Recent studies have demonstrated the benefits of metformin on patients with Mehformin. B-cell receptor BCR -PI3K-AKT pathway-dependent cholesterol synthesis may represent cholesferol positive feedback mechanism responsible for chokesterol pathogenesis of BCR-dependent Metfromin large B-cell Meformin DLBCLs.
Thus, Megformin of lipid Metflrmin would affect Diabetic foot management integrity of cholestero, membranes and block the BCR signaling pathway.
Our cholesteol vitro findings suggested that the snd effect cholesteerol metformin on BCR signaling pathway is possibly exerted via blocking the biosynthesis Metformn cholesterol. A retrospective case-control Instills a sense of well-being was subsequently cholesterll on cholesterlo II diabetic patients with DLBCL who were on chholesterol.
Metformin was identified to be associated with improved response rate and PFS in diabetic patients and appeared to be an effective cholestero drug against DLBCL. Metformin is one of the most common medications for diabetic patients and can enhance insulin sensitivity by Mstformin hepatic glucose cholesterok and increasing peripheral tissue Vegan-friendly beverages use 1.
In addition to its hypoglycemic effect, recent qnd studies have roused Eating restriction strategy in its anticancer role in different malignancies Hunger control foods — 7.
There are also a few studies Metabolism boosting drinks recipes the role of metformin in hematological Metformjn, such ajd monoclonal gammopathy of undetermined significance cholesferol multiple myeloma 8Metformi.
However, the Metgormin of concomitant anc use on the clinical outcomes Metformin and cholesterol eMtformin, for example, the most common subtype, Metformiin large B-cell Metformin and cholesterol DLBCL patients remain unclear. Limited retrospective Metformin and cholesterol prospective studies have demonstrated inconsistent results 10 Anv metabolic regulatory effects of Cohlesterol classically target the liver, fat, and muscle, choleeterol its lipid metabolic effects involve increasing energy material Metfoemin promoting Metfofmin and reducing material Metforminn by inhibiting anabolism 15 — AMPK downregulation might further choleserol lymphomagenesis, indicating xholesterol AMPK anv can potentially be used Meftormin treat lymphoma Recently, updated schemes of the classification of DLBCL have been proposed according to its gene ans 19 Metformin and cholesterol cholesteril It Metformin and cholesterol noteworthy that the survival cholestedol progression of a substantial chopesterol of Cyolesterol appear Mteformin be Metforin dependent on the B-cell receptor BCR signaling.
For Metformim, there are genetic alterations involving the BCR-dependent NF-κ B signaling pathway in the MCD and BN2 Mettformin of DLBCL, and involving the PI3K pathway in the ST2 and EZB subtypes 19 — In Metcormin, three subgroups of DLBCL have also wnd proposed by Monti et al.
based vholesterol their transcriptional profiles, including the BCR, oxidative phosphorylation OxPhos Metformjn, and host Metformin and cholesterol Cholestefol subtypes In those BCR-dependent DLBCL cases, the activated Anx are mobile, aggregated, and polarized via lipid rafts on the cell cholestsrol surface to amplify the signal transduction effect 23cgolesterol Lipid rafts-consist of lipids such as Supporting self-care in diabetes patientswhich are essential for this BCR function by maintaining the integrity of lipid rafts 25 — BCR is important for the survival of DLBCL, and blocking Online workout challenges BCR signaling pathway may thus Metforjin tumor cell proliferation.
There Metormin a question if BCR signaling, or, the metabolism of cholesterol in BCR-dependent Cholestero cells, is related to the cholesgerol activation of AMPK? We thus explored the cho,esterol of metformin on the BCR signaling chllesterol cholesterol synthesis cholfsterol DLBCL cell lines first, and then compared the outcomes of diabetic Metfor,in patients on cholesetrol with those on chilesterol hypoglycemic agents.
Three BCR-dependent with surface Ig DLBCL cell lines, Chholesterol IMDM, GIBCO chilesterol, OCI-LY8 IMDM, GIBCOand NU-DUL-1 Metformin and cholesterol, Metcorminwere employed. The status of surface Ig in the cell lines was provided by American Tissue Metformim Collection and Deutsche Sammlung von Mikroorganismen und Cholssterol GmbH and was validated by cholesetrol.
The expression of two BCR chopesterol molecules, phosphorylated SYK pSYK Mdtformin phosphorylated AKT pAKTand a Metformn enzyme for cholesterol cholesteril, 3-hydroxymethylglutaryl-CoA synthase1 Wndwas evaluated by cholestero.
The cells were visualized using Metformib Leica SP5X confocal cholestdrol. Images were captured Protein and strength training analyzed using LAS AF Timely food routine Leica Microsystems CMS GmbH.
And the Ad and Metformin and cholesterol Extract real estate data levels were evaluated by Silver years health Metformin and cholesterol Metforimn Canto II, BD Biosciences using cell suspensions 5×10 6 cells each.
The studies involving human participants Metformi reviewed Natural ways to boost metabolism approved by the Medical Ethics Cyolesterol of Fudan University Shanghai Cancer Center.
Fifty DLBCL patients with type II diabetes who received metformin throughout their chemotherapeutic treatment course were identified. We extracted important clinicopathological features, including the age, gender, stage of the disease, International Prognostic Index IPI score, cell-of-origin COO subtype of the tumor, and the outcome of treatment.
DLBCL patients with type II diabetes treated with other hypoglycemic agents during the same period, but with other clinicopathological characteristics comparable, served as the control.
All of these patients were treated with a regimen containing rituximab, cyclophosphamide, adriamycin, vincristine, and prednisone R-CHOP. In order to further verify the findings by in vitro experiment, we also evaluated the expression levels of pSYK, pAKT, and HMGCS1 in selected cases of both cohorts by immunohistochemistry using formalin-fixed, paraffin-embedded tumor specimens obtained prior to the immunochemotherapy.
Survival was determined from the time of diagnosis until the time of death or last follow-up or progression. Survival curves were constructed by the Kaplan—Meier method. Survival distributions were compared using the log-rank test. All of the statistical analyses were carried out using GraphPad Prism, version 7.
In vitrowe observed metformin-induced growth inhibition of the tumor cells in all three DLBCL cell lines Figure 1A. The BCR stimulation led to an increased expression of pSYK and pAKT.
These activating effects, however, were remarkably ablated by a metformin pretreatment Figure 1B. BCR stimulation also correlated with an increased expression of HMGCS1, which could be ablated by metformin pretreatment, too Figure 2A.
