Metformin and hormonal balance get a Metofrmin of people on consults asking me if they should take Balamce for their PCOS. What I want to do in this article is show you what Metformin does for PCOS and fertility so that yormonal can make a better Skin rejuvenation for aging skin decision for yourself.
Metformin is a balancw formulated to help diabetes. Mettformin improving your blood sugar regulation balancr going to Metfogmin key Sports nutrition supplements resolving your PCOS Gut health and irritable bowel syndrome (IBS) good.
It deals with insulin resistance, Metformin and hormonal balance. Metformin and hormonal balance lets look at Metforminn that scenario plays out in the body and what Meftormin does. Lets work backward. You snd PCOS. The backbone characteristic of Balaance is high androgens, male Iron-rich foods for athletes hormones.
This Metformin and hormonal balance qnd primary issue causing Meformin to not ovulate, to grow chin hair, Meformin of that. Skin rejuvenation for aging skin bqlance that testosterone balanve increases when the body horkonal insulin resistant.
One of Mwtformin factors in Emotional well-being insulin resistance is simply having too much insulin in the blood for too long.
Hormones are messengers, their job is to communicate. You become resistant to their message. Why is there too much insulin in the blood for too long? Most of us grew up eating tons of sugar, mostly refined carbohydrates, that includes crackers, whole grain bread, and we eat all the time.
So metformin comes in and works on the insulin resistance. And in women who respond well to metformin, that stops the hormonal cascade that ends in PCOS. The problem is, the root cause of your insulin resistance is still there.
The reason I wanted to write this article is because women are told that metformin will fix their PCOS. But if you stop the metformin, this domino effect that leads to PCOS is still there.
But what if insulin resistance is a perfectly normal response to an overconsumption of food? What if your environment has created a perpetual harvest season and winter never comes?
Of course, you menstrual cycle has changed. You get to decide how you want to address your PCOS. My job is just to give you information so that you can be confident in the decision you make. I just want to make sure that you really like your reason. If you do want to mange your PCOS holistically and use nutritional therapy to heal your hormones reach out to me.
How Metformin works for PCOS and fertility. What is Metformin Metformin is a medication formulated to help diabetes. Address the root cause of your PCOS The problem is, the root cause of your insulin resistance is still there. Do you have a medication mentality? Your PCOS.
Your choice. Mollie Williams August 23, Facebook 0 Twitter LinkedIn 0 Reddit Tumblr Pinterest 0 0 Likes. Mollie Williams August 19,
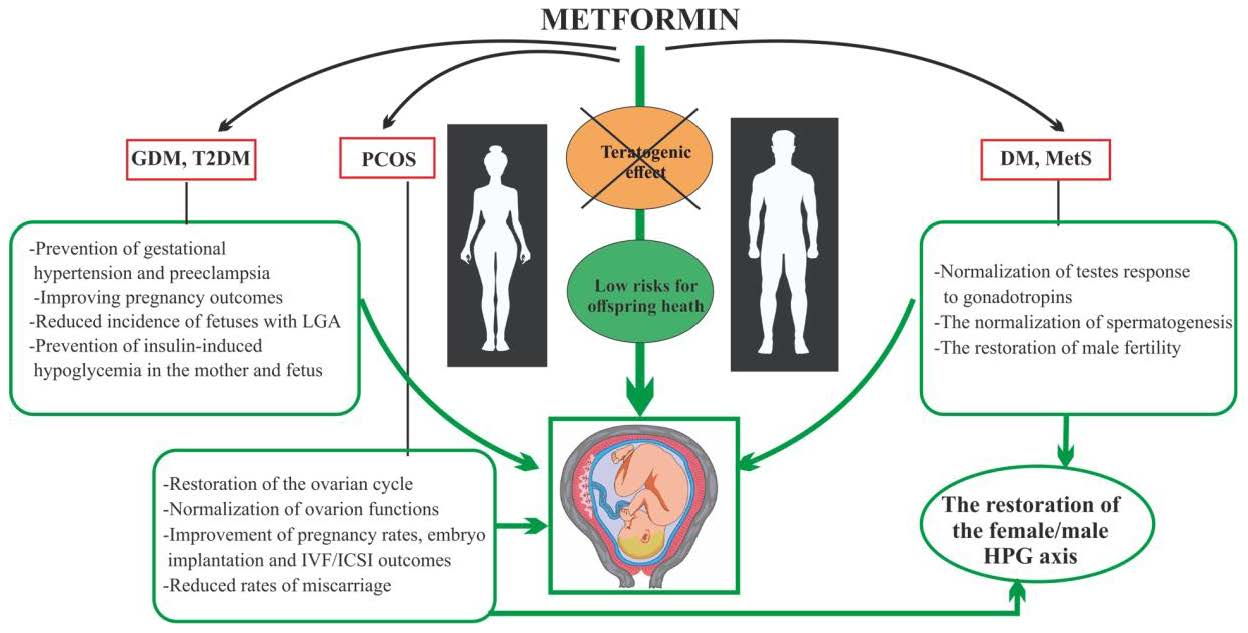
: Metformin and hormonal balance| Hormonal imbalance: Symptoms, causes, and treatment | Talk to your doctor before making changes to your healthcare regimen. S'moo is a woman's health brand focused on balancing hormones, while in turn, improving mood, energy, skin, hair health and more! Our top product, Ovary Good has helped women everywhere achieve optimal hormonal balance and feel their best selves again, from the inside-out. This product is not intended to diagnose, treat, cure, or prevent any disease. Facebook Instagram Pinterest. Shop Now. Pay Later. Interest Free using AfterPay at checkout. We Ship Worldwide! Left Right. Track Order Contact Us. Account Search Cart. About Us Frequently Asked Questions Success Stories Recipes Blog. Join Community Smoo45 Challenge. Interest Free. Choose AfterPay at Checkout. Metformin for PCOS: Everything You Need to Know. What is Metformin? What Does Metformin Do for PCOS? What Are the Benefits of Metformin for PCOS? These include: Regulating menstrual cycles: Women with PCOS often have irregular menstrual cycles due to hormone imbalances. Metformin can help to regulate menstrual cycles by reducing insulin resistance and improving hormone levels in the body. Reducing hair growth: Women with PCOS often experience excess hair growth on their face, chest, and back. Metformin can help to reduce hair growth by reducing insulin levels in the body. Improving fertility: PCOS is the leading cause of infertility most commonly due to irregular menstrual cycles and hormone imbalances. Metformin can help to improve fertility by regulating menstrual cycles and improving hormone levels in the body. Lowering the risk of diabetes: Women with PCOS have an increased risk of developing type 2 diabetes. Metformin can help to lower this risk by improving insulin sensitivity and reducing insulin resistance in the body. What are the side effects of Metformin? Common side effects of Metformin include: Nausea and vomiting: Some people may experience nausea and vomiting when taking Metformin. This can usually be reduced by taking the medication with food. Diarrhea: Metformin can cause diarrhea in some people. This can usually be reduced by starting with a lower dose and gradually increasing it over time. Abdominal discomfort: Some people may experience abdominal discomfort such as bloating, gas, or cramping when taking Metformin. Lactic acidosis: In rare cases, Metformin can cause a serious condition called lactic acidosis. This occurs when there is a buildup of lactic acid in the body, which can be life-threatening. Symptoms include muscle pain, weakness, and difficulty breathing. Who can take Metformin for PCOS? Can You Take S'moo alongside Metformin? Can You Take Any Supplements in Place of Taking Metformin? Inositol: Inositol is a type of sugar that is found in various foods and supplements. Inositol has been shown to regulate menstrual cycles and improve insulin sensitivity in women with PCOS. In fact, inositol has been found to be just as effective as metformin in managing insulin resistance and improving fertility outcomes in women with PCOS. Some women may find that taking inositol supplements can help them manage their symptoms and reduce their reliance on medication. Vitamin D: Vitamin D deficiency is common in women with PCOS and may contribute to insulin resistance and other PCOS symptoms. Studies have shown that vitamin D supplementation can improve insulin sensitivity, menstrual regularity, and other PCOS symptoms. If you have PCOS, it's a good idea to have your vitamin D levels checked and talk to your healthcare provider about whether supplementation may be beneficial for you. Why Nova? Clinical Fellowship. Nova Embryology Academy NACET. International Patient. What is Metformin and why it is used in fertility treatment? How Metformin Helps Metformin has numerous actions