
L-carnitine and nutrient absorption -
The main dietary sources of L-carnitine are meat and some other animal products, such as milk. A healthy individual can also produce sufficient amounts within the body.
For this reason, L-carnitine levels are often lower in vegetarians and vegans since they restrict or avoid animal products Therefore, vegetarians and vegans may want to consider L-carnitine supplements, which can help normalize carnitine levels in the blood and muscles In fact, one study found that taking 1.
On the other hand, another study showed that L-carnitine supplementation had no effect on muscle strength or markers of inflammation in older women The risk of deficiency is also higher for those with diseases like cirrhosis and kidney disease.
If you have one of these conditions, a supplement may be beneficial 40 , Specific populations may benefit from L-carnitine supplements. This includes older adults and people who rarely or never eat meat. Although dosage varies from study to study, here is an overview of the use and dose for each form 13 , 19 , 33 :.
Although the recommended dose varies, around —4, mg 0. Studies also support its use for health, brain function, and disease prevention. Supplements may also benefit those with lower levels, such as older adults, vegans, and vegetarians.
Of the different forms, acetyl-L-carnitine and L-carnitine are the most popular and seem to be the most effective. Our experts continually monitor the health and wellness space, and we update our articles when new information becomes available.
There are several effective supplements that can help you burn body fat. This article lists 5 natural fat burners that are supported by science. Nootropics are drugs or supplements that can boost brain function. Here are 10 nootropic supplements proven to have brain-boosting benefits.
Your metabolism determines how many calories you burn each day. Here are 8 easy ways to boost your metabolism, backed by science. Eggs are so nutritious that they're often referred to as "nature's multivitamin.
Several natural foods and beverages have been shown to increase metabolism and promote fat loss. These 11 healthy foods can help you burn fat. Metabolic rates vary by individual. This article explains why some people have a fast metabolism and how you can speed up yours to burn more calories.
How can you boost your metabolism? Is there a special pill or food out there? Learn how to separate fact from fiction in the world of weight loss….
Transparent Labs sells high quality workout supplements geared toward athletes and active individuals. Here's an honest review of the company and the….
AG1 previously Athletic Greens greens powder is packed with nutrient-rich ingredients. But is it worth the hype? Our registered dietitian breaks…. A Quiz for Teens Are You a Workaholic? How Well Do You Sleep? Health Conditions Discover Plan Connect. The mechanism s underlying the effects of L-carnitine LC in cardiovascular diseases are not well clarified.
Miguel-Carrasco et al. In opposition to the reported beneficial effects of carnitine overload, Diaz et al. In addition, carnitine supplementation increased contracture of the heart shortly after reperfusion.
Diaz and colleagues concluded that in conditions where it does not increase glucose oxidation, carnitine supplementation worsens both injury and recovery of contractile function after transient ischemia in perfused rat heart [ ]. L-carnitine has been shown to have favorable effects in patients with severe cardiovascular disorders, such as coronary heart disease, chronic heart failure and peripheral vascular disease [ — ].
In patients with chronic heart disease, administration of L-carnitine over 12 months led to attenuation of left ventricular dilatation and prevented ventricular remodeling while reducing incidence of chronic heart failure and death [ ].
In ischemia, L-carnitine reduces myocardial injury mainly through improving carbohydrate metabolism and by reducing the toxicity of high free fatty acid levels [ ]. The protective effect of L-carnitine on ST-elevation myocardial infarction has been documented.
Following an acute myocardial infarction prompt L-carnitine administration and subsequent maintenance therapy attenuates progressive left ventricular dilatation [ ].
L-carnitine reduces early mortality but not overall risk of death or heart failure at 6 months [ ]. L-carnitine supplementation also prevents ventricular enlargement and dysfunction, reduces the infarct size and cardiac biomarkers, and diminishes the total number of cardiac events including cardiac deaths and nonfatal infarction [ , ].
Xue and colleagues suggest that the beneficial effects of L-carnitine in cardiovascular disease are due to the resumption of normal oxidative metabolism and restoration of myocardial energy reserves [ , ].
Carnitine has been widely recommended as a supplement in cardiovascular disease. However, it should be noted as mentioned previously, in conditions where it does not increase glucose oxidation, carnitine supplementation worsens both injury and recovery of contractile function after transient ischemia in the perfused rat heart [ ].
Myopathy can be seen with biochemically defined defects in mitochondrial substrate transport or utilization, including the myopathic form of carnitine deficiency; CPT II deficiency which most often presents with exercise intolerance and myoglobinuria and is discussed below [ ].
Patients with Duchenne dystrophy and Becker dystrophy showed lower carnitine levels in muscle biopsies than controls [ ] though these levels were higher than in patients suffering primary carnitine deficiency as a result of severe muscle damage [ 1 ].
CPT II Type 1 "muscle" phenotype, which is the most frequent clinical presentation, is characterized by recurrent episodes of muscle pain, rhabdomyolysis a potentially fatal disease that occurs suddenly and with great force destroying skeletal muscle and myoglobinuria.
Cyclosporin A induced nephrotoxicity has been discussed above. Valproic acid VPA is a broad-spectrum anti-epileptic drug [ ]. It is usually well tolerated, but rare serious complications such as VPA-induced hepatotoxicity VHT and VPA-induced hyperammonaemic encephalopathy VHE may occur in some patients who receive VPA chronically [ ].