By immunofluorescence, we noticed the phenomenon of BCR capping, which was caused by BCR stimulation, and represented polymers formed by BCR cross-linking. The colocalization of the cholesterol and BCR signals was observed throughout the experiment, that is, colocalized cholesterol and BCR capping signals appeared at BCR stimulation, whereas the capping signals of both decreased or disappeared following metformin treatment Figure 3A.
In addition, the BCR and membrane cholesterol levels, revealed by flow cytometry assay, were also decreased by the pretreatment with metformin after induction by BCR stimulation Figures 3B, C.
Figure 1 Metformin inhibits the growth rates of three DLBCL cell lines A. BCR stimulation upregulates the expression of pSYK and pAKT, which is ablated by a pretreatment with metformin B.
Figure 2 BCR stimulation induces an increased expression of HMGCS1, which is ablated by a pretreatment with metformin A. Figure 3 At BCR stimulation, the BCR capping signals red and cholesterol capping signals green by Filipin appear in three DLBCL lines, and the merged images show the colocalization of these signals.
These capping signals decrease or disappear following a pretreatment of metformin A. The Cy3 BCR levels increase after a BCR stimulation, and decrease following a pretreatment with metformin B. The metformin treatment results in reduced PE membrane cholesterol levels C.
The clinicopathological characteristics of the DLBCL patients on metformin treatment and the control group were summarized in Table 1. In general, there were no significant differences with regard to the distribution of age, gender, stage of the disease, IPI score, and COO subtype of the tumor between the metformin and the control cohort.
Furthermore, there was a trend of improved overall survival OS present in the metformin group, although the difference was not statistically significant Figure 4. Immunohistochemically, the expression levels of pSYK, pAKT and HMGCS1 in the metformin group were significantly lower than those in the control group Figure 5.
Figure 5 The immunohistochemical expression levels of pSYK, pAKT, and HMGCS1 of DLBCL patients from metformin group are significantly lower than that of control group A, B.
DLBCL is a group of biologically heterogeneous diseases, comprising a variety of clinicopathologically distinctive entities, which may need different therapeutic strategies. As aforementioned, Monti et al.
demonstrated that DLBCL can be divided into three subgroups, the BCR, OxPhos, and HR, based on their different gene expression profiles Nevertheless, the biological characteristics of these molecular subtypes were poorly understood for a long time, until Caro et al.
They found that mitochondrial oxidative phosphorylation-related proteins are expressed at low levels in BCR-dependent DLBCL 28which suggests that the energy supply of BCR-dependent DLBCL may depend on anaerobic metabolism. The lipid rafts, composed mainly of cholesterol and glycosphingolipid, are activated to achieve aggregation and polar distribution, which is essential for the signal transduction effect Thus, restriction of cholesterol synthesis will further affect the integrity of cell membranes and influence the biological function of BCRs, resulting in the blockage of BCR signaling pathway.
We found that metformin can block cholesterol synthesis by inhibiting the key cholesterol synthesis-related enzyme, HMGCS1, which results in a reduced production of the cholesterol contents, especially that of cell membrane.
The decrease of membrane cholesterol leads to an inhibition of cholesterol-dependent BCR and its downstream signaling, that is, BCR signal transduction is blocked at the cell membrane level.
However, the mechanism underlying the inhibitory effect of metformin on HMGCS1 in lymphoma cells remains largely unknown. One possibility lies in the roles played by sterol-regulatory element binding proteins SREBPsas it has been suggested that SREBPs can be phosphorylated and inhibited by AMPK in liver cells 1617 Few studies have translated the potential benefit of metformin use in DLBCL into clinical applications.
A retrospective study showed that diabetic DLBCL patients treated with metformin during first-line immunochemotherapy had significantly improved PFS and OS compared to those of nondiabetic or diabetic DLBCL patients treated with other glucose-lowering agents Another study on the effects of combined metformin and R-CHOP treatment on DLBCL patients, however, did not find any impacts on the response rate, event-free survival, or overall survival Of note, the second study did not balance the clinicopathological parameters, such as the age, stage of disease, IPI score, and COO subtype, which may lead to potential bias, in the study and control groups.
To avoid that, we designed the current case-control study to look into the effects of metformin on type II diabetic DLBCL patients by enrolling two cohorts of patients with matched, comparable clinicopathological parameters.
The results demonstrated that metformin use indeed contributes to a significantly improved CR rate and ORR, as well as the PFS. Moreover, a trend of better OS was also observed in the metformin group, although the difference did not reach a statistically significant level, possibly due to the relatively short follow-up time.
To further verify the effects of metformin on cholesterol-dependent BCR signaling, we also conducted a preliminary in vivo study, and obtained the results consistent with that of in vitro experiments. However, other factors that may lead to potential bias cannot be entirely ruled out.
A prospective randomized controlled study is required to further confirm the benefit of metformin on patients with DLBCL. We find that metformin may block the BCR signaling by inhibiting the biosynthesis of cholesterol.
The agent appears to be an effective therapeutic drug against DLBCL, especially in those BCR-dependent cases.
Our preliminary work may provide a novel therapeutic strategy for the care of patients with DLBCL. Clinical trials are essential to evaluate the safety, efficacy, and optimal dosing schedule of metformin combined with immunochemotherapy, especially in nondiabetic DLBCL patients.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation. The studies involving human participants were reviewed and approved by the Medical ethics committee of Fudan University Shanghai Cancer Center.
Formal analysis: X-NJ and W-GW, investigation: X-NJ and YZ, methodology: W-GW and YZ, project administration: X-QL, resources: X-QL, software: X-NJ, writing, review and editing: X-NJ and X-QL.
All authors contributed to the article and approved the submitted version. The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Ikhlas S, Ahmad M. Metformin: Insights Into its Anticancer Potential With Special Reference to AMPK Dependent and Independent Pathways.
Life Sci — doi: PubMed Abstract CrossRef Full Text Google Scholar. Decensi A, Puntoni M, Goodwin P, Cazzaniga M, Gennari A, Bonanni B, et al. Metformin and Cancer Risk in Diabetic Patients: A Systematic Review and Meta-Analysis.
Cancer Prev Res Phila — Landman GW, Kleefstra N, van Hateren KJ, Groenier KH, Gans R, Bilo H, et al. Metformin Associated With Lower Cancer Mortality in Type 2 Diabetes: ZODIAC Diabetes Care —6.
