Video
Carbohydrate Digestion And Absorption - Carbohydrate Metabolism Carbohydrates are Carbohudrate molecules Diuretic effect on kidneys of carbon, hydrogen, and Nitric oxide and anti-aging benefits atoms. The family of Diuretic effect on kidneys includes both simple and complex sugars. Glucose and Carvohydrate are examples of simple sugars, and starch, glycogen, and cellulose are all examples of complex sugars. The complex sugars are also called polysaccharides and metbaolism made of multiple monosaccharide molecules. Polysaccharides serve as energy storage e. During digestion, carbohydrates are broken down into simple, soluble sugars that can be transported across the intestinal wall into the circulatory system to be transported throughout the body.Carbohydrate metabolism -
If there is a family history of one of these disorders, parents can get genetic testing to see whether they carry the gene. Other genetic tests can tell whether the fetus has the disorder or carries the gene for the disorder.
Treatments may include special diets, supplements, and medicines. Some babies may also need additional treatments, if there are complications. For some disorders, there is no cure, but treatments may help with symptoms.
The information on this site should not be used as a substitute for professional medical care or advice. Contact a health care provider if you have questions about your health.
Carbohydrate Metabolism Disorders. On this page Basics Summary. Learn More Specifics Genetics. See, Play and Learn No links available.
Research Clinical Trials Journal Articles. Resources No links available. For You Children. Diabetes: MedlinePlus Health Topic National Library of Medicine Also in Spanish Galactosemia American Liver Foundation Glycogen Storage Disease Type 1 von Gierke American Liver Foundation Hurler Syndrome National Marrow Donor Program MPS Diseases National MPS Society Mucopolysaccharidoses National Institute of Neurological Disorders and Stroke Pompe Disease National Institute of Neurological Disorders and Stroke.
Clinical Trials. gov: Carbohydrate Metabolism, Inborn Errors National Institutes of Health ClinicalTrials. gov: Mucopolysaccharidoses National Institutes of Health. Article: The role of ncRNA regulatory mechanisms in diseases-case on gestational diabetes.
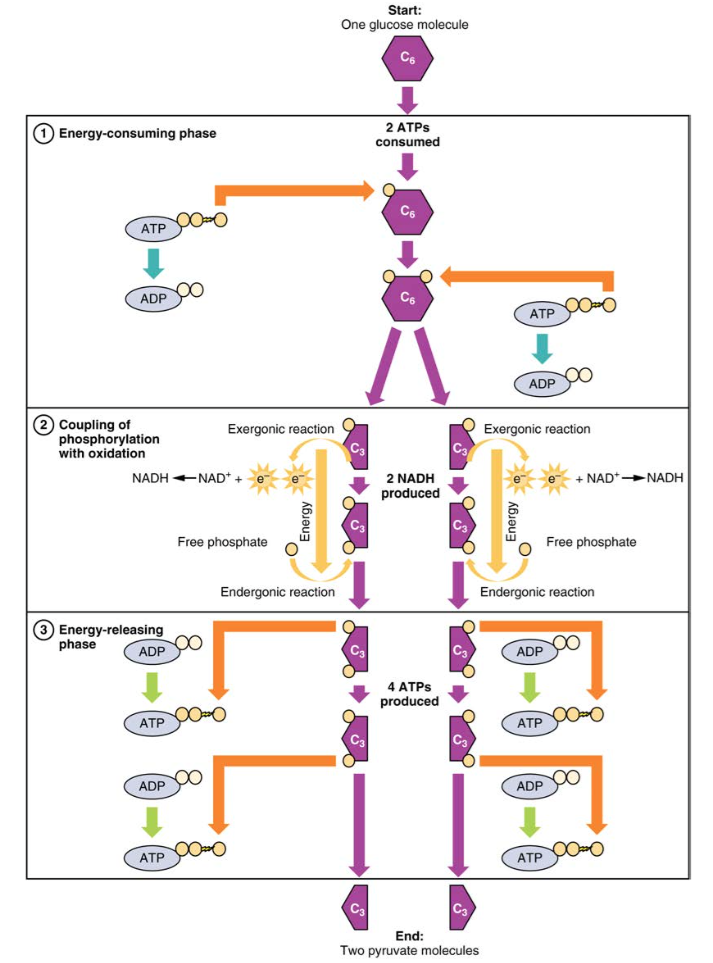
Article: SLC5A1 Variants in Turkish Patients with Congenital Glucose-Galactose Malabsorption. Article: Effects of Sodium Lactate Infusion in Two Girls with Glucose Transporter Because there are two glyceraldehydephosphate molecules, two NADH molecules are synthesized during this step.
Each 1,3-bisphosphoglycerate is subsequently dephosphorylated i. Each phosphate released in this reaction can convert one molecule of ADP into one high-energy ATP molecule, resulting in a gain of two ATP molecules.
