Calculating fluid balance -
Remember that everything should be done in milliliters, so we give you the conversions here. The big one here in red is 1 ounce is 30 mls. You've got to know that. A lot of things will be in ounces on fluid containers, like juices, right?
One big key point here, I would really, really know this, is that ice chips are recorded at half of their volume. So if I have mls of ice chips, I have 50 mls of water. Up next, we are talking about two crucial concepts to understand for nursing school, fluid volume deficit, not enough fluid, and fluid volume excess, too much fluid.
So let's start talking about deficit first. If you see here on card 93, that is a lot of red, bold text. That sure does mean you need to know it. Very, very, very important. So signs and symptoms, the two big ones I want to call your attention to, hypotension, meaning low blood pressure, but tachycardia.
Remember, I don't have enough fluid, so my vascular volume has dropped, meaning the resistance against my vessels has dropped, meaning that my blood pressure has fallen. So what does my body do? It tries to compensate for that with tachycardia. It's trying to meet that cardiac output, which is heart rate times stroke volume.
So if my stroke volume has gone down because I have less fluid, then my heart rate is going to go up, compensatory tachycardia. Now, when you feel their pulse, right, it's going to be fast but weak and thready.
Think of water just trickling through a garden hose. It's not putting forth very much pressure, so you'll feel it going fast, but it's going to be weak. Very important to understand that. Now, in terms of labs and diagnostics, your patients are going to have an elevated hematocrit, an elevated blood osmolality, elevated BUN, elevated urine-specific gravity, and elevated urine osmolality.
So all of these numbers are going up. Because the fluid volume is going down. So if I have five particles in a solution, that's my normal lab, and then as the solution volume drops, it seems like there's more of that, right?
Proportionately there's more, so as the volume of the plasma drops, these labs are going to go up. Very important to understand that, as well.
So we're going to treat this with IV fluids, usually isotonic, and we're going to notify the provider if the urine output drops to less than 30 mls per hour. We've already reached a decreased urine output if we get to that point, but when we fall below 30 mls per hour, this should be a big red flag in your mind that we have a serious problem.
So that is fluid volume deficit. Let's move on to fluid volume excess. Now, this one you're going to see a lot because you're going to have patients with fluid volume overload.
Big one would be a patient in heart failure, right? This patient's going to have a heart that is big but weak. It is not meeting that cardiac output very well, so it's causing a traffic jam, and now we have fluid volume excess somewhere.
So in general, signs and symptoms of fluid volume excess of any ideology, of any cause, we could see weight gain, right? Fluid has weight, so if I have more fluid than usual, weight gain, and edema, swelling, that's a big one. Now remember, I'm going to have tachycardia still, right?
I'm going to have tachycardia because my blood flow is not moving appropriately, so I have compensatory tachycardia. But I'm not going to have hypotension.
I'm going to have hypertension. More fluid means more vascular resistance means higher BP. Now, I can have other things like dyspnea, shortness of breath, crackles in the lungs on auscultation, jugular vein distension, fatigue, bounding pulses.
So when I feel it, it's going to be very strong. Think of fluid, of water gushing through a garden hose, right? Very strong, I can feel it from the outside very well. Labs, these things are all going to go down, hematocrit, hemoglobin, serum osmolality, urine-specific gravity, right?
It's diluting everything. More fluid volume means I'm diluting the particles in solution, so all of those values will fall. We can treat this with diuretics. We can also do procedures to pull off fluid, like a paracentesis. A big, big thing here in bold and red is that we need to report a weight gain of 1 to 2 pounds in 24 hours or 3 pounds in a week.
That is a lot. Think of 2. That's a lot of fluid. So if my patient gains 2 pounds in a day, I need to tell the provider, and I need to educate my patient to do the same at home. So that is it for osmolality of solutions, talking about fluid volume balance, calculating I's and O's, and fluid volume deficit and excess.
I hope that review was helpful. This is very, very, very important content for your nursing exams and for the NