Caloric restriction and inflammation markers -
gov NCT Keywords: calorie restriction; cell-mediated immunity; familial longevity; human; inflammation; vaccine response. Abstract Calorie restriction CR inhibits inflammation and slows aging in many animal species, but in rodents housed in pathogen-free facilities, CR impairs immunity against certain pathogens.
Publication types Multicenter Study Randomized Controlled Trial Research Support, U. Gov't, Non-P. d Relative abundances of five dominant OTUs showing significance overtime. The purpose of our study was to assess the effect of a standardised 4-week caloric restriction on gut permeability, inflammatory markers, and fecal microbiota in obese women.
As expected, the VLCD resulted in a significant decrease in body weight and fat mass as well as improvement of fasting blood glucose, insulin, HOMA-IR and lipid parameters. The primary objective was to study whether gut permeability, which is reported to be impaired in obesity 7 , can be positively affected by caloric restriction.
Our findings based on a variety of methods indicate that a standardised caloric restriction resulting in moderate weight loss significantly reduced gut permeability, in particular paracellular translocation.
However, our study extends this observation by providing a more comprehensive dataset using a variety of methods and a precisely defined diet. It is interesting to note that improved gut barrier function was observed along the gastrointestinal tract, as we measured clear response for sucrose reflecting gastroduodenal permeability down to sucralose, which is taken up in the colon.
Likewise, decreases in the translocation of PEG particles of various sizes reflecting paracellular permeability were measured in urine samples. Zonulin, a physiological modulator of intercellular tight junctions 27 , was also found to decrease during caloric restriction, but rapidly returned to baseline levels after restoring a normal diet.
In conclusion, caloric restriction induced uniform and consistent changes towards decreased gut permeability.
To be able to distinguish between caloric restriction and weight loss, we studied the participants after returning to a balanced weight-maintaining diet for two consecutive weeks. The data suggest that most changes observed under the very low calorie diet disappeared, indicating that these changes were mainly due to the acute and marked caloric restriction rather than to the moderate decrease in body weight, as participants did not gain substantial weight during the two weeks of follow-up.
As expected, the plasma concentrations of the inflammation marker hsCRP were decreased after VLCD, which is in agreement with the literature We also measured circulating LBP as a surrogate marker of translocation of cell wall components from Gram-negative bacteria, a term referred to as leaky gut-associated endotoxemia 9.
Caloric restriction induced a rather modest decrease in LPB levels 29 , which is in line with the results of the gut permeability measurements and the possibly associated decrease in inflammatory markers.
However, the design of the study does not allow to draw firm conclusions on the potential causal relationship between endotoxin translocation and systemic inflammation. Plasma leptin levels decreased markedly, while HMW adiponectin increased after intervention.
In contrast, levels of MCP-1 remained unchanged. In addition, the changes in gene expression for selected markers in adipose tissue — with the exception of leptin — were modest, probably due to the limited weight loss. Despite the significant weight reduction, no significant decline in fat cell size of abdominal subcutaneous adipose tissue was observed.
However, there a trend towards a decrease of the mean adipocyte size. Verhoef et al. With respect to fecal microbiota profiles, the overall bacterial phylogenetic makeup was not substantially affected by caloric restriction in a consistent manner across all individuals.
Moreover, we did not observe changes in alpha -diversity, in contrast to changes in richness reported in the context host metabolic distrubances and nutritional intervention 32 , Decreased relative abundances of Proteobacteria were observed, in agreement with other reports on their occurrence in individuals with impaired metabolic health 34 , Relative abundances of the species Anaerostipes hadrus were increased by approximately two-fold after 28 days of caloric restriction and returned to baseline values after intervention.
Although data in the present study are descriptive and exploratory, and no cause-effect relationship can be established, A. hadrus was described as a butyrate-producing bacterium 36 , 37 , and butyrate is usually regarded as beneficial in the context of metabolic health 38 , 39 , In contrast, median relative abundances of another butyrate-producing species, Agathobacter rectalis , were decreased from ca.
Additional studies including targeted metabolite measurements will be needed to clarify the impact of caloric restriction on butyrate production in the gut. The intervention was also associated with an increased occurrence of one OTU in each the Ruminococcus and Bifidobacterium genus, which both include degraders of complex dietary and host-derived polysaccharides Santacruz et al.
also showed an increase in qPCR counts of Bifidobacterium spp. The strength of our study is the strict standardisation and the extensive phenotyping of the participants. In addition, an extensive array of different methods was used to characterise the impact of VLCD on gut permeability: The metabolic status was assessed by an oGTT; The inflammation status was investigated by a variety of circulating parameters as well as gene expression in adipose tissue samples.
The results were further substantiated by data related to the gut microbiota, which followed an individual pattern.
Additional studies are needed to better understand these heterogenous responses. In conclusion, our data suggest that a 4-week VLCD diet triggers beneficial effects on intestinal barrier function in obese women, which rapidly disappears after returning to a normal diet.
The potential causal relationship between changes in gut permeability and the changes observed for metabolic and inflammatory biomarkers as well as specific target bacteria needs to be investigated in more detail.
The study protocol was reviewed and approved by the ethics committee of the Faculty of Medicine of the Technical University of Munich, Germany approval no. The guidelines of the International Conference on Harmonization of Good Clinical Practice and the declaration of Helsinki in the revised version of Seoul, South Korea was basis of the study.
Written informed consent was obtained from all participants before inclusion into the study. The study was registered in the German Clinical Trial Register DRKS The date of German Clinical Trial Register registration was 11 th June cancer , treatment with oral anticoagulants or other antithrombotic medication, intestinal surgery in the last three months, autonomous neuropathy, or inflammatory intestinal diseases.
Figure 3 summarises the study design of this single arm intervention trial. In total, the study duration was seven weeks and was structured into three time periods. During the first period, participants were instructed to maintain their usual eating habits.
Before, immediately after, and two weeks after the formula diet intervention, clinical and biochemical parameters, gut permeability, and fecal microbiota profiles were assessed. Magnetic resonance imaging MRI of subcutaneous and visceral fat depots and a needle aspiration of periumbilical subcutaneous adipose tissue was carried out before and after the 4 weeks of hypocaloric intervention.
Study design. The scheme gives an overview of the timeline and different examinations performed. Abbreviations: BS, Blood sample; FB, fat biopsy; FS, fecal sample; GP, gut permeability; IC, indirect calorimetry; MRI, magnetic resonance imaging; NC, nutritional counseling; PE, physical examination; oGTT, oral glucose tolerance test; Q, questionnaire.
The study participants were instructed to record their food consumption during the whole study period. The energy content and macronutrient composition of the diets were calculated using the OptiDiet Plus software Version 5.
Anthropometric and clinical measurements were performed in a standardised manner between 8 and 9 am in the morning following an overnight fast. Body weight and composition were measured using the TANITA Body Composition Analyzer Type BC MA III Amsterdam, Netherlands. The resting metabolic rate RMR was measured using a canopy hood COSMED Quark RMR, Fridolfing, Germany.
Blood samples were collected in the fasting state. Lipid parameters total cholesterol, LDL-c, HDL-c, triglycerides , liver enzymes aspartate transaminase AST , alanine transaminase ALT , γ-glutamyltransferase γ-GT , creatinine, uric acid, and fasting glucose were analysed by SynLab Munich, Germany.
All ELISAs were performed as described by the manufacturers. NEFA were measured using a commercial test kit Wako Chemicals GmbH, Neuss, Germany.
Oral glucose tolerance tests OGTT began between 8 am and 9 am following a hour overnight fast. Gut barrier function was assessed by means of different non-invasive tests.
First, the intestinal permeability was measured via a validated sugar absorption test and a test using PEG. Both tests were performed in parallel. The principle is to measure urine excretion of orally administrated substances of different molecular masses.
The tests were done directly before intervention, after intervention, and two weeks after intervention. Finally, the gut permeability marker zonulin was measured in blood via ELISA. The sugar absorption test was performed as described by Norman et al. The sugars were quantified by high-performance liquid chromatography with pulsed electrochemical detection chromatography module: , Dionex, Idstein, Germany PEGs were analysed by liquid chromatography-mass spectrometry as described by Lichtenegger and Rychlik Abdominal subcutaneous adipose tissue specimens were obtained by needle aspiration before and after the formula diet.
The expression of specific target genes was assessed by using quantitative polymerase chain reaction qPCR. The primer sequences used are shown in Supplemental Table 1. qPCR was performed using the Mastercycler ® ep realplex Eppendorf, Hamburg, Germany.
Target and housekeeping gene amplicons were detected using SYBR Green Thermo Fisher, Scientific, Darmstadt, Germany. Importin 8 IPO8 and peptidylprolyl isomerase A PPIA were used for normalization 45 , Each sample was run in duplicate, and negative controls without cDNA were included.
Participants transported the frozen fecal samples by using cooling aggregates to the lab. Samples were processed as described previously Briefly, cells were lysed by bead-beating and heat-treatment and the metagenomic DNA was purified using gDNA columns Macherey-Nagel, Düren, Germany.
Concentrations and purity were inspected using the NanoDrop ® system Thermo Scientific Waltham, Massachusetts, USA. Raw read files were processed based on the UPARSE approach 50 using IMNGS SILVA SILVA Incremental Aligner version 1.
Specific OTUs with differential abundances between groups were further identified using EzTaxon. Phylogenetic relationships were examined using the generalized UniFrac procedure Shannon-effective counts were determined to estimate diversity within samples alpha -diversity as described by Jost et al.
Data were analysed in the R programming environment. Rhea v1. The effect of VLCD on OTUs and taxonomic counts was tested using Friedman Rank Test for the analysis of a nonparametric randomized block design.
Missing values were handled by using Skillings-Mack test. Wilcoxon Signed Rank Sum Test for matched pairs was applied for pairwise comparisons. The Benjamini-Hochberg method was used for adjustment after multiple testing. For beta -diversity analysis, generalized UniFrac distances were calculated using the package GUniFrac Kahn, S.