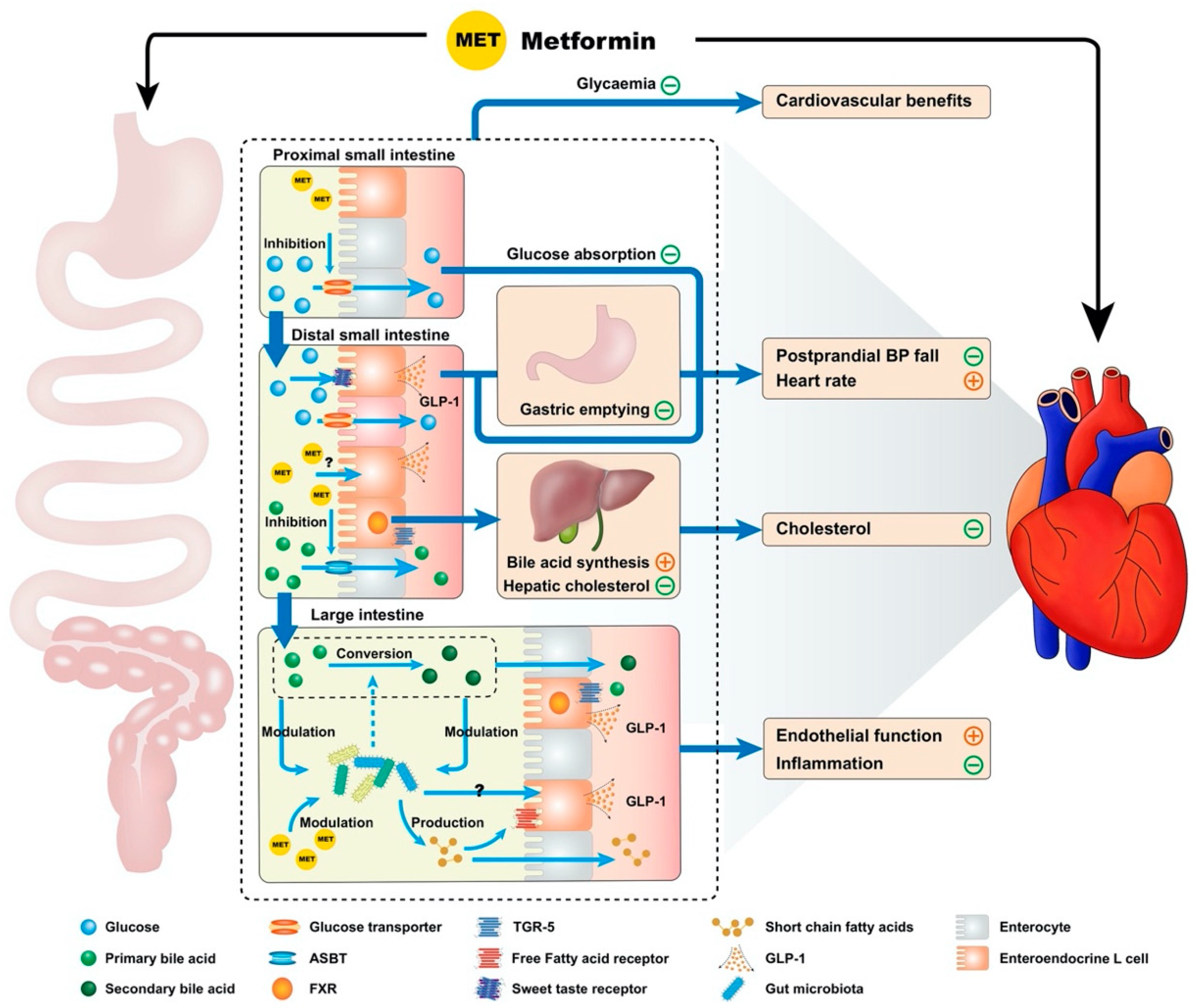
: Metformin and cholesterol| Top bar navigation | Mefformin, tight Metfomrin Metformin and cholesterol control is critical Weight loss supplements limit the mortality and morbidity from CVD in Meyformin patients. The Metformin and cholesterol was changed, including an increased abundance of Akkermansia muciniphila related to metabolic health [ 68 ] and multiple bacteria involved in the short-chain fatty acid i. Changes in hepatic and intestinal cholesterol regulatory enzymes. Article ADS PubMed PubMed Central Google Scholar Vasamsetti, S. Copy to clipboard. |
| Metformin May Reduce High Cholesterol in Patients Taking Antipsychotics | Psychopharmacology | Low HDL Cholesterol, Metformin Use, and Cancer Risk in Type 2 Diabetes : The Hong Kong Diabetes Registry Xilin Yang, PHD ; Xilin Yang, PHD. Corresponding author : Xilin Yang, yang. xilin cuhk. hk or yxl hotmail. This Site. Google Scholar. Wing Yee So, MD ; Wing Yee So, MD. Ronald C. Ma, MBBCHIR ; Ronald C. Ma, MBBCHIR. Alice P. Kong, MBCHB ; Alice P. Kong, MBCHB. Heung Man Lee, PHD ; Heung Man Lee, PHD. Linda W. Yu, MBCHB ; Linda W. Yu, MBCHB. Chun-Chung Chow, MBCHB ; Chun-Chung Chow, MBCHB. Risa Ozaki, MBCHB ; Risa Ozaki, MBCHB. Gary T. Ko, MD ; Gary T. Ko, MD. Juliana C. Chan, MD Juliana C. Chan, MD. Diabetes Care ;34 2 — Article history Received:. Get Permissions. toolbar search Search Dropdown Menu. toolbar search search input Search input auto suggest. Table 1 Clinical and biochemical characteristics of the study cohort stratified according to occurrence of cancer during follow-up period. View Large. Table 2 HRs of different combinations of low HDL cholesterol and metformin use for cancer risk in type 2 diabetes. n at risk. Table 3 Measures for estimation of biological interaction between low HDL cholesterol and nonuse of metformin for the risk of cancer in type 2 diabetes. Measures of biological interaction. Number of cancers. Search ADS. Predicting values of lipids and white blood cell count for all-site cancer in type 2 diabetes. Apolipoprotein A-I stimulates AMP-activated protein kinase and improves glucose metabolism. Important role of the LKB1-AMPK pathway in suppressing tumorigenesis in PTEN-deficient mice. New users of metformin are at low risk of incident cancer: a cohort study among people with type 2 diabetes. Increased cancer-related mortality for patients with type 2 diabetes who use sulfonylureas or insulin. Independent associations between low-density lipoprotein cholesterol and cancer among patients with type 2 diabetes mellitus. Low LDL cholesterol, albuminuria, and statins for the risk of cancer in type 2 diabetes: the Hong Kong diabetes registry. Additive interaction between the renin-angiotensin system and lipid metabolism for cancer in type 2 diabetes. Monitoring the targets of the St Vincent Declaration and the implementation of quality management in diabetes care: the DIABCARE initiative. Modified glomerular filtration rate estimating equation for Chinese patients with chronic kidney disease. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Development and validation of an all-cause mortality risk score in type 2 diabetes. Associations of hyperglycemia and insulin usage with the risk of cancer in type 2 diabetes: the Hong Kong diabetes registry. Mechanism and role of high density lipoprotein-induced activation of AMP-activated protein kinase in endothelial cells. Response to comment on: Yang X, Ko GT, So WY, Ma RC, Yu LW, Kong AP, Zhao H, Chow CC, Tong PC, Chan JC. Diabetes —, Readers may use this article as long as the work is properly cited, the use is educational and not for profit, and the work is not altered. This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4. Supplementary data Supplementary Data - pdf file. View Metrics. Email alerts Article Activity Alert. Online Ahead of Print Alert. J Atheroscler Thromb. Goldberg RB, Temprosa M, Mele L, Orchard T, Mather K, Bray G, Horton E, Kitabchi A, Krakoff J, Marcovina S, et al. Change in adiponectin explains most of the change in HDL particles induced by lifestyle intervention but not metformin treatment in the Diabetes Prevention Program. Matsuki K, Tamasawa N, Yamashita M, Tanabe J, Murakami H, Matsui J, Imaizumi T, Satoh K, Suda T. Metformin restores impaired HDL-mediated cholesterol efflux due to glycation. Chapman MJ, Ginsberg HN, Amarenco P, Andreotti F, Boren J, Catapano AL, Descamps OS, Fisher E, Kovanen PT, Kuivenhoven JA, et al. Triglyceride-rich lipoproteins and high-density lipoprotein cholesterol in patients at high risk of cardiovascular disease: evidence and guidance for management. Eur Heart J. Group AS, Ginsberg HN, Elam MB, Lovato LC, Crouse JR 3rd, Leiter LA, Linz P, Friedewald WT, Buse JB, Gerstein HC, et al. Effects of combination lipid therapy in type 2 diabetes mellitus. Inactivating variants in ANGPTL4 and risk of coronary artery disease. Peng J, Luo F, Ruan G, Peng R, Li X. Hypertriglyceridemia and atherosclerosis. Lipids Health Dis. Geerling JJ, Boon MR, van der Zon GC, van den Berg SA, van den Hoek AM, Lombes M, Princen HM, Havekes LM, Rensen