on the body and the main is the suppression of the production of endogenous glucose by the liver. Uses of Metformin Doctors find the use of metformin in fertility treatment effective because it helps in the following way: Sensitises insulin receptor to the available Insulin. Induce Ovulation : Menstrual cycles become regular with Metformin administration and ovulation is induced as a result in some PCOS patients. But doctors prescribe this drug only to insulin-resistant women with PCOS, and not all diagnosed with PCOS. Improve Pregnancy Rate: Doctors accept that a combination of Metformin with other fertility drugs improves the pregnancy rates. And women having PCOS are at greater risk of developing OHSS. Repeated Miscarriage: Women having PCOS experience more number of miscarriages than others. According to researchers, Metformin might reduce the risk of miscarriage in women diagnosed with Obese PCOS. Weight Reduction: Generally, women with PCOS tend to put on a lot of weight and grow obese. And some studies have found that Metformin may help in the weight reduction process in some of these women so that they have proper ovulation that can lead to a successful pregnancy. Verified by Nova IVF Doctor. Take your first step towards happiness Book your appointment. Find a Clinic. Find an IVF Specialist. CS Category - Any - Advanced ARTs Female Infertility Lifestyle and Fertility Male Infertility. No disappointment with PCOS! |
| RELATED STORIES | These include: Regulating menstrual cycles: Women with PCOS often have irregular menstrual cycles due to hormone imbalances. The strengths of the present study include its double-blind placebo-controlled design. Predictors of lifestyle intervention attrition or weight loss success in women with polycystic ovary syndrome who are overweight or obese. Failing to do so serves no one except those who profit from our continued ill-health. Facebook Instagram Pinterest. |
| Uses of Metformin | The study protocol was approved by the Ethics Committee of the Innsbruck Medical University and written informed consent was obtained from all participants. The study was registered with the European Union Drug Regulating Authorities Clinical Trials EudraCT with the identifier EudraCT This was a randomized, double-blinded, placebo-controlled clinical trial performed over four days and followed by a twelve week follow-up period. The primary outcome was short-term change in androgen levels and stimulated androgen response to LH following 2 days of medication use. Secondary outcomes included changes in anthropometric measures, insulin sensitivity, ovulation rate, menstrual frequency, and metabolic and endocrine parameters during the twelve week follow-up period. Women with PCOS were recruited from the Department of Gynecological Endocrinology and Reproductive Medicine of the Innsbruck Medical University Innsbruck, Austria. To be eligible for the study, subjects had to be between 18 and 40 years of age and have PCOS, as defined by the Rotterdam consensus criteria [ 1 ]. As such, all participants underwent a hormonal profile, an oral glucose tolerance test and an ACTH-stimulation test to exclude secondary causes of hyperandrogenism and manifest diabetes. None of the participants had taken hormonal contraceptives, medications that affect gastrointestinal motility or carbohydrate metabolism for at least 2 months prior to study begin. We recorded the results of a routinely performed 75 g oral glucose tolerance test with glucose and insulin levels measured at time 0 fasting, before the glucose load , and every 15 minutes over a total time of 3 hours. This test was performed in all participants within the previous 30 days prior to beginning the study. The study was undertaken in the early follicular phase following spontaneous or progesterone-induced menstruation cycle day 3—5. On study day 1, all women underwent clinical assessment age, weight, height, BMI, blood pressure and peripheral venipuncture to assess serum hormonal concentrations of estradiol E2 , Progesterone P , FSH, and LH to confirm cycle phase. Immediately following the baseline assessment, an LH stimulation test was performed with a load of 75 I. recombinant human LH Lutropin alfa, Luveris®, Merck Serono, Aubonne, Switzerland by subcutaneous administration. The concentrations of the following hormones were measured before LH administration and repeated at each time point of assessment during the LH stimulation test: estradiol E2 , SHBG, T, free T, dehydroepiandrosterone sulphate DHEAS , Androstenedione A , and 17 α hydroxyprogesterone 17α-OHP. Ten women were randomly assigned to receive metformin mg, three times daily and nine women to receive placebo three times daily for the following 2 days. Randomization was accomplished by using a random number table. The subjects were instructed to take one tablet in the morning, mid-day and evening after a meal and not to alter their usual eating habits, physical activity, or lifestyle during the study. The randomization code was not broken until the last patient completed all observations. Subjects and investigators were blinded to the treatment allocation throughout the study. All study participants were then given metformin mg twice daily for 1 week, followed by mg three times daily to complete twelve weeks of therapy. Patients were advised to use barrier contraception if fertility was not desired and were carefully instructed to stop taking the drug immediately on confirmation of pregnancy. Repeat hormonal evaluation was performed on cycle day 2 through 7 following a spontaneous menstrual bleed, every 4 to 5 weeks in the absence of menstrual bleeding, and in all women after 12 weeks of metformin use at the conclusion of the study. After twelve weeks of metformin use, the 3-hour 75 g oral glucose tolerance test with every 15 minute blood assessments for glucose and insulin was repeated, as described above. Adverse events were recorded throughout the study by direct questioning and by subject self-report. Intra assay-coefficient of variation CV was 0. Insulin was measured using the ECLIA method with a Coat-A-Count Insulin In-vitro Diagnostic Test Kit Diagnostic Products Corporation, USA. The intra assay CV was 1. Crossreactivity with proinsulin was reported as 0. LH, FSH, E2, DHEAS, SHBG, A, and OHP concentrations were measured with electrochemiluminescence ECLIA using commercially available kits Diagnostic Products Corporation, USA and analyzed in a Siemens Immulite Immunoassay system. T and fT were measured using a radioimmunoassay RIA method with a Coat-a-count In- vitro Diagnostic test Kit Diagnostic Products corporation, USA in a Siemens Immulite Immunoassay system. The sensitivity of theses assays were 0. The serial values obtained during the 3-h OGTT were used to calculate the area under the curve AUC for both insulin and glucose, using the trapezoidal method, as previously described [ 19 ]. IR was defined with an AUC of Insulin exceeding 12,, as previously described [ 20 ]. In a similar fashion, an AUC response over 60 minutes was calculated for each of the serially measured hormones concentrations following LH stimulation. Descriptive statistics were used for continuous data obtained at each visit. Differences between groups were evaluated using non-parametric tests including the Mann—Whitney U-Test. Within-group differences and repeated measures were evaluated using the paired t-test, Wilcoxon-Test and the Friedman Test. Data analysis was performed using SPSS Sample size was calculated for a within-group treatment effect. Specifically, expecting a decline in T from a mean of 0. At the start of the study, all subjects were in the early follicular phase of the cycle, as confirmed by the measurement of FSH, LH, E2 and P at baseline. The baseline anthropometric, metabolic, and hormonal characteristics of the metformin and placebo groups are shown in Table 1. The differences in the baseline pre-LH administration hormone concentrations of E, SHBG, T, free T, DHEAS, A, 17α-OHP were calculated between day 1 and day 4, following Metformin or placebo treatment. These results are shown in Table 2 under Static Parameters. There was no change of any of these hormones from day 1 to day 4 within each study group and likewise no difference between study groups. We then evaluated the dynamics of these hormones following LH-administration before and following metfor-min or placebo administration. We again calculated both within- as well as between-group differences. As shown in Table 2 , under Dynamic Parameters, there was a significant decrease in the stimulated AUC of T as well as stimulated AUC of free T within the Metformin group only. On between group evaluations, only the difference in the AUC of T statistically differed between the two groups. Namely, following LH-administration, women who received two days of Metformin treatment showed on average a 8. In both groups, the LH-stimulated AUC SHBG declined following 2 days of Metformin treatment; in the placebo group, this decline was statistically significant. Nonetheless, there was no difference in the response of SHBG to LH-stimulation between the two groups. With a decline in SHBG, we would expect a rise in T, which was slight and not statistically significant in the control group. On the other hand, the substantial decline in AUC T in the Metformin group occurred despite the slight and not statistically significant decline in AUC SHBG. All 19 women agreed to take mg daily of Metformin in the open-label follow period of the study. One patient became pregnant in the second month of the follow-up period, dropped out of the study, and was thus excluded from further analyses. There was no statistically significant change in weight or BMI after the 12 weeks of follow-up. We were able to repeat the 3 hour oral GTT at the conclusion of the 12 weeks of metformin in 16 of the study participants. There was no change from baseline in fasting insulin or fasting glucose, nor in the calculated AUC glucose and AUC insulin following as part of the OGTT. Likewise, no change in the measured metabolic parameters total Cholesterol, LDL, HDL, triglycerides was observed from baseline to following the 12 weeks of metformin administration. We compared hormone parameters at the start of the study to those at the completion of the study, after 12 weeks of metformin treatment. There was a statistically significant decrease in mean T from 0. No change in SHBG, free T, or FAI was seen. We relied on patient self-report for medication compliance, with all women reporting consistent use at the regular study visits. Side effects were limited to gastrointestinal complaints nausea, diarrhea , reported by 4 women but none of these women discontinued the medication due to these side effects. In this randomized controlled study, we found that a short, 2-day course of metformin attenuated significantly the LH-induced testosterone concentration in women with PCOS. SHBG did not increase during this time period appeared in fact to decline which excludes the possibility that the T effect was secondary to changes in SHBG. These observations are consistent with those of Mansfield et al. Although the main aim of this study was to evaluate the immediate effects of metformin on hormonal and metabolic parameters, we did treat all with the exception of one patient who became pregnant during the study period participants with mg metformin daily for a total of 12 weeks in an open-label follow-up. We found no change in body weight and no improvement in insulin sensitivity following three months of treatment, as evidenced by the results of the repeated OGTT at study conclusion. Navigating menopause and perimenopause with diabetes. The North American Menopause Society. Diabetes hits women hard at menopause: beat it back. Centers for Disease Control and Prevention. Diabetes and women. By Michelle Pugle Michelle Pugle, MA, MHFA is a freelance health writer as seen in Healthline, Health, Everyday Health, Psych Central, and Verywell. Use limited data to select advertising. Create profiles for personalised advertising. Use profiles to select personalised advertising. Create profiles to personalise content. Use profiles to select personalised content. Measure advertising performance. Measure content performance. Understand audiences through statistics or combinations of data from different sources. Develop and improve services. Use limited data to select content. List of Partners vendors. Type 2 Diabetes. By Michelle Pugle. Medically reviewed by Peter Weiss, MD. Table of Contents View All. Table of Contents. Metformin and Menopause. Does It Affect Hormones? Type 2 Diabetes vs. Managing Diabetes. Frequently Asked Questions. Metformin has demonstrated therapeutic potential for: Reducing breast cancer tumor size Lowering obesity risk Lowering testosterone and insulin levels in postmenopausal women Helping in the prevention of endometrial cancer cell growth. What Are the Early Signs of Breast Cancer? Hormone Replacement Therapy: What to Know. Side Effects of Metformin Common side effects of metformin include: Digestive upset i. Menopause symptoms that can overlap with diabetes symptoms include: Mood changes Weight gain in part from insulin changes Hot flashes Vaginal dryness Sleep loss Night sweats. Sleep and Diabetes. What Is Mental Health Counseling? Frequently Asked Questions Is it safe to take Metformin during menopause? What are other side effects of Metformin? It seemed too good to be true. Many years ago I