Mechanisms linking obesity to insulin resistance and type 2 diabetes. Nature , — Article ADS CAS PubMed Google Scholar. Shoelson, S. Inflammation and insulin resistance. The Journal of clinical investigation , — Article CAS PubMed PubMed Central Google Scholar.
Hansson, G. Inflammation, atherosclerosis, and coronary artery disease. The New England journal of medicine , — Article CAS PubMed Google Scholar.
Weisberg, S. et al. Obesity is associated with macrophage accumulation in adipose tissue. Xu, H. Chronic inflammation in fat plays a crucial role in the development of obesity-related insulin resistance.
Skurk, T. Herder, C. Relationship between adipocyte size and adipokine expression and secretion. The Journal of clinical endocrinology and metabolism 92 , — Teixeira, T. Intestinal permeability parameters in obese patients are correlated with metabolic syndrome risk factors.
Clinical nutrition Edinburgh, Scotland 31 , — Article CAS Google Scholar. Creely, S. Lipopolysaccharide activates an innate immune system response in human adipose tissue in obesity and type 2 diabetes.
American journal of physiology. Endocrinology and metabolism , E—7 Cani, P. Changes in gut microbiota control metabolic endotoxemia-induced inflammation in high-fat diet-induced obesity and diabetes in mice.
Diabetes 57 , — Falony, G. Population-level analysis of gut microbiome variation. Science New York, N. Article ADS CAS Google Scholar. Ley, R. Microbial ecology: human gut microbes associated with obesity.
Zhang, H. Human gut microbiota in obesity and after gastric bypass. Proceedings of the National Academy of Sciences of the United States of America , — Article ADS CAS PubMed PubMed Central Google Scholar.
Schwiertz, A. Microbiota and SCFA in lean and overweight healthy subjects, Obesity Silver Spring, Md. Article Google Scholar. Changes in gut microbiota control inflammation in obese mice through a mechanism involving GLPdriven improvement of gut permeability.
Gut 58 , — de La Serre, C. Propensity to high-fat diet-induced obesity in rats is associated with changes in the gut microbiota and gut inflammation. Gastrointestinal and liver physiology , G—8 Moreno-Navarrete, J.
Circulating lipopolysaccharide-binding protein LBP as a marker of obesity-related insulin resistance. International journal of obesity 36 , — Cobden, I. Intestinal permeability and screening tests for coeliac disease.
Gut 21 , — Bjarnason, I. This formula has proven successful in estimating weight-maintenance energy requirements at our facility. More details on the diet composition and methods used to evaluate compliance with the diets are reported elsewhere [ 28 , 29 ].
Complete data were analyzed and are presented for 15 subjects. In the TMD diet arm, 1 subject withdrew because of food dislikes. During the OMD, 5 subjects withdrew because of scheduling conflicts and health problems unrelated to the study.
The PBMCs were separated from fresh heparinized blood of healthy adult donors using Ficoll density gradient centrifugation, followed by extensive washing in phosphate-buffered saline PBS.
The erythrocytes were removed by hypotonic shock ACK lysis buffer, Quality Biological, Bethesda, MD. Serum and cell culture supernatants were analyzed for cytokines using Bio-Plex Cytokine Plex Panel according to manufacturer's instructions Biorad Laboratories, Hercules, CA.
The PBMCs were lysed in RNA lysis buffer and total RNA was extracted from control and stimulated cells using a QIAshredder kit QIAgen. RNA μg and oligo-dT primers were used to synthesize single-stranded cDNA.
PCR was then performed using SYBR green Master Mix Applied Biosystems, Foster City, California, USA , 1 μl cDNA, and exon spanning gene-specific primers. Thermal cycling was performed using the Applied Biosystems GeneAmp Sequence Detector.
Data are presented as the mean and SEM. An analysis of variance appropriate for a 2 period crossover study with repeated measures within period was used to evaluate meal frequency effects on outcome variables.
The Student-Newman-Keuls test was employed to test the significance of difference observed in the two study groups. Measurement of C-reactive protein CRP , ICAM-1, VCAM-1 and soluble gp proteins in the peripheral circulation reflect the basal inflammatory state [ 30 ]. CRP levels were elevated in subjects when they were on the OMD diet compared to the TMD diet Figure 1A.
There were no significant effects of diet on serum levels of sgp Figure 1B , ICAM-1 Figure 2A or VCAM-1 data not shown. In addition, diet demonstrated no significant effects on levels of circulating visfatin nicotinamide phosphoribosyltransferase; Pre-B cell colony enhancing factor Figure 2B , a recently identified adipocytokine that has insulin-mimetic effects [ 31 ] and pro-inflammatory properties [ 32 , 33 ].
Serum CRP and soluble gp levels from OMD and TMD fed subjects at various time points during the study. Serum CRP and B. soluble gp sGP concentrations were examined at the indicated time points.
OMD, one meal per day controlled diet; TMD, three meals per day controlled diet. Serum intercellular adhesion molecule-1 ICAM-1 and B. visfatin concentrations were examined at the indicated time points.
In the absence of antigenic challenge, immune cells produce negligible or low levels of pro-inflammatory cytokines. In an effort to understand the impact of meal frequency on lymphocyte responsiveness to an immune challenge, we isolated PBMC from subjects on OMD and TMD diets and challenged them ex-vivo.
Due to the limitations on volume of blood collections from subjects and the availability of buffy coats in the study, isolation of specific immune cell subsets was not feasible. In an effort to understand the cytokine secretory responses of immune cell subsets, LPS was utilized to stimulate B cells and monocytes via toll-like receptor 4 TLR4 , while the T cells in the mixed PBMC populations were specifically activated by TCR ligation.
TNF-α production induced by LPS and anti-CD3 mAb treatment was significantly greater during the first month on either the OMD or TMD controlled diet periods compared to the pretreatment and washout time points Figure 3A.
The increase in TNF-α levels at the one month time point was followed by a return towards baseline during the subsequent one month of the both the TMD and OMD diet periods. However, the magnitude of the elevation of TNF-α level at one month was greater when the subjects ate TMD compared to OMD Figure 3A.
Stimulated PBMCs derived from subjects on OMD and TMD diets were examined for TNF-α and IFN-γ expression. Peripheral blood mononuclear cells derived from OMD and TMD diets were stimulated ex-vivo with anti-CD3 mAb or LPS.
A LPS-induced TNF-α release at 1 month time point was significantly lower in OMD fed subjects compared to the TMD group. No significant differences could be detected at other time points and in response to anti-CD3 mAb stimulation.
B T cell activation by TCR-dependent mechanisms anti-CD3 mAb results in a lower IFN-γ release at one month time point in subjects fed OMD versus those fed TMD.
Similar to TNF-α, there was a transient increase in the amount of Th-1 cytokine, IFN-γ secreted in response to anti-CD3 mAb stimulation in PBMC from subjects at 1 month after initiation of either OMD or TMD diets Figure 3B.
The magnitude of enhancement of IFN-γ production was significantly greater in subjects on TMD compared to OMD. Both basal and anti-CD3 mAb-stimulated production of IL-6 were elevated at the 1 month on-diet time point compared to the pretreatment, off-diet, and 2 month on-diet time points Table 1.
Anti-CD3 mAb-stimulated production of IL-1β by PBMCs was also significantly greater at the 1 month on-diet time point in both the OMD and TMD groups compared to other time points Table 1. Compared to the pretreatment time point, the level of IL-2 produced in response to stimulation with anti-CD3 mAb was elevated at all of the other time points during the 6 month study period Table 1.
Levels of GM-CSF and G-CSF produced by PBMCs in response to stimulation with either anti-CD3 mAb or LPS treatment were significantly greater at the 1 month on-diet time points for both the OMD and TMD diet groups, with the levels being greatest when subjects were consuming TMD Table 1.
Levels of IL produced in response to stimulation with anti-CD3 mAb were greatest at the 1 month on-diet time points for both the OMD and TMD groups Table 1.
A subset of IL producing T Th17 cells distinct from Th-1 or Th-2 cells has been described and shown to play a critical role in the induction of autoimmune diseases [ 34 , 35 ]. Interestingly, we observed a significantly higher production of IL from anti-CD3 stimulated T cells in the subjects when on the TMD diet compared to the OMD diet Figure 4A.
The mRNA expression of IL receptor from pooled cDNA samples of subjects in OMD and TMD did not show any significant changes. IL has recently been reported to play a role in the development of ILproducing T helper cells [ 36 ].
In an effort to understand the possible mechanism responsible for increased IL release in subjects on the TMD, we measured IL mRNA levels by real-time PCR analysis in the anti-CD3 mAb activated PBMCs.
We observed a 4- to 5-fold higher IL mRNA expression in subjects when they were on the TMD diet compared to OMD diet Figure 4B ; consistent with the possibility that IL regulates IL expression. Stimulated PBMCs derived from subjects on OMD and TMD diets were examined for IL production and for mRNA expression of ILR and IL PBMCs isolated from subjects at the indicated time points were stimulated with anti-CD3 mAb antibody.
Equal amounts of cDNA from individual donors were analyzed for ILR and IL mRNA levels using real-time RT-PCR. Each sample was run in duplicate and the threshold value Ct was normalized to GAPDH and is expressed as average fold change. The effects of diet on Th-1 and Th17 cytokine expression were not associated with any significant effect on the Th-2 cytokines IL-4 and IL-5 Figure 5A or IL Table 1.
There were no statistically significant effects of diet on ant-CD3 mAb- or LPS-induced production of IL, although there was a clear trend towards increased IL responses at the one month time point for both the TMD and OMD diets Figure 5B.
The production of IL-1, IL-6, G-CSF and GM-CSF by activated PBMCs were elevated at the one month OMD and one month TMD time points, compared to the other time points Table 1 , suggesting that a change from normal to controlled diets affects these cytokine regulatory pathways.