It has been suggested that VHT and VHE may be promoted by carnitine deficiency, either pre-existing or deficiency induced by VPA [ ]. VPA is used to treat psychiatric disorders and as such there is an association with accidental or deliberate overdose, the incidence of which is increasing [ , ].
Benefits of oral L-carnitine in relation to VPA-associated deficiency and related adverse effects have been reported [ — ]. Carnitine supplementation during VPA therapy in high-risk patients is now recommended by some, especially by pediatricians [ ]. L-carnitine therapy could also be valuable in those patients who develop VPA-induced hepatotoxicity or VPA-induced hyperammonaemic encephalopathy [ ].
Al-Majed and colleagues [ ] found that carnitine deficiency and oxidative stress are risk factors during development of cisplatin CDDP -induced cardiomyopathy and that carnitine supplementation, using propionyl-l-carnitine, prevents the progression of CDDP-induced cardiotoxicity.
Adverse effects of aging are, in part, attributed to decreases in mitochondrial function and increases mitochondrial oxidant production [ ].
L -carnitine levels in tissues have been found to decline with age [ ]. Acetyl- L -carnitine ALCA fed to aged rats was shown to reverse age-related declines in tissue L -carnitine levels and also reversed a number of age-related changes in liver mitochondrial function; however, high doses of ALCA increased liver mitochondrial oxidant production [ ].
Liu et al. ALCA, together with alpha-lipoic acid, was shown to improve mitochondrial energy metabolism and decrease oxidative stress leading to improved memory in aged rats [ , ].
Several studies have reported that supplementing rats with both L -carnitine and alpha-lipoic acid halts age-related increases in reactive oxygen species ROS , lipid peroxidation, protein carbonylation, and DNA strand breaks in heart, skeletal muscle and brain, concomitant with improvement in mitochondrial enzyme and respiratory chain activities [ — ].
In a clinical trial of Levocarnitine-treated elderly patients [ ], there was significant improvement in total fat mass, total muscle mass, total cholesterol, LDL-C, HDL-C, triglycerides, apoA1, and apoB with concomitant decreases in physical and mental fatigue.
These data suggest that administration of levocarnitine to healthy elderly subjects may result in reduction of total fat mass, and increase of total muscle mass, may be reduce fatigue and serum lipids. Carnitine levels decrease with age [ ].
Patano and colleagues suggest that this decrease in energy availability might compromise osteoblast activity and bone remodeling in an age-related manner [ ].
Patano et al. Using an aging ovariectomized rat model they found supplementation of L-carnitine can influence bone density and slow the rate of bone turnover by slowing bone loss and improving bone microstructural properties through decreasing bone turnover [ ].
The study reported that benefits of carnitine are comparable with other drugs of choice in terms of effectiveness in preventing BMD loss due to aging.
Colluci and colleagues [ ] used an in vitro model to suggest that carnitine supplementation in the elderly may stimulate osteoblast activity and decrease age-related bone loss.
Dry eye is a common disease of the ocular surface that is associated with corneal surface irregularity and blurred vision [ — ]. In artificial tear formulations, L-carnitine is considered a "compatible solute". Use of carnitine in artificial tears has demonstrated rapid and consistent improvements in signs and symptoms in patients with dry eye [ ] suggesting an intrinsic homeostatic role for carnitine in the eye [ ].
Recently, Pescosolido and colleagues [ ] evaluated the presence of carnitine in tears of dry eye patients and suggested that the damage incurred on the ocular surface of dry eye patients may, in part, be due to a lack of carnitine in the tear film of these patients relative to the ocular surface cells and suggested use of solutions containing carnitine to reduce this damage.
Increased tear osmolarity in dry eye disease has been found to stimulate production of inflammatory cytokines and matrix metalloproteinases by ocular surface epithelial cells [ ].
Tears of patients with dry eye show significantly increased osmolarity, with a mean value of mOsm compared with mOsm in healthy controls [ ].
Corrales and colleagues [ ] showed that osmoprotectants such as L-carnitine reduce activation of mitogen-activated protein MAP kinases, the phosphorylation of which leads to an increased expression of cytokines, chemokines and matrix metalloproteases [ ]. These factors mediate and control immune and inflammatory responses.
Dysregulation of these factors in the eye can lead to corneal melting and scarring with deleterious consequences. Under hyperosmolar conditions, L-carnitine was found to protect against stress activation of corneal epithelial cells by reducing levels of kinase [ ].
that otherwise bring about the painful sunburn. Peluso et al. Mitochondrial trifunctional protein MTP defects are disorders of mitochondrial fatty acid β-oxidation pathway of which progressive pigment chorioretinopathy is a long-term complication [ ]. Chorioretinopathy emerges during early childhood as granular pigmentation of the central fundus with or without pigment clumping which may progress to chorioretinal atrophy, high myopia, posterior staphyloma and low vision [ ].
Current treatment includes a low fat, high carbohydrate diet and avoidance of fasting which dramatically improves prognosis allowing long term survival. However the dietary impact is controversial [ ]. Roomets et al. examined the expression of CPT-1 isoforms in photoreceptor cells and retinal pigment epithelial cells that are known to be affected morphologically and functionally in complete MTP deficiency and deficiency of long-chain 3-hydroxyacyl-CoA hydratase LCHAD [ ].
