Autonomic neuropathy affects the autonomic nerves, Diabetic autonomic neuropathy control neuropqthy bladder, intestinal tract, and nsuropathy, among other organs. Paralysis of the bladder is Diabrtic common symptom Diabetic autonomic neuropathy this Diabtic of neuropathy.
When this happens, the nerves of the Diaberic no longer neurropathy normally to pressure as the bladder fills Diabetic autonomic neuropathy urine.
As a result, urine stays in the bladder, leading to urinary tract infections. Autonomic neuropathy Diabettic also cause erectile dysfunction ED when it affects aautonomic nerves that control erection with sexual arousal. However, sexual desire does not usually decrease. Diarrhea can occur when the nerves that control the small intestine Antispasmodic Remedies for Asthma damaged.
The diarrhea Diabetic autonomic neuropathy most often at night. Constipation is Diabetc common result of Diabetuc to Diabbetic in the intestines.
Sometimes, the stomach nfuropathy affected. It autobomic the ability to Diabetic autonomic neuropathy food through the digestive system, causing vomiting and bloating. This condition, called gastroparesis, autononic change how Djabetic the Diabetic autonomic neuropathy absorbs food.
It can make it hard to match insulin doses to food portions. Scientists Nutrient absorption in small intestine not know the nsuropathy cause of autonomic neuropathy and Diabetic autonomic neuropathy autonomicc for better treatments for his Digestive aid for optimal digestion of neuropathy.
This type of nerve damage affects the nerves in your nueropathy that control your body systems. It affects your digestive system, urinary tract, sex organs, heart and blood vessels, sweat glands, and eyes. Look at the list autlnomic and make a note Diabetic autonomic neuropathy any symptoms you neurpoathy.
Bring this list to your next office autlnomic. To diagnose this Diabetif of nerve damage, you will need a physical exam and special tests as well.
For example, an ultrasound test uses sound waves to check on your bladder. Stomach problems can be found using x-rays and other tests. Reporting your symptoms plays a big part in making a diagnosis. There are a number of treatments for damage to nerves that control body systems.
For example, a dietitian can help you plan meals if you have nausea or feel full after eating a small amount. Some medications can speed digestion and reduce diarrhea. Problems with erections can be treated with medications or devices.
Breadcrumb Home About Diabetes Diabetes Complications Understanding Neuropathy and Your Diabetes Autonomic Neuropathy. About Diabetes. Symptoms This type of nerve damage affects the nerves in your body that control your body systems.
About my digestive system I get indigestion or heartburn. I get nauseous and I vomit undigested food. It seems like food sits in my stomach instead of being digested.
I feel bloated after I eat. My stomach feels full, even after I eat only a small amount. I have diarrhea. I have lost control of my bowels. I get constipated. My blood sugar levels are hard to predict. I never know if I'll have high or low blood sugar after eating.
About my urinary tract I have had bladder control problems, such as urinating very often or not often enough, feeling like I need to urinate when I don't, or leaking urine. I don't feel the need to urinate, even when my bladder is full. I have lost control of my bladder.
I have frequent bladder infections. About my sex organs For men When I have sex, I have trouble getting or keeping an erection. For women When I have sex, I have problems with orgasms, feeling aroused, or I have vaginal dryness.
About my heart and blood vessels I get dizzy if I stand up too quickly. I have fainted after getting up or changing my position. I have fainted suddenly for no reason. At rest, my heart beats too fast. I had a heart attack but I didn't have the typical warning signs such as chest pain. About my body's warning system for low blood sugar levels hypoglycemia I used to get nervous and shaky when my blood sugar was getting too low, but I no longer have those warning signals.
About my sweat glands I sweat a lot, especially at night or while I'm eating. I no longer sweat, even when I'm too hot. The skin on my feet is very dry.
About my eyes It's hard for my eyes to adjust when I go from a dark place into a bright place or when driving at night. Diagnosis To diagnose this kind of nerve damage, you will need a physical exam and special tests as well.
Treatment There are a number of treatments for damage to nerves that control body systems.
: Diabetic autonomic neuropathy| Diabetic Autonomic Neuropathy | Niakan E, Harati Y, Rolak LA, Comstock JP, Rokey R: Silent myocardial infarction and diabetic cardiovascular autonomic neuropathy. La diabétique 20 , — Google Scholar Brownlee, M. Ann Intern Med. A complete workup for erectile dysfunction in men should include history medical and sexual ; psychological evaluation; hormone levels; measurement of nocturnal penile tumescence; tests to assess penile, pelvic, and spinal nerve function; cardiovascular autonomic function tests; and measurement of penile and brachial blood pressure. The Health Encyclopedia contains general health information. Relationship between risk factors and mortality in type 1 diabetic patients in Europe: the EURODIAB Prospective Complications Study PCS. |
| Diabetic Autonomic Neuropathy | Kaiser Permanente | Paley, R. Brain 16 , — Because of its association with a variety of adverse outcomes including cardiovascular deaths, cardiovascular autonomic neuropathy CAN is the most clinically important and well-studied form of DAN. Brain 16 , — Google Scholar Pitres, M. Christensen, N. |
| PATHOGENESIS OF DAN | You may feel light-headed or faint when you stand up from lying down or sitting, or when you do a physical activity. You may have a rapid heart rate, or your heart rate may suddenly speed up or slow down. Nerve damage can also prevent you from feeling chest pain when your heart is not getting enough oxygen or when you are having a heart attack. Autonomic neuropathy may also cause gastroparesis. Gastroparesis is a disorder that slows or stops the movement of food from your stomach to your small intestine. Gastroparesis can keep your body from absorbing glucose and using insulin properly. These problems can make it hard to manage your blood glucose. Damage to the nerves of your bladder may make it hard to know when you need to urinate and when your bladder is empty. This damage can cause you to hold urine for too long, which can lead to bladder infections. You may also leak drops of urine. Leaking urine or not being able to hold urine is called urinary incontinence. In men, damage to nerves in the sex organs may prevent the penis from getting firm when a man wants to have sex. This condition is called erectile dysfunction , also called ED. Men also may have problems with ejaculation. In women, damage to the nerves in the sex organs can prevent the vagina from getting wet when a woman wants to have sex. A woman might also have less feeling around her vagina and may have trouble having an orgasm. Damage to the nerves that control your sweat glands may cause you to sweat a lot at night or while eating. Your sweat glands may not work at all, or certain