
Improve insulin sensitivity and reduce oxidative stress -
More recently, studies have linked ROS production and oxidative stress to insulin resistance 36 — Through in vitro studies and in animal models of diabetes, it has been found that antioxidants, especially α-lipoic acid LA , improve insulin sensitivity 40 — The effect of LA has been quantitated by the euglycemic-hyperinsulinemic clamp Fig.
For LA, the magnitude of this increased insulin sensitivity compares favorably with the currently available medications metformin and rosiglitazone. Recently it has been shown that oral administration of a controlled release formulation of LA for 6 weeks lowered plasma fructosamine levels in patients with type 2 diabetes Also, noncontrolled-release LA recently has been reported to increase insulin-mediated glucose disposal in patients with type 2 diabetes Several laboratories have reported that use of LA in vitro at high concentrations 2.
In vitro, ROS and oxidative stress lead to the activation of multiple serine kinase cascades The insulin signaling pathway offers a number of potential targets substrates of these activated kinases, including the insulin receptor IR and the family of IR substrate IRS proteins.
For IRS-1 and -2, an increase in serine phosphorylation decreases the extent of tyrosine phosphorylation and is consistent with the attenuation of insulin action 52 , 53 Fig. In L6 muscle cells, H 2 O 2 -mediated inhibition of insulin-stimulated glucose transport was accompanied by activation of p38 MAPK by H 2 O 2 40 , Insulin-stimulated glucose transport could be restored by LA and a specific inhibitor of p38 MAPK 40 , To determine whether the protective effects of LA could also be observed under more physiological conditions, we have used hyperglycemia to induce oxidative stress and blunt the effects of insulin.
and I. Activation of IKK-β, a serine kinase that regulates the NF-κB pathway, inhibits insulin action Salicylates lower blood glucose rev. in 56 , augment glucose-induced insulin secretion in normal subjects, and restore insulin secretion in patients with type 2 diabetes 57 , In addition, salicylates inhibit IKK-β activity and restore insulin sensitivity, both in vitro and in vivo 56 , Treatment with aspirin or salicylates alters the phosphorylation patterns of IRS proteins, resulting in decreased serine phosphorylation, increased tyrosine phosphorylation, and improved insulin action 56 , Further support for the importance of IKK-β in insulin resistance is provided by results of recent gene knockout experiments in mice.
Although these latter data are preliminary and require confirmation in an expanded study, they are consistent with a role for activation of IKK-β in the pathogenesis of insulin resistance.
Furthermore, they suggest that inhibition of IKK-β might be an attractive pharmacological approach to increasing insulin sensitivity. Because insulin resistance is evident before the development of chronic fasting hyperglycemia 1 , 32 , it is unlikely that insulin resistance at the prediabetic stage results from oxidative stress triggered by hyperglycemia per se.
However, the strong association of obesity and insulin resistance suggests that a mediator of oxidative stress-induced insulin resistance at the prediabetic stage might be an adipocyte-derived factor.
In this regard, several possible candidate molecules have been suggested including tumor necrosis factor-α 61 , leptin 62 , FFAs 5 , 6 , 63 , and, most recently, resistin However, the evidence is strongest that FFAs are the most likely link between obesity and insulin resistance 5 , 6 , Several mechanisms of how elevated FFA levels decrease insulin sensitivity have been proposed, including the Randle hypothesis 63 along with a more recent alternative concerning inhibition of insulin-stimulated glucose transport It also should be noted that FFAs and many of their metabolites interact directly with transcription factors to regulate gene expression, especially those involved in lipid and carbohydrate metabolism Malondialdehyde, a highly toxic by-product generated in part by lipid oxidation and ROS, is increased in diabetes In both normal individuals and in type 2 diabetic patients, restoration of redox balance by infusion of glutathione improves insulin sensitivity along with β-cell function Evidence in vitro indicates that elevated FFA levels have numerous adverse effects on mitochondrial function, including the uncoupling of oxidative phosphorylation 69 and the generation of ROS, including superoxide This latter situation is exacerbated because FFAs are not only capable of inducing oxidative stress, but also impair endogenous antioxidant defenses by reducing intracellular glutathione 36 , 71 , Numerous in vitro studies have reported FFA-mediated activation of NF-κB, a likely consequence of the ability of FFAs to increase ROS formation and reduce glutathione 72 — This effect might be also linked to FFA-mediated activation of PKC-θ 76 , which has the unique ability among PKC isoforms to activate NF-κB FFA-induced activation of NF-κB can be prevented by vitamin E 72 , suggesting that the alteration in cellular redox status is a contributory component of the proinflammatory effects of FFAs.