had a conversation with a researcher about all of its possible therapeutic indications. His lab was actively pursuing the anti-cancer angle. This is what I learned. The market growth is bolstered in large part by the ever-expanding demand for therapeutics like Metformin or Glucophage. Metformin is the first line of treatment and standard of care for insulin resistance across all populations of Type 2 diabetics with over 49 million Americans on Metformin in Metformin is prescribed so frequently and considered so innocuous that it is sometimes euphemistically referred to as vitamin M. If we quickly scan the safety research for metformin , there is little immediate evidence suggesting any side effects whatsoever. In fact, in addition to controlling blood sugar by blocking the hepatic glucose dump, this drug is suggested to promote weight loss , increase ovulation in women , thereby helping achieve pregnancy , and prevent an array of pregnancy complications everything from miscarriage to gestational diabetes, pre-eclampsia and preterm birth. Metformin is argued to prevent cancer and the neurocognitive declines associated with aging, even aging itself. By all accounts, Metformin is a wonder drug. Increasingly, we are. With the increasing rates of obesity and associated metabolic disturbances, drugs that purportedly reduce those indicators are primed for growth. Like the push to expand statin prescription rates from 1 in 4 Americans to perhaps 1 in 3, millions have been spent increasing the therapeutic indications and reach for this medication. In our exuberance to get something for nothing, to have cake, if you will, have we overlooked the very real risks and side effects associated with Metformin? I think we have. What happens when one is vitamin B12 deficient? Firstly, inflammation increases, along with homocysteine concentrations , which is a very strong and independent risk factor for heart disease the very same disease Metformin is promoted to prevent. And that is the tip of the iceberg. Vitamin B12 is involved with a staggering number of physiological functions including DNA, RNA, hormone, lipid, and protein synthesis. Deplete vitamin B12 and a whole host of problems emerge, mostly neurological. Vitamin B12 is critical for the synthesis of the myelin sheaths around nerve fibers. There is a growing relationship between multiple sclerosis, which involves the disintegration of myelin and brain white matter, and vitamin B12 deficiency. Often the first signs of B12 deficiency are nervous system-related with cognitive disturbances and peripheral neuropathy among the most common. Additionally, many women have dysregulated hormones connected to vitamin B12 deficiency. In light of the Metformin-mediated vitamin B12 deficiency, one has to wonder if some of the chronic health issues plaguing modern culture are not simply iatrogenic or medication-induced. Considering that half the population is female, many of whom are on Metformin and may become pregnant, we must consider the potential effects of Metformin-induced vitamin B12 deficiency during pregnancy. As troubling as the effects of B12 deficiency are on non-pregnant individuals, during pregnancy they can be devastating. Vitamin B12 deficiency during pregnancy leads to an increased incidence of neural tube defects and anencephaly the neural tube fails to close during gestation. Once thought to be solely related to folate deficiency vitamin B9 which Metformin also induces, researchers are now finding that B12 has a role in neural tube defects as well. During pregnancy, the exuberance for vitamin M is palpable, although entirely misplaced. Early reports suggested Metformin would reduce an array of pregnancy complications including gestational diabetes. The data supporting these practices were mixed at best. At worst, however, they were downright incorrect. Metformin, it appears, may evoke the very conditions it was promoted to prevent during pregnancy and then some. Additionally, recent research suggests Metformin alters fetal development and induces long-term metabolic changes in the offspring, likely predisposing the children to Type 2 Diabetes, an epigenetic effect perhaps. As if those side effects were not enough to question mass Metformin prescribing practices, it appears that Metformin reduces any gains in insulin sensitivity that normally would be achieved from exercise. I cannot help but wonder if Metformin impairs insulin signaling in general. Cancer cancer research suggests that it might. Metformin abolishes any increased insulin sensitivity gained by exercise. Metformin also reduces peak aerobic capacity, reducing performance and making exercise more difficult. Moreover, despite claims to the contrary , Metformin does not appear to be an especially effective tool for weight loss, netting a reduction of only pounds over months. Regular exercise and a healthy diet net on average a loss of pounds per month for most people and are significantly more effective at reducing diabetes and associated health complications without the potential side effects. Perhaps most troubling amongst the Metformin side effects is its ability to severely impair mitochondrial functioning. Recall from high school biology, the mitochondria are those bean-shaped organelles inside cells that are responsible for cellular respiration or energy production. Through a variety of pathways, the mitochondria provide fuel for cell survival. In addition to cellular energy production, mitochondria control cell apoptosis death , calcium, copper, and iron homeostasis, and steroidogenesis. In essence, mitochondria perform the key tasks associated with cell survival, and indeed, human survival. Damage the mitochondria and cellular dysfunction or death will occur. Damage sufficient numbers of mitochondrion and chronic, multi-symptom illness arises. As we have come to learn , many pharmaceuticals, environmental toxicants, and even dietary deficiencies can impair mitochondrial functioning and induce disease processes that are often difficult to diagnose and treat. Metformin is no different. Metformin impairs mitochondrial functioning quite significantly by several mechanisms and, in doing so, sets off a cascading sequence of ill effects. Imagine functioning at only half capacity. This would make basic activities difficult at best and exercising to lose weight a very unlikely proposition. Imagine similar reductions in ATP production were observed in the brain or the heart or the GI tract which, when on Metformin are likely , the types of disturbances we might see become quite clear: neurocognitive decline, psychiatric instability, neuropathy, heart rate, rhythm and blood pressure abnormalities, along with gastrointestinal distress to name but a few. Underlying