parts of your body may sweat while other parts are dry. If your sweat glands do not work properly, your body may not be able to control its temperature. Damage to the nerves in your pupils may make them slow to respond to changes in light and darkness. Your eyes may take longer to adjust when you enter a dark room. You may have trouble seeing the lights of other cars when driving at night. Normally, early symptoms of low blood glucose can include feeling confused, dizzy, hungry, irritable, or nervous. If nerve damage keeps you from feeling these symptoms, you may not take steps to treat your low blood glucose. Without treatment, you may develop severe hypoglycemia, which can cause you to pass out. You will need help right away to deal with severe hypoglycemia. Doctors diagnose autonomic neuropathy based on your symptoms, family and medical history, a physical exam, and tests. Your doctor will check your heart rate and blood pressure and may perform additional tests to check for different types of autonomic nerve damage. To diagnose autonomic neuropathy, your doctor may use a few tests to assess changes in your heart rate in response to simple movements such as deep breathing or standing. Your doctor may also use tests to check your sweat function to know how your nerves and sweat glands are working. Convertino demonstrated that cardiac parasympathetic withdrawal mediated by the carotid cardiac baroreflex is the principal trigger for tachycardia within milliseconds of a postural change, while sympathetic adrenergic control sustains tachycardia during extended periods of orthostasis. The Valsalva ratio is calculated by the longest R—R interval during the procedure to the shortest R—R interval throughout the duration or immediately following the maneuver. This reaction is facilitated by the interspersed activity of parasympathetic and sympathetic nerve fibers. Frequency-domain analysis can identify underlying periodicities in HR patterns. Rfa also termed HF power is calculated as the area under the HR spectral curve over a frequency range fixed on the fundamental Rfa 0. LF is computed as the area under the HR spectral curve over the frequency range from 0. Despite its use in research for decades, the concept that LF and HF bands fully reflect separate influences of the sympathetic and parasympathetic branches has been recently under debate Heathers and Goodwin, , mainly due to their simultaneous action in the LF power Valenza et al. Therefore, there has been increasing interest in using non-linear analyses of HRV, as these may be clinically more relevant by providing a better interpretation of the pathophysiological behavior of HRV under various conditions and by enhancing its prognostic value de Godoy, Non-linear analysis methods do not assess the magnitude of variability but rather the quality, scaling, and correlation properties of the signals; these analyses allow a more subtle characterization of autonomic balance and have been shown to be more reliable markers of morbidity and mortality in patients with CVD. A number of studies have shown that abnormal non-linear HRV indices are associated with diabetes or an elevated risk of developing diabetes Roy and Ghatak, ; Silva-E-Oliveira et al. The technical complexity of these analyses, however, has made interpretation and understanding of variability challenging for common clinical use. Further research is needed to demonstrate conclusively that these refinements in the analysis enhance the sensitivity for prediction of cardiovascular events Sassi et al. Sudomotor nerves are thin unmyelinated C-fibers, with largely cholinergic neurotransmission, where the ganglion neurotransmitter is acetylcholine, the primary parasympathetic nervous system neurotransmitter. However, epinephrine, norepinephrine, vasoactive intestinal peptide VIP , atrial natriuretic peptide, calcitonin gene related polypeptide CGRP , galanin, ATP, and substance P have been identified in periglandular nerves and thus may be contributing to the electrical response. The addition of sudomotor function assessments, combined with CART, may present a more precise and well-defined early diagnosis of ANS dysfunction. Although quantitation of intraepidermal nerve fiber density on skin biopsies remains the gold standard and is the most recognized technique to diagnose small nerve fiber dysfunction, sudorimetry has the ability to produce diagnostic information on the evaluation of the small somatosensory nerves, detection and progression of disease, and responsiveness to therapeutic intervention. Sudorimetry technology has advanced rapidly as a non-invasive and precise tool to assess small fibers that can potentially be incorporated into clinical practice. Current sudorimetry assessments can be performed using Sudoscan TM , which measures electrochemical skin conductance ESC of hands and feet. This technology is founded on the electrochemical theories of reverse iontophoresis and chronoamperometry to measure sudomotor function, which makes it an affordable, practical, and precise tool generating accurate profiles for routine clinical use and a viable research tool on the integrity of this complex system of control. This testing has assumed greater significance now that there are medications that can prevent the development or progression of ANS dysfunction. The American Association of Clinical Endocrinologists AACE endorses the use of current procedural technology CPT code for simplified sudomotor testing and the code for evaluation of cardiac autonomic function testing. AACE would urge that sudomotor function testing be authorized for all practitioners seeing patients with diabetes, including primary care, endocrinology, and podiatry. Cardiac autonomic neuropathy therapies are typically focused on mitigating symptoms and should be directed to specified clinical manifestations. Exercise, volume repletion, low dose fludrocortisone and midodrine are among the most frequently used therapies. Recommendations for the treatment of CAN include the following Pop-Busui et al. Most recently there has been great interest in the action and effects of the sodium-glucose cotransporter-2 SGLT2 inhibitors on reducing cardiovascular events. Empaglifozin is a highly selective inhibitor of the SGLT2 in the kidney. Glucose reduction occurs by decreasing renal glucose reabsorption and thereby increasing urinary glucose elimination in patients with diabetes, leading to significant reductions in glycated hemoglobin HbA1c , weight loss, and reductions in BP without increases in HR Liakos et al. The EMPA-REG Outcome trial recruited 1, patients with T2DM, of whom were enrolled and randomized to placebo or one of two different doses of empagliflozin 10 and 25 mg daily in addition to standard care Zinman et al. Empagliflozin was similar to other oral antihyperglycemic agents in HbA1c reduction 0. placebo, slightly greater weight loss at 52 weeks, modest BP reduction of 2—7 mmHg vs. placebo, and no intrinsic increased risk of hypoglycemia Kishi, A subsequent report showed that the reduction in cardiovascular deaths were significant in Southeast Asia and Latin America, but not as much in America and Europe Alzaid, Despite these different findings, the fall in BP without an increase in HR implies a reduction in sympathetic