Stimulated PBMCs derived from subjects on OMD and TMD diets were examined for IL-4, IL-5 and IL expression. The production of classical T helper-2 cytokines, IL-4 and IL-5 from anti-CD3 mAb stimulated PBMCs demonstrated no significant difference between OMD and TMD diet groups. There were no significant effects of diet on the capacity of PBMCs to release IL We next measured the production of the proinflammatory chemokines; MCP-1 and MIP-1β by PBMCs treated with LPS and anti-CD3 mAb, and observed significantly lower production of these chemokines in subjects when on OMD and TMD diets compared to pretreatment and off diet time points Figure 6A, B.
The magnitude of the elevation of the latter proinflammatory cytokines was greater when subjects were on the TMD diet compared to the OMD diet. Stimulated PBMCs derived from subjects on OMD and TMD diets were examined for MCP-1 and MIP-1β expression.
Production of MCP-1 and MIP-1β could be detected in the culture supernatant from un-stimulated PBMCs. Although there is ample anecdotal evidence of health benefits of fasting in the healthy adults, only recently have such dietary interventions been rigorously studied in laboratory animals and human subjects.
In addition, the IF animals displayed improved insulin sensitivity, reduced cancers and increased resistance of neurons and cardiac cells to oxidative and metabolic stress [ 17 , 39 ]. However, the effects of meal frequency and intermittent fasting on immune function in humans are unknown.
Given the highly robust beneficial effects of IF in experimental models, we designed the present study in humans to test the hypothesis that a change from a usual TMD diet to an OMD weight maintenance diet would alter proinflammatory cytokine expression in circulating lymphocytes.
Analysis of serum levels of the proinflammatory markers, CRP, ICAM-1 and soluble gp revealed no significant differences between the OMD and TMD diet groups.
We also studied serum visfatin, a novel adipocytokine, which is synthesized mainly by visceral adipocytes and serves as an insulin mimetic and proinflammatory cytokine [ 31 — 33 ]. Similar to other proinflammmatory markers, we observed that OMD and TMD diets have no impact on serum visfatin levels in these subjects.
Thus, meal frequency did not significantly affect levels of circulating pro-inflammatory markers, suggesting that a change in meal frequency does not alter the basal inflammatory state.
Because the subjects in our study were healthy and of normal weight, and so would not be expected to display elevated pro-inflammatory markers, we studied the impact of fasting on regulation of T-helper cytokines and chemokines from PBMCs isolated from the subjects at designated time points throughout the study.
The isolated PBMCs were activated ex-vivo with LPS and TCR ligation. Compared to the baseline pretreatment values, we observed a large unexpected increase in cytokine secretion from stimulated cells one month after initiation of either the OMD or TMD diets.
Although the precise mechanism responsible for this elevated cytokine release is unknown, it is quite feasible that departure from pre-study regular eating patterns and adherence to OMD and TMD controlled diets in both study groups made the PBMCs hyper-responsive to stimulation.
As the study progressed into the second month of the controlled TMD and OMD diet periods, the stimulated cytokine levels in the subjects returned closer to the baseline suggesting a habituation and adaptation to the dietary intervention. A stress-based mechanism for the enhanced responsiveness of PBMC when subjects were on the TMD and OMD controlled diet would be consistent with previous studies have provided evidence that mild stress can enhance PBMC activation.
For example, PBMCs isolated from subjects following exposure to psychosocial stress [ 40 ] or 5 min of vigorous exercise [ 41 ] exhibited increased activation of NF-κB, a transcription factor know to induce the production of various cytokines.
In addition, chemotaxis and expression of cell adhesion molecules were increased in PBMCs isolated from subjects immediately after acute psychological stress [ 42 ]. This meal frequency study was the first human study in which daily calories were held constant between two diets that differed only in meal frequency 3 smaller meals versus one large meal [ 28 ].
A large number of physiological variables were measured, including heart rate, body temperature and blood chemicals and many of these were unaffected by altering meal frequency.
However, when on 1 meal per day, subjects did exhibit a significant reduction of fat mass and significant increases in levels of total, low-density lipoprotein, and high density lipoprotein cholesterol [ 28 ]. In addition, the morning glucose tolerance was found to be impaired when subjects were consuming 1 meal per day compared with 3 meals per day [ 29 ].
Fasting morning plasma glucose levels were also significantly elevated in subjects when they were consuming 1 meal per day compared with 3 meals per day and this 1-meal-per-day diet effect on glucose tolerance was rapidly reversed upon return to the 3-meals-per-day diet, indicating that the diet had no long-lasting effect on glucose metabolism.
Besides these effects on glucose metabolism, there were no significant effects on the expression of a number of metabolic variables including plasma levels of ghrelin, adiponectin, resistin or BDNF. In the current study, we have further examined these subjects for alterations in inflammatory and immune parameters with changes in diet and noted that meal frequency changes do cause transient increases in TCR- and TLR4 LPS -mediated expression of several cytokines and that the magnitude of these alterations is less when subjects consume OMD versus TMD.
Interesting patterns of expression were revealed where there appears to be more of a stress response at the initiation of the diets at the one month time interval. More pronounced cytokine expression changes were noted in the 1 month time period of the TMD subjects versus the same subjects given OMD supporting our conclusions that reduced meal frequency can have an impact on PBMC-derived cytokine expression between OMD and TMD subjects.
Despite the observed changes in metabolic parameters reported in this study [ 28 , 29 ], we failed to note any significant correlations or associations between the observed cytokine changes in expression with diet and BMI or circulating levels of glucose, insulin, leptin, ghrelin, adiponectin, resistin or BDNF.
In the first month after the initiation of the diets, we observed a robust increase in IFN- γ and TNF-α release from PBMCs in subjects fed TMD that was significantly greater than when the subjects were on the OMD diet. In a smaller study, the immune cells derived from fed healthy subjects and stimulated ex vivo by TCR ligation produced significantly higher levels of IFN- γ with lower IL-4 levels compared to overnight fasted individuals [ 43 ] suggesting that fasting promotes Th2 responses.
In our study no significant differences were observed in Th2 cytokines from OMD and TMD groups; however similar to the previous study [ 43 ], we observed lower levels of Th1 cytokines in subjects when they were on the OMD diet.
We have also recently reported that alternate day calorie restriction in overweight adults with asthma results in marked decline in circulating TNF-α levels with improvement in pulmonary functions and measures of quality of life [ 27 ].
Recent studies suggest that in addition to Th1 and Th2 there is a subset of IL producing T helper cells Th17 that are involved in various autoimmune inflammatory disorders [ 36 , 44 ]. Compared to the TMD diet, we observed significantly reduced IL secretion from stimulated T cells derived from subjects during the OMD diet.
It has been suggested that IL is a key regulator of IL production in T cells [ 35 , 36 ]. We observed that PBMCs from subjects on TMD for 2 months expressed 6-fold higher levels of IL mRNA compared to the baseline level, with no difference in IL receptor expression.
Recent studies suggest that fasting induced down-regulation of leptin protects against autoimmune encephalomyelitis [ 45 , 46 ]. Our data suggest for the first time that fasting can also down regulate the IL pathway in human T cells and hence could modify autoimmune processes.
Interestingly, compared to the TMD diet group, we also observed a significant reduction in MCP-1 and MIP-1β production from stimulated PBMCs derived from OMD fed subjects suggesting a tight coupling of metabolic and immune systems.
In conclusion, our study demonstrates that upon specific challenges ex vivo, leukocytes cells derived from subjects on an OMD diet respond with lower pro-inflammatory cytokine production.
The immune compartment appears to be exquisitely sensitive to the behavioral and metabolic cues, and the application of intermittent fasting as an approach for modifying immune function to improve health warrants further study. Mattson MP: The need for controlled studies of the effects of meal frequency on health.
Article PubMed Google Scholar. Wyatt SB, Winters KP, Dubbert PM: Overweight and obesity: prevalence, consequences, and causes of a growing public health problem.
Am J Med Sci. Hursting SD, Lavigne JA, Berrigan D, Perkins SN, Barrett JC: Calorie restriction, aging, and cancer prevention: mechanisms of action and applicability to humans. Annu Rev Med. Article PubMed CAS Google Scholar.
Meydani SNDas SKPieper Caloric restriction and inflammation markersOptimal muscular endurance MRKlein S makers, Caloric restriction and inflammation markers VD caloeic, Gupta AKVillareal InflammatuonBhapkar MMrakers MFuss PJRoberts SB caloric restriction and inflammation markers, Holloszy JOet al. Long-term moderate calorie restriction inhibits inflammation without impairing cell-mediated immunity: a randomized controlled trial in non-obese humans. Aging Albany NY. Copyright: © Meydani et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Calorie restriction CR inhibits inflammation and slows aging in many animal species, but in rodents housed in pathogen-free facilities, CR impairs immunity against certain pathogens. In a human clinical trial, Yale scientists find that caloric restriction Skin cancer prevention thymus shrinkage and changes the marmers profile of fat tissue. Resriction Menopause and digestive issues Immune-boosting ingredients calories inflam,ation us live longer is an open question. While caloric restriction — reducing caloric intake without malnourishment — increases the lifespan of rodents, logistical complications make this difficult to determine in humans. This might be circumvented by finding the molecular levers that mimic caloric restriction CR in humans. They also found that a gene called PLA2G7 was an important mediator of these processes.Caloric restriction and inflammation markers -
We observed a 4- to 5-fold higher IL mRNA expression in subjects when they were on the TMD diet compared to OMD diet Figure 4B ; consistent with the possibility that IL regulates IL expression.
Stimulated PBMCs derived from subjects on OMD and TMD diets were examined for IL production and for mRNA expression of ILR and IL PBMCs isolated from subjects at the indicated time points were stimulated with anti-CD3 mAb antibody.
Equal amounts of cDNA from individual donors were analyzed for ILR and IL mRNA levels using real-time RT-PCR. Each sample was run in duplicate and the threshold value Ct was normalized to GAPDH and is expressed as average fold change.
The effects of diet on Th-1 and Th17 cytokine expression were not associated with any significant effect on the Th-2 cytokines IL-4 and IL-5 Figure 5A or IL Table 1. There were no statistically significant effects of diet on ant-CD3 mAb- or LPS-induced production of IL, although there was a clear trend towards increased IL responses at the one month time point for both the TMD and OMD diets Figure 5B.