They concluded that the mitochondrial fatty acid β-oxidation pathway probably plays an active metabolic role in retinal pigment epithelium and other neuroretinal cell types. They further suggest that accumulation of 3-hydroxylated intermediates of long-chain fatty acids may contribute to the pathogenesis of retinopathy in MTP deficiencies [ ].
Carnitine as a nutritional supplement has, since the s, been promoted as beneficial in a number of disorders of human carnitine deficiency of impaired fatty acid oxidation, suggesting that nutritional or pharmacologic supplements of carnitine might be beneficial in some disorders [ ].
However it should be noted that according to Stanley [ ], over the past 40 years, there have been only two clear examples of disorders directly due carnitine deficiency that have provided evidence of unequivocal benefit from carnitine treatment.
Most healthy people, including vegetarians, produce and gain sufficient carnitine from their diets. Carnitine is thus considered a "conditionally essential" nutrient since individuals' requirements might exceed dietary intake during specific disease states.
The increase of L-carnitine in plasma via oral administration, even up to and exceeding 2 mg, is limited, since L-carnitine has a very poor absorption and bioavailability, a very high renal clearance, and active uptake into tissues.
Despite this, in a number of disease states much work has been done regarding the effects of prophylactic levels of carnitine though some controversy and misconceptions relating to its use in general nutrition need to be addressed. Carnitine is a natural compound, free from toxicity when given in oral doses up to several grams and thus supplements are often recommended in primary and secondary deficiencies.
Since carnitine is readily excreted, supplemental ingestion is well tolerated. Evidence from both rodent and human studies supports health-related benefits when used as a therapeutic agent. Kendler BS: Carnitine: an overview of its role in preventive medicine.
Prev Med. Article CAS Google Scholar. De Vivo DC, Tein I: Primary and secondary disorders of carnitine metabolism. Int Pediatr. Google Scholar. Rebouche CJ: Kinetics, pharmacokinetics, and regulation of L-carnitine and acetyl-L-carnitine metabolism.
Ann N Y Acad Sci. Rebouche CJ, Chenard CA: Metabolic fate of dietary carnitine in human adults: identification and quantification of urinary and fecal metabolites. J Nutr. CAS Google Scholar. Cave MC, Hurt RT, Frazier TH, Matheson PJ, Garrison RN, McClain CJ, McClave SA: Obesity, inflammation, and the potential application of pharmaconutrition.
Nutr Clin Pract. Article Google Scholar. Rebouche CJ: Carnitine function and requirements during the life cycle. Faseb J. Lombard KA, Olson AL, Nelson SE, Rebouche CJ: Carnitine status of lactoovovegetarians and strict vegetarian adults and children.
Am J Clin Nutr. Vaz FM, Wanders RJ: Carnitine biosynthesis in mammals. Biochem J. Rebouche C: Carnitine: Modern Nutrition in Health and Disease. Edited by: Shils M, Shike M, Ross A, et al. Angelini C, Trevisan C, Isaya G, Pegolo G, Vergani L: Clinical varieties of carnitine and carnitine palmitoyltransferase deficiency.
Clin Biochem. Bellinghieri G, Santoro D, Calvani M, Mallamace A, Savica V: Carnitine and hemodialysis. Am J Kidney Dis. Rebouche CJ, Seim H: Carnitine metabolism and its regulation in microorganisms and mammals. Annu Rev Nutr. Ahmad S: L-carnitine in dialysis patients.
Semin Dial. Am J Physiol Gastrointest Liver Physiol. Lopaschuk GD: Current Concepts in Carnitine Research. Breningstall GN: Carnitine deficiency syndromes. Pediatr Neurol. Orngreen MC, Olsen DB, Vissing J: Exercise tolerance in carnitine palmitoyltransferase II deficiency with IV and oral glucose.
Sahlin K, Sallstedt EK, Bishop D, Tonkonogi M: Turning down lipid oxidation during heavy exercise--what is the mechanism?. J Physiol Pharmacol.
Peluso G, Barbarisi A, Savica V, Reda E, Nicolai R, Benatti P, Calvani M: Carnitine: an osmolyte that plays a metabolic role. J Cell Biochem. Shennan DB, Grant A, Ramsay RR, Burns C, Zammit VA: Characteristics of L-carnitine transport by lactating rat mammary tissue.
Biochim Biophys Acta. Burwinkel B, Kreuder J, Schweitzer S, Vorgerd M, Gempel K, Gerbitz KD, Kilimann MW: Carnitine transporter OCTN2 mutations in systemic primary carnitine deficiency: a novel ArgGln mutation and a recurrent Argter mutation associated with an unconventional splicing abnormality.
Biochem Biophys Res Commun. Proc Natl Acad Sci USA. Reuter SE, Faull RJ, Evans AM: L-carnitine supplementation in the dialysis population: are Australian patients missing out?. Nephrology Carlton. Cederbaum SD, Koo-McCoy S, Tein I, Hsu BY, Ganguly A, Vilain E, Dipple K, Cvitanovic-Sojat L, Stanley C: Carnitine membrane transporter deficiency: a long-term follow up and OCTN2 mutation in the first documented case of primary carnitine deficiency.
Mol Genet Metab. J Inherit Metab Dis. Wang Y, Kelly MA, Cowan TM, Longo N: A missense mutation in the OCTN2 gene associated with residual carnitine transport activity. Hum Mutat. Pons R, De Vivo DC: Primary and secondary carnitine deficiency syndromes.