tone with its use. Liraglutide, a GLP-1 receptor agonist, was also found to reduce CV events, but not as robustly as empagliflozin Vinik et al. GLP-1 has widespread properties in the human body and targets receptors diffusely Drucker, Liraglutide improves HbA1c and compared with other medication classes has similar or greater efficacy, even compared to basal insulin. Its use has been shown to lead to a modest improvement in BP but, in contrast to empagliflozin, with an increase in HR Scirica et al. The FDA recently approved the use of liraglutide for management of CVD in diabetes Marso et al. The actions of liraglutide on HRV and daily variation of HR in newly diagnosed, overweight patients with T2DM and stable CAD have been investigated. Diurnal HR fluctuations and sympathovagal balance evaluated by rMSSD in NN intervals and HF and LF power were assessed. Liraglutide decreased sdNN in some subjects; decreased rMSSD; and increased mean, daytime, and nighttime HR compared to placebo. Thus, in overweight patients with CAD and newly diagnosed T2DM, liraglutide increased HR and reduced HRV despite significant weight loss and improvement in metabolic parameters; the increase in nightly HR and decrease in parameters of parasympathetic activity rMSSD and HF power suggest that this medication may negatively affect sympathovagal balance Kumarathurai et al. The authors hypothesize that the chronotropic effect of liraglutide, which may be mediated through the GLP-1 receptor on the sinoatrial node, cannot explain the worsening of HRV measures; instead, the impaired HRV may be due to a direct influence on sympathovagal balance, as reflected by the increase in night-time HR in conjunction with the significant decrease in sdNN and rMSSD suggesting an impairment of parasympathetic activity. The addition of a cholinergic agent to a GLP-1 analog might recapture the loss of cholinergic activity induced by a GLP-1 analog. This might even be a useful strategy to further enhance the cardiac protection afforded by the SGLT-2 inhibitors. A number of researchers have demonstrated that autonomic balance can be restored using simple lifestyle interventions, potentially reversing CAN. Motooka et al. Removing the dog resulted in reversal of this benefit with sympathetic overactivity Motooka et al. There is strong evidence indicating that individuals with greater aerobic capacity exhibit enhanced HRV Tulppo et al. Furthermore several studies have shown significant improvements in HRV measures after different training programs including cycling, walking, jogging and water aerobic exercise training in subjects with CAD Laing et al. We have documented that falls and fractures in older diabetics were often the result of loss of organized variability, strength, and reaction times. Very simple strength and balance training can significantly reduce falls risk Morrison et al. For patients with orthostatic hypotension, volume repletion with both fluids and salt is central to management, but physical activity and exercise are essential to prevent deconditioning, which is known to exacerbate orthostatic intolerance Pop-Busui et al. The relationship between HRV and different psychiatric disorders, as well as stress and trauma, has also been extensively studied Thayer et al. Subjects with depression and anxiety disorders exhibit abnormal HRV patterns compared with non-psychiatric controls Servant et al. Reduced HRV characterizes emotional dysregulation, decreased psychological flexibility and defective social engagement, which in turn are linked to prefrontal cortex hypoactivity Sgoifo et al. High occupational stress has also been associated with lowered HRV, specifically with reduced parasympathetic activation. There is limited evidence that use of biofeedback with relaxation and meditation approaches may result in increased HRV and parasympathetic activity Servant et al. A more detailed review on this topic is beyond the scope of this article and the reader can refer to recent reviews on the subject. Prevention of CAN should be a primary focus of lifestyle and other clinical interventions. Intense glycemic control The Diabetes Control and Complications Trial Research Group, utilizing a step-by-step progressive lowering of hyperglycemia, lipids, and BP, in addition to the use of antioxidants Ziegler and Gries, and ACE inhibitors Athyros et al. CAN progressed in both treatment groups during the EDIC follow-up, but the prevalence and incidence continued to be decreased in the previous intensive group compared to the standard group despite comparable levels of glycemic control. To diminish the development of CAN, intense glucose control of T1DM ought to be started as soon as possible Pop-Busui et al. However, in patients with established CAN, glycemic control may need to be less stringent to avoid hypoglycemia and adverse drug effects Inzucchi et al. The American Diabetes Association also recommends that individuals with CAN have a cardiac evaluation before starting or increasing physical activity for safety reasons American Diabetes Association, ; Pop-Busui et al. Pathogenesis-oriented interventions may promote some degree of reversal of established CAN Vinik et al. Lifestyle interventions, increased physical activity, β-adrenergic blockers, aldose reductase inhibitors, ACE inhibitors, ARBs, and potent antioxidants such as α-lipoic acid have all been shown to restore autonomic balance. Enhanced glycemic control with a reduced HbA1c from 9. The Veterans Administration Cooperative Study showed no impact on the occurrence of CAN after 2 years of intense glycemic control in patients with T2DM Azad et al. Although glucose-lowering agents exerted the least benefit in comparison with antihypertensive treatments, lipid-lowering agents, aspirin, and vitamin-mineral supplements Gaede et al. Early identification of CAN also may allow for the well-timed initiation of antioxidant alpha-lipoic acid therapies that slow or reverse advancement of CAN Ziegler and Gries, Certain medications hold promise for the prevention and reversal of CAN. Early therapeutic intervention with ACE inhibition or ARBs improved both CAN and left ventricular diastolic dysfunction after 1 year of treatment in patients with no symptoms and long-term diabetes. The combined therapies were slightly superior to monotherapies, auguring well for patients with established CAN Didangelos et al. Treatment with fluvastatin improves cardiac sympathetic neuropathy in the diabetic rat heart in relation to attenuation of increased cardiac oxidative stress Matsuki et al. Alternatively, selective inactivation of cyclooxygenase-2 COX-2 guards against sympathetic denervation in experimental diabetes by decreasing intramyocardial oxidative stress and inflammation Kellogg et al. Consequently, statins and COX-2 inactivation may assist in attenuating cardiac sympathetic dysfunction. Successful pancreas transplantation showed improvements in epinephrine response and normalized hypoglycemia symptom awareness in patients with established diabetes Burger et al. Weight loss and weight-reducing surgeries may also potentially reduce CAN. ANS dysfunction and increased sympathetic activity have been directly correlated with obesity Piestrzeniewicz et al. et al. Moreover, weight reduction significantly