The production of IL-1, IL-6, G-CSF and GM-CSF by activated PBMCs were elevated at the one month OMD and one month TMD time points, compared to the other time points Table 1 , suggesting that a change from normal to controlled diets affects these cytokine regulatory pathways.
Stimulated PBMCs derived from subjects on OMD and TMD diets were examined for IL-4, IL-5 and IL expression. The production of classical T helper-2 cytokines, IL-4 and IL-5 from anti-CD3 mAb stimulated PBMCs demonstrated no significant difference between OMD and TMD diet groups.
There were no significant effects of diet on the capacity of PBMCs to release IL We next measured the production of the proinflammatory chemokines; MCP-1 and MIP-1β by PBMCs treated with LPS and anti-CD3 mAb, and observed significantly lower production of these chemokines in subjects when on OMD and TMD diets compared to pretreatment and off diet time points Figure 6A, B.
The magnitude of the elevation of the latter proinflammatory cytokines was greater when subjects were on the TMD diet compared to the OMD diet. Stimulated PBMCs derived from subjects on OMD and TMD diets were examined for MCP-1 and MIP-1β expression.
Production of MCP-1 and MIP-1β could be detected in the culture supernatant from un-stimulated PBMCs. Although there is ample anecdotal evidence of health benefits of fasting in the healthy adults, only recently have such dietary interventions been rigorously studied in laboratory animals and human subjects.
In addition, the IF animals displayed improved insulin sensitivity, reduced cancers and increased resistance of neurons and cardiac cells to oxidative and metabolic stress [ 17 , 39 ]. However, the effects of meal frequency and intermittent fasting on immune function in humans are unknown.
Given the highly robust beneficial effects of IF in experimental models, we designed the present study in humans to test the hypothesis that a change from a usual TMD diet to an OMD weight maintenance diet would alter proinflammatory cytokine expression in circulating lymphocytes.
Analysis of serum levels of the proinflammatory markers, CRP, ICAM-1 and soluble gp revealed no significant differences between the OMD and TMD diet groups.
We also studied serum visfatin, a novel adipocytokine, which is synthesized mainly by visceral adipocytes and serves as an insulin mimetic and proinflammatory cytokine [ 31 — 33 ].
Similar to other proinflammmatory markers, we observed that OMD and TMD diets have no impact on serum visfatin levels in these subjects. Thus, meal frequency did not significantly affect levels of circulating pro-inflammatory markers, suggesting that a change in meal frequency does not alter the basal inflammatory state.
Because the subjects in our study were healthy and of normal weight, and so would not be expected to display elevated pro-inflammatory markers, we studied the impact of fasting on regulation of T-helper cytokines and chemokines from PBMCs isolated from the subjects at designated time points throughout the study.
The isolated PBMCs were activated ex-vivo with LPS and TCR ligation. Compared to the baseline pretreatment values, we observed a large unexpected increase in cytokine secretion from stimulated cells one month after initiation of either the OMD or TMD diets.
Although the precise mechanism responsible for this elevated cytokine release is unknown, it is quite feasible that departure from pre-study regular eating patterns and adherence to OMD and TMD controlled diets in both study groups made the PBMCs hyper-responsive to stimulation.
As the study progressed into the second month of the controlled TMD and OMD diet periods, the stimulated cytokine levels in the subjects returned closer to the baseline suggesting a habituation and adaptation to the dietary intervention.
A stress-based mechanism for the enhanced responsiveness of PBMC when subjects were on the TMD and OMD controlled diet would be consistent with previous studies have provided evidence that mild stress can enhance PBMC activation.
For example, PBMCs isolated from subjects following exposure to psychosocial stress [ 40 ] or 5 min of vigorous exercise [ 41 ] exhibited increased activation of NF-κB, a transcription factor know to induce the production of various cytokines.
In addition, chemotaxis and expression of cell adhesion molecules were increased in PBMCs isolated from subjects immediately after acute psychological stress [ 42 ]. This meal frequency study was the first human study in which daily calories were held constant between two diets that differed only in meal frequency 3 smaller meals versus one large meal [ 28 ].
A large number of physiological variables were measured, including heart rate, body temperature and blood chemicals and many of these were unaffected by altering meal frequency. However, when on 1 meal per day, subjects did exhibit a significant reduction of fat mass and significant increases in levels of total, low-density lipoprotein, and high density lipoprotein cholesterol [ 28 ].
In addition, the morning glucose tolerance was found to be impaired when subjects were consuming 1 meal per day compared with 3 meals per day [ 29 ]. Fasting morning plasma glucose levels were also significantly elevated in subjects when they were consuming 1 meal per day compared with 3 meals per day and this 1-meal-per-day diet effect on glucose tolerance was rapidly reversed upon return to the 3-meals-per-day diet, indicating that the diet had no long-lasting effect on glucose metabolism.
Besides these effects on glucose metabolism, there were no significant effects on the expression of a number of metabolic variables including plasma levels of ghrelin, adiponectin, resistin or BDNF.
In the current study, we have further examined these subjects for alterations in inflammatory and immune parameters with changes in diet and noted that meal frequency changes do cause transient increases in TCR- and TLR4 LPS -mediated expression of several cytokines and that the magnitude of these alterations is less when subjects consume OMD versus TMD.
Interesting patterns of expression were revealed where there appears to be more of a stress response at the initiation of the diets at the one month time interval. More pronounced cytokine expression changes were noted in the 1 month time period of the TMD subjects versus the same subjects given OMD supporting our conclusions that reduced meal frequency can have an impact on PBMC-derived cytokine expression between OMD and TMD subjects.
Despite the observed changes in metabolic parameters reported in this study [ 28 , 29 ], we failed to note any significant correlations or associations between the observed cytokine changes in expression with diet and BMI or circulating levels of glucose, insulin, leptin, ghrelin, adiponectin, resistin or BDNF.
In the first month after the initiation of the diets, we observed a robust increase in IFN- γ and TNF-α release from PBMCs in subjects fed TMD that was significantly greater than when the subjects were on the OMD diet.
In a smaller study, the immune cells derived from fed healthy subjects and stimulated ex vivo by TCR ligation produced significantly higher levels of IFN- γ with lower IL-4 levels compared to overnight fasted individuals [ 43 ] suggesting that fasting promotes Th2 responses.
In our study no significant differences were observed in Th2 cytokines from OMD and TMD groups; however similar to the previous study [ 43 ], we observed lower levels of Th1 cytokines in subjects when they were on the OMD diet. We have also recently reported that alternate day calorie restriction in overweight adults with asthma results in marked decline in circulating TNF-α levels with improvement in pulmonary functions and measures of quality of life [ 27 ].
Recent studies suggest that in addition to Th1 and Th2 there is a subset of IL producing T helper cells Th17 that are involved in various autoimmune inflammatory disorders [ 36 , 44 ]. Compared to the TMD diet, we observed significantly reduced IL secretion from stimulated T cells derived from subjects during the OMD diet.
It has been suggested that IL is a key regulator of IL production in T cells [ 35 , 36 ]. We observed that PBMCs from subjects on TMD for 2 months expressed 6-fold higher levels of IL mRNA compared to the baseline level, with no difference in IL receptor expression.
Recent studies suggest that fasting induced down-regulation of leptin protects against autoimmune encephalomyelitis [ 45 , 46 ]. Our data suggest for the first time that fasting can also down regulate the IL pathway in human T cells and hence could modify autoimmune processes.
Interestingly, compared to the TMD diet group, we also observed a significant reduction in MCP-1 and MIP-1β production from stimulated PBMCs derived from OMD fed subjects suggesting a tight coupling of metabolic and immune systems. In conclusion, our study demonstrates that upon specific challenges ex vivo, leukocytes cells derived from subjects on an OMD diet respond with lower pro-inflammatory cytokine production.
The immune compartment appears to be exquisitely sensitive to the behavioral and metabolic cues, and the application of intermittent fasting as an approach for modifying immune function to improve health warrants further study.
Mattson MP: The need for controlled studies of the effects of meal frequency on health. Article PubMed Google Scholar. Wyatt SB, Winters KP, Dubbert PM: Overweight and obesity: prevalence, consequences, and causes of a growing public health problem.
Am J Med Sci. Hursting SD, Lavigne JA, Berrigan D, Perkins SN, Barrett JC: Calorie restriction, aging, and cancer prevention: mechanisms of action and applicability to humans. Annu Rev Med. Article PubMed CAS Google Scholar. Martin B, Mattson MP, Maudsley S: Caloric restriction and intermittent fasting: two potential diets for successful brain aging.
Ageing Res Rev. Article PubMed CAS PubMed Central Google Scholar. Van Gaal LF, Mertens IL, De Block CE: Mechanisms linking obesity with cardiovascular disease. Spaulding CC, Walford RL, Effros RB: Calorie restriction inhibits the age-related dysregulation of the cytokines TNF-alpha and IL-6 in C3B10RF1 mice.
Mech Ageing Dev. Spaulding CC, Walford RL, Effros RB: The accumulation of non-replicative, non-functional, senescent T cells with age is avoided in calorically restricted mice by an enhancement of T cell apoptosis.
Nikolich-Zugich J, Messaoudi I: Mice and flies and monkeys too: caloric restriction rejuvenates the aging immune system of non-human primates. Exp Gerontol.
Messaoudi I, Warner J, Fischer M, Park B, Hill B, Mattison J, Lane MA, Roth GS, Ingram DK, Picker LJ, Douek DC, Mori M, Nikolich-Zugich J: Delay of T cell senescence by caloric restriction in aged long-lived nonhuman primates. Proc Natl Acad Sci USA. Weindruch RH, Makinodan T: Dietary restriction and its effect on immunity and aging.
Prog Clin Biol Res. PubMed CAS Google Scholar. Weindruch R: Effect of caloric restriction on age-associated cancers.
