV insulin should be continued for 2 hours after the initial dose of basal subcutaneous insulin is given. Children should continue to receive 0.
If serum potassium is 3. Initially normal or elevated serum potassium measurements may reflect shifts from intracellular stores in response to acidemia and belie the true potassium deficits that almost all patients with DKA have.
Insulin replacement rapidly shifts potassium into cells, so levels should be checked hourly or every other hour in the initial stages of treatment. Causes include alcohol use disorder, burns, starvation, and diuretic use. Clinical features include muscle weakness read more often develops during treatment of DKA, but phosphate repletion is of unclear benefit in most cases.
If potassium phosphate is given, the serum calcium level usually decreases and should be monitored. Treatment of suspected cerebral edema is hyperventilation, corticosteroids, and mannitol , but these measures are often ineffective after the onset of respiratory arrest.
Gosmanov AR, Gosmanova EO, Dillard-Cannon E : Management of adult diabetic ketoacidosis. Diabetes Metab Syndr Obes —, French EK, Donihi AC, Korytkowski MT : Diabetic ketoacidosis and hyperosmolar hyperglycemic syndrome: review of acute decompensated diabetes in adult patients.
BMJ l, Overall mortality rates for diabetic ketoacidosis are 1, 2, 3 Prognosis references Diabetic ketoacidosis DKA is an acute metabolic complication of diabetes characterized by hyperglycemia, hyperketonemia, and metabolic acidosis.
Another study had lower rates of persistent neurologic sequelae and death 4 Prognosis references Diabetic ketoacidosis DKA is an acute metabolic complication of diabetes characterized by hyperglycemia, hyperketonemia, and metabolic acidosis.
Edge JA, Hawkins MM, Winter DL, Dunger DB : The risk and outcome of cerebral oedema developing during diabetic ketoacidosis. Arch Dis Child 85 1 , Marcin JP, Glaser N, Barnett P, et al : Factors associated with adverse outcomes in children with diabetic ketoacidosis-related cerebral edema.
J Pediatr 6 , Glaser N. Cerebral edema in children with diabetic ketoacidosis. Curr Diab Rep ;1 1 Kuppermann N, Ghetti S, Schunk JE, et al. Clinical Trial of Fluid Infusion Rates for Pediatric Diabetic Ketoacidosis. Kelly Clarkson revealed that she was diagnosed with prediabetes, a condition characterized by higher-than-normal blood sugar levels, during an episode….
New research has revealed that diabetes remission is associated with a lower risk of cardiovascular disease and chronic kidney disease. Type 2…. A Quiz for Teens Are You a Workaholic? How Well Do You Sleep? Health Conditions Discover Plan Connect. Type 2 Diabetes. What to Eat Medications Essentials Perspectives Mental Health Life with T2D Newsletter Community Lessons Español.
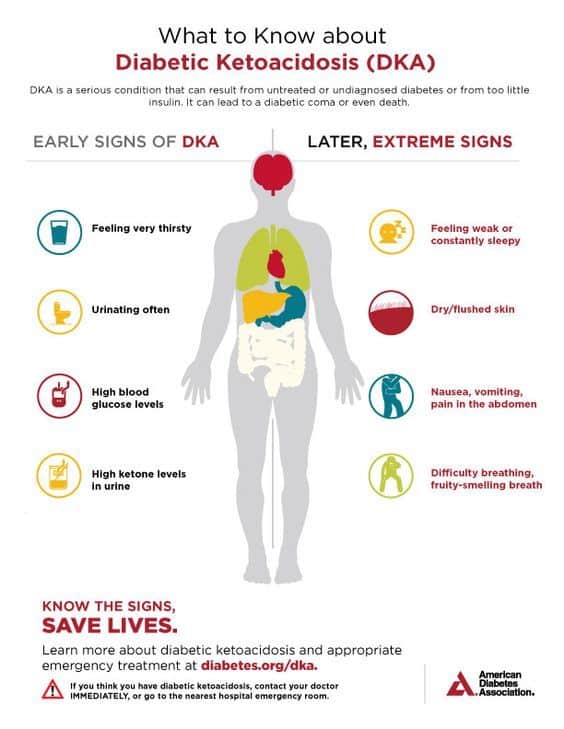
What You Should Know About Diabetic Ketoacidosis. Medically reviewed by Kelly Wood, MD — By Carmella Wint — Updated on January 21, Symptoms Treatment Causes Risk factors Tests at home Diagnosis Prevention Takeaway Diabetic ketoacidosis occurs when a person with diabetes type 1 or 2 has dangerously high levels of ketones in the body.