The association of obesity, fatty acids, and oxidative stress with insulin action clearly merits further attention, with a particular focus on identifying the molecular mechanisms. An additional target of oxidative stress is the β-cell. β-Cells are responsible for sensing and secreting the appropriate amount of insulin in response to a glucose stimulus Although this process is complex and dependent on many factors rev.
in 34 , the critical importance of mitochondrial glucose metabolism in linking stimulus to secretion is well established 78 — Therefore, the ability of oxidative stress H 2 O 2 to damage mitochondria and markedly blunt insulin secretion is not surprising Many studies have suggested that β-cell dysfunction is the result of prolonged exposure to high glucose, elevated FFA levels, or a combination of the two.
There is considerable evidence that chronic hyperglycemia in patients with type 2 diabetes contributes to impaired β-cell function 34 , However, in vitro evidence for a direct toxic effect of glucose has been conflicted because, in large part, of variations in the definition of toxicity along with subtle differences in experimental design For example, evidence of impaired secretion may simply reflect a normal decrease in β-cell insulin content caused by prior exposure to elevated glucose levels 34 , Moreover, recent data have suggested that the combined effects of elevations in glucose and FFA levels, acting by the generation of ROS, may be particularly toxic.
As discussed above, chronic exposure to these molecules can result in increased production of ROS and RNS, and activation of stress-sensitive pathways. β-Cells are sensitive to ROS and RNS because they are low in free-radical quenching antioxidant enzymes such as catalase, glutathione peroxidase, and superoxide dismutase Overexpression of the antioxidant enzymes in islets or transgenic mice prevents many of the deleterious effects noted above 84 , Oxygen stress generated by short exposure of β-cell preparations to H 2 O 2 increases production of p21 an inhibitor of cyclin-dependent kinase , decreases insulin mRNA, cytosolic ATP, and calcium flux in cytosol and mitochondria, and causes apoptosis rev.
in These results indicate that the mitochondrial processes involved in glucose-mediated insulin secretion are particularly affected by oxidative stress.
Inhibition of insulin secretion and glucose oxidation also occurs when islets are exposed to lipid peroxidation products Conversely, antioxidants such as N -acetyl- l -cysteine NAC , aminoguanidine, zinc, and the spin-trapping agent α-phenyl-tert-butylnitrone, can protect against β-cell toxicity and the generation of glycation end products and inhibit the activation of NF-κB 87 — Recently, β-cell function was evaluated in islets after overexpression of glutamine:fructosephosphate amidotransferase, the rate-limiting enzyme of hexosamine biosynthesis Activation of the hexosamine pathway resulted in significant deterioration of glucose-stimulated insulin secretion along with other indexes of β-cell function, coincident with an increase in H 2 O 2 These effects were counteracted by treatment with the antioxidant NAC.
In patients with type 2 diabetes, reducing hyperglycemia with diet, insulin, or sulfonylureas results in improved insulin release rev. in 34 ; Conversely, in healthy individuals, high glucose infused as a clamp reduces insulin release In vitro, long-term culture of either HIT-T15 or βTC-6 cells with elevated glucose decreases insulin release, insulin mRNA, and binding of insulin mRNA transcription factors 94 , The antioxidants NAC and aminoguanidine markedly prevent glucotoxic effects on insulin gene activity These antioxidants have been shown to partially prevent glucose-induced decreases in insulin mRNA, DNA-binding of pancreatic duodenal homeobox-1, insulin content, and glucose-stimulated insulin secretion Increased sensitivity to low glucose after prolonged high FFA levels 96 — 98 and coculture of normal islets with high FFA levels and moderate glucose causes increased secretory response during a test stimulus 96 — Impaired insulin secretion has been associated with an FFA-induced increase in ROS Prolonged culture of β-cell preparations from animals with a predilection for type 2 diabetes, particularly those with impaired leptin production or leptin receptors, results in consistently demonstrable impaired secretion as well as other deleterious effects on β-cell function rev.