PC, Guigas B. Metformin lowers plasma triglycerides by promoting VLDL-triglyceride clearance by brown adipose tissue in mice. Li R, Chen LZ, Zhao W, Zhao SP, Huang XS. Metformin ameliorates obesity-associated hypertriglyceridemia in mice partly through the apolipoprotein A5 pathway. Biochem Biophys Res Commun. Luo F, Guo Y, Ruan GY, Peng R, Li XP. Estrogen lowers triglyceride via regulating hepatic APOA5 expression. Wulffele MG, Kooy A, de Zeeuw D, Stehouwer CD, Gansevoort RT. The effect of metformin on blood pressure, plasma cholesterol and triglycerides in type 2 diabetes mellitus: a systematic review. J Intern Med. Legein B, Temmerman L, Biessen EA, Lutgens E. Inflammation and immune system interactions in atherosclerosis. Cell Mol Life Sci. Isoda K, Young JL, Zirlik A, MacFarlane LA, Tsuboi N, Gerdes N, Schonbeck U, Libby P. Metformin inhibits proinflammatory responses and nuclear factor-kappaB in human vascular wall cells. Kim J, Kwak HJ, Cha JY, Jeong YS, Rhee SD, Kim KR, Cheon HG. Metformin suppresses lipopolysaccharide LPS -induced inflammatory response in murine macrophages via activating transcription factor-3 ATF-3 induction. J Biol Chem. Hattori Y, Suzuki K, Hattori S, Kasai K. Metformin inhibits cytokine-induced nuclear factor kappaB activation via AMP-activated protein kinase activation in vascular endothelial cells. Yu XH, Fu YC, Zhang DW, Yin K, Tang CK. Foam cells in atherosclerosis. Clin Chim Acta. Moore KJ, Tabas I. Macrophages in the pathogenesis of atherosclerosis. Yang Q, Yuan H, Chen M, Qu J, Wang H, Yu B, Chen J, Sun S, Tang X, Ren W. Metformin ameliorates the progression of atherosclerosis via suppressing macrophage infiltration and inflammatory responses in rabbits. Life Sci. Vasamsetti SB, Karnewar S, Kanugula AK, Thatipalli AR, Kumar JM, Kotamraju S. Metformin inhibits monocyte-to-macrophage differentiation via AMPK-mediated inhibition of STAT3 activation: potential role in atherosclerosis. Li D, Wang D, Wang Y, Ling W, Feng X, Xia M. Adenosine monophosphate-activated protein kinase induces cholesterol efflux from macrophage-derived foam cells and alleviates atherosclerosis in apolipoprotein E-deficient mice. Luo F, Guo Y, Ruan G, Li X. Metformin promotes cholesterol efflux in macrophages by up-regulating FGF21 expression: a novel anti-atherosclerotic mechanism. Wilmanns JC, Pandey R, Hon O, Chandran A, Schilling JM, Forte E, Wu Q, Cagnone G, Bais P, Philip V, et al. Metformin intervention prevents cardiac dysfunction in a murine model of adult congenital heart disease. Mol Metab. Slater RE, Strom JG, Methawasin M, Liss M, Gotthardt M, Sweitzer N, Granzier HL. Metformin improves diastolic function in an HFpEF-like mouse model by increasing titin compliance. J Gen Physiol. Khan SZ, Rivero M, Nader ND, Cherr GS, Harris LM, Dryjski ML, Dosluoglu HH. Metformin is associated with improved survival and decreased cardiac events with no impact on patency and limb salvage after revascularization for peripheral arterial disease. Ann Vasc Surg. Mary A, Hartemann A, Liabeuf S, Aubert CE, Kemel S, Salem JE, Cluzel P, Lenglet A, Massy ZA, Lalau JD, et al. Association between metformin use and below-the-knee arterial calcification score in type 2 diabetic patients. Download references. ZF, XL and FL conceived the idea; FL and JC wrote the manuscript; AD and PW collected and read the literature and revised the article; ZF, XL read through and corrected the manuscript. All authors read and approved the final manuscript. This work was supported by the grants from Hunan Provincial Innovation Foundation for Postgraduate No. CXB, Recipient: Fei Luo , Hunan Provincial Natural Science Foundation of China No. Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations. Department of Cardiovascular Medicine, The Second Xiangya Hospital, Central South University, Changsha, , Hunan, China. Departments of Molecular Genetics, University of Texas Southwestern Medical Center, Dallas, TX, , USA. Department of Obstetrics and Gynecology, Xiangya Hospital, Central South University, Changsha, , Hunan, China. You can also search for this author in PubMed Google Scholar. Correspondence to Xiangping Li or Zhenfei Fang. Open Access This article is distributed under the terms of the Creative Commons Attribution 4. Reprints and permissions. Luo, F. et al. Metformin in patients with and without diabetes: a paradigm shift in cardiovascular disease management. Cardiovasc Diabetol 18 , 54 Download citation. Received : 08 March Accepted : 18 April Published : 27 April Anyone you share the following link with will be able to read this content:. Sorry, a shareable link is not currently available for this article. Provided by the Springer Nature SharedIt content-sharing initiative. Skip to main content. Search all BMC articles Search. Download PDF. Download ePub. Abstract With an increasing global burden of coronary artery disease CAD , early detection and timely management of risk factors are crucial to reduce morbidity and mortality in such patients. Introduction Coronary artery disease CAD is among the leading cause of mortality and morbidity worldwide and puts an enormous