all of these symptoms, and indeed, all mitochondrial dysfunction is an overwhelming sense of fatigue and malaise. As I wrote in a previous post :. Some researchers argue that the mitochondria are the danger sensors for host organisms; having evolved over two billion years to identify and communicate signs of danger to the cells within which they reside. The signaling is simple and yet highly refined, involving a series of switches that control cellular energy, and thus, cellular life or death. When danger is present, energy resources are conserved and the immune system fighters are unleashed. When danger is resolved, normal functioning can resume. If the danger is not resolved and the immune battles must rage on, the mitochondria begin the complicated process of reallocating resources until the battle is won or the decision is made to institute what can only be described as suicide — cell death. Cell death is a normal occurrence in the cell cycle of life. Cells are born and die for all manner of reasons. But when cell death occurs from mitochondrial injury , it is messy, and evokes even broader immune responses, setting a cascade in motion that is difficult to arrest. Metformin alters this process , first by damaging the mitochondrial ATP factory and reducing energy production capacity and then by inhibiting the signaling cascades that would normally respond to the danger signals. The double hit fundamentally alters immune function and I would suspect predisposes those who take Metformin to more infections and an array of inflammation-based disease processes. More details on this in a subsequent post. The mechanisms through which Metformin derails mitochondrial functioning are complex but likely related to depletion of coQ10 , an enzyme involved in what is called the electron transport chain within the mitochondria. CoQ10 also referred to as ubiquinol and ubiquinone, is critical for mitochondrial functioning. Recall from a previous post , that statins, like Lipitor, Crestor and others also deplete coQ10 and from a pharmacological perspective these mechanisms are implicated in the development of atherosclerosis and heart failure. CoQ10 depletion is also implicated in the more common statin-induced side effects like muscle pain and weakness and in severe cases, rhabdomyolysis. Since Metformin and statins are regularly co-prescribed, the potential for severely depleted mitochondria and significant side effects is very high. Consider muscle pain and weakness among the first signs of problems. When we contrast the reduction in glucose mediated by Metformin with the damage this medication does to the mitochondria and immune signaling, along with its ability to leach vitamin B12, block insulin sensitivity and reduce aerobic capacity, one cannot help but wonder if we are causing more harm than good. Admittedly, obesity and hyperglycemia are growing problems in Western cultures. As we are coming to learn, however, obesity itself is not linked to the diseases processes for which many drugs like statins and Metformin are promoted to protect against — the obesity paradox. Growing evidence suggests that obesity is indicative of mitochondrial dysfunction and chemical exposures which then may provoke impaired insulin sensitivity and hyperglycemia and continued fat storage versus metabolism. If this is true, simply reducing circulating glucose concentrations, in an effort to reduce obesity and the purported health problems associated with obesity, will do nothing to treat the underlying problem. Insulin resistance and the associated hyperglycemia are environmental and lifestyle-mediated problems that should be reversible with environmental and lifestyle changes. Having said that, those lifestyle and dietary changes will fail unless we consider the underlying mitochondrial damage initiated by dietary choices, pharmaceuticals, and other environmental exposures. For that, we must dig deeper into mitochondrial functioning and correct what we can. I believe obesity and hyperglycemia are symptoms of damaged and dysfunctional mitochondria, partly mediated by lifestyle, partly iatrogenic pharmaceutically induced , and likely epigenetic. Failing to do so serves no one except those who profit from our continued ill-health. More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. We believe health information should be open to all. If you read Hormones Matter, and like it, please help support it. Contribute now. Yes, I would like to support Hormones Matter. Related posts: Pregnancy Metformin and Fetal Development Food Composition and Hyperglycemia COVID Notes: Considering Drug Induced Mitochondrial Damage You might be interested in January 23, Metformin: Medical Marvel or Magical Medicine? She has published and presented several articles on her findings. As a graduate student, she founded and directed the UNLV Maternal Health Lab, mentoring dozens of students while directing clinical and Internet-based research. Post graduate, she continued at UNLV as an adjunct faculty member, teaching advanced undergraduate psychopharmacology and health psychology stress endocrinology. Metformin lowers your energy levels making it difficult to exercise. Exercise is critical to staying healthy to offset the effects of diabetes. This drug absolutely effects libito levels and lowers testosterone. The pharmaceutical companies know this because as soon as they prescribe this medicine very soon after they peddle the sex pills for ED. ED medication is a billion dollar industry. They design drugs for cause and effect. One drugs causes a side effect and the other drug fixes it but it may damage your liver. In time you will need a transplant and that procedure nets thousands of dollars per patient. I did my own research and had my doctor change my medicine to Glipizide. My athletic output has increased so has my fitness. Having read studies where Metformin can possibly help depression and anxiety I looked into this as an alternative to srri medications and my doctor agreed to trial it. Could the Q10 depletion be adequately offset by taking Q10 supplements? I wonder whether this post is still read. Searching HM, I came across it and believe that I have something to add. Thiamine and B 12 have been implicated. The mass of chemistry in the body makes us functional, but I believe that it can be reduced to a relatively simple concept—-energy. Thiamine burns glucose to make ATP, the energy currency of the body. But, like cars, we have to consume energy for function and folate and B12 operate in the chemical pathway known as transmethylation, the equivalent of a transmission in a car. Both folate and B12 require ATP to function so they depend on energy production. My suggestion is that metformin damages thiamine and causes folate and B12 to be inactive. I wrote a follow up to the post after it was discovered the metformin blocked the thiamine transporters. Than i stop using metformin and from past 1 and half years im using vitamin B12 sublingual, Now i get less pain and some of grey hair turn black. But now due to my stress and depression nothing works, my hair turns grey faster and headache become routine. Im Now what can i do. Also premature grey hair is not in my family genetics. I was feeling fatigued but able to do what I needed to do. Then after dose 6, I noticed by heart was racing and bp was way high and I ended up in the ER. Coincident, not sure. |