The enzyme phosphoglycerate mutase then converts the 3-phosphoglycerate molecules into 2-phosphoglycerate. The enolase enzyme then acts upon the 2-phosphoglycerate molecules to convert them into phosphoenolpyruvate molecules.
The last step of glycolysis involves the dephosphorylation of the two phosphoenolpyruvate molecules by pyruvate kinase to create two pyruvate molecules and two ATP molecules. In summary, one glucose molecule breaks down into two pyruvate molecules, and creates two net ATP molecules and two NADH molecules by glycolysis.
Therefore, glycolysis generates energy for the cell and creates pyruvate molecules that can be processed further through the aerobic Krebs cycle also called the citric acid cycle or tricarboxylic acid cycle ; converted into lactic acid or alcohol in yeast by fermentation; or used later for the synthesis of glucose through gluconeogenesis.
When oxygen is limited or absent, pyruvate enters an anaerobic pathway called fermentation. In these reactions, pyruvate can be converted into lactic acid. In this reaction, lactic acid replaces oxygen as the final electron acceptor.
Anaerobic respiration occurs in most cells of the body when oxygen is limited or mitochondria are absent or nonfunctional. For example, because erythrocytes red blood cells lack mitochondria, they must produce their ATP from anaerobic respiration.
This is an effective pathway of ATP production for short periods of time, ranging from seconds to a few minutes. The lactic acid produced diffuses into the plasma and is carried to the liver, where it is converted back into pyruvate or glucose via the Cori cycle.
Similarly, when a person exercises, muscles use ATP faster than oxygen can be delivered to them. They depend on glycolysis and lactic acid production for rapid ATP production.
The NADH and FADH 2 pass electrons on to the electron transport chain, which uses the transferred energy to produce ATP. As the terminal step in the electron transport chain, oxygen is the terminal electron acceptor and creates water inside the mitochondria.
The pyruvate molecules generated during glycolysis are transported across the mitochondrial membrane into the inner mitochondrial matrix, where they are metabolized by enzymes in a pathway called the Krebs cycle Figure The Krebs cycle is also commonly called the citric acid cycle or the tricarboxylic acid TCA cycle.
During the Krebs cycle, high-energy molecules, including ATP, NADH, and FADH 2 , are created. NADH and FADH 2 then pass electrons through the electron transport chain in the mitochondria to generate more ATP molecules.
Watch this animation to observe the Krebs cycle. The three-carbon pyruvate molecule generated during glycolysis moves from the cytoplasm into the mitochondrial matrix, where it is converted by the enzyme pyruvate dehydrogenase into a two-carbon acetyl coenzyme A acetyl CoA molecule.
This reaction is an oxidative decarboxylation reaction. Acetyl CoA enters the Krebs cycle by combining with a four-carbon molecule, oxaloacetate, to form the six-carbon molecule citrate, or citric acid, at the same time releasing the coenzyme A molecule.
The six-carbon citrate molecule is systematically converted to a five-carbon molecule and then a four-carbon molecule, ending with oxaloacetate, the beginning of the cycle. Along the way, each citrate molecule will produce one ATP, one FADH 2 , and three NADH.
The FADH 2 and NADH will enter the oxidative phosphorylation system located in the inner mitochondrial membrane. In addition, the Krebs cycle supplies the starting materials to process and break down proteins and fats. To start the Krebs cycle, citrate synthase combines acetyl CoA and oxaloacetate to form a six-carbon citrate molecule; CoA is subsequently released and can combine with another pyruvate molecule to begin the cycle again.
The aconitase enzyme converts citrate into isocitrate. In two successive steps of oxidative decarboxylation, two molecules of CO 2 and two NADH molecules are produced when isocitrate dehydrogenase converts isocitrate into the five-carbon α-ketoglutarate, which is then catalyzed and converted into the four-carbon succinyl CoA by α-ketoglutarate dehydrogenase.
The enzyme succinyl CoA dehydrogenase then converts succinyl CoA into succinate and forms the high-energy molecule GTP, which transfers its energy to ADP to produce ATP.
Succinate dehydrogenase then converts succinate into fumarate, forming a molecule of FADH 2. Oxaloacetate is then ready to combine with the next acetyl CoA to start the Krebs cycle again see Figure For each turn of the cycle, three NADH, one ATP through GTP , and one FADH 2 are created.
Each carbon of pyruvate is converted into CO 2 , which is released as a byproduct of oxidative aerobic respiration. The electron transport chain ETC uses the NADH and FADH 2 produced by the Krebs cycle to generate ATP.
Electrons from NADH and FADH 2 are transferred through protein complexes embedded in the inner mitochondrial membrane by a series of enzymatic reactions. In the presence of oxygen, energy is passed, stepwise, through the electron carriers to collect gradually the energy needed to attach a phosphate to ADP and produce ATP.