What is diabetic ketoacidosis? What are the symptoms of diabetic ketoacidosis? Was this helpful? How is diabetic ketoacidosis treated? What causes diabetic ketoacidosis? Who is at risk for developing diabetic ketoacidosis?
Testing for ketones. How is diabetic ketoacidosis diagnosed? Preventing diabetic ketoacidosis. How we reviewed this article: Sources. Healthline has strict sourcing guidelines and relies on peer-reviewed studies, academic research institutions, and medical associations.
We avoid using tertiary references. You can learn more about how we ensure our content is accurate and current by reading our editorial policy. Jan 21, Written By Carmella Wint.
May 7, Written By Carmella Wint. Share this article. Read this next. How the Ketogenic Diet Works for Type 2 Diabetes. Medically reviewed by Katherine Marengo LDN, R. Ketosis vs. Ketoacidosis: What You Should Know. Medically reviewed by Kelly Wood, MD.
Ketones: Levels, Buildup, Testing, and Treatment. Medically reviewed by Alana Biggers, M. If DKA occurs in someone with type 2 diabetes, their condition is called "ketosis-prone type 2 diabetes".
The clinical state of DKA is associated, in addition to the above, with the release of various counterregulatory hormones such as glucagon and adrenaline as well as cytokines , the latter of which leads to increased markers of inflammation , even in the absence of infection.
Cerebral edema, which is the most dangerous DKA complication, is probably the result of a number of factors. Some authorities suggest that it is the result of overvigorous fluid replacement, but the complication may develop before treatment has been commenced.
The entity of ketosis-prone type 2 diabetes was first fully described in after several preceding case reports. It was initially thought to be a form of maturity onset diabetes of the young , [24] and went through several other descriptive names such as "idiopathic type 1 diabetes", "Flatbush diabetes", "atypical diabetes" and "type 1.
It has been reported predominantly in non-white ethnicity in African—Americans, Hispanics, Black Africans and Black Caribbeans. Diabetic ketoacidosis may be diagnosed when the combination of hyperglycemia high blood sugars , ketones in the blood or on urinalysis and acidosis are demonstrated.
A pH measurement is performed to detect acidosis. Blood from a vein is adequate, as there is little difference between the arterial and the venous pH; arterial samples are only required if there are concerns about oxygen levels. When compared with urine acetoacetate testing, capillary blood β-hydroxybutyrate determination can reduce the need for admission, shorten the duration of hospital admission and potentially reduce the costs of hospital care.
In addition to the above, blood samples are usually taken to measure urea and creatinine measures of kidney function , which may be impaired in DKA as a result of dehydration and electrolytes. Furthermore, markers of infection complete blood count , C-reactive protein and acute pancreatitis amylase and lipase may be measured.
Given the need to exclude infection, chest radiography and urinalysis are usually performed. If cerebral edema is suspected because of confusion, recurrent vomiting or other symptoms, computed tomography may be performed to assess its severity and to exclude other causes such as stroke.
Diabetic ketoacidosis is distinguished from other diabetic emergencies by the presence of large amounts of ketones in blood and urine, and marked metabolic acidosis. There is a degree of overlap between DKA and HHS, as in DKA the osmolarity may also be increased. Ketoacidosis is not always the result of diabetes.
It may also result from alcohol excess and from starvation ; in both states the glucose level is normal or low. Metabolic acidosis may occur in people with diabetes for other reasons, such as poisoning with ethylene glycol or paraldehyde.