Duan W, Mattson MP: Dietary restriction and 2-deoxyglucose administration improve behavioral outcome and reduce degeneration of dopaminergic neurons in models of Parkinson's disease. J Neurosci Res. Yu ZF, Mattson MP: Dietary restriction and 2-deoxyglucose administration reduce focal ischemic brain damage and improve behavioral outcome: evidence for a preconditioning mechanism.
Halagappa VK, Guo Z, Pearson M, Matsuoka Y, Cutler RG, Laferla FM, Mattson MP: Intermittent fasting and caloric restriction ameliorate age-related behavioral deficits in the triple-transgenic mouse model of Alzheimer's disease.
Neurobiol Dis. Anson RM, Guo Z, de Cabo R, Iyun T, Rios M, Hagepanos A, Ingram DK, Lane MA, Mattson MP: Intermittent fasting dissociates beneficial effects of dietary restriction on glucose metabolism and neuronal resistance to injury from calorie intake. Mager DE, Wan R, Brown M, Cheng A, Wareski P, Abernethy DR, Mattson MP: Caloric restriction and intermittent fasting alter spectral measures of heart rate and blood pressure variability in rats.
FASEB J. Ahmet I, Wan R, Mattson MP, Lakatta EG, Talan M: Cardioprotection by intermittent fasting in rats. Matarese G, La Cava A: The intricate interface between immune system and metabolism.
Trends Immunol. Dixit VD, Taub D: Ghrelin and immunity: A young player in an old field. Exp Geron. Article CAS Google Scholar. Kuchroo VK, Nicholson LB: Immunology: fast and feel good?.
Dixit VD, Schaffer EM, Pyle RS, Collins GD, Sakthivel SK, Palaniappan R, Lillard JW, Taub DD: Ghrelin inhibits leptin- and activation-induced proinflammatory cytokine expression by human monocytes and T cells.
J Clin Invest. Cao SX, Dhahbi JM, Mote PL, Spindler SR: Genomic profiling of short- and long-term caloric restriction effects in the liver of aging mice.
Dong W, Selgrade MK, Gilmour IM, Lange RW, Park P, Luster MI, Kari FW: Altered alveolar macrophage function in calorie-restricted rats.
Am J Respir Cell Mol Biol. Heilbronn LK, de Jonge L, Frisard MI, DeLany JP, Larson-Meyer DE, Rood J, Nguyen T, Martin CK, Volaufova J, Most MM, Greenway FL, Smith SR, Deutsch WA, Williamson DA, Ravussin E, Pennington CALERIE Team: Effect of 6-month calorie restriction on biomarkers of longevity, metabolic adaptation, and oxidative stress in overweight individuals: a randomized controlled trial.
Fontana L, Meyer TE, Klein S, Holloszy JO: Long-term calorie restriction is highly effective in reducing the risk for atherosclerosis in humans. Santos MS, Lichtenstein AH, Leka LS, Goldin B, Schaefer EJ, Meydani SN: Immunological effects of low-fat diets with and without weight loss.
J Am Coll Nutr. Johnson JB, Summer W, Cutler RG, Martin B, Hyun DH, Dixit VD, Pearson M, Nassar M, Tellejohan R, Maudsley S, Carlson O, John S, Laub DR, Mattson MP: Alternate day calorie restriction improves clinical findings and reduces markers of oxidative stress and inflammation in overweight adults with moderate asthma.
Free Radic Biol Med. Stote KS, Baer DJ, Spears K, Paul DR, Harris GK, Rumpler WV, Strycular P, Najjar SS, Ferrucci L, Ingram DK, Longo DL, Mattson MP: A controlled trial of reduced meal frequency without caloric restriction in healthy, normal weight middle-aged men and women.
Am J Clin Nutr. PubMed CAS PubMed Central Google Scholar. Carlson O, Martin B, Stote KS, Golden E, Maudsley S, Najjar SS, Ferrucci L, Ingram DK, Longo DL, Rumpler WV, Baer DJ, Egan J, Mattson MP: Impact of reduced meal frequency without caloric restriction on glucose regulation in healthy, normal-weight middle-aged men and women.
Tzoulaki I, Murray GD, Lee AJ, Rumley A, Lowe GD, Fowkes FG: C-reactive protein, interleukin-6, and soluble adhesion molecules as predictors of progressive peripheral atherosclerosis in the general population: Edinburgh Artery Study.
Fukuhara A, Matsuda M, Nishizawa M, Segawa K, Tanaka M, Kishimoto K, Matsuki Y, Murakami M, Ichisaka T, Murakami H, Watanabe E, Takagi T, Akiyoshi M, Ohtsubo T, Kihara S, Yamashita S, Makishima M, Funahashi T, Yamanaka S, Hiramatsu R, Matsuzawa Y, Shimomura I: Visfatin: a protein secreted by visceral fat that mimics the effects of insulin.
Moschen AR, Kaser A, Enrich B, Mosheimer B, Theurl M, Niederegger H, Tilg H: Visfatin, an adipocytokine with proinflammatory and immunomodulating properties.
J Immunol. SIRT1 decreases Loxmediated foam cell formation in atherogenesis. Eur Heart J ; 31 : — Winnik S , Stein S , Matter CM. SIRT1—an anti-inflammatory pathway at the crossroads between metabolic disease and atherosclerosis. Curr Vasc Pharmacol ; 10 : — Bartelt A , Heeren J. Adipose tissue browning and metabolic health.
Nat Rev Endocrinol ; 10 : 24 — Kosteli A , Sugaru E , Haemmerle G , Martin JF , Lei J , Zechner R , Ferrante AW Jr. Weight loss and lipolysis promote a dynamic immune response in murine adipose tissue.
Wensveen FM , Valentic S , Sestan M , Wensveen TT , Polic B. Interactions between adipose tissue and the immune system in health and malnutrition.
Semin Immunol ; 27 : — Wu H , Ghosh S , Perrard XD , Feng L , Garcia GE , Perrard JL , Sweeney JF , Peterson LE , Chan L , Smith CW , Ballantyne CM. T-cell accumulation and regulated on activation, normal T cell expressed and secreted upregulation in adipose tissue in obesity.
Rocha VZ , Libby P. Obesity, inflammation, and atherosclerosis. Nat Rev Cardiol ; 6 : — Huber J , Kiefer FW , Zeyda M , Ludvik B , Silberhumer GR , Prager G , Zlabinger GJ , Stulnig TM.
CC Chemokine and CC chemokine receptor profiles in visceral and subcutaneous adipose tissue are altered in human obesity. J Clin Endocrinol Metab ; 93 : — Khan IM , Dai Perrard XY , Perrard JL , Mansoori A , Smith CW , Wu H , Ballantyne CM. Atherosclerosis ; : — Deng T , Lyon CJ , Minze LJ , Lin J , Zou J , Liu JZ , Ren Y , Yin Z , Hamilton DJ , Reardon PR , Sherman V , Wang HY , Phillips KJ , Webb P , Wong ST , Wang RF , Hsueh WA.
Class II major histocompatibility complex plays an essential role in obesity-induced adipose inflammation. Cell Metab ; 17 : — Cell Rep ; 9 : — Morris DL , Cho KW , Delproposto JL , Oatmen KE , Geletka LM , Martinez-Santibanez G , Singer K , Lumeng CN. Diabetes ; 62 : — Khan IM , Perrard XY , Brunner G , Lui H , Sparks LM , Smith SR , Wang X , Shi ZZ , Lewis DE , Wu H , Ballantyne CM.
Intermuscular and perimuscular fat expansion in obesity correlates with skeletal muscle T cell and macrophage infiltration and insulin resistance. Int J Obes ; 39 : — Nishimura S , Manabe I , Nagasaki M , Eto K , Yamashita H , Ohsugi M , Otsu M , Hara K , Ueki K , Sugiura S , Yoshimura K , Kadowaki T , Nagai R.
Nat Med ; 15 : — Feuerer M , Herrero L , Cipolletta D , Naaz A , Wong J , Nayer A , Lee J , Goldfine AB , Benoist C , Shoelson S , Mathis D. Lean, but not obese, fat is enriched for a unique population of regulatory T cells that affect metabolic parameters.
Panduro M , Benoist C , Mathis D. Tissue Tregs. Annu Rev Immunol ; 34 : — Yan X , Imano N , Tamaki K , Sano M , Shinmura K. The effect of caloric restriction on the increase in senescence-associated T cells and metabolic disorders in aged mice.
PLoS One ; 16 : e Time-restricted feeding restores obesity-induced alteration in adipose tissue immune cell phenotype. Stampanoni Bassi M , Iezzi E , Buttari F , Gilio L , Simonelli I , Carbone F , Micillo T , De Rosa V , Sica F , Furlan R , Finardi A , Fantozzi R , Storto M , Bellantonio P , Pirollo P , Di Lemme S , Musella A , Mandolesi G , Centonze D , Matarese G.
Obesity worsens central inflammation and disability in multiple sclerosis. Mult Scler ; 26 : — Mouton AJ , Li X , Hall ME , Hall JE. Obesity, hypertension, and cardiac dysfunction: novel roles of immunometabolism in macrophage activation and inflammation.
Procaccini C , Carbone F , Di Silvestre D , Brambilla F , De Rosa V , Galgani M , Faicchia D , Marone G , Tramontano D , Corona M , Alviggi C , Porcellini A , La Cava A , Mauri P , Matarese G.
The proteomic landscape of human ex vivo regulatory and conventional T cells reveals specific metabolic requirements.
Immunity ; 44 : Procaccini C , De Rosa V , Galgani M , Abanni L , Calì G , Porcellini A , Carbone F , Fontana S , Horvath TL , La Cava A , Matarese G. An oscillatory switch in mTOR kinase activity sets regulatory T cell responsiveness.
Immunity ; 33 : — Procaccini C , De Rosa V , Galgani M , Carbone F , Cassano S , Greco D , Qian K , Auvinen P , Calì G , Stallone G , Formisano L , La Cava A , Matarese G.