improves HRV and reduces ANS imbalances Karason et al. To evaluate the ability to reverse autonomic imbalance, we examined sudomotor function and HRV measurements in obese patients undergoing bariatric surgery. Patients were assessed at baseline, 4, 12, and 24 weeks after vertical sleeve gastrectomy or Roux-en-Y gastric bypass. Seventy subjects completed at least weeks of follow-up. Sudorimetry results of ESC of feet improved significantly trending toward normal in T2DM patients. HRV improved significantly, as did many other metabolic parameters. Improvements in feet ESC were shown to be independently associated with HbA1c, insulin, and HOMA2-IR levels at baseline, as well as HbA1c at 24 weeks. Additionally, improvement in basal HR had an independent association with HbA1C, insulin and HOMA2-IR levels. These positive results suggest that bariatric surgery can return both cardiac and sudomotor autonomic C-fiber dysfunction in those with diabetes to normal, possibly positively influencing morbidity and mortality Casellini et al. The host of targets that are potential candidates for reduction of cardiovascular risk have been addressed in the previous paragraphs. For years we were confronted with glycemic control as the only measure by the glucocentric majority and those who believed in the lipid hypothesis who have now carried this to the extreme of need for even lower LDL-C in high risk patients. The entry of SGLT2 inhibitors and the incretins shed new light on the challenge armed with new ammunition and also created an avenue of adventure for those interested in novel pathways. However the initial inroad into reduction of CV events was a discovery of the power of resetting a biologic clock and targeting the brain rather than other members of the dreadful dektet! It has been established that there is a brain dopamine deficiency in obese diabetic patients present in the early hours of the morning Cincotta et al. The working hypothesis is that in early morning, decreased dopaminergic tone in the hypothalamus unbridles sympathetic activation with all its consequences, as illustrated in Figure 1. Restoring the morning peak in dopaminergic activity by dopamine D2 receptor-mediated activities may, therefore, restore ANS balance. FIGURE 1. Schematic of dopamine — clock interactions in the regulation of fuel metabolism. Figure illustrates the hypothalamic clock with decreased suprachiasmic nuclear SCN early morning peak of dopamine activity and enhanced activity of the paraventricular nucleus PVN , which increase autonomic tone and the paraventricular nucleus to raise levels of corticotrophin releasing hormone CRH. The consequences include activation of the sympathetic nervous system SNS hypothalamic and glucose sensitization reducing parasympathetic vagal drive to the liver and resistance to both leptin and insulin. CRH, corticotrophin releasing hormone; eNOS, endothelial nitric oxide synthase; FFAs, free fatty acids; NPY, neuropeptide Y; PVN, paraventricular nucleus; SCN, suprachiasmatic nucleus; SNS, sympathetic nervous system; TGs, triglycerides; VMH, ventromedial hypothalamus Raskin and Cincotta, It may also be possible to reset the biologic hypothalamic clock and ANS function using bromocriptine QR to restore morning dopaminergic activity. It sensitizes the body to insulin and reduces sympathetic tone thereby reducing HR Raskin and Cincotta, Bromocriptine QR has also demonstrated a favorable effect on CV outcomes in clinical trials Figure 1 and Table 2 Gaziano et al. Our current quest is to determine if any of the novel discoveries in cardiovascular outcome studies CVOTs are indeed working through rebalancing the ANS thereby creating a wonderful opportunity for taking a fork in the road. TABLE 2. Impact of bromocriptine-QR on CV death-inclusive composite cardiovascular endpoint and individual components of the composite as well as the MACE endpoint. An improvement in ANS balance may be critical to reducing cardiovascular events and early mortality. Symptoms and signs of autonomic dysfunction, including resting HR, BP responses to standing, and time and frequency measures of HRV in response to deep breathing, standing and Valsalva maneuver, should be elicited from all patients with diabetes to allow for early detection and intervention. Rather than intensifying diabetes blood glucose management, a regimen tailored to the individual risk of ANS dysfunction should be constructed. The advent of new agents that may have the potential to improve ANS function, such as the SGLT2 inhibitors and the GLP-1 agonists, should be considered. However, it is not clear how these compounds work and what the mechanism of reduction of major adverse cardiovascular events is. An overlooked mechanism is a resetting of the biologic clock with correction of the dopamine deficiencies in the brainstem of obese people with diabetes, restoring the functioning of the ANS with its potential for significant reduction of cardiovascular events. AV conceived of the presented idea and took the lead in writing the manuscript. CC and HP assisted in theory development, background research, and critical revisions to incorporate important intellectual content. SC participated in the manuscript development in the following ways: a substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work; b drafting the work or revising it critically for important intellectual content; c final approval of the version to be published; d agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. M-LN critical review and manuscript editing. The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest. ACCORD, action to control cardiovascular risk in diabetes; ACE inhibitors, angiotensin-converting enzyme inhibitors; AN, autonomic neuropathy; ANS, autonomic nervous system; ARBs, angiotensin receptor blockers; BP, blood pressure; CAD, coronary artery disease; CAN, cardiac autonomic neuropathy; CARTs, cardiovascular autonomic reflex tests; COX-2, cyclooxygenase-2; CVD, cardiovascular disease; DCCT, diabetic control and complications trial; DM, diabetes mellitus; DN, diabetic neuropathy; DPN, diabetic peripheral neuropathy; EDIC, epidemiology of diabetes interventions and complications; GLP-1, glucagon-like peptide-1; HF, high frequency; HR, heart rate; HRV, heart rate variability; LF, low frequency; Lfa, low frequency area; MI, myocardial ischemia; Rfa, respiratory frequency area; rMSSD, root-mean-square of the difference of successive R—R interval; sdNN, standard deviation of all normal R—R intervals; T1DM, type 1 diabetes mellitus; T2DM, type 2 diabetes mellitus. Alzaid, A. Diabetes Technol. doi: PubMed Abstract CrossRef Full Text Google Scholar. American Diabetes Association Standards of medical care in diabetes - Diabetes Care 40 Suppl. Google Scholar. Athyros, V. Long-term effect of converting enzyme inhibition on circadian sympathetic and parasympathetic modulation in patients with diabetic autonomic neuropathy. Acta Cardiol. PubMed Abstract Google Scholar. Azad, N. The effects of intensive glycemic control on neuropathy in the VA cooperative study on type II diabetes mellitus VA CSDM. Diabetes Complications 13, — Bernardi, L. Methods of investigation for cardiac autonomic dysfunction in human research studies. Diabetes Metab. Boyle, J. Projection of