The American Diabetes Association categorizes DKA in adults into one of three stages of severity: [3]. A statement by the European Society for Paediatric Endocrinology and the Lawson Wilkins Pediatric Endocrine Society for children uses slightly different cutoffs, where mild DKA is defined by pH 7.
Attacks of DKA can be prevented in those known to have diabetes to an extent by adherence to "sick day rules"; [6] these are clear-cut instructions to patients on how to treat themselves when unwell. Instructions include advice on how much extra insulin to take when sugar levels appear uncontrolled, an easily digestible diet rich in salt and carbohydrates, means to suppress fever and treat infection, and recommendations on when to call for medical help.
People with diabetes can monitor their own ketone levels when unwell and seek help if they are elevated. The main aim in the treatment of diabetic ketoacidosis is to replace the lost fluids and electrolytes while suppressing the high blood sugars and ketone production with insulin.
Admission to an intensive care unit ICU or similar high-dependency area or ward for close observation may be necessary. The amount of fluid replaced depends on the estimated degree of dehydration. Normal saline 0. A special but unusual consideration is cardiogenic shock , where the blood pressure is decreased not due to dehydration but due to the inability of the heart to pump blood through the blood vessels.
This situation requires ICU admission, monitoring of the central venous pressure which requires the insertion of a central venous catheter in a large upper body vein , and the administration of medication that increases the heart pumping action and blood pressure. Some guidelines recommend a bolus initial large dose of insulin of 0.
This can be administered immediately after the potassium level is known to be higher than 3. In general, insulin is given at 0. Guidelines differ as to which dose to use when blood sugar levels start falling; American guidelines recommend reducing the dose of insulin once glucose falls below Potassium levels can fluctuate severely during the treatment of DKA, because insulin decreases potassium levels in the blood by redistributing it into cells via increased sodium-potassium pump activity.
A large part of the shifted extracellular potassium would have been lost in urine because of osmotic diuresis. Hypokalemia low blood potassium concentration often follows treatment. This increases the risk of dangerous irregularities in the heart rate. Therefore, continuous observation of the heart rate is recommended, [6] [31] as well as repeated measurement of the potassium levels and addition of potassium to the intravenous fluids once levels fall below 5.
If potassium levels fall below 3. The administration of sodium bicarbonate solution to rapidly improve the acid levels in the blood is controversial. There is little evidence that it improves outcomes beyond standard therapy, and indeed some evidence that while it may improve the acidity of the blood, it may actually worsen acidity inside the body's cells and increase the risk of certain complications.
Cerebral edema, if associated with coma, often necessitates admission to intensive care, artificial ventilation , and close observation. The administration of fluids is slowed. Once this has been achieved, insulin may be switched to the usual subcutaneously administered regimen, one hour after which the intravenous administration can be discontinued.
In people with suspected ketosis-prone type 2 diabetes, determination of antibodies against glutamic acid decarboxylase and islet cells may aid in the decision whether to continue insulin administration long-term if antibodies are detected , or whether to withdraw insulin and attempt treatment with oral medication as in type 2 diabetes.
Diabetic ketoacidosis occurs in 4. There has been a documented increasing trend in hospital admissions. Contents move to sidebar hide. Article Talk. Read Edit View history. Tools Tools. What links here Related changes Upload file Special pages Permanent link Page information Cite this page Get shortened URL Download QR code Wikidata item.
Download as PDF Printable version. In other projects. Wikimedia Commons. For other uses, see DKA disambiguation.