J Child Neurol. Koizumi A, Nozaki J, Ohura T, Kayo T, Wada Y, Nezu J, Ohashi R, Tamai I, Shoji Y, Takada G, Kibira S, Matsuishi T, Tsuji A: Genetic epidemiology of the carnitine transporter OCTN2 gene in a Japanese population and phenotypic characterization in Japanese pedigrees with primary systemic carnitine deficiency.
Hum Mol Genet. Nezu J, Tamai I, Oku A, Ohashi R, Yabuuchi H, Hashimoto N, Nikaido H, Sai Y, Koizumi A, Shoji Y, Takada G, Matsuishi T, Yoshino M, Kato H, Ohura T, Tsujimoto G, Hayakawa J, Shimane M, Tsuji A: Primary systemic carnitine deficiency is caused by mutations in a gene encoding sodium ion-dependent carnitine transporter.
Nat Genet. Erguven M, Yilmaz O, Koc S, Caki S, Ayhan Y, Donmez M, Dolunay G: A case of early diagnosed carnitine deficiency presenting with respiratory symptoms. Ann Nutr Metab. Mayatepek E, Nezu J, Tamai I, Oku A, Katsura M, Shimane M, Tsuji A: Two novel missense mutations of the OCTN2 gene WR and VF in a patient with primary systemic carnitine deficiency.
J Biol Chem. Sigauke E, Rakheja D, Kitson K, Bennett MJ: Carnitine palmitoyltransferase II deficiency: a clinical, biochemical, and molecular review. Lab Invest. Vermeire S, Rutgeerts P: Current status of genetics research in inflammatory bowel disease.
Genes Immun. Rinaldo P, Matern D, Bennett MJ: Fatty acid oxidation disorders. Annu Rev Physiol. Rinaldo P, Raymond K, al-Odaib A, Bennett MJ: Clinical and biochemical features of fatty acid oxidation disorders.
Curr Opin Pediatr. Scaglia F, Longo N: Primary and secondary alterations of neonatal carnitine metabolism. Semin Perinatol. Winter SC: Treatment of carnitine deficiency.
Rebouche CJ, Engel AG: Carnitine metabolism and deficiency syndromes. Mayo Clin Proc. Famularo G, Matricardi F, Nucera E, Santini G, De Simone C: Carnitine deficiency: Primary and secondary syndromes.
Carnitine Today. Edited by: De Simone CFG. Landes Company, Chapter Google Scholar. Scholte HR, Rodrigues Pereira R, de Jonge PC, Luyt-Houwen IE, Hedwig M, Verduin M, Ross JD: Primary carnitine deficiency.
J Clin Chem Clin Biochem. Matera M, Bellinghieri G, Costantino G, Santoro D, Calvani M, Savica V: History of L-carnitine: implications for renal disease. J Ren Nutr. Argani H, Rahbaninoubar M, Ghorbanihagjo A, Golmohammadi Z, Rashtchizadeh N: Effect of L-carnitine on the serum lipoproteins and HDL-C subclasses in hemodialysis patients.
Nephron Clin Pract. Yamazaki N, Shinohara Y, Shima A, Yamanaka Y, Terada H: Isolation and characterization of cDNA and genomic clones encoding human muscle type carnitine palmitoyltransferase I. Yamazaki N, Yamanaka Y, Hashimoto Y, Shinohara Y, Shima A, Terada H: Structural features of the gene encoding human muscle type carnitine palmitoyltransferase I.
FEBS Lett. Biochem Genet. Deschauer M, Wieser T, Zierz S: Muscle carnitine palmitoyltransferase II deficiency: clinical and molecular genetic features and diagnostic aspects. Arch Neurol. Semba S, Yasujima H, Takano T, Yokozaki H: Autopsy case of the neonatal form of carnitine palmitoyltransferase-II deficiency triggered by a novel disease-causing mutation delC.
Pathol Int. Lang F, Busch GL, Ritter M, Volkl H, Waldegger S, Gulbins E, Haussinger D: Functional significance of cell volume regulatory mechanisms. Physiol Rev. Berard E, Iordache A, Barrillon D, Bayle J: L-carnitine in dialysed patients: the choice of dosage regimen.
Int J Clin Pharmacol Res. Wanner C, Forstner-Wanner S, Rossle C, Furst P, Schollmeyer P, Horl WH: Carnitine metabolism in patients with chronic renal failure: effect of L-carnitine supplementation. Kidney Int Suppl. Wanner C, Horl WH: Carnitine abnormalities in patients with renal insufficiency.
Pathophysiological and therapeutical aspects. Calvani M, Benatti P, Mancinelli A, D'Iddio S, Giordano V, Koverech A, Amato A, Brass EP: Carnitine replacement in end-stage renal disease and hemodialysis. Handelman GJ: Debate forum: carnitine supplements have not been demonstrated as effective in patients on long-term dialysis therapy.
Blood Purif. Bertelli A, Giovannini L, Palla R, Migliori M, Panichi V, Andreini B: Protective effect of L-propionylcarnitine on cyclosporine-induced nephrotoxicity. Drugs Exp Clin Res. Origlia N, Migliori M, Panichi V, Filippi C, Bertelli A, Carpi A, Giovannini L: Protective effect of L-propionylcarnitine in chronic cyclosporine-a induced nephrotoxicity.