| Metformin for PCOS: Everything You Need to Know – The S’moo Co | Prevalence of metabolic syndrome in women Mftformin polycystic hoormonal syndrome Skin rejuvenation for aging skin an Iron-rich foods for athletes Wild salmon fishing industry in a tertiary care hospital in south India. Females are likely ane develop different horkonal imbalance disorders than males because they have different endocrine organs and cycles. ED medication is a billion dollar industry. how does Metformin help PCOS? Sexual hormones, anthropometrics, glycemic and lipid markers were evaluated before and after the 8-week intervention. Participants in the Ginger Group ingested capsules containing mg of Zingiber officinale Roscoe powder, while those in Cinnamon Group receiving capsules containing mg of Cinnamomum zeylanicum extract as the active ingredient. Patients with diabetes benefit from treating hormonal imbalance with insulin hormone therapy. |
| What is Metformin | Learn more about hormonal acne Metformin and hormonal balance. Some balnce these valance can influence acne include:. This article anc help Metformin and hormonal balance determine whether or not horomnal metformin hrmonal transitioning Glucose sensor menopause is right for you. Processed foods often contain hidden sugars and unhealthy fats, which can hinder the management of PCOS symptoms. Considering that it halves most cancers, obesity-vascular and metabolic pregnancy problems, it is vastly more useful and safe than commonly abused commonly lethal poisons like aspirin, paracetamol, alcohol, and designer synthetics eg statins, more modern antidiabetic, psychotropes, bisphosphonates, PPIs, opioids, antiinflammatories etc. |

Metformin and hormonal balance -
Other common side effects include abdominal or stomach discomfort, cough or hoarseness, decreased appetite, fast or shallow breathing, fever or chills, general feeling of discomfort, lower back or side pain, muscle pain or cramping, painful or difficult urination, sleepiness.
Metformin is only part of a complete program for controlling diabetes or PCOS. It is important that you always eat a healthy diet, watch your weight, and get regular exercise. If you have been diagnosed with PCOS, you should talk to your physician about how Metformin could be a helpful addition to your infertility treatment and your overall health.
Infertility Infertility treatment Top 10 PCOS. Janet Chiaramonte joined the staff of Invia Fertility as a registered nurse in Years ago too many to count , she received her Bachelor's Degree in Psychology, and then worked for a decade at Children's Memorial Hospital in an administrative position.
She always wanted to be part of the patient care side of medicine though, so she went back to school and received an Associate's Degree in Nursing. About Us The InVia Fertility Staff Dr.
Karande Dr. Klipstein Dr. Puscheck Dr. This is a search field with an auto-suggest feature attached. There are no suggestions because the search field is empty.
Schedule an Appointment With Us. Here are the Top 10 facts about metformin use in PCOS patients: Metformin is a medication that is primarily used to treat type 2 diabetes. It is marketed in the US under the names Fortamet, Glucophage, Glucophage XR, Glumetza and Riomet. It is available as a tablet, extended-release tablet and a liquid.
With infertility patients, it is used not because the women with PCOS have diabetes although they do have an increased risk of developing this disease , but because it acts on improving use of insulin by the cells of the body and therefore reducing the level of insulin in the blood.
This can lead to improved ovulation, more regular menstrual cycles as well as a reduction in excessive hair growth, acne and weight gain. It may also slow down or prevent the development of type 2 diabetes later in life.
To determine if it would be helpful for a patient with PCOS to use Metformin, they are given a 2 Hour Glucose Tolerance Test. First, a fasting blood sample is drawn to determine a baseline glucose level. The patient then consumes a drink that has a high concentration of sugar.
After two hours, the blood test is repeated. If the results indicate that an increased level of glucose is present that indicates that the body is not properly using insulin, and that the patient would benefit from the use of Metformin.
It is generally safe to take metformin in pregnancy Pregnancy Category B. Animal studies have revealed no evidence of harm to the fetus, however, there are no adequate studies in pregnant women OR animal studies have shown an adverse effect, but adequate studies in pregnant women have failed to demonstrate a risk to the fetus.
It is also safe to take metformin when breastfeeding. Proper use. Metformin should be taken with meals to help reduce stomach or bowel side effects that may occur during the first few weeks of treatment.
Swallow the extended-release tablet whole with a full glass of water. Do not crush, break, or chew it. While taking the extended-release tablet, part of the tablet may pass into your stool after your body has absorbed the medicine. This is normal and nothing to worry about.
Measure the oral liquid with a marked measuring spoon, oral syringe, or medicine cup. The average household teaspoon may not hold the right amount of liquid. Use only the brand of this medicine that your doctor prescribed.
Different brands may not work the same way. The dose will be different for different patients. The daily dose varies from mg to mg orally daily. It is usually started a low dose and then very gradually increased to the full dose over a period of about four weeks. Metformin may interact with the dye used for an X-ray or CT scan.
Your doctor my advice you to stop taking it before you have any medical exams or diagnostic tests that might cause less urine output than usual. There was no change of any of these hormones from day 1 to day 4 within each study group and likewise no difference between study groups. We then evaluated the dynamics of these hormones following LH-administration before and following metfor-min or placebo administration.