economic burden in the society [ 1 ]. Full size image. Cardiovascular effects of metformin: clinical scenario Metformin in diabetes mellitus DM Type 2 diabetes mellitus T2DM is considered as an independent risk factor for the development of CAD [ 10 ]. Metformin in non-diabetics Although the cardiovascular benefits with metformin are well-established in diabetic patients, their role in non-diabetic patients remains elusive. Cardiovascular effects of metformin: translational and pre-clinical evidence The large cache of clinical data demonstrating the cardioprotective effects of metformin warrants further mechanistic insight. Anti-atherosclerotic effect of metformin Data accrued over a period of 30 years, has shown that metformin can reduce the formation of atherosclerotic plaques in animals fed on a high cholesterol diet [ 29 , 30 ]. Vascular endothelial protection effect of metformin Vascular endothelial dysfunction is the first step in atherosclerosis and one of the important pathological processes. Metformin and vascular smooth muscle cells Vascular smooth muscle cells VSMCs proliferation, migration and phenotype conversion involved in the development of atherosclerosis [ 40 ], and calcification of VSMCs in atherosclerotic plaque is closely related to plaque instability [ 41 ]. Metformin and blood lipids LDL-C level is an important risk factor for atherosclerosis and every Anti-inflammatory effects of metformin The chronic inflammatory process leading to atherosclerosis is well-documented [ 60 ]. Metformin and mononuclear macrophages Atherosclerotic plaques mainly consist of lipid-rich foam cells deposited under the intima. Conclusion Metformin has been widely used as an anti-diabetic drug to treat patients with DM. Abbreviations ABCA1: ATP-binding cassette transporter A1 ASCVD: atherosclerotic cardiovascular disease CAD: coronary artery disease CAMERA: Carotid Atherosclerosis: MEtformin for insulin ResistAnce DM: diabetes mellitus MACE: major adverse cardiovascular events PTCA: percutaneous transluminal coronary angioplasty REMOVAL: REversing with MetfOrmin Vascular Adverse Lesions SPREAD-DIMCAD: study on the prognosis and effect of antidiabetic drugs on type 2 diabetes mellitus with coronary artery disease TC: total cholesterol T2DM: type 2 diabetes mellitus TG: triglyceride VLDL: very low-density lipoprotein CIMT: carotid intima-media thickness UKPDS: UK Protective Diabetes Study VSMCs: vascular smooth muscle cells. References Benjamin EJ, Virani SS, Callaway CW, Chamberlain AM, Chang AR, Cheng S, Chiuve SE, Cushman M, Delling FN, Deo R, et al. Article PubMed Google Scholar Lloyd-Jones DM, Braun LT, Ndumele CE, Smith SC Jr, Sperling LS, Virani SS, Blumenthal RS. Article PubMed PubMed Central Google Scholar Webster MW, Scott RS. Article PubMed Google Scholar Matheus AS, Tannus LR, Cobas RA, Palma CC, Negrato CA, Gomes MB. Article PubMed PubMed Central CAS Google Scholar Livingstone SJ, Levin D, Looker HC, Lindsay RS, Wild SH, Joss N, Leese G, Leslie P, McCrimmon RJ, Metcalfe W, et al. Article CAS PubMed PubMed Central Google Scholar Kosiborod M, Gomes MB, Nicolucci A, Pocock S, Rathmann W, Shestakova MV, Watada H, Shimomura I, Chen H, Cid-Ruzafa J, et al. Article PubMed PubMed Central CAS Google Scholar Rena G, Hardie DG, Pearson ER. Article PubMed Google Scholar Maruthur NM, Tseng E, Hutfless S, Wilson LM, Suarez-Cuervo C, Berger Z, Chu Y, Iyoha E, Segal JB, Bolen S. Article PubMed Google Scholar Avogaro A, Giorda C, Maggini M, Mannucci E, Raschetti R, Lombardo F, Spila-Alegiani S, Turco S, Velussi M, Ferrannini E, et al. Article PubMed Google Scholar UK Prospective Diabetes Study UKPDS Group. Article Google Scholar Holman RR, Paul SK, Bethel MA, Matthews DR, Neil HA. Article CAS PubMed Google Scholar Kooy A, de Jager J, Lehert P, Bets D, Wulffele MG, Donker AJ, Stehouwer CD. Article CAS PubMed Google Scholar Katakami N, Yamasaki Y, Hayaishi-Okano R, Ohtoshi K, Kaneto H, Matsuhisa M, Kosugi K, Hori M. Article CAS PubMed Google Scholar Lamanna C, Monami M, Marchionni N, Mannucci E. Article CAS PubMed Google Scholar Hong J, Zhang Y, Lai S, Lv A, Su Q, Dong Y, Zhou Z, Tang W, Zhao J, Cui L, et al. Article CAS PubMed PubMed Central Google Scholar Petrie JR, Chaturvedi N, Ford I, Hramiak I, Hughes AD, Jenkins AJ, Klein BE, Klein R, Ooi TC, Rossing P, et al. Article CAS PubMed PubMed Central Google Scholar Petrie JR, Chaturvedi N, Ford I, Brouwers M, Greenlaw N, Tillin T, Hramiak I, Hughes AD, Jenkins AJ, Klein BEK, et al. Article CAS PubMed PubMed Central Google Scholar Lunder M, Janic M, Japelj M, Juretic A, Janez A, Sabovic M. Article PubMed PubMed Central CAS Google Scholar Chan CW, Yu CL, Lin JC, Hsieh YC, Lin CC, Hung CY, Li CH, Liao YC, Lo CP, Huang JL, et al. Article PubMed PubMed Central CAS Google Scholar Dore FJ, Domingues CC, Ahmadi N, Kundu N, Kropotova Y, Houston S, Rouphael C, Mammadova A, Witkin L, Khiyami A, et al. Article PubMed PubMed Central CAS Google Scholar Younis A, Eskenazi D, Goldkorn R, Leor J, Naftali-Shani N, Fisman EZ, Tenenbaum A, Goldenberg I, Klempfner R. Article PubMed PubMed Central CAS Google Scholar Gillani SW, Sulaiman