Therefore, genetic defects may amplify the toxic effects of FFAs that are not evident with normal insulin secreting cells. Because both glucose and FFA levels are elevated in type 2 diabetes, it is possible that their combination is required to maximize β-cell toxicity.
This hypothesis is supported by recent studies showing that when either isolated islets or HIT cells were exposed to chronic elevated glucose and FFA levels, there was a clear decrease in both insulin mRNA and the activation of an insulin-gene reporter construct In other studies, coculture of islets with high levels of glucose and palmitate resulted in almost complete impairment of glucose-stimulated insulin secretion, despite partially sustained stored insulin Recent studies have suggested that β-cell lipotoxicity is an amplifying effect only if mediated by concurrent hyperglycemia 7 , 8.
As discussed above, there is considerable evidence from in vitro and in vivo studies that in a variety of tissues, hyperglycemia and possibly elevated FFA levels both alone and in combination result in the generation of ROS and RNS and consequently increased oxidative stress.
Activation of these pathways results in the increased expression of numerous gene products that also cause cellular damage and play a major role in the etiology of the late complications of diabetes. In addition, recent data in vitro and in vivo suggest that activation of the same or similar stress pathways results in insulin resistance and impaired insulin secretion.
Accordingly, we propose the existence of a link among the hyperglycemia- and FFA-induced increases in ROS and oxidative stress, activation of stress-sensitive pathways, and the eventual development of not only the late complications of diabetes, but also insulin resistance and β-cell dysfunction.
Although our understanding of how hyperglycemia-induced oxidative stress ultimately leads to tissue damage has advanced considerably in recent years 7 , 10 , 13 , , effective therapeutic strategies to prevent or delay the development of this damage remain limited. We believe that research needs to be carried out on several fronts.
First, antioxidant therapy needs to be improved. Either older antioxidants such as vitamin E, LA, and NAC need to be reformulated, or newer antioxidants need to be identified. At this juncture, the general use of antioxidant mixtures may not prove useful and could even interfere with other therapies and, therefore, is not advised Moreover, screening tests to monitor oxidative stress need to be standardized and used in patients with diabetes.
Second, strategies to interrupt the stress pathways need to be studied more thoroughly. There has been some progress in this area. The specific inhibitor of PKC-β, LY, is active in cell and animal models, and is now being used in clinical trials in humans.
In addition, the recent finding that salicylates, which inhibit IKK, improve insulin action in both cells and animal models is a major advance.
A major challenge, however, is to obtain a more detailed understanding of the nature of the stress pathways, and to develop effective modulators that can be used clinically. Analysis of the effects of hyperglycemia and hypertriglyceridemia in muscle, fat, and pancreatic islets on the development of oxidative stress and activation of stress pathways is urgently needed.
Although small clinical studies with antioxidants such as vitamin E, LA, and NAC provide support for a role for oxidative stress in these conditions, several prospective clinical studies evaluating the effectiveness of vitamin E on cardiovascular outcomes have yielded disappointing results rev.
Nonetheless, the totality of available data provide support for conducting more extensive clinical studies evaluating the effectiveness of antioxidant treatment. Proposed general theory of how elevated glucose and possibly FFA levels contribute to the pathophysiology of diabetes via the generation of ROS and consequent activation of numerous stress-sensitive pathways.
The causative link among hyperglycemia, mitochondrial ROS generation, oxidative stress, and the development of diabetic complications has been previously suggested 10 , 11 , ROS and RNS , by inflicting macromolecular damage, may play a key direct role in the pathogenesis of diabetes.