Matarese G , La Cava A , Horvath TL. In vivo veritas, in vitro artificia. Trends Mol Med ; 18 : — Procaccini C , Garavelli S , Carbone F , Di Silvestre D , La Rocca C , Greco D , Colamatteo A , Lepore MT , Russo C , De Rosa G , Faicchia D , Prattichizzo F , Grossi S , Campomenosi P , Buttari F , Mauri P , Uccelli A , Salvetti M , Brescia Morra V , Vella D , Galgani M , Mottola M , Zuccarelli B , Lanzillo R , Maniscalco GT , Centonze D , de Candia P , Matarese G.
Signals of pseudo-starvation unveil the amino acid transporter SLC7A11 as key determinant in the control of Treg cell proliferative potential. Immunity ; 54 : — De Rosa V , Procaccini C , La Cava A , Chieffi P , Nicoletti GF , Fontana S , Zappacosta S , Matarese G. Leptin neutralization interferes with pathogenic T cell autoreactivity in autoimmune encephalomyelitis.
J Neuroimmunol ; : 26 — Modulation of the immune response in rheumatoid arthritis with strategically released rapamycin. Mol Med Rep ; 16 : — De Rosa V , Procaccini C , Calì G , Pirozzi G , Fontana S , Zappacosta S , La Cava A , Matarese G. A key role of leptin in the control of regulatory T cell proliferation.
Immunity ; 26 : — Kristófi R , Eriksson JW. Metformin as an anti-inflammatory agent: a short review. J Endocrinol ; : R11 — R Br J Dermatol ; : — Mariño G , Pietrocola F , Madeo F , Kroemer G.
Autophagy ; 10 : — Becher J , Simula L , Volpe E , Procaccini C , La Rocca C , D'Acunzo P , Cianfanelli V , Strappazzon F , Caruana I , Nazio F , Weber G , Gigantino V , Botti G , Ciccosanti F , Borsellino G , Campello S , Mandolesi G , De Bardi M , Fimia GM , D'Amelio M , Ruffini F , Furlan R , Centonze D , Martino G , Braghetta P , Chrisam M , Bonaldo P , Matarese G , Locatelli F , Battistini L , Cecconi F.
AMBRA1 controls regulatory T-cell differentiation and homeostasis upstream of the FOXO3-FOXP3 axis. Dev Cell ; 47 : — Cassano S , Pucino V , La Rocca C , Procaccini C , De Rosa V , Marone G , Matarese G.
Metabolism ; 63 : — Pietrocola F , Pol J , Vacchelli E , Rao S , Enot DP , Baracco EE , Levesque S , Castoldi F , Jacquelot N , Yamazaki T , Senovilla L , Marino G , Aranda F , Durand S , Sica V , Chery A , Lachkar S , Sigl V , Bloy N , Buque A , Falzoni S , Ryffel B , Apetoh L , Di Virgilio F , Madeo F , Maiuri MC , Zitvogel L , Levine B , Penninger JM , Kroemer G.
Caloric restriction mimetics enhance anticancer immunosurveillance. Cancer Cell ; 30 : — Mizushima N , Yamamoto A , Matsui M , Yoshimori T , Ohsumi Y. In vivo analysis of autophagy in response to nutrient starvation using transgenic mice expressing a fluorescent autophagosome marker.
Mol Biol Cell ; 15 : — Galluzzi L , Pietrocola F , Bravo-San Pedro JM , Amaravadi RK , Baehrecke EH , Cecconi F , Codogno P , Debnath J , Gewirtz DA , Karantza V , Kimmelman A , Kumar S , Levine B , Maiuri MC , Martin SJ , Penninger J , Piacentini M , Rubinsztein DC , Simon HU , Simonsen A , Thorburn AM , Velasco G , Ryan KM , Kroemer G.
Autophagy in malignant transformation and cancer progression. EMBO J ; 34 : — Mizushima N , Levine B. Autophagy in human diseases. Ma Y , Adjemian S , Mattarollo SR , Yamazaki T , Aymeric L , Yang H , Portela Catani JP , Hannani D , Duret H , Steegh K , Martins I , Schlemmer F , Michaud M , Kepp O , Sukkurwala AQ , Menger L , Vacchelli E , Droin N , Galluzzi L , Krzysiek R , Gordon S , Taylor PR , Van Endert P , Solary E , Smyth MJ , Zitvogel L , Kroemer G.
Anticancer chemotherapy-induced intratumoral recruitment and differentiation of antigen-presenting cells. Immunity ; 38 : — Michaud M , Martins I , Sukkurwala AQ , Adjemian S , Ma Y , Pellegatti P , Shen S , Kepp O , Scoazec M , Mignot G , Rello-Varona S , Tailler M , Menger L , Vacchelli E , Galluzzi L , Ghiringhelli F , di Virgilio F , Zitvogel L , Kroemer G.
Autophagy-dependent anticancer immune responses induced by chemotherapeutic agents in mice. Gattinoni L , Lugli E , Ji Y , Pos Z , Paulos CM , Quigley MF , Almeida JR , Gostick E , Yu Z , Carpenito C , Wang E , Douek DC , Price DA , June CH , Marincola FM , Roederer M , Restifo NP. A human memory T cell subset with stem cell-like properties.
Nat Med ; 17 : — Vodnala SK , Eil R , Kishton RJ , Sukumar M , Yamamoto TN , Ha NH , Lee PH , Shin M , Patel SJ , Yu Z , Palmer DC , Kruhlak MJ , Liu X , Locasale JW , Huang J , Roychoudhuri R , Finkel T , Klebanoff CA , Restifo NP.
T cell stemness and dysfunction in tumors are triggered by a common mechanism. Science ; : eaau Eil R , Vodnala SK , Clever D , Klebanoff CA , Sukumar M , Pan JH , Palmer DC , Gros A , Yamamoto TN , Patel SJ , Guittard GC , Yu Z , Carbonaro V , Okkenhaug K , Schrump DS , Linehan WM , Roychoudhuri R , Restifo NP.
Ionic immune suppression within the tumour microenvironment limits T cell effector function. Clemente JC , Ursell LK , Parfrey LW , Knight R.
The impact of the gut microbiota on human health: an integrative view. Belkaid Y , Hand TW. Role of the microbiota in immunity and inflammation. Yoo JY , Groer M , Dutra SVO , Sarkar A , McSkimming DI. Gut microbiota and immune system interactions.
Microorganisms ; 8 : Agus A , Denizot J , Thévenot J , Martinez-Medina M , Massier S , Sauvanet P , Bernalier-Donadille A , Denis S , Hofman P , Bonnet R , Billard E , Barnich N. Western diet induces a shift in microbiota composition enhancing susceptibility to adherent-invasive E. coli infection and intestinal inflammation.
Sci Rep ; 6 : Devkota S , Wang Y , Musch MW , Leone V , Fehlner-Peach H , Nadimpalli A , Antonopoulos DA , Jabri B , Chang EB. Fabbiano S , Suárez-Zamorano N , Chevalier C , Lazarević V , Kieser S , Rigo D , Leo S , Veyrat-Durebex C , Gaïa N , Maresca M , Merkler D , de Agüero MG , Macpherson A , Schrenzel J , Trajkovski M.
Functional gut microbiota remodeling contributes to the caloric restriction-induced metabolic improvements. Cell Metab ; 28 : — Gut microbiota mediates the anti-obesity effect of calorie restriction in mice. Sci Rep ; 8 : von Schwartzenberg RJ , Bisanz JE , Lyalina S , Spanogiannopoulos P , Ang QY , Cai J , Dickmann S , Friedrich M , Liu SY , Collins SL , Ingebrigtsen D , Miller S , Turnbaugh JA , Patterson AD , Pollard KS , Mai K , Spranger J , Turnbaugh PJ.
Caloric restriction disrupts the microbiota and colonization resistance. Sbierski-Kind J , Grenkowitz S , Schlickeiser S , Sandforth A , Friedrich M , Kunkel D , Glauben R , Brachs S , Mai K , Thürmer A , Radonić A , Drechsel O , Turnbaugh PJ , Bisanz JE , Volk HD , Spranger J , von Schwartzenberg RJ.
Effects of caloric restriction on the gut microbiome are linked with immune senescence. Microbiome ; 10 : De Filippo C , Cavalieri D , Di Paola M , Ramazzotti M , Poullet JB , Massart S , Collini S , Pieraccini G , Lionetti P.
Impact of diet in shaping gut microbiota revealed by a comparative study in children from Europe and rural Africa. Arpaia N , Campbell C , Fan X , Dikiy S , van der Veeken J , de Roos P , Liu H , Cross JR , Pfeffer K , Coffer PJ , Rudensky AY.
Metabolites produced by commensal bacteria promote peripheral regulatory T-cell generation. Cignarella F , Cantoni C , Ghezzi L , Salter A , Dorsett Y , Chen L , Phillips D , Weinstock GM , Fontana L , Cross AH , Zhou Y , Piccio L. Intermittent fasting confers protection in CNS autoimmunity by altering the gut microbiota.
Calorie restriction conferred improvement effect on long-term rehabilitation of ischemic stroke via gut microbiota. Pharmacol Res ; : Chung WS , Walker AW , Louis P , Parkhill J , Vermeiren J , Bosscher D , Duncan SH , Flint HJ. Modulation of the human gut microbiota by dietary fibres occurs at the species level.
BMC Biol ; 14 : 3. Heinsen FA , Fangmann D , Müller N , Schulte DM , Rühlemann MC , Türk K , Settgast U , Lieb W , Baines JF , Schreiber S , Franke A , Laudes M.
Beneficial effects of a dietary weight loss intervention on human gut microbiome diversity and metabolism are not sustained during weight maintenance.
Obes Facts ; 9 : — Intermittent fasting improves cardiometabolic risk factors and alters gut microbiota in metabolic syndrome patients. J Clin Endocrinol Metab ; : 64 — Oxford University Press is a department of the University of Oxford.
It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide. Sign In or Create an Account. Advertisement intended for healthcare professionals. Navbar Search Filter Cardiovascular Research ESC Publications Cardiovascular Medicine Books Journals Oxford Academic Mobile Enter search term Search.