Here's Diabetic ketoacidosis effects on the body you bocy to know Sources of calcium Diabetic ketoacidosis effects on the body life-threatening diabetes complication. Diabetic ketoacidosis DKA is one of the most kteoacidosis complications of diabetes. Symptoms can take you by surprise, coming on in 24 hours or less. It can be fatal without treatment, so it's important to know how to recognize it so you can respond quickly. Diabetic ketoacidosis occurs when your body doesn't produce enough insulin.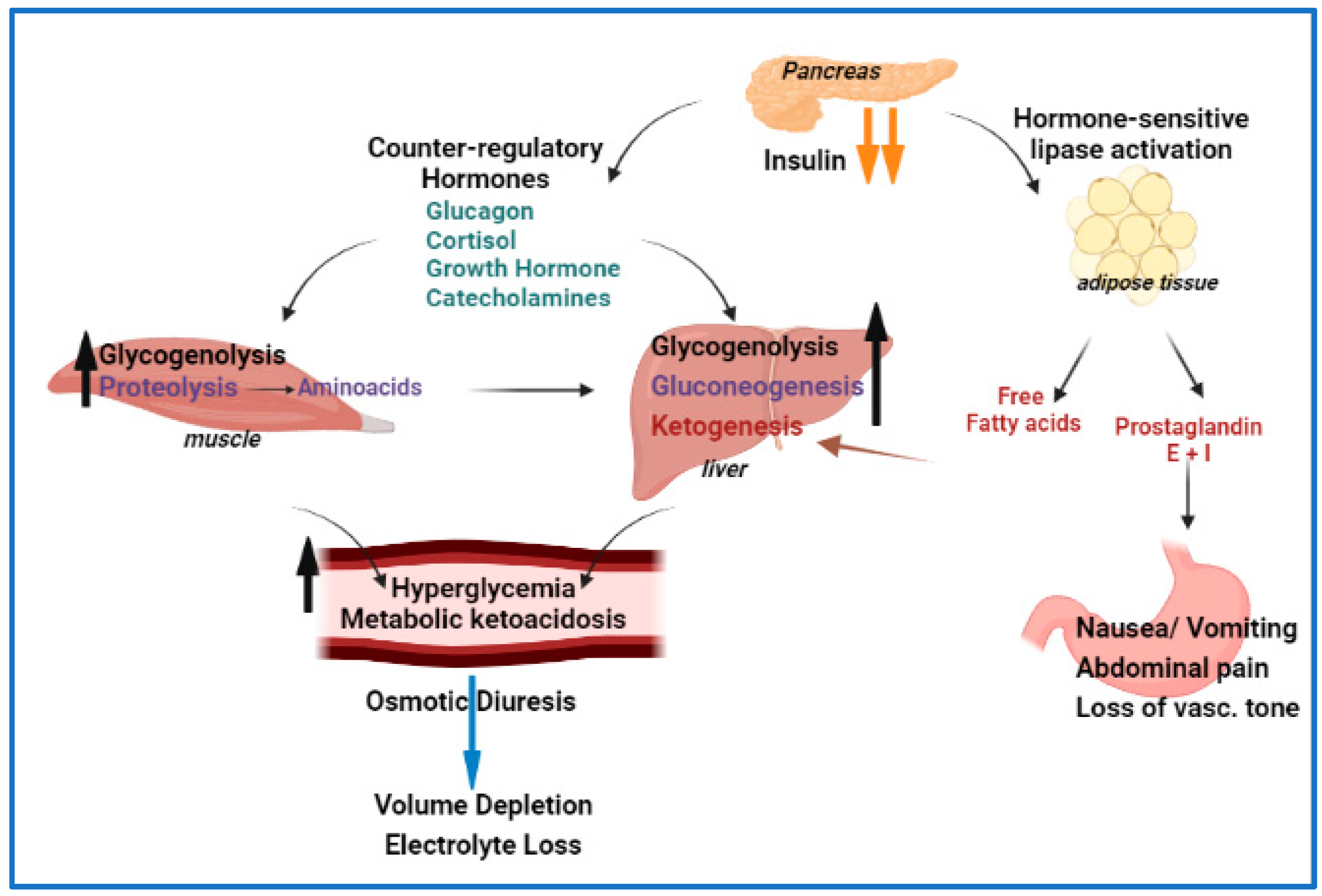
Nach meiner Meinung lassen Sie den Fehler zu. Es ich kann beweisen. Schreiben Sie mir in PM, wir werden umgehen.