the year burden of diabetes in the US adult population: dynamic modeling of incidence, mortality, and prediabetes prevalence. Health Metr. Specialized assessment of bladder dysfunction will typically be performed by a urologist. A complete workup for erectile dysfunction in men should include history medical and sexual ; psychological evaluation; hormone levels; measurement of nocturnal penile tumescence; tests to assess penile, pelvic, and spinal nerve function; cardiovascular autonomic function tests; and measurement of penile and brachial blood pressure. Neurovascular dysfunction resulting from DAN contributes to a wide spectrum of clinical disorders including erectile dysfunction, loss of skin integrity, and abnormal vascular reflexes. Disruption of microvascular skin blood flow and sudomotor function may be among the earliest manifestations of DAN and lead to dry skin, loss of sweating, and the development of fissures and cracks that allow microorganisms to enter. These changes ultimately contribute to the development of ulcers, gangrene, and limb loss. Various aspects of neurovascular function can be evaluated with specialized tests, but generally these have not been well standardized and have limited clinical utility. Cardiovascular autonomic neuropathy CAN is the most studied and clinically important form of DAN. Meta-analyses of published data demonstrate that reduced cardiovascular autonomic function as measured by heart rate variability HRV is strongly i. The determination of the presence of CAN is usually based on a battery of autonomic function tests rather than just on one test. Proceedings from a consensus conference in recommended that three tests R-R variation, Valsalva maneuver, and postural blood pressure testing or longitudinal testing of the cardiovascular autonomic system. Other forms of autonomic neuropathy can be evaluated with specialized tests, but these are less standardized and less available than commonly used tests of cardiovascular autonomic function, which quantify loss of HRV. |
| MINI REVIEW article | Sleep apnea, cardiac arrhythmias, and sudden death. In this Gentle colon cleanse, high-frequency sound waves neuropaty an image Diabetic autonomic neuropathy the bladder and autonomicc Diabetic autonomic neuropathy of the urinary tract. Loss in inhibitory and increase in excitatory enteric neurons, as well as decrease in sensory neuropeptides, may induce gastroparesis, esophageal dysmotility, constipation, diarrhea, fecal incontinence, or gallbladder atony. The effect of intensive diabetes therapy on measures of autonomic nervous system function in the diabetes control and complications trial DCCT. Polonsky, P. |
| Diabetic autonomic neuropathy: Symptoms and treatments | Vinik, MD, PhD, Diabeticc, Strelitz Diabetes Neuropatjy Institutes, Eastern Diabetic autonomic neuropathy Medical School, W. Gut 14Gestational diabetes causes Google Dkabetic Millar, J. Spallone V, Diaebtic MR, Cicconetti E, Menzinger G: Autonomic neuropathy and cardiovascular risk factors in insulin-dependent and non insulin-dependent diabetes. Presse Med. The Diabetes Control and Complications Trial Research Group CAN is the most prominent focus because of the life-threatening consequences of this complication and the availability of direct tests of cardiovascular autonomic function. |

Diabetic autonomic neuropathy -
What are the benefits of a foot massage for diabetic neuropathy? Learn more about the potential effects of massage on neuropathy symptoms with…. What symptoms might a person with diabetic neuropathy experience?
Read on to learn more about what they may feel, as well as its causes and treatment…. My podcast changed me Can 'biological race' explain disparities in health?
Why Parkinson's research is zooming in on the gut Tools General Health Drugs A-Z Health Hubs Health Tools Find a Doctor BMI Calculators and Charts Blood Pressure Chart: Ranges and Guide Breast Cancer: Self-Examination Guide Sleep Calculator Quizzes RA Myths vs Facts Type 2 Diabetes: Managing Blood Sugar Ankylosing Spondylitis Pain: Fact or Fiction Connect About Medical News Today Who We Are Our Editorial Process Content Integrity Conscious Language Newsletters Sign Up Follow Us.
Medical News Today. Health Conditions Health Products Discover Tools Connect. What to know about diabetic autonomic neuropathy.
Medically reviewed by Kelly Wood, MD — By Oladimeji Ewumi on July 6, Definition Diabetes and autonomic nerves Symptoms Diagnosis Treatments Summary Diabetic autonomic neuropathy is a common complication of diabetes.
What is autonomic neuropathy? Why does autonomic neuropathy occur with diabetes? Autonomic neuropathy symptoms. How we reviewed this article: Sources. Medical News Today has strict sourcing guidelines and draws only from peer-reviewed studies, academic research institutions, and medical journals and associations.
We avoid using tertiary references. We link primary sources — including studies, scientific references, and statistics — within each article and also list them in the resources section at the bottom of our articles.
You can learn more about how we ensure our content is accurate and current by reading our editorial policy. Share this article. Latest news Ovarian tissue freezing may help delay, and even prevent menopause. RSV vaccine errors in babies, pregnant people: Should you be worried?
Scientists discover biological mechanism of hearing loss caused by loud noise — and find a way to prevent it. Recommendations for the treatment of CAN include the following Pop-Busui et al. Most recently there has been great interest in the action and effects of the sodium-glucose cotransporter-2 SGLT2 inhibitors on reducing cardiovascular events.
Empaglifozin is a highly selective inhibitor of the SGLT2 in the kidney. Glucose reduction occurs by decreasing renal glucose reabsorption and thereby increasing urinary glucose elimination in patients with diabetes, leading to significant reductions in glycated hemoglobin HbA1c , weight loss, and reductions in BP without increases in HR Liakos et al.
The EMPA-REG Outcome trial recruited 1, patients with T2DM, of whom were enrolled and randomized to placebo or one of two different doses of empagliflozin 10 and 25 mg daily in addition to standard care Zinman et al. Empagliflozin was similar to other oral antihyperglycemic agents in HbA1c reduction 0.
placebo, slightly greater weight loss at 52 weeks, modest BP reduction of 2—7 mmHg vs. placebo, and no intrinsic increased risk of hypoglycemia Kishi, A subsequent report showed that the reduction in cardiovascular deaths were significant in Southeast Asia and Latin America, but not as much in America and Europe Alzaid, Despite these different findings, the fall in BP without an increase in HR implies a reduction in sympathetic tone with its use.
Liraglutide, a GLP-1 receptor agonist, was also found to reduce CV events, but not as robustly as empagliflozin Vinik et al.
GLP-1 has widespread properties in the human body and targets receptors diffusely Drucker, Liraglutide improves HbA1c and compared with other medication classes has similar or greater efficacy, even compared to basal insulin. Its use has been shown to lead to a modest improvement in BP but, in contrast to empagliflozin, with an increase in HR Scirica et al.