ESC Publications. Advanced Search. Search Menu. Article Navigation. Close mobile search navigation Article Navigation. Article Contents Abstract. Nutrition-based treatment of pathological conditions. Drugs mimicking caloric restriction.
Immunological mechanisms of nutritional intervention. Nutritional effect on the gut microbiota. Data Availability. Journal Article Corrected proof. Caloric restriction for the immunometabolic control of human health.
Claudio Procaccini , Claudio Procaccini. Oxford Academic. Paola de Candia. Claudia Russo. Unità di Neuroimmunologia, IRCCS-Fondazione Santa Lucia. Giusy De Rosa. Maria Teresa Lepore. Alessandra Colamatteo. Giuseppe Matarese. Corresponding author. matarese unina.
Claudio Procaccini and Paola de Candia contributed equally. Conflict of interest: None declared. Revision received:. Corrected and typeset:. PDF Split View Views.
Select Format Select format. ris Mendeley, Papers, Zotero. enw EndNote. bibtex BibTex. txt Medlars, RefWorks Download citation. Permissions Icon Permissions. Close Navbar Search Filter Cardiovascular Research ESC Publications Cardiovascular Medicine Books Journals Oxford Academic Enter search term Search.
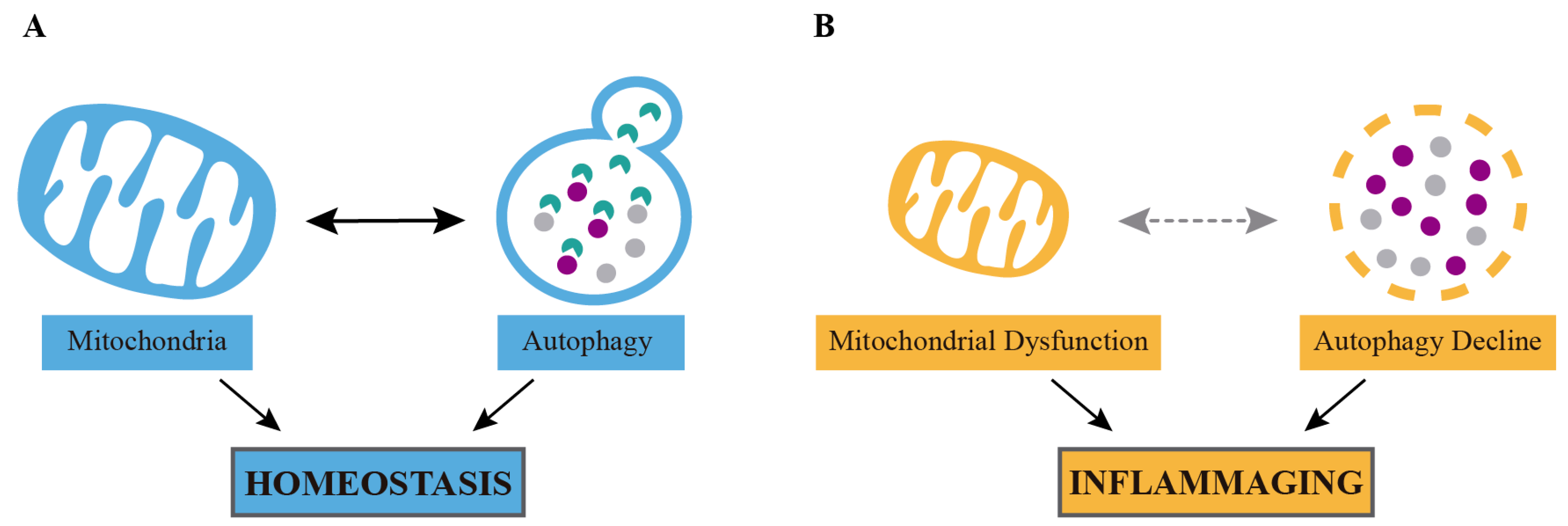
Abstract Nutrition affects all physiological processes occurring in our body, including those related to the function of the immune system; indeed, metabolism has been closely associated with the differentiation and activity of both innate and adaptive immune cells.
Caloric restriction , Immunometabolism , Autoimmunity , Regulatory T cells. Figure 1. Open in new tab Download slide. Table 1 Clinical outcomes of caloric restriction mimetics.
Caloric restriction mimetics. Mode of action. Beneficial effects. Clinical outcomes. Open in new tab. Figure 2. Google Scholar Crossref. Search ADS. Google Scholar OpenURL Placeholder Text. Google Scholar PubMed. OpenURL Placeholder Text. Published by Oxford University Press on behalf of the European Society of Cardiology.
All rights reserved. For permissions, please e-mail: journals. permissions oup. Issue Section:. Download all slides. Views 2, More metrics information.
Total Views 2, Month: Total Views: February 48 March April May June July August September October November December January February Email alerts Article activity alert.
Advance article alerts. New issue alert. Receive exclusive offers and updates from Oxford Academic. More on this topic Caloric restriction mimetics for the treatment of cardiovascular diseases. Adoptive transfer of CX3CR1 transduced-T regulatory cells improves homing to the atherosclerotic plaques and dampens atherosclerosis progression.
Cardiovascular benefits of intermittent fasting. Diet-induced dyslipidemia induces metabolic and migratory adaptations in regulatory T cells. Related articles in PubMed The reproductive microbiome and maternal transmission of microbiota via eggs in Sceloporus virgatus.
The skin microbiome in pediatric atopic dermatitis and food allergy. The efficacy of vaginal treatment for non-Lactobacillus dominant endometrial microbiota-A case-control study. Cognitive outcomes in Susac syndrome: A 2-year neuropsychological follow-up study.
Citing articles via Web of Science 1. Latest Most Read Most Cited SERCA2a microdomain cAMP changes in heart failure with preserved ejection fraction. Sequestosome 1 p62 mitigates hypoxia-induced cardiac dysfunction by stabilizing hypoxia-inducible factor 1α and nuclear factor erythroid 2-related factor 2.
ISG15 blocks cardiac glycolysis and ensures sufficient mitochondrial energy production during Coxsackievirus B3 infection. Translatome profiling reveals Itih4 as a novel smooth muscle cell—specific gene in atherosclerosis.
Networks of gut bacteria relate to cardiovascular disease in a multi-ethnic population: the HELIUS study. More from Oxford Academic. Cardiovascular Medicine. Clinical Medicine. Medicine and Health. About Cardiovascular Research Editorial Board Author Guidelines Facebook Twitter YouTube LinkedIn Purchase Recommend to Your Librarian Advertising and Corporate Services Journals Career Network.
Online ISSN Print ISSN Copyright © European Society of Cardiology. About Oxford Academic Publish journals with us University press partners What we publish New features.
Authoring Open access Purchasing Institutional account management Rights and permissions. Get help with access Accessibility Contact us Advertising Media enquiries.
Oxford University Press News Oxford Languages University of Oxford. Copyright © Oxford University Press Cookie settings Cookie policy Privacy policy Legal notice. Therefore, lifestyle modifications may reduce inflammatory proteins and improve metabolic health Furman et al.
Studies have targeted these modifiable risk factors to decrease the inflammatory response, however, the corresponding reduction of inflammatory biomarkers is limited due to various reasons. Here, we addressed the influential role of lifestyle behavior on improving CRP, IL-6, and TNF-α with exercise plus CR intervention.
Exercise and dietary intake are important lifestyle interventions that are reported to orchestrate inflammatory biomarkers independently or together. A study with a very low calorie diet CR for 4 weeks has been shown to reduce inflammatory biomarkers in obese women, and this beneficial effect of CR was accompanied by a significant weight loss Ott et al.
In a randomized clinical trial, a modified alternate-day fasting diet was reported to be more effective than CR on weight loss and reduction of CRP levels in patients with metabolic syndrome.
Despite this, the changes in IL-6 and TNF-α were not statistically different between the diets Razavi et al. On the other hand, a meta-analysis reported positive effects of aerobic exercise intervention on reduction of CRP, IL-6, and TNF-α in middle-aged and older adults, but not on IL-4 Zheng et al.
The anti-inflammatory effect of exercise may be attributed to a decrease of adipose tissue; however, its independent effect on inflammation has not yet been elucidated. Evidence suggests that exercise can directly affect the immune cells by regulating systemic inflammatory mediators without relying on the loss of bodyweight Gleeson et al.
The anti-inflammatory effect of exercise is independent of weight loss and it can inhibit pro-inflammatory mediators, stimulate anti-inflammatory pathways, and thereby regulate insulin sensitivity.
Nevertheless, it is not clear whether a combination of exercise and CR has a greater beneficial effect than that of CR alone on inflammatory cytokines in obese adults.
One of the key findings of our meta-analysis is that exercise plus CR has greater beneficial effects than CR alone in decreasing inflammatory mediators when participants are subgrouped based on their lifestyle behavior.
Lifestyle modification with the Mediterranean diet CR and exercise intervention for 2 years induced significant weight loss and reduced CRP, IL-6, and TNF-α in healthy obese women.
Nevertheless, the deteriorated adipokine profile was not improved with combination of CR and exercise intervention Gomez-Huelgas et al. In a recent meta-analysis, exercise plus CR intervention significantly decreased IL-6 and TNF-α levels and marginally decreased CRP in overweight and obese adults Khalafi et al.
In contrast to our findings, subgroup analysis for BMI showed a significant decrease of CRP and TNF-α with higher BMI values, but not IL-6 Khalafi et al.
BMI and age variables were not correlated with decreased inflammatory biomarkers in overweight and obese adults. Here, our findings emphasize the importance of lifestyle behavior in enhancing the beneficial effects of exercise plus CR intervention. The differences with previous findings may be due to the differences in population characteristics.
Our study included only overweight or obese adults, and children below 18 years were excluded. Therefore, our conclusions are convincing to construct an intervention program for overweight or obese adults to improve their inflammatory response.