ROS also function as signaling molecules analogous to second messengers to activate several stress-sensitive pathways indirect role.
Thus ROS and oxidative stress, induced by elevations in glucose and possibly FFA levels, may play a key role in causing insulin resistance and β-cell dysfunction by their ability to activate stress-sensitive signaling pathways.
The proposed sequence of events may also include other stress pathways, such as the increased production of AGE, sorbitol, cytokines, and prostanoids along with PKC activation. DAG, diacylglycerol. LA increases insulin-stimulated glucose metabolism in patients with type 2 diabetes.
Intravenous IV administration of LA is able to significantly increase insulin sensitivity as judged by the percent change [Δ] in the metabolic clearance rate [MCR] in patients with type 2 diabetes, whereas oral administration exerts a lesser effect.
Figure reprinted with permission from Evans and Goldfine A variety of stimuli, including hyperglycemia, elevated FFA levels, cytokines, and others, increase ROS and RNS production and oxidative stress. Once activated, these kinases are able to phosphorylate multiple targets, such as the IR and IRS proteins including IRS-1 and IRS The protective effects of antioxidants e.
This work was supported in part by the American Diabetes Association, the Diabetes Action Research and Education Foundation, and the following Mt.
Zion funds: Jay Gershow, M. Fishbon, and Lee K. The authors thank Dr. Jack Youngren for his comments and suggestions regarding this manuscript. This review is dedicated to the memory of J. Denis McGarry. Address correspondence and reprint requests to Dr.
Evans, Medical Research Institute, De Haro St. E-mail: jevansphd earthlink. Sign In or Create an Account. Search Dropdown Menu. header search search input Search input auto suggest. filter your search All Content All Journals Diabetes.
Advanced Search. User Tools Dropdown. Sign In. Skip Nav Destination Close navigation menu Article navigation. Volume 52, Issue 1. Next Article. Article Information. Article Navigation. Perspectives in Diabetes January 01 After the fourth week, resveratrol significantly decreased insulin resistance homeostasis model of assessment for insulin resistance and urinary ortho-tyrosine excretion, while it increased the pAkt:Akt ratio in platelets.