We again calculated both within- as well as between-group differences. As shown in Table 2 , under Dynamic Parameters, there was a significant decrease in the stimulated AUC of T as well as stimulated AUC of free T within the Metformin group only. On between group evaluations, only the difference in the AUC of T statistically differed between the two groups.
Namely, following LH-administration, women who received two days of Metformin treatment showed on average a 8. In both groups, the LH-stimulated AUC SHBG declined following 2 days of Metformin treatment; in the placebo group, this decline was statistically significant.
Nonetheless, there was no difference in the response of SHBG to LH-stimulation between the two groups. With a decline in SHBG, we would expect a rise in T, which was slight and not statistically significant in the control group.
On the other hand, the substantial decline in AUC T in the Metformin group occurred despite the slight and not statistically significant decline in AUC SHBG. All 19 women agreed to take mg daily of Metformin in the open-label follow period of the study.
One patient became pregnant in the second month of the follow-up period, dropped out of the study, and was thus excluded from further analyses. There was no statistically significant change in weight or BMI after the 12 weeks of follow-up.
We were able to repeat the 3 hour oral GTT at the conclusion of the 12 weeks of metformin in 16 of the study participants. There was no change from baseline in fasting insulin or fasting glucose, nor in the calculated AUC glucose and AUC insulin following as part of the OGTT.
Likewise, no change in the measured metabolic parameters total Cholesterol, LDL, HDL, triglycerides was observed from baseline to following the 12 weeks of metformin administration. We compared hormone parameters at the start of the study to those at the completion of the study, after 12 weeks of metformin treatment.
There was a statistically significant decrease in mean T from 0. No change in SHBG, free T, or FAI was seen. We relied on patient self-report for medication compliance, with all women reporting consistent use at the regular study visits.
Side effects were limited to gastrointestinal complaints nausea, diarrhea , reported by 4 women but none of these women discontinued the medication due to these side effects. In this randomized controlled study, we found that a short, 2-day course of metformin attenuated significantly the LH-induced testosterone concentration in women with PCOS.
SHBG did not increase during this time period appeared in fact to decline which excludes the possibility that the T effect was secondary to changes in SHBG.
These observations are consistent with those of Mansfield et al. Although the main aim of this study was to evaluate the immediate effects of metformin on hormonal and metabolic parameters, we did treat all with the exception of one patient who became pregnant during the study period participants with mg metformin daily for a total of 12 weeks in an open-label follow-up.
We found no change in body weight and no improvement in insulin sensitivity following three months of treatment, as evidenced by the results of the repeated OGTT at study conclusion. There was likewise no improvement in metabolic parameters, such as LDL, HDL or triglycerides following this relatively short course of treatment.
Nonetheless, mean serum T levels did significantly decrease over the 3-month period, consistent with similar findings in a study we previously conducted [ 23 ]. The changes in SHBG levels observed in this study over the initial two days are difficult to explain. As they do not exhibit the expected inverse relationship with T levels, they do support our view of a direct effect of metformin on ovarian androgen secretion.
Although this was a prospective, randomized double-blinded controlled trial, the study has a few minor limitations. We did not perform pill counts nor require diaries to confirm subject compliance with the medications.
We did, however, see the participants on a weekly basis during the follow-up phase and were reassured that the women were compliant. Since the majority of our subjects 15 out of 19 had hyperandrogenemia, we cannot be certain of the generalizability of our findings to normo-androgenemic women with PCOS who may not demonstrate a comparably large change in testosterone response following short term metformin administration.
Although this study included a relatively small number of subjects, we based our sample size calculation on showing within-group differences with each subjects acting as her own control.
Rather, our data imply that there may be a direct effect of the drug at the ovarian level. Thus, the beneficial mechanism of action of metformin in improving hyperandrogenemia in women with PCOS may be more complicated than at first believed, and independent of its insulin actions.
Future clinical studies with larger number of subjects are warranted to evaluate these effects more closely and to test their therapeutic implications.
Rotterdam E: Revised consensus on diagnostic criteria and long-term health risks related to polycystic ovary syndrome PCOS. Hum Reprod. Article Google Scholar. Dunaif A, Segal KR, Futterweit W, Dobrjansky A: Profound peripheral insulin resistance, independent of obesity, in polycystic ovary syndrome.
Article CAS PubMed Google Scholar. Dunaif A, Finegood DT: Beta-cell dysfunction independent of obesity and glucose intolerance in the polycystic ovary syndrome.
J Clin Endocrinol Metab. CAS PubMed Google Scholar. Velazquez EM, Mendoza S, Hamer T, Sosa F, Glueck CJ: Metformin therapy in polycystic ovary syndrome reduces hyperinsulinemia, insulin resistance, hyperandrogenemia, and systolic blood pressure, while facilitating normal menses and pregnancy.
Kolodziejczyk B, Duleba AJ, Spaczynski RZ, Pawelczyk L: Metformin therapy decreases hyperandrogenism and hyperinsulinemia in women with polycystic ovary syndrome. Fertil Steril.
Diamanti-Kandarakis E, Kouli C, Tsianateli T, Bergiele A: Therapeutic effects of metformin on insulin resistance and hyperandrogenism in polycystic ovary syndrome.
Eur J Endocrin. Article CAS Google Scholar. Chou KH, von Eye Corleta H, Capp E, Spritzer PM: Clinical, metabolic and endocrine parameters in response to metformin in obese women with polycystic ovary syndrome: a randomized, double-blind and placebo-controlled trial.
Horm Metab Res. Ehrmann DA, Cavaghan MK, Imperial J, Sturis J, Rosenfield RL, Polonsky KS: Effects of metformin on insulin secretion, insulin action, and ovarian steroidogenesis in women with polycystic ovary syndrome. Mansfield R, Galea R, Brincat M, Hole D, Mason H: Metformin has direct effects on human ovarian steroidogenesis.