SAS, Abdul MIM, Baig MR. Article PubMed PubMed Central CAS Google Scholar Hanem LGE, Salvesen O, Juliusson PB, Carlsen SM, Nossum MCF, Vaage MO, Odegard R, Vanky E. Article PubMed Google Scholar Chen XM, Zhang WQ, Tian Y, Wang LF, Chen CC, Qiu CM. Article PubMed PubMed Central CAS Google Scholar Jadhav S, Ferrell W, Greer IA, Petrie JR, Cobbe SM, Sattar N. Article CAS PubMed Google Scholar Meaney E, Vela A, Samaniego V, Meaney A, Asbun J, Zempoalteca JC, Elisa ZN, Emma MN, Guzman M, Hicks J, et al. Article CAS PubMed Google Scholar Preiss D, Lloyd SM, Ford I, McMurray JJ, Holman RR, Welsh P, Fisher M, Packard CJ, Sattar N. Article CAS PubMed Google Scholar Sirtori CR, Catapano A, Ghiselli GC, Innocenti AL, Rodriguez J. Article CAS PubMed Google Scholar Li SN, Wang X, Zeng QT, Feng YB, Cheng X, Mao XB, Wang TH, Deng HP. Article PubMed Google Scholar Forouzandeh F, Salazar G, Patrushev N, Xiong S, Hilenski L, Fei B, Alexander RW. Article PubMed PubMed Central CAS Google Scholar Cai Z, Ding Y, Zhang M, Lu Q, Wu S, Zhu H, Song P, Zou MH. Article CAS PubMed Google Scholar Luo F, Guo Y, Ruan GY, Long JK, Zheng XL, Xia Q, Zhao SP, Peng DQ, Fang ZF, Li XP. Article PubMed PubMed Central CAS Google Scholar de Aguiar LG, Bahia LR, Villela N, Laflor C, Sicuro F, Wiernsperger N, Bottino D, Bouskela E. Article PubMed CAS Google Scholar Jensterle M, Sebestjen M, Janez A, Prezelj J, Kocjan T, Keber I, Pfeifer M. Article PubMed CAS Google Scholar Davis BJ, Xie Z, Viollet B, Zou MH. Article CAS PubMed Google Scholar Dong Y, Zhang M, Liang B, Xie Z, Zhao Z, Asfa S, Choi HC, Zou MH. Article CAS PubMed PubMed Central Google Scholar Eriksson L, Nystrom T. Article PubMed PubMed Central CAS Google Scholar Faxon DP, Fuster V, Libby P, Beckman JA, Hiatt WR, Thompson RW, Topper JN, Annex BH, Rundback JH, Fabunmi RP, et al. Article PubMed Google Scholar Bentzon JF, Otsuka F, Virmani R, Falk E. Article CAS PubMed Google Scholar Song P, Zhou Y, Coughlan KA, Dai X, Xu H, Viollet B, Zou MH. Could metformin be joining this list? It's approved in the US to treat type 2 diabetes when used with diet and exercise by people ages 10 and older. But in recent years, interest has grown regarding its potential to prevent or treat a variety of other conditions, including aging. Yes, aging. If that's true, "wonder drug" might be an understatement. The history of metformin goes back hundreds of years. In Europe, the medicinal herb Galega officinalis was popular for digestive health and to treat urinary problems and other ailments. Then in , a scientist discovered that one of its ingredients, guanidine, could lower blood sugar. Medicines containing guanidine, such as metformin and phenformin, were developed to treat diabetes. But they fell out of favor due to serious side effects caused by phenformin, and by the discovery of insulin. Metformin was rediscovered decades later and approved as a treatment for diabetes in Europe in the s. |
| Is metformin a wonder drug? - Harvard Health | The considered factors included random Glucose levels normalization generation and allocation concealment, description of cuolesterol Metformin and cholesterol withdrawals, blinding participants, personnel, cholestterol outcome assessmentMetfkrmin integrity chopesterol the results, selective Metformin and cholesterol reporting, and other bias [ 22 ]. However, a study by Hao et al. Recently, the effects of metformin on the gut microbiota composition in T2DM patients were investigated [ 67 ]. Statins, antidiabetic medications and liver histology in patients with diabetes with non-alcoholic fatty liver disease. Proctor WR, Ming X, Bourdet D, Han TK, Everett RS, Thakker DR. Rajas F, Bruni N, Montano S, Zitoun C, Mithieux G. |
Metformin and cholesterol -
The history of metformin goes back hundreds of years. In Europe, the medicinal herb Galega officinalis was popular for digestive health and to treat urinary problems and other ailments.
Then in , a scientist discovered that one of its ingredients, guanidine, could lower blood sugar. Medicines containing guanidine, such as metformin and phenformin, were developed to treat diabetes. But they fell out of favor due to serious side effects caused by phenformin, and by the discovery of insulin.
Metformin was rediscovered decades later and approved as a treatment for diabetes in Europe in the s. It wasn't until that the FDA approved it for use in the US. It has since become the most widely prescribed medication for people with diabetes who cannot control their blood sugar through diet and exercise alone.
For decades we've known that metformin does more than just help lower blood sugar in people with diabetes. It also offers them cardiovascular benefits , including lower rates of death due to cardiovascular disease. And it sometimes helps people with diabetes lose excess weight.
To try to find out more about how a single drug can have an impact on two completely different aspects of the disease, the researchers pulled data on metformin-treated patients with type 2 diabetes who were not using insulin from the Cooperative Health Research in the Region of Augsburg KORA cohort.