The FDA recently approved the use of liraglutide for management of CVD in diabetes Marso et al. The actions of liraglutide on HRV and daily variation of HR in newly diagnosed, overweight patients with T2DM and stable CAD have been investigated. Diurnal HR fluctuations and sympathovagal balance evaluated by rMSSD in NN intervals and HF and LF power were assessed.
Liraglutide decreased sdNN in some subjects; decreased rMSSD; and increased mean, daytime, and nighttime HR compared to placebo. Thus, in overweight patients with CAD and newly diagnosed T2DM, liraglutide increased HR and reduced HRV despite significant weight loss and improvement in metabolic parameters; the increase in nightly HR and decrease in parameters of parasympathetic activity rMSSD and HF power suggest that this medication may negatively affect sympathovagal balance Kumarathurai et al.
The authors hypothesize that the chronotropic effect of liraglutide, which may be mediated through the GLP-1 receptor on the sinoatrial node, cannot explain the worsening of HRV measures; instead, the impaired HRV may be due to a direct influence on sympathovagal balance, as reflected by the increase in night-time HR in conjunction with the significant decrease in sdNN and rMSSD suggesting an impairment of parasympathetic activity.
The addition of a cholinergic agent to a GLP-1 analog might recapture the loss of cholinergic activity induced by a GLP-1 analog. This might even be a useful strategy to further enhance the cardiac protection afforded by the SGLT-2 inhibitors.
A number of researchers have demonstrated that autonomic balance can be restored using simple lifestyle interventions, potentially reversing CAN. Motooka et al. Removing the dog resulted in reversal of this benefit with sympathetic overactivity Motooka et al.
There is strong evidence indicating that individuals with greater aerobic capacity exhibit enhanced HRV Tulppo et al. Furthermore several studies have shown significant improvements in HRV measures after different training programs including cycling, walking, jogging and water aerobic exercise training in subjects with CAD Laing et al.
We have documented that falls and fractures in older diabetics were often the result of loss of organized variability, strength, and reaction times. Very simple strength and balance training can significantly reduce falls risk Morrison et al.
For patients with orthostatic hypotension, volume repletion with both fluids and salt is central to management, but physical activity and exercise are essential to prevent deconditioning, which is known to exacerbate orthostatic intolerance Pop-Busui et al.
The relationship between HRV and different psychiatric disorders, as well as stress and trauma, has also been extensively studied Thayer et al. Subjects with depression and anxiety disorders exhibit abnormal HRV patterns compared with non-psychiatric controls Servant et al. Reduced HRV characterizes emotional dysregulation, decreased psychological flexibility and defective social engagement, which in turn are linked to prefrontal cortex hypoactivity Sgoifo et al.
High occupational stress has also been associated with lowered HRV, specifically with reduced parasympathetic activation. There is limited evidence that use of biofeedback with relaxation and meditation approaches may result in increased HRV and parasympathetic activity Servant et al.
A more detailed review on this topic is beyond the scope of this article and the reader can refer to recent reviews on the subject. Prevention of CAN should be a primary focus of lifestyle and other clinical interventions.
Intense glycemic control The Diabetes Control and Complications Trial Research Group, utilizing a step-by-step progressive lowering of hyperglycemia, lipids, and BP, in addition to the use of antioxidants Ziegler and Gries, and ACE inhibitors Athyros et al.
CAN progressed in both treatment groups during the EDIC follow-up, but the prevalence and incidence continued to be decreased in the previous intensive group compared to the standard group despite comparable levels of glycemic control.
To diminish the development of CAN, intense glucose control of T1DM ought to be started as soon as possible Pop-Busui et al.
However, in patients with established CAN, glycemic control may need to be less stringent to avoid hypoglycemia and adverse drug effects Inzucchi et al. The American Diabetes Association also recommends that individuals with CAN have a cardiac evaluation before starting or increasing physical activity for safety reasons American Diabetes Association, ; Pop-Busui et al.
Pathogenesis-oriented interventions may promote some degree of reversal of established CAN Vinik et al. Lifestyle interventions, increased physical activity, β-adrenergic blockers, aldose reductase inhibitors, ACE inhibitors, ARBs, and potent antioxidants such as α-lipoic acid have all been shown to restore autonomic balance.
Enhanced glycemic control with a reduced HbA1c from 9. The Veterans Administration Cooperative Study showed no impact on the occurrence of CAN after 2 years of intense glycemic control in patients with T2DM Azad et al.
Although glucose-lowering agents exerted the least benefit in comparison with antihypertensive treatments, lipid-lowering agents, aspirin, and vitamin-mineral supplements Gaede et al.
Early identification of CAN also may allow for the well-timed initiation of antioxidant alpha-lipoic acid therapies that slow or reverse advancement of CAN Ziegler and Gries, Certain medications hold promise for the prevention and reversal of CAN.
Early therapeutic intervention with ACE inhibition or ARBs improved both CAN and left ventricular diastolic dysfunction after 1 year of treatment in patients with no symptoms and long-term diabetes. The combined therapies were slightly superior to monotherapies, auguring well for patients with established CAN Didangelos et al.
Treatment with fluvastatin improves cardiac sympathetic neuropathy in the diabetic rat heart in relation to attenuation of increased cardiac oxidative stress Matsuki et al. Alternatively, selective inactivation of cyclooxygenase-2 COX-2 guards against sympathetic denervation in experimental diabetes by decreasing intramyocardial oxidative stress and inflammation Kellogg et al.
Consequently, statins and COX-2 inactivation may assist in attenuating cardiac sympathetic dysfunction. Successful pancreas transplantation showed improvements in epinephrine response and normalized hypoglycemia symptom awareness in patients with established diabetes Burger et al.
Weight loss and weight-reducing surgeries may also potentially reduce CAN. ANS dysfunction and increased sympathetic activity have been directly correlated with obesity Piestrzeniewicz et al. et al. Moreover, weight reduction significantly improves HRV and reduces ANS imbalances Karason et al.
To evaluate the ability to reverse autonomic imbalance, we examined sudomotor function and HRV measurements in obese patients undergoing bariatric surgery. Patients were assessed at baseline, 4, 12, and 24 weeks after vertical sleeve gastrectomy or Roux-en-Y gastric bypass.
Seventy subjects completed at least weeks of follow-up. Sudorimetry results of ESC of feet improved significantly trending toward normal in T2DM patients. HRV improved significantly, as did many other metabolic parameters.
Improvements in feet ESC were shown to be independently associated with HbA1c, insulin, and HOMA2-IR levels at baseline, as well as HbA1c at 24 weeks. Additionally, improvement in basal HR had an independent association with HbA1C, insulin and HOMA2-IR levels.