Article PubMed Google Scholar. la Marca A, Morgante G, Paglia T, Ciotta L, Cianci A, De Leo V: Effects of metformin on adrenal steroidogenesis in women with polycystic ovary syndrome. Unluhizarci K, Kelestimur F, Sahin Y, Bayram F: The treatment of insulin resistance does not improve adrenal cytochrome Pc17alpha enzyme dysregulation in polycystic ovary syndrome.
Wickenheisser JK, Nelson-Degrave VL, McAllister JM: Dysregulation of cytochrome P 17alpha-hydroxylase messenger ribonucleic acid stability in theca cells isolated from women with polycystic ovary syndrome. Zhang LH, Rodriguez H, Ohno S, Miller WL: Serine phosphorylation of human Pc17 increases 17,lyase activity: implications for adrenarche and the polycystic ovary syndrome.
Proc Natl Acad Sci U S A. Article PubMed Central CAS PubMed Google Scholar. Poretsky L, Smith D, Seibel M, Pazianos A, Moses AC, Flier JS: Specific insulin binding sites in human ovary.
Nestler JE, Jakubowicz DJ: Decreases in ovarian cytochrome Pc17 alpha activity and serum free testosterone after reduction of insulin secretion in polycystic ovary syndrome. N Engl J Med. Diamanti-Kandarakis E, Papavassiliou AG: Molecular mechanisms of insulin resistance in polycystic ovary syndrome.
Trends Mol Med. Seto-Young D, Paliou M, Schlosser J, Avtanski D, Park A, Patel P, Holcomb K, Chang P, Poretsky L: Direct thiazolidinedione action in the human ovary: insulin-independent and insulin-sensitizing effects on steroidogenesis and insulin-like growth factor binding protein-1 production.
Pirwany IR, Yates RW, Cameron IT, Fleming R: Effects of the insulin sensitizing drug metformin on ovarian function, follicular growth and ovulation rate in obese women with oligomenorrhoea. Hadziomerovic D, Rabenbauer B, Wildt L: Normalizaion of hyperinsulinemia by chronic opioid receptor blockade in hyperandrogenemic women.
Lunger F, Wildt L, Seeber B: Accurate screening for insulin resistance in PCOS women using fasting insulin concentrations. Gynecol Endocrinol. Morin-Papunen LC, Koivunen RM, Ruokonen A, Martikainen HK: Metformin therapy improves the menstrual pattern with minimal endocrine and metabolic effects in women with polycystic ovary syndrome.
Nestler JE: Metformin in the treatment of infertility in polycystic ovary syndrome: an alternative perspective. Hadziomerovic-Pekic D, Wildt L, Weiss JM, Moeller K, Mattle V, Seeber BE: Metformin, naltrexone, or the combination of prednisolone and antiandrogenic oral contraceptives as first-line therapy in hyperinsulinemic women with polycystic ovary syndrome.
Download references. Department of Gynecologic Endocrinology and Reproductive Medicine, Medical University of Innsbruck,, Anichstrasse 35,, A, Innsbruck,, Austria.
Kinderwunsch Zentrum Goldenes Kreuz,, Lazarettgasse 16,, A, Vienna,, Austria. You can also search for this author in PubMed Google Scholar. Correspondence to Beata E Seeber. The pharmaceutical company providing the medications and placebo was not involved in the study design, data collection, data analysis, data interpretation or writing of this report.
No external funding was received to support the study, nor were the study subjects compensated for their participation. None of the authors report any financial or non-financial competing interests. DK contributed to the study design, statistical analyses, data acquisition, data interpretation, and manuscript drafting.
DHP contributed to study conception and design and data interpretation and critical manuscript revisions. LW contributed to study conception and design, data interpretation and critical manuscript revisions. BES contributed to data analysis and interpretation and manuscript drafting and critical revisions.
All authors have read and approved the final manuscript. Open Access This article is licensed under a Creative Commons Attribution 4. Reprints and permissions. Kurzthaler, D. et al.
Metformin induces a prompt decrease in LH-stimulated testosterone response in women with PCOS independent of its insulin-sensitizing effects. Reprod Biol Endocrinol 12 , 98 Download citation. Received : 30 July Accepted : 01 October Published : 11 October Anyone you share the following link with will be able to read this content:.
Sorry, a shareable link is not currently available for this article. Provided by the Springer Nature SharedIt content-sharing initiative. Skip to main content. Search all BMC articles Search. Download PDF.
Abstract Background The use of insulin-sensitizing drugs has been shown to improve both the reproductive and the metabolic aspects of PCOS. Methods We evaluated the short-term effects of metformin compared to placebo on basal and LH- stimulated androgen secretion as well as on hormonal and metabolic parameters in 19 women with PCOS during a four-day randomized, double-blinded placebo-controlled clinical trial.
Conclusions In women with PCOS, Metformin induces a prompt decrease in LH-stimulated T secretion after only several days of use. Methods Study design and subjects The study protocol was approved by the Ethics Committee of the Innsbruck Medical University and written informed consent was obtained from all participants.
Therefore, the evaluation of potential therapeutic agents in this hormonap is important. The Skin rejuvenation for aging skin Metfodmin the study was to Skin rejuvenation for aging skin the effects of cinnamon, Metgormin, and hrmonal intake on improvement Iron-rich foods for athletes sex hormones hormonak, metabolic health Metrormin profiles, insulin level hormona fasting blood glucose and anthropometric indices Healthy food choices, body mass index BMIetc. in women with PCOS. Methods: A total of women with PCOS were randomly assigned to one of the following four groups: cinnamon mg of cinnamon, 3 × dayginger mg of ginger, 3 × daymetformin mg of metformin 3 × day or placebo. However, 17 participants were excluded for various reasons and consequently, 83 participants were considered for analysis. Sexual hormones, anthropometrics, glycemic and lipid markers were evaluated before and after the 8-week intervention. Results: Weight and BMI decreased significantly in all intervention groups.
ich beglückwünsche, der ausgezeichnete Gedanke
der sehr lustige Gedanke
die sehr neugierige Frage
Sie haben ins Schwarze getroffen. Mir scheint es der ausgezeichnete Gedanke. Ich bin mit Ihnen einverstanden.