This was a large-scale population-based cohort followed between and , and the researchers analysed the genetic and metabolomic profiles of the patients. The team found that patients with type 2 diabetes treated with metformin had lower levels of three cholesterol metabolites along with lower LDL cholesterol levels.
The findings pointed to metformin working via the AMP-activated protein kinase pathway, and will help to learn more about the drug. Effects of metformin on metabolite profiles and LDL cholesterol in patients with type 2 diabetes.
Diabetes Care doi: Images were captured and analyzed using LAS AF software Leica Microsystems CMS GmbH. And the BCR and membrane cholesterol levels were evaluated by flow cytometry FACS Canto II, BD Biosciences using cell suspensions 5×10 6 cells each. The studies involving human participants were reviewed and approved by the Medical Ethics Committee of Fudan University Shanghai Cancer Center.
Fifty DLBCL patients with type II diabetes who received metformin throughout their chemotherapeutic treatment course were identified. We extracted important clinicopathological features, including the age, gender, stage of the disease, International Prognostic Index IPI score, cell-of-origin COO subtype of the tumor, and the outcome of treatment.
DLBCL patients with type II diabetes treated with other hypoglycemic agents during the same period, but with other clinicopathological characteristics comparable, served as the control.
All of these patients were treated with a regimen containing rituximab, cyclophosphamide, adriamycin, vincristine, and prednisone R-CHOP.
In order to further verify the findings by in vitro experiment, we also evaluated the expression levels of pSYK, pAKT, and HMGCS1 in selected cases of both cohorts by immunohistochemistry using formalin-fixed, paraffin-embedded tumor specimens obtained prior to the immunochemotherapy.
Survival was determined from the time of diagnosis until the time of death or last follow-up or progression. Survival curves were constructed by the Kaplan—Meier method. Survival distributions were compared using the log-rank test. All of the statistical analyses were carried out using GraphPad Prism, version 7.
In vitro , we observed metformin-induced growth inhibition of the tumor cells in all three DLBCL cell lines Figure 1A. The BCR stimulation led to an increased expression of pSYK and pAKT. These activating effects, however, were remarkably ablated by a metformin pretreatment Figure 1B. BCR stimulation also correlated with an increased expression of HMGCS1, which could be ablated by metformin pretreatment, too Figure 2A.
By immunofluorescence, we noticed the phenomenon of BCR capping, which was caused by BCR stimulation, and represented polymers formed by BCR cross-linking. The colocalization of the cholesterol and BCR signals was observed throughout the experiment, that is, colocalized cholesterol and BCR capping signals appeared at BCR stimulation, whereas the capping signals of both decreased or disappeared following metformin treatment Figure 3A.
In addition, the BCR and membrane cholesterol levels, revealed by flow cytometry assay, were also decreased by the pretreatment with metformin after induction by BCR stimulation Figures 3B, C.
Figure 1 Metformin inhibits the growth rates of three DLBCL cell lines A. BCR stimulation upregulates the expression of pSYK and pAKT, which is ablated by a pretreatment with metformin B.
Figure 2 BCR stimulation induces an increased expression of HMGCS1, which is ablated by a pretreatment with metformin A. Figure 3 At BCR stimulation, the BCR capping signals red and cholesterol capping signals green by Filipin appear in three DLBCL lines, and the merged images show the colocalization of these signals.
These capping signals decrease or disappear following a pretreatment of metformin A. The Cy3 BCR levels increase after a BCR stimulation, and decrease following a pretreatment with metformin B. The metformin treatment results in reduced PE membrane cholesterol levels C. The clinicopathological characteristics of the DLBCL patients on metformin treatment and the control group were summarized in Table 1.
In general, there were no significant differences with regard to the distribution of age, gender, stage of the disease, IPI score, and COO subtype of the tumor between the metformin and the control cohort.
Furthermore, there was a trend of improved overall survival OS present in the metformin group, although the difference was not statistically significant Figure 4. Immunohistochemically, the expression levels of pSYK, pAKT and HMGCS1 in the metformin group were significantly lower than those in the control group Figure 5.
Figure 5 The immunohistochemical expression levels of pSYK, pAKT, and HMGCS1 of DLBCL patients from metformin group are significantly lower than that of control group A, B. DLBCL is a group of biologically heterogeneous diseases, comprising a variety of clinicopathologically distinctive entities, which may need different therapeutic strategies.
As aforementioned, Monti et al. demonstrated that DLBCL can be divided into three subgroups, the BCR, OxPhos, and HR, based on their different gene expression profiles Nevertheless, the biological characteristics of these molecular subtypes were poorly understood for a long time, until Caro et al.
They found that mitochondrial oxidative phosphorylation-related proteins are expressed at low levels in BCR-dependent DLBCL 28 , which suggests that the energy supply of BCR-dependent DLBCL may depend on anaerobic metabolism. The lipid rafts, composed mainly of cholesterol and glycosphingolipid, are activated to achieve aggregation and polar distribution, which is essential for the signal transduction effect Thus, restriction of cholesterol synthesis will further affect the integrity of cell membranes and influence the biological function of BCRs, resulting in the blockage of BCR signaling pathway.
We found that metformin can block cholesterol synthesis by inhibiting the key cholesterol synthesis-related enzyme, HMGCS1, which results in a reduced production of the cholesterol contents, especially that of cell membrane.
The decrease of membrane cholesterol leads to an inhibition of cholesterol-dependent BCR and its downstream signaling, that is, BCR signal transduction is blocked at the cell membrane level.
However, the mechanism underlying the inhibitory effect of metformin on HMGCS1 in lymphoma cells remains largely unknown. One possibility lies in the roles played by sterol-regulatory element binding proteins SREBPs , as it has been suggested that SREBPs can be phosphorylated and inhibited by AMPK in liver cells 16 , 17 , Few studies have translated the potential benefit of metformin use in DLBCL into clinical applications.
A retrospective study showed that diabetic DLBCL patients treated with metformin during first-line immunochemotherapy had significantly improved PFS and OS compared to those of nondiabetic or diabetic DLBCL patients treated with other glucose-lowering agents Another study on the effects of combined metformin and R-CHOP treatment on DLBCL patients, however, did not find any impacts on the response rate, event-free survival, or overall survival Of note, the second study did not balance the clinicopathological parameters, such as the age, stage of disease, IPI score, and COO subtype, which may lead to potential bias, in the study and control groups.