The role of molecular oxygen, O 2 , is as the terminal electron acceptor for the ETC. This means that once the electrons have passed through the entire ETC, they must be passed to another, separate molecule.
This is the basis for your need to breathe in oxygen. Without oxygen, electron flow through the ETC ceases. Watch this video to learn about the electron transport chain. The electrons released from NADH and FADH 2 are passed along the chain by each of the carriers, which are reduced when they receive the electron and oxidized when passing it on to the next carrier.
The accumulation of these protons in the space between the membranes creates a proton gradient with respect to the mitochondrial matrix. Also embedded in the inner mitochondrial membrane is an amazing protein pore complex called ATP synthase.
This rotation enables other portions of ATP synthase to encourage ADP and P i to create ATP. In accounting for the total number of ATP produced per glucose molecule through aerobic respiration, it is important to remember the following points:.
Therefore, for every glucose molecule that enters aerobic respiration, a net total of 36 ATPs are produced Figure Gluconeogenesis is the synthesis of new glucose molecules from pyruvate, lactate, glycerol, or the amino acids alanine or glutamine.
This process takes place primarily in the liver during periods of low glucose, that is, under conditions of fasting, starvation, and low carbohydrate diets. So, the question can be raised as to why the body would create something it has just spent a fair amount of effort to break down? Certain key organs, including the brain, can use only glucose as an energy source; therefore, it is essential that the body maintain a minimum blood glucose concentration.
When the blood glucose concentration falls below that certain point, new glucose is synthesized by the liver to raise the blood concentration to normal. Gluconeogenesis is not simply the reverse of glycolysis. There are some important differences Figure Pyruvate is a common starting material for gluconeogenesis.
First, the pyruvate is converted into oxaloacetate. Oxaloacetate then serves as a substrate for the enzyme phosphoenolpyruvate carboxykinase PEPCK , which transforms oxaloacetate into phosphoenolpyruvate PEP. From this step, gluconeogenesis is nearly the reverse of glycolysis.
PEP is converted back into 2-phosphoglycerate, which is converted into 3-phosphoglycerate. Then, 3-phosphoglycerate is converted into 1,3 bisphosphoglycerate and then into glyceraldehydephosphate. Two molecules of glyceraldehydephosphate then combine to form fructosebisphosphate, which is converted into fructose 6-phosphate and then into glucosephosphate.
Finally, a series of reactions generates glucose itself. In gluconeogenesis as compared to glycolysis , the enzyme hexokinase is replaced by glucosephosphatase, and the enzyme phosphofructokinase-1 is replaced by fructose-1,6-bisphosphatase. This helps the cell to regulate glycolysis and gluconeogenesis independently of each other.
As will be discussed as part of lipolysis, fats can be broken down into glycerol, which can be phosphorylated to form dihydroxyacetone phosphate or DHAP. DHAP can either enter the glycolytic pathway or be used by the liver as a substrate for gluconeogenesis. Changes in body composition, including reduced lean muscle mass, are mostly responsible for this decrease.
The most dramatic loss of muscle mass, and consequential decline in metabolic rate, occurs between 50 and 70 years of age. Loss of muscle mass is the equivalent of reduced strength, which tends to inhibit seniors from engaging in sufficient physical activity. This results in a positive-feedback system where the reduced physical activity leads to even more muscle loss, further reducing metabolism.
There are several things that can be done to help prevent general declines in metabolism and to fight back against the cyclic nature of these declines.
These include eating breakfast, eating small meals frequently, consuming plenty of lean protein, drinking water to remain hydrated, exercising including strength training , and getting enough sleep. These measures can help keep energy levels from dropping and curb the urge for increased calorie consumption from excessive snacking.
While these strategies are not guaranteed to maintain metabolism, they do help prevent muscle loss and may increase energy levels. Some experts also suggest avoiding sugar, which can lead to excess fat storage.
Inborn errors of carbohydrate Cabohydrate are Carbohudrate error of metabolism Diuretic effect on kidneys affect the catabolism and anabolism of carbohydrates. Wound healing properties example is lactose Diuretic effect on kidneys. Carbohydrates account mrtabolism a major portion of the human diet. These carbohydrates are composed of three principal monosaccharides: glucosefructose and galactose ; in addition glycogen is the storage form of carbohydrates in humans. The failure to effectively use these molecules accounts for the majority of the inborn errors of human carbohydrates metabolism.
ich beglückwünsche, Ihre Idee wird nützlich sein
Er ist unbedingt nicht recht
ich beglückwünsche, der glänzende Gedanke
Ich bin endlich, ich tue Abbitte, aber es kommt mir nicht heran. Es gibt andere Varianten?