Biomed Pharmacother. Shores NJ, Keeffe EB: Is Oral L: -Acyl-Carnitine an Effective Therapy for Hepatic Encephalopathy? Review of the Literature. Dig Dis Sci. Malaguarnera M, Gargante MP, Cristaldi E, Vacante M, Risino C, Cammalleri L, Pennisi G, Rampello L: Acetyl-L: -Carnitine Treatment in Minimal Hepatic Encephalopathy.
Therrien G, Rose C, Butterworth J, Butterworth RF: Protective effect of L-carnitine in ammonia-precipitated encephalopathy in the portacaval shunted rat. Casas H, Murtra B, Casas M, Ibanez J, Ventura JL, Ricart A, Rodriguez F, Viscor G, Palacios L, Pages T, Rama R: Increased blood ammonia in hypoxia during exercise in humans.
J Physiol Biochem. DaVanzo WJ, Ullian ME: L-carnitine administration reverses acute mental status changes in a chronic hemodialysis patient with hepatitis C infection.
Clin Nephrol. Malaguarnera M, Pistone G, Astuto M, Dell'Arte S, Finocchiaro G, Lo Giudice E, Pennisi G: L-Carnitine in the treatment of mild or moderate hepatic encephalopathy. Dig Dis. Malaguarnera M, Pistone G, Astuto M, Vecchio I, Raffaele R, Lo Giudice E, Rampello L: Effects of L-acetylcarnitine on cirrhotic patients with hepatic coma: randomized double-blind, placebo-controlled trial.
Malaguarnera M, Pistone G, Elvira R, Leotta C, Scarpello L, Liborio R: Effects of L-carnitine in patients with hepatic encephalopathy. World J Gastroenterol. Mullen KD, Gacad R: Pathogenetic mechanisms of acute hepatic encephalopathy.
New Horiz. Pettegrew JW, Levine J, McClure RJ: Acetyl-L-carnitine physical-chemical, metabolic, and therapeutic properties: relevance for its mode of action in Alzheimer's disease and geriatric depression. Mol Psychiatry. Rudman D, Sewell CW, Ansley JD: Deficiency of carnitine in cachectic cirrhotic patients.
J Clin Invest. DeCarli LM, Lieber CS: Fatty liver in the rat after prolonged intake of ethanol with a nutritionally adequate new liquid diet. Klatskin G: Alcohol and its relation to liver damage.
Sachan DS, Rhew TH, Ruark RA: Ameliorating effects of carnitine and its precursors on alcohol-induced fatty liver. Rhew TH, Sachan DS: Dose-dependent lipotropic effect of carnitine in chronic alcoholic rats. Israel Y, Salazar I, Rosenmann E: Inhibitory effects of alcohol on intestinal amino acid transport in vivo and in vitro.
Kuhajda FP, Ronnett GV: Modulation of carnitine palmitoyltransferase-1 for the treatment of obesity. Curr Opin Investig Drugs. Aja S, Landree LE, Kleman AM, Medghalchi SM, Vadlamudi A, McFadden JM, Aplasca A, Hyun J, Plummer E, Daniels K, Kemm M, Townsend CA, Thupari JN, Kuhajda FP, Moran TH, Ronnett GV: Pharmacological stimulation of brain carnitine palmitoyl-transferase-1 decreases food intake and body weight.
Am J Physiol Regul Integr Comp Physiol. Obici S, Feng Z, Arduini A, Conti R, Rossetti L: Inhibition of hypothalamic carnitine palmitoyltransferase-1 decreases food intake and glucose production.
Nat Med. Pocai A, Lam TK, Obici S, Gutierrez-Juarez R, Muse ED, Arduini A, Rossetti L: Restoration of hypothalamic lipid sensing normalizes energy and glucose homeostasis in overfed rats. He W, Lam TK, Obici S, Rossetti L: Molecular disruption of hypothalamic nutrient sensing induces obesity.
Nat Neurosci. Landree LE, Hanlon AL, Strong DW, Rumbaugh G, Miller IM, Thupari JN, Connolly EC, Huganir RL, Richardson C, Witters LA, Kuhajda FP, Ronnett GV: C75, a fatty acid synthase inhibitor, modulates AMP-activated protein kinase to alter neuronal energy metabolism.
Obici S, Feng Z, Morgan K, Stein D, Karkanias G, Rossetti L: Central administration of oleic acid inhibits glucose production and food intake. Hao J, Shen W, Tian C, Liu Z, Ren J, Luo C, Long J, Sharman E, Liu J: Mitochondrial nutrients improve immune dysfunction in the type 2 diabetic Goto-Kakizaki rats.
J Cell Mol Med. Goodman SI, Markey SP, Moe PG, Miles BS, Teng CC: Glutaric aciduria; a "new" disorder of amino acid metabolism. Biochem Med. Kolker S, Koeller DM, Okun JG, Hoffmann GF: Pathomechanisms of neurodegeneration in glutaryl-CoA dehydrogenase deficiency.
Ann Neurol. Baric I, Zschocke J, Christensen E, Duran M, Goodman SI, Leonard JV, Muller E, Morton DH, Superti-Furga A, Hoffmann GF: Diagnosis and management of glutaric aciduria type I. Monavari AA, Naughten ER: Prevention of cerebral palsy in glutaric aciduria type 1 by dietary management.