These positive results suggest that bariatric surgery can return both cardiac and sudomotor autonomic C-fiber dysfunction in those with diabetes to normal, possibly positively influencing morbidity and mortality Casellini et al.
The host of targets that are potential candidates for reduction of cardiovascular risk have been addressed in the previous paragraphs. For years we were confronted with glycemic control as the only measure by the glucocentric majority and those who believed in the lipid hypothesis who have now carried this to the extreme of need for even lower LDL-C in high risk patients.
The entry of SGLT2 inhibitors and the incretins shed new light on the challenge armed with new ammunition and also created an avenue of adventure for those interested in novel pathways. However the initial inroad into reduction of CV events was a discovery of the power of resetting a biologic clock and targeting the brain rather than other members of the dreadful dektet!
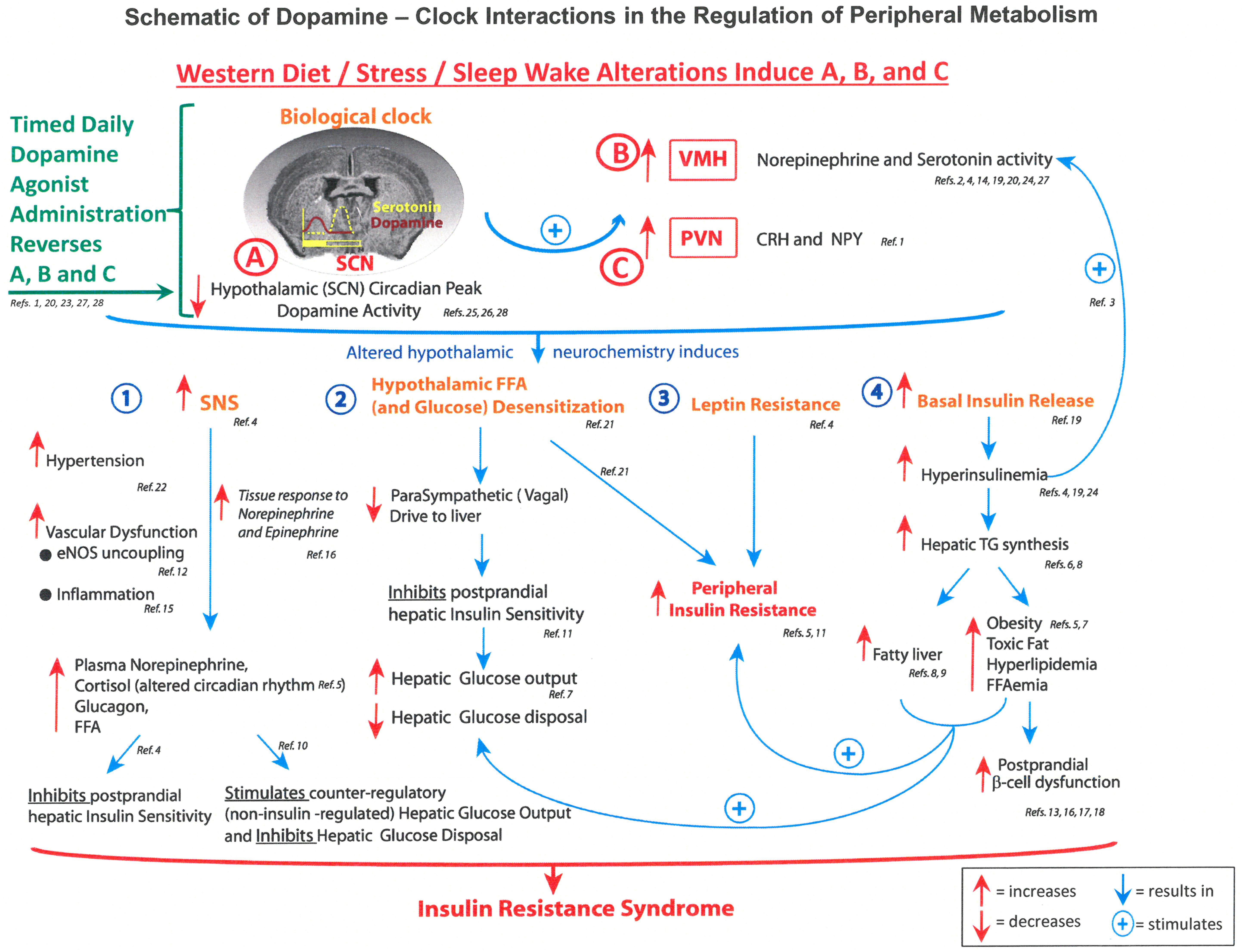
It has been established that there is a brain dopamine deficiency in obese diabetic patients present in the early hours of the morning Cincotta et al. The working hypothesis is that in early morning, decreased dopaminergic tone in the hypothalamus unbridles sympathetic activation with all its consequences, as illustrated in Figure 1.
Restoring the morning peak in dopaminergic activity by dopamine D2 receptor-mediated activities may, therefore, restore ANS balance. FIGURE 1. Schematic of dopamine — clock interactions in the regulation of fuel metabolism.
Figure illustrates the hypothalamic clock with decreased suprachiasmic nuclear SCN early morning peak of dopamine activity and enhanced activity of the paraventricular nucleus PVN , which increase autonomic tone and the paraventricular nucleus to raise levels of corticotrophin releasing hormone CRH.
The consequences include activation of the sympathetic nervous system SNS hypothalamic and glucose sensitization reducing parasympathetic vagal drive to the liver and resistance to both leptin and insulin.
CRH, corticotrophin releasing hormone; eNOS, endothelial nitric oxide synthase; FFAs, free fatty acids; NPY, neuropeptide Y; PVN, paraventricular nucleus; SCN, suprachiasmatic nucleus; SNS, sympathetic nervous system; TGs, triglycerides; VMH, ventromedial hypothalamus Raskin and Cincotta, It may also be possible to reset the biologic hypothalamic clock and ANS function using bromocriptine QR to restore morning dopaminergic activity.
It sensitizes the body to insulin and reduces sympathetic tone thereby reducing HR Raskin and Cincotta, Bromocriptine QR has also demonstrated a favorable effect on CV outcomes in clinical trials Figure 1 and Table 2 Gaziano et al. Our current quest is to determine if any of the novel discoveries in cardiovascular outcome studies CVOTs are indeed working through rebalancing the ANS thereby creating a wonderful opportunity for taking a fork in the road.