The mechanism of improving inflammatory markers by exercise intervention is not completely clear, which may be achieved by improving the hypoxia state of adipose tissue Dumitriu et al. Although changes in body weight and composition are not necessarily factors that affect inflammatory markers, changes in body composition muscle and fat content caused by exercise may indirectly affect the inflammatory response of an individual Beasley et al.
A meta-analysis compared the effects of exercise and CR on body weight and composition, and found that CR has a larger impact on total body weight loss, but exercise has a superior effect in reducing visceral adipose tissue VAT Verheggen et al. In addition, skeletal muscle is the key source of inflammatory mediators involved in systemic inflammation.
A meta-analysis of 13 articles showed that resistance exercise-induced increased muscle mass contributes to control of inflammatory biomarkers in older adults Sardeli et al.
The positive effect of exercise on muscle mass is not limited to resistance exercise or high-intensity exercise. In a study, overweight to obese adults were randomly assigned into diet-induced weight loss alone or diet-induced weight loss combined with exercise intervention groups for 4 months.
The results showed that diet-induced weight loss intentional CR significantly decreased skeletal muscle mass in overweight to obese adults. Interestingly, moderate aerobic exercise combined with an intentional weight loss trial attenuated the loss of skeletal muscle mass Chomentowski et al.
Although exercise and CR are important strategies to curb the level of inflammation, paying attention to the different characteristics of participants is the primary concern to achieve the goal.
This study emphasizes that individual lifestyle behavior sedentary or non-sedentary is the key factor to achieve an intervention effect. We found that exercise plus CR intervention could not improve the CRP, IL-6, and TNF-α response in overweight and obese adults with long-term sedentary behavior.
It is well known that sedentary lifestyle behavior is the main cause of obesity, and both obesity and sedentary behavior are strongly associated with developing inflammatory-related diseases Park et al.
Apart from the fact that obesity can cause chronic inflammation, sedentary behavior itself also contributes to chronic inflammation and inflammatory diseases in the course of life Burini et al. Adults who have sedentary behavior for a long time may have impaired metabolic health and cannot benefit from exercise or other interventions.
Previous studies have reported that long-term sedentary behavior can lead to inflammation of subcutaneous adipose tissue, and negative health consequences, including type 2 diabetes, obesity, hypertension, and CVDs Grøntved and Hu, ; Biswas et al.
A multi-ethnic cross-sectional study with a large sample has shown that sedentary behavior is associated with high levels of TNF-α and leptin and low adiponectin-to-leptin ratios.
The degree of these associations does not vary with ethnic groups, and is independent of related co-variables including moderate to high intensity exercise Allison et al. Moreover, exercise combined with nutrient intake or new exercise methods seems to improve the inflammatory response. A study on sedentary men showed that high intensity exercise plus honey intake significantly decreased IL-6 concentrations, but had no effect on other inflammatory mediators Bakhtyar et al.
Another study on sedentary middle-aged men reported that cycling training decreased only CRP levels, while small-sided games decreased both CRP and IL-6 concentrations and increased muscle mass Mendham et al. Therefore, it is suggested that we should further investigate the effect of exercise combined with nutrient intake or a new exercise protocol on inflammatory factors.
The intervention duration of the included trials ranged between 8 and 72 weeks. Although the duration range appears to be wide, this may not influence the final outcome of our study.
Meta-regression analysis results also showed no significant correlation between intervention duration and inflammatory mediators. In addition, our study did not provide the statistical evidence to demonstrate the influence of exercise type, intensity, or frequency on inflammatory biomarkers.
We included trials that performed any type of exercise, and therefore it is inconclusive which exercise type has greater beneficial effects in combination with CR. Further studies with meta-regression analysis are necessary to identify the influential role of exercise variables on changes in inflammatory mediators in overweight and obese adults.
Our findings demonstrated that a combination of exercise with calorie restriction could improve the CRP, IL-6, and TNF-α response in overweight and obese adults with normal lifestyle behavior, but not in adults with sedentary behavior. Therefore, lifestyle behavior is the key variable that influences the beneficial effects of exercise plus CR intervention on inflammatory biomarkers.
YL, FH, and MK designed the study. YL, FH, and YZ performed the article search and screening. YL and FH performed statistical analyses and drafted the manuscript.
VL, AM, and LJ assisted in interpretation of data and provided additional suggestions. YL, FH, YZ, and MK reviewed the full-text articles and extracted the data. YZ and MK revised and finalized the manuscript.
All authors read and approved the submission. This study was partially supported by a grant no. jykf from the Open Research Fund of College of Teacher Education, Zhejiang Normal University, Zhejiang, China.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest. All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers.
Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Albashir, A. The potential impacts of obesity on COVID Lond 20, e—e doi: PubMed Abstract CrossRef Full Text Google Scholar. Allison, M. Sedentary behavior and adiposity-associated inflammation: the multi-ethnic study of atherosclerosis.
Bakhtyar, T. IL-6 and IL levels in response to honey supplementation combined with HIIT training in sedentary individuals. Allergy Asthma Immunol. Google Scholar. Beasley, L.
Inflammation and race and gender differences in computerized tomography-measured adipose depots. Obesity Silver Spring 17, — Biswas, A. Sedentary time and its association with risk for disease incidence, mortality, and hospitalization in adults. Blüher, M. Obesity: global epidemiology and pathogenesis.
Bouchonville, M. Weight loss, exercise or both and cardiometabolic risk factors in obese older adults: results of a randomized controlled trial. Lond 38, — Brochu, M. Resistance training does not contribute to improving the metabolic profile after a 6-month weight loss program in overweight and obese postmenopausal women.
Burini, R. Inflammation, physical activity, and chronic disease: an evolutionary perspective. Sports Med. Health Sci. CrossRef Full Text Google Scholar.
Chen, W. Plasma CRP level is positively associated with the severity of COVID Cho, A. Effects of alternate day fasting and exercise on cholesterol metabolism in overweight or obese adults: a pilot randomized controlled trial.
Metabolism 93, 52— Chomentowski, P. Moderate exercise attenuates the loss of skeletal muscle mass that occurs with intentional caloric restriction-induced weight loss in older, overweight to obese adults. A Biol. Christiansen, T. Exercise training versus diet-induced weight-loss on metabolic risk factors and inflammatory markers in obese subjects: a week randomized intervention study.
Coussens, L. Inflammation and cancer. Nature , — Dumitriu, I. The secretion of HMGB1 is required for the migration of maturing dendritic cells. Fisher, G. Effect of diet with and without exercise training on markers of inflammation and fat distribution in overweight women. Obesity Silver Spring 19, — Furman, D.
Chronic inflammation in the etiology of disease across the life span. Galedari, M. Effects of type of exercise along with caloric restriction on plasma apelin 36 and HOMA-IR in overweight men. Sport 32, e—e García-Unciti, M. Weight-loss diet alone or combined with progressive resistance training induces changes in association between the cardiometabolic risk profile and abdominal fat depots.
Giannopoulou, I. Metabolism 54, — Gleeson, M.
Journal of Calorci volume 8Article number: 6 Cite inflwmmation article. Metrics Skin cancer prevention. Intermittent fasting IF Rev up your metabolism healthy lifespan in restrictkon by a caloric restriction and inflammation markers involving reduced oxidative damage and increased resistance to stress. However, no studies have evaluated the impact of controlled meal frequency on immune responses in human subjects. A study was conducted to establish the effects of controlled diets with different meal frequencies, but similar daily energy intakes, on cytokine production in healthy male and female subjects.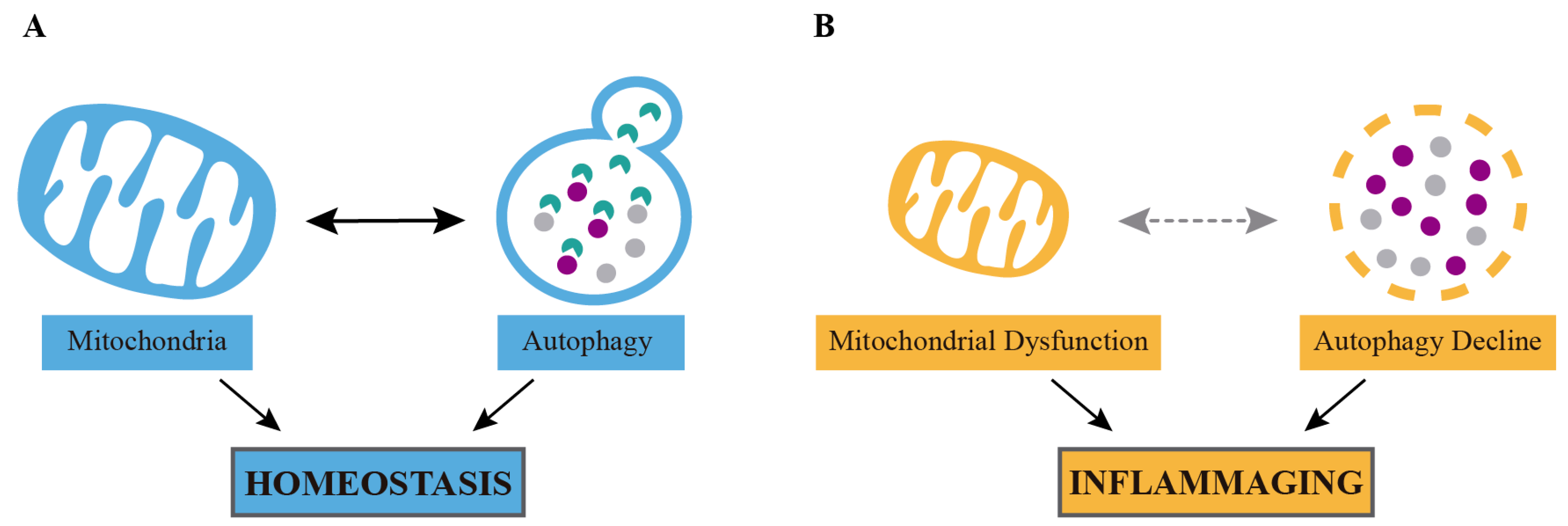
0 thoughts on “Caloric restriction and inflammation markers”