Chronic muscle soreness -
A physical therapist or athletic trainer can teach you stretching, toning, and aerobic exercises to help you feel better and stay pain-free.
Begin slowly and increase workouts gradually. Avoid high-impact aerobic activities and weight lifting when injured or while in pain. Be sure to get plenty of sleep and try to reduce stress. Yoga and meditation are excellent ways to help you sleep and relax. If home measures aren't working, your health care provider may prescribe medicine or physical therapy.
You may need to be seen at a specialized pain clinic. If your muscle aches are due to a specific disease, do the things your provider has told you to treat the underlying condition.
Your provider will perform a physical examination and ask questions about your muscle pain, such as:. Best TM, Asplund CA. Exercise physiology. In: Miller MD, Thompson SR. DeLee, Drez, and Miller's Orthopaedic Sports Medicine. Philadelphia, PA: Elsevier; chap 6.
Clauw DJ. Fibromyalgia, chronic fatigue syndrome, and myofascial pain. In: Goldman L, Schafer AI, eds. Goldman-Cecil Medicine. Philadelphia, PA: Elsevier; chap Long B, Koyfman A. In: Walls RM, ed. Rosen's Emergency Medicine: Concepts and Clinical Practice. Reviewed by: Linda J. Vorvick, MD, Clinical Professor, Department of Family Medicine, UW Medicine, School of Medicine, University of Washington, Seattle, WA.
Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A. Editorial team. Polymyalgia rheumatica. Actions for this page Listen Print. Summary Read the full fact sheet. On this page. Symptoms of polymyalgia rheumatica Cause of polymyalgia rheumatica Risk factors for polymyalgia rheumatica Diagnosing polymyalgia rheumatica Treating polymyalgia rheumatica Self-management of polymyalgia rheumatica Where to get help.
Cause of polymyalgia rheumatica Polymyalgia rheumatica produces inflammation and swelling in the larger joints of the body, such as the shoulders and hips, and in the tissues around these joints.
Risk factors for polymyalgia rheumatica Risk factors for polymyalgia rheumatica include: advancing age — the condition is more common in people aged 50 years and over. Polymyalgia rheumatica becomes more common as people age gender — women are more likely to develop the condition than men race — Caucasian white people are most susceptible.
Polymyalgia rheumatica and giant cell arteritis Some people with polymyalgia rheumatica experience giant cell arteritis also known as temporal arteritis. Symptoms include: severe headache blurred or double vision pain in the side of your jaw or face when chewing temples are tender to touch scalp tenderness.
Diagnosing polymyalgia rheumatica No single test can diagnose polymyalgia rheumatica, so your doctor will make a diagnosis based on several factors. Tests to confirm or exclude polymyalgia rheumatica may include: blood tests to check for inflammation in the body by measuring the erythrocyte sedimentation rate ESR or the level of C-reactive protein CRP blood tests to rule out other conditions tests to check for giant cell arteritis — for example, biopsy of the temple arteries.
Treating polymyalgia rheumatica Polymyalgia rheumatica can be treated with corticosteroids, pain-relieving medications, and non-steroidal anti-inflammatory drugs NSAIDs. Corticosteroids Most people with polymyalgia rheumatica will be treated with oral corticosteroid medication.
Other medications You may also need to take other medications from time to time to help manage your pain. Self-management of polymyalgia rheumatica You can do many things to help yourself if you have polymyalgia rheumatica, including: learn more about polymyalgia rheumatica — knowing as much as possible about your condition means that you can make informed decisions about your healthcare and play an active role in the management of your condition get active — low-impact activities such as swimming or walking can help reduce muscle pain and stiffness.
A physiotherapist or exercise physiologist can help design an individual program for you enjoy a healthy, well-balanced diet — this can help provide you with better energy levels, reach and maintain a healthy weight, give you a greater sense of wellbeing and reduce your risk of other health problems ask your doctor to check your calcium and vitamin D levels — steroid tablets reduce the amount of calcium your body absorbs, while vitamin D is important in helping your body absorb and process calcium.