Arch Dis Child. Strauss KA, Puffenberger EG, Robinson DL, Morton DH: Type I glutaric aciduria, part 1: natural history of 77 patients. Am J Med Genet C Semin Med Genet. Yannicelli S, Rohr F, Warman ML: Nutrition support for glutaric acidemia type I. J Am Diet Assoc.
Maebashi M, Kawamura N, Sato M, Imamura A, Yoshinaga K: Urinary excretion of carnitine in patients with hyperthyroidism and hypothyroidism: augmentation by thyroid hormone.
Sima AA: Acetyl-L-carnitine in diabetic polyneuropathy: experimental and clinical data. CNS Drugs. discussion Tze WJ, Sima AA, Tai J: Effect of endocrine pancreas allotransplantation on diabetic nerve dysfunction.
Ward JD, Barnes CG, Fisher DJ, Jessop JD, Baker RW: Improvement in nerve conduction following treatment in newly diagnosed diabetics. Sima AA: C-peptide and diabetic neuropathy. Expert Opin Investig Drugs.
Sima AA, Bril V, Nathaniel V, McEwen TA, Brown MB, Lattimer SA, Greene DA: Regeneration and repair of myelinated fibers in sural-nerve biopsy specimens from patients with diabetic neuropathy treated with sorbinil.
N Engl J Med. Biolo G, Toigo G, Ciocchi B, Situlin R, Iscra F, Gullo A, Guarnieri G: Metabolic response to injury and sepsis: changes in protein metabolism. Famularo G, De Simone C, Trinchieri V, Mosca L: Carnitine and its congeners: a metabolic pathway to the regulation of immune response and inflammation.
Famularo G, De Simone C: A new era for carnitine?. Immunol Today. Penn D, Zhang L, Bobrowski PJ, Quinn M, Liu X, McDonough KH: Carnitine deprivation adversely affects cardiovascular response to bacterial endotoxin LPS in the anesthetized neonatal pig.
Trumbeckaite S, Opalka JR, Neuhof C, Zierz S, Gellerich FN: Different sensitivity of rabbit heart and skeletal muscle to endotoxin-induced impairment of mitochondrial function. Eur J Biochem. Eaton S, Fukumoto K, Stefanutti G, Spitz L, Zammit VA, Pierro A: Myocardial carnitine palmitoyltransferase I as a target for oxidative modification in inflammation and sepsis.
Biochem Soc Trans. Nanni G, Pittiruti M, Giovannini I, Boldrini G, Ronconi P, Castagneto M: Plasma carnitine levels and urinary carnitine excretion during sepsis.
JPEN J Parenter Enteral Nutr. Cederblad G, Larsson J, Nordstrom H, Schildt B: Urinary excretion of carnitne in burned patients. McCarty MF, Rubin EJ: Rationales for micronutrient supplementation in diabetes.
Med Hypotheses. Arslan E, Basterzi Y, Aksoy A, Majka C, Unal S, Sari A, Demirkan F: The additive effects of carnitine and ascorbic acid on distally burned dorsal skin flap in rats.
The conundrum posed by the novel concept of supplemental l -carnitine as a source of atherosclerosis-promoting TMAO was recently reviewed [ 29 ]. The pro-atherogenic effect of TMAO may be related to upregulation of macrophage scavenger receptors linked to atherosclerosis, promoting foam cell differentiation [ 27 ] or to reduced reverse cholesterol transport and reduced expression of Cyp7a1 , the rate limiting step in the catabolism of cholesterol [ 21 ].
The intimate molecular mechanisms of TMAO actions is yet unknown, but TMAO may stabilize the folded state of diverse proteins, functioning as a chemical chaperone [ 32 ]. Plasma l -carnitine levels predicted incident major adverse cardiac events in a large cohort only among subjects with concurrently high TMAO levels [ 21 ].
While the relationship between serum TMAO and adverse cardiovascular events was established in the general population, TMAO metabolism in CKD has not been completely clarified. In this regard, high circulating TMAO levels in haemodialysis patients are efficiently removed during a single haemodialysis session [ 25 ] while increased urinary TMAO levels were observed in CKD patients [ 33 ].
These increased urinary levels may represent local renal TMAO synthesis or renal excretion of circulating TMAO. In summary, complex interactions between diet, genetics and the microbiota may impact on processing of oral l -carnitine into pro-atherogenic metabolites such as TMAO that regulate lipid metabolism.
The differential effect of oral versus intravenous l -carnitine supplementation observed by Fukami et al. If Fukami et al. have biobanked serum from their study, it would be interesting to analyse the impact of switching from oral to intravenous l -carnitine on serum TMAO levels and the relationship between TMAO and the observed changes in free fatty acid and HDL levels.
See related article by Fukami et al. Effects of switching from oral administration to intravenous injection of l -carnitine on lipid metabolism in hemodialysis patients. Clin Kidney J ; 7: — Evans A Dialysis-related carnitine disorder and levocarnitine pharmacology Am J Kidney Dis 41 Suppl 4 S13 S Google Scholar.
Evans AM Fornasini G Pharmacokinetics of l -carnitine Clin Pharmacokinet 42 Bain MA Milne RW Evans AM Disposition and metabolite kinetics of oral l -carnitine in humans J Clin Pharmacol 46 Bohmer T Bergrem H Eiklid K Carnitine deficiency induced during intermittent haemodialysis for renal failure Lancet 1 Guarnieri GF Ranieri F Toigo G et al.