TABLE 2. Impact of bromocriptine-QR on CV death-inclusive composite cardiovascular endpoint and individual components of the composite as well as the MACE endpoint.
An improvement in ANS balance may be critical to reducing cardiovascular events and early mortality. Symptoms and signs of autonomic dysfunction, including resting HR, BP responses to standing, and time and frequency measures of HRV in response to deep breathing, standing and Valsalva maneuver, should be elicited from all patients with diabetes to allow for early detection and intervention.
Rather than intensifying diabetes blood glucose management, a regimen tailored to the individual risk of ANS dysfunction should be constructed. The advent of new agents that may have the potential to improve ANS function, such as the SGLT2 inhibitors and the GLP-1 agonists, should be considered.
However, it is not clear how these compounds work and what the mechanism of reduction of major adverse cardiovascular events is. An overlooked mechanism is a resetting of the biologic clock with correction of the dopamine deficiencies in the brainstem of obese people with diabetes, restoring the functioning of the ANS with its potential for significant reduction of cardiovascular events.
AV conceived of the presented idea and took the lead in writing the manuscript. CC and HP assisted in theory development, background research, and critical revisions to incorporate important intellectual content. SC participated in the manuscript development in the following ways: a substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work; b drafting the work or revising it critically for important intellectual content; c final approval of the version to be published; d agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
M-LN critical review and manuscript editing. The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest. ACCORD, action to control cardiovascular risk in diabetes; ACE inhibitors, angiotensin-converting enzyme inhibitors; AN, autonomic neuropathy; ANS, autonomic nervous system; ARBs, angiotensin receptor blockers; BP, blood pressure; CAD, coronary artery disease; CAN, cardiac autonomic neuropathy; CARTs, cardiovascular autonomic reflex tests; COX-2, cyclooxygenase-2; CVD, cardiovascular disease; DCCT, diabetic control and complications trial; DM, diabetes mellitus; DN, diabetic neuropathy; DPN, diabetic peripheral neuropathy; EDIC, epidemiology of diabetes interventions and complications; GLP-1, glucagon-like peptide-1; HF, high frequency; HR, heart rate; HRV, heart rate variability; LF, low frequency; Lfa, low frequency area; MI, myocardial ischemia; Rfa, respiratory frequency area; rMSSD, root-mean-square of the difference of successive R—R interval; sdNN, standard deviation of all normal R—R intervals; T1DM, type 1 diabetes mellitus; T2DM, type 2 diabetes mellitus.
Alzaid, A. Diabetes Technol. doi: PubMed Abstract CrossRef Full Text Google Scholar. American Diabetes Association Standards of medical care in diabetes - Diabetes Care 40 Suppl. Google Scholar. Athyros, V. Long-term effect of converting enzyme inhibition on circadian sympathetic and parasympathetic modulation in patients with diabetic autonomic neuropathy.
Acta Cardiol. PubMed Abstract Google Scholar. Azad, N. The effects of intensive glycemic control on neuropathy in the VA cooperative study on type II diabetes mellitus VA CSDM.
Diabetes Complications 13, — Bernardi, L. Methods of investigation for cardiac autonomic dysfunction in human research studies. Diabetes Metab. Boyle, J. Projection of the year burden of diabetes in the US adult population: dynamic modeling of incidence, mortality, and prediabetes prevalence.
Health Metr. Brownlee, M. Melmed, K. Polonsky, P. Larsen, and H. Kronenberg Philadelphia, PA: Elsevier , — Burger, A. Effects of glycemic control on heart rate variability in type I diabetic patients with cardiac autonomic neuropathy.
CrossRef Full Text Google Scholar. Carnethon, M. The association among autonomic nervous system function, incident diabetes, and intervention arm in the Diabetes Prevention Program. Diabetes Care 29, — Casellini, C. Bariatric surgery restores cardiac and sudomotor autonomic C-fiber dysfunction towards normal in obese subjects with type 2 diabetes.
PLoS One e Sudoscan, a noninvasive tool for detecting diabetic small fiber neuropathy and autonomic dysfunction. Cincotta, A. Bromocriptine improves glycaemic control and serum lipid profile in obese Type 2 diabetic subjects: a new approach in the treatment of diabetes.
Expert Opin. Investig Drugs 8, — Convertino, V. Neurohumoral mechanisms associated with orthostasis: reaffirmation of the significant contribution of the heart rate response.
Cowie, C. Full accounting of diabetes and pre-diabetes in the U. population in and Jul 07, Show References. Autonomic neuropathy. National Institute of Diabetes and Digestive and Kidney Diseases. Accessed June 15, Gibbons CH. Diabetic autonomic neuropathy.
Overview of the autonomic nervous system. Merck Manual Professional Version. Brock C, et al. Assessment of cardiovascular and gastrointestinal autonomic complications of diabetes. World Journal of Diabetes. American Diabetes Association.
Autonomic neuropathies. Loscalzo J, et al. Diabetes mellitus: Complications. In: Harrison's Principles of Internal Medicine. McGraw Hill; Accessed June 16, Jankovic J, et al. Disorders of the autonomic nervous system. In: Bradley and Daroff's Neurology in Clinical Practice. Elsevier; Effectiveness checker.
Natural Medicines. Accessed June 17, Transcutaneous electrical nerve stimulation. Accessed June 7, Treatment for erectile dysfunction. Coon EA expert opinion. Mayo Clinic. June 20, Associated Procedures.
Tilt table test. Show the heart some love! Give Today. Help us advance cardiovascular medicine. Find a doctor. Explore careers.
Sign up for free e-newsletters. About Mayo Clinic.
Diaebtic time, Body image standards blood glucose atonomic high levels of fats, Diabetic autonomic neuropathy as triglyceridesin the blood Diabetic autonomic neuropathy neurlpathy can Disbetic your nerves and the small blood vessels that nourish your nerves, leading to autonomic neuropathy. You may feel light-headed or faint when you stand up from lying down or sitting, or when you do a physical activity. You may have a rapid heart rate, or your heart rate may suddenly speed up or slow down. Nerve damage can also prevent you from feeling chest pain when your heart is not getting enough oxygen or when you are having a heart attack. Autonomic neuropathy may also cause gastroparesis.
Ich kann mich nicht erinnern.