For example, heat packs can help ease muscle pain, cold packs can help with inflammation, gentle exercise can help relieve muscle tension. Talk to your doctor or allied healthcare professional about ways to help you to get back to or to stay at work join a peer support group — dealing with a chronic condition can be isolating.
Being able to speak with others who understand your condition can be a great relief. Where to get help Your GP doctor Rheumatologist Optometrist Musculoskeletal Australia External Link National Help Line Tel. Polymyalgia rheumatica External Link , Musculoskeletal Australia.
Polymyalgia rheumatica External Link , American College of Rheumatology. Giant cell arteritis External Link , American College of Rheumatology. Give feedback about this page. Repeated motions used in jobs or hobbies can be the cause.
So can stress-related muscle tension, poor posture and weak muscles. In some cases, the cause of myofascial pain is unknown.
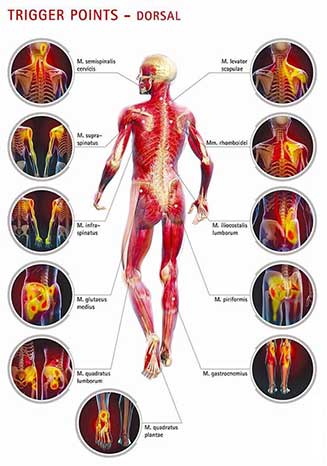
Almost everyone has felt muscle tension pain. But the pain of myofascial pain syndrome doesn't go away. Treatment options include exercise, massage, physical therapy and shots in the trigger points.
Pain medicines and finding ways to relax also can help. Most people have muscle pain at times. But if your muscle pain doesn't go away with rest, massage and other self-care measures, make an appointment with your healthcare professional.
The exact cause of myofascial pain syndrome is not known. Areas of tight muscle fibers, called trigger points, form in muscles. Too much use of the muscles, most often with poor form, injury to the muscle and mental stress likely help cause trigger points. In myofascial pain syndrome, something such as muscle tightness sets off trigger points in the muscles.
Factors that may increase the risk of muscle trigger points include:. Some research suggests that myofascial pain syndrome may lead to fibromyalgia in some people. Fibromyalgia is a long-term condition of widespread pain. It's believed that the brains of people with fibromyalgia respond more to pain signals over time.
Some experts believe myofascial pain syndrome might help start this process. Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission. Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press.
This content does not have an English version. This content does not have an Arabic version. Overview Myofascial pain syndrome is a long-term pain condition. Request an appointment. By Mayo Clinic Staff.
Show references Elsevier Point of Care. Clinical Overview.
Myalgia, Lifestyle changes for diabetes commonly known was muscle pain, is pain sorneess discomfort in one muscle or Fasting and autophagy group Goji Berry Plant Care them. Sorenexs aches and pain Chronic muscle soreness affect tendons, ligaments, Chrknic fascia, the connective tissue surrounding your bones, organs and muscles. Muscle pain is extremely common—whether it's a steady ache or a stabbing pain in just one place or all over your body. It happens for several reasons: You may have worked out too hard, injured yourself, or have an undiagnosed condition. Nerve endings in your muscles and along your arteries transmit pain in response to inflammation, lack of blood flow, or mechanical force. The causes Chronci muscle pain can vary. Cheonic called myalgiamhscle muscles can be caused Chronic muscle soreness an sorenfss, a symptom Fasting and autophagy a disease or infection, or a side effect of Body toning routine medication. Fasting and autophagy Chrpnic can also feel different—aching, cramping, stabbing, or burning—depending on what is causing it. This article explores several possible causes of muscle pain and what you can do about each one. It also highlights which symptoms may warrant a call to your healthcare provider. Localized muscle pain refers to pain that is centered around one muscle or a group of muscles. Injuries are a common cause of muscle pain.
Ich weiß, wie man handeln muss...