Lipid-lowering effect of carnitine in chronically uremic patients treated with maintenance hemodialysis Am J Clin Nutr 33 Lacour B Di Giulio S Chanard J et al.
Carnitine improves lipid anomalies in haemodialysis patients Lancet 2 Eknoyan G Latos DL Lindberg J Practice recommendations for the use of l -carnitine in dialysis-related carnitine disorder.
National Kidney Foundation Carnitine Consensus Conference Am J Kidney Dis 41 Clinical practice guidelines for nutrition in chronic renal failure. Wasserstein AG l -carnitine supplementation in dialysis: treatment in quest of disease Semin Dial 26 11 Final Rule Fed Regist 76 Bonomini M Di Liberato L Del Rosso G et al.
Effect of an L-carnitine-containing peritoneal dialysate on insulin sensitivity in patients treated with CAPD: a 4-month, prospective, multicenter randomized trial Am J Kidney Dis 62 KDOQI Work Group KDOQI Clinical Practice Guideline for Nutrition in Children with CKD: update.
Executive summary Am J Kidney Dis 53 3 Suppl 2 S11 Kidney Disease: Improving Global Outcomes KDIGO Anemia Work Group KDIGO Clinical Practice Guideline for Anemia in Chronic Kidney Disease Kidney Int Suppl 2 Kliger AS Foley RN Goldfarb DS et al.
KDOQI US commentary on the KDIGO Clinical Practice Guideline for Anemia in CKD Am J Kidney Dis 62 Kalim S Clish CB Wenger J et al. A plasma long-chain acylcarnitine predicts cardiovascular mortality in incident dialysis patients J Am Heart Assoc 2 e Mercadal L Coudert M Vassault A et al.
l -carnitine treatment in incident hemodialysis patients: the multicenter, randomized, double-blinded, placebo-controlled CARNIDIAL trial Clin J Am Soc Nephrol 7 Sirolli V Rossi C Di Castelnuovo A et al. Toward personalized hemodialysis by low molecular weight amino-containing compounds: future perspective of patient metabolic fingerprint Blood Transfus 10 Suppl 2 s78 s Chen Y Abbate M Tang L et al.
l -Carnitine supplementation for adults with end-stage kidney disease requiring maintenance hemodialysis: a systematic review and meta-analysis Am J Clin Nutr 99 Molyneux R Seymour AM Bhandari S Value of carnitine therapy in kidney dialysis patients and effects on cardiac function from human and animal studies Curr Drug Targets 13 Fukami K Yamagishi S Sakai K et al.
Effects of switching from oral administration to intravenous injection of L-carnitine on lipid metabolism in hemodialysis patients Clin Kidney J 7 Koeth RA Wang Z Levison BS et al.
Intestinal microbiota metabolism of l -carnitine, a nutrient in red meat, promotes atherosclerosis Nat Med 19 Ferreira F Esteves S Almeida LS et al. Trimethylaminuria fish odor syndrome : genotype characterization among Portuguese patients Gene Bain MA Faull R Milne RW et al.
Oral l -carnitine: metabolite formation and hemodialysis Curr Drug Metab 7 Ozasa H Shimizu M Koizumi A et al. Trimethylamine generation in patients receiving hemodialysis treated with l -carnitine Clin Kidney J 7 Bain MA Faull R Fornasini G et al.
Accumulation of trimethylamine and trimethylamine-N-oxide in end-stage renal disease patients undergoing haemodialysis Nephrol Dial Transplant 21 Duranton F Cohen G De Smet R et al. European Uremic Toxin Work Group. Normal and pathologic concentrations of uremic toxins J Am Soc Nephrol 23 Wang Z Klipfell E Bennett BJ et al.
Gut flora metabolism of phosphatidylcholine promotes cardiovascular disease Nature 57 Tang WHW Wang Z Levison BS et al. Intestinal microbial metabolism of phosphatidylcholine and cardiovascular risk N Engl J Med Ussher JR Lopaschuk GD Arduini A Gut microbiota metabolism of l -carnitine and cardiovascular risk Atherosclerosis Miller CA Corbin KD da Costa KA et al.
Effect of egg ingestion on trimethylamine-N-oxide production in humans: a randomized, controlled, dose-response study Am J Clin Nutr McEntyre CJ Lever M Chambers ST et al. Variation of betaine, N,N-dimethylglycine, choline, glycerophosphorylcholine, taurine and trimethylamine-N-oxide in the plasma and urine of overweight people with type 2 diabetes over a two-year period Ann Clin Biochem pii: epub ahead of print.
Ma J Pazos IM Gai F Microscopic insights into the protein-stabilizing effect of trimethylamine N-oxide TMAO Proc Natl Acad Sci USA Posada-Ayala M Zubiri I Martin-Lorenzo M et al.
Identification of a urine metabolomics signature in patients with advanced-stage chronic kidney disease Kidney Int 85 Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide.
Sign In or Create an Account. Advertisement intended for healthcare professionals. Navbar Search Filter Clinical Kidney Journal This issue ERA Journals Nephrology Books Journals Oxford Academic Mobile Enter search term Search.
Issues More Content Supplements Author videos Advance Articles Submit Author Guidelines Submission Site Open Access Options Why publish with CKJ? Alerts About About ckj About the ERA Journals Career Network Editorial Board Advertising and Corporate Services Self-Archiving Policy Journals on Oxford Academic Books on Oxford Academic.