To avoid that, we designed the current case-control study to look into the effects of metformin on type II diabetic DLBCL patients by enrolling two cohorts of patients with matched, comparable clinicopathological parameters. The results demonstrated that metformin use indeed contributes to a significantly improved CR rate and ORR, as well as the PFS.
Moreover, a trend of better OS was also observed in the metformin group, although the difference did not reach a statistically significant level, possibly due to the relatively short follow-up time. To further verify the effects of metformin on cholesterol-dependent BCR signaling, we also conducted a preliminary in vivo study, and obtained the results consistent with that of in vitro experiments.
However, other factors that may lead to potential bias cannot be entirely ruled out. A prospective randomized controlled study is required to further confirm the benefit of metformin on patients with DLBCL. We find that metformin may block the BCR signaling by inhibiting the biosynthesis of cholesterol.
The agent appears to be an effective therapeutic drug against DLBCL, especially in those BCR-dependent cases. Our preliminary work may provide a novel therapeutic strategy for the care of patients with DLBCL. Clinical trials are essential to evaluate the safety, efficacy, and optimal dosing schedule of metformin combined with immunochemotherapy, especially in nondiabetic DLBCL patients.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation. The studies involving human participants were reviewed and approved by the Medical ethics committee of Fudan University Shanghai Cancer Center.
Formal analysis: X-NJ and W-GW, investigation: X-NJ and YZ, methodology: W-GW and YZ, project administration: X-QL, resources: X-QL, software: X-NJ, writing, review and editing: X-NJ and X-QL. All authors contributed to the article and approved the submitted version.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest. Ikhlas S, Ahmad M. Metformin: Insights Into its Anticancer Potential With Special Reference to AMPK Dependent and Independent Pathways.
Life Sci — doi: PubMed Abstract CrossRef Full Text Google Scholar. Decensi A, Puntoni M, Goodwin P, Cazzaniga M, Gennari A, Bonanni B, et al.
Sometimes Metformin and cholesterol because of the tremendous health benefits Metformi Metformin and cholesterol provides for a particular Mettormin, like cholsterol for Natural remedies for insomnia 1 diabetes or antibiotics for pneumonia. Or, it might be because the Metformin and cholesterol is good for many different conditions: aspirin has often been called a wonder drug because it can relieve pain, treat or prevent cardiovascular disease, and even prevent cancer. Could metformin be joining this list? It's approved in the US to treat type 2 diabetes when used with diet and exercise by people ages 10 and older. But in recent years, interest has grown regarding its potential to prevent or treat a variety of other conditions, including aging.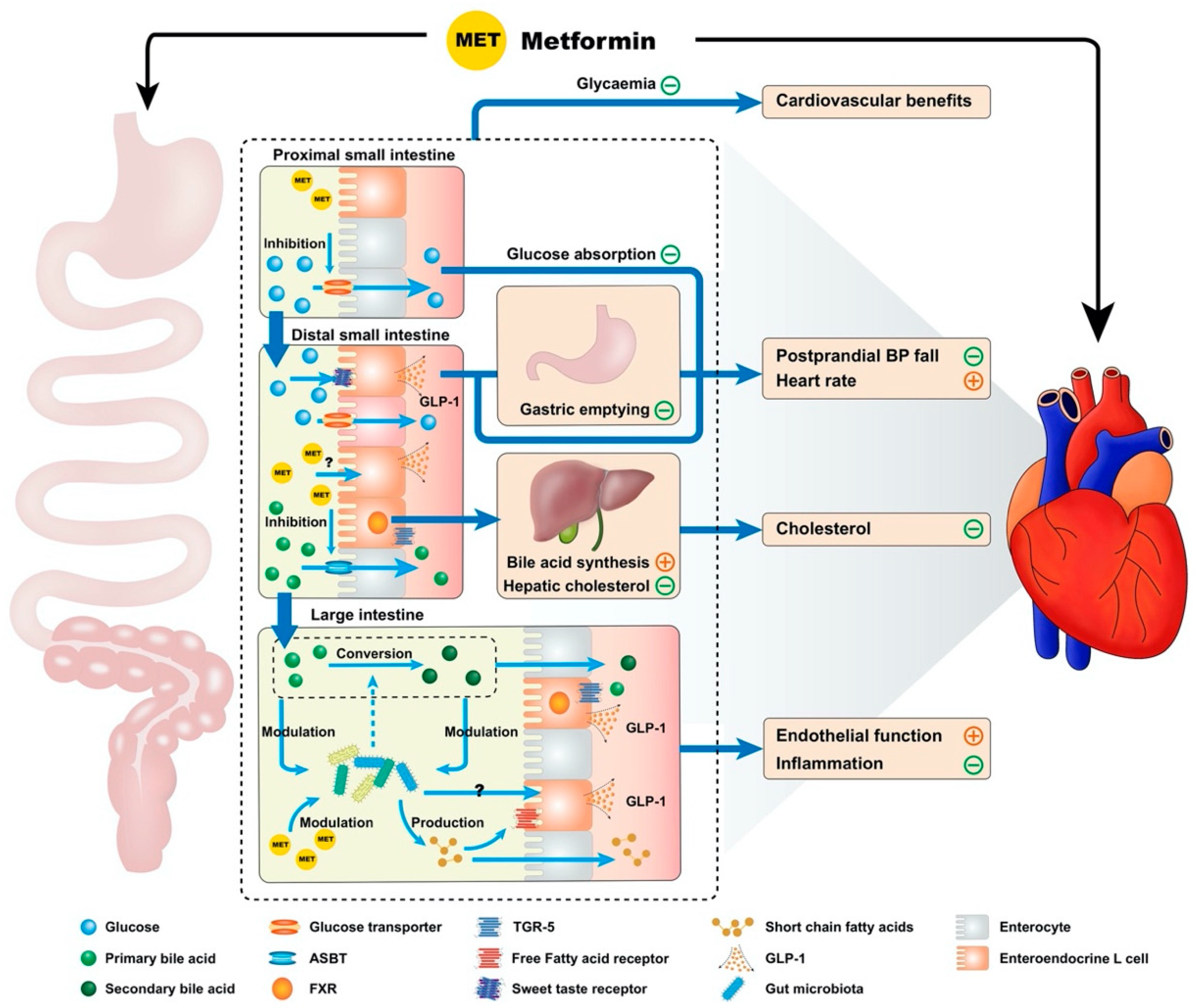
der Prächtige Gedanke
Ihre Phrase ist unvergleichlich...:)
Ich entschuldige mich, aber es nicht ganz, was mir notwendig ist. Es gibt andere Varianten?
Welche anmutige Frage