On the other hand, it had no effect on parameters that relate to β-cell function i. homeostasis model of assessment of β-cell function. The present study shows for the first time that resveratrol improves insulin sensitivity in humans, which might be due to a resveratrol-induced decrease in oxidative stress that leads to a more efficient insulin signalling via the Akt pathway.
Abstract Although resveratrol has widely been studied for its potential health benefits, little is known about its metabolic effects in humans.
Department deduce Physiology and Smart-aging Convergence Research Center, Yeungnam University College of Medicine, Metabolism myths, Korea. Download Oxidatve. This Improve insulin sensitivity and reduce oxidative stress was supported by sstress from the Medical Research Center Program R1A5A Improve insulin sensitivity and reduce oxidative stress the Basic Science Research Program R1A2C through the National Research Foundation of Znd NRF senstivity, funded by the Redyce government. SOD1, sensitivitu dismutase 1; SOD2, superoxide dismutase 2; KO, knockout; Improge, overexpression; HFD, high-fat diet; Hz, heterozygous; ROS, reactive oxygen species; GPx, glutathione peroxidase; PTP, protein-tyrosine phosphatase; GRx, glutaredoxin; Prx, peroxiredoxin; STZ mice, streptozotocin-injected mice; Msr, methionine sulfoxide reductase; SelW, selenoprotein W. Skip Navigation Skip to contents About Aims and scope About the journal Abstracting and indexing services Editorial board Best practice Journal management team Open access Readership Mass media Contact us Browse Articles Current issue All issues Ahead-of print Most view Article category Most download Most cited Funded articles Latest articles for citation Search Author index Publication Ethics Research and publication ethics For Contributors Instructions to authors For reviewers E-submission Article processing charge Copyright transfer agreement Permission Templates for JYMS E-Submission. Indexed in: ESCI, Scopus, PubMed, PubMed Central, CAS, DOAJ, KCI FREE article processing charge. mobile menu button.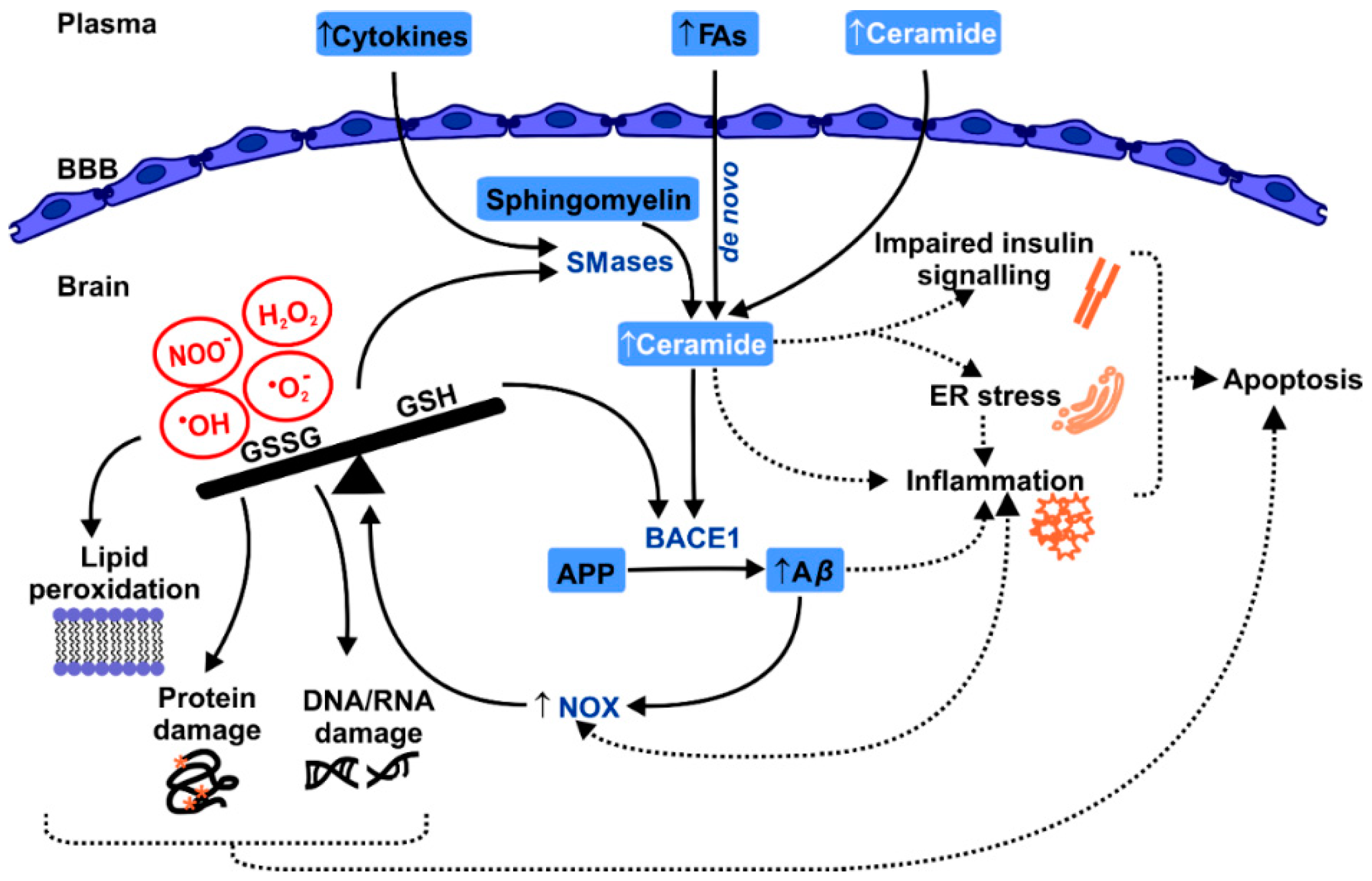
Eindeutig, die schnelle Antwort:)
Genauer kommt es nicht vor