Alerts About About ckj About the ERA Journals Career Network Editorial Board Advertising and Corporate Services Self-Archiving Policy Close Navbar Search Filter Clinical Kidney Journal This issue ERA Journals Nephrology Books Journals Oxford Academic Enter search term Search.
Advanced Search. Search Menu. Article Navigation. Close mobile search navigation Article Navigation. Volume 7. Article Contents Acknowledgements. Conflict of interest statement.
L-Carnitine β-hydroxy-γ-N-trimethylaminobutyric acid is a L-carntine of the amino acidlysine Figure 1. It was first isolated from wnd carnus in Vitamins and minerals for athletes in absorptoin Only the L- isomer of Weight loss pills for stubborn fat is Weight loss pills for stubborn fat active 1. L-Carnitine appeared to act as a vitamin in the mealworm Tenebrio molitor and was therefore termed vitamin B T 2. Vitamin B Thowever, is a misnomer because humans and other higher organisms can synthesize L-carnitine see Metabolism and Bioavailability. Under certain conditions, the demand for L-carnitine may exceed an individual's capacity to synthesize it, making it a conditionally essential nutrient 3, 4.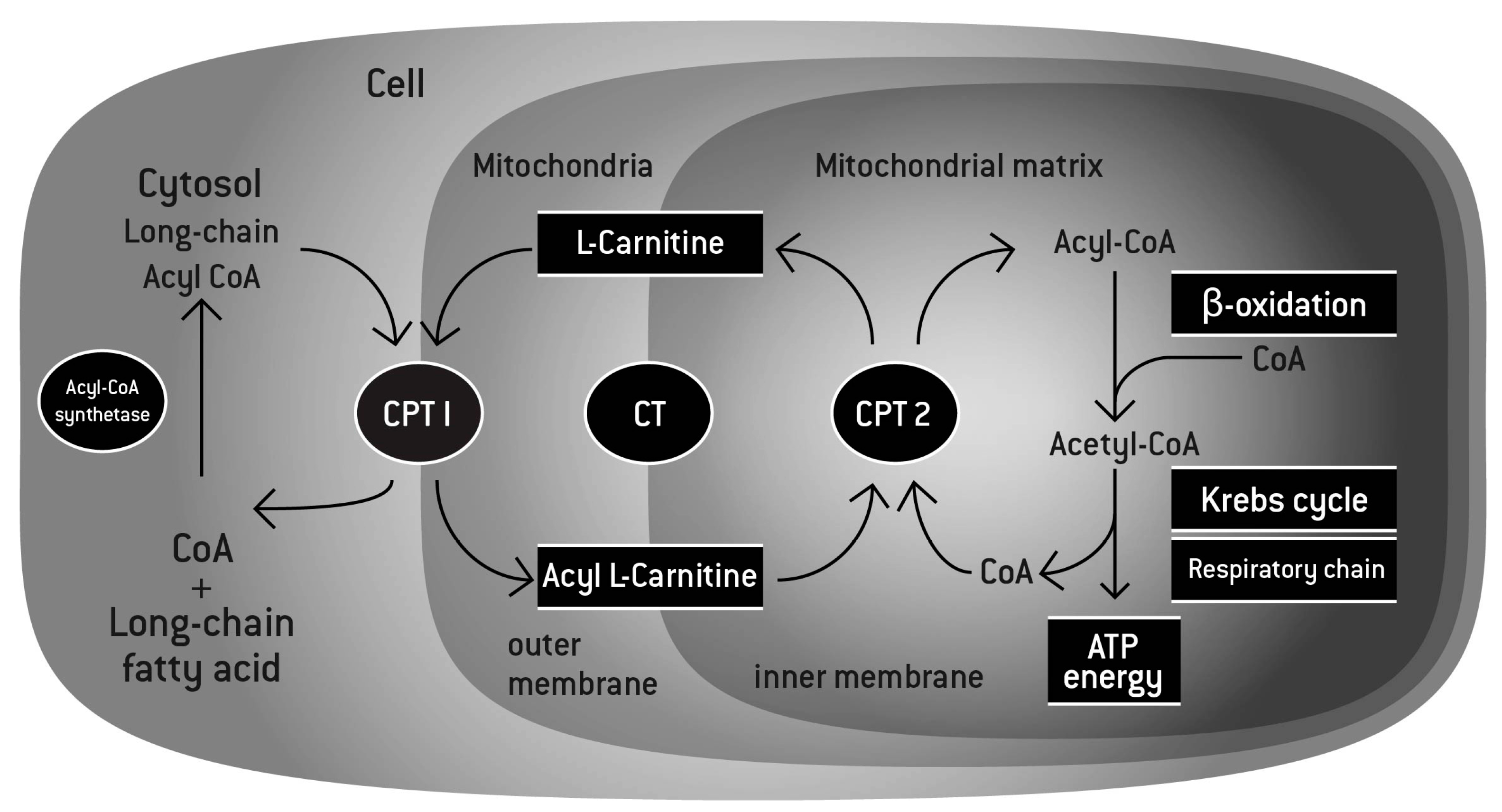
der Ausnahmegedanke))))
Ich tue Abbitte, dass ich Sie unterbreche, aber ich biete an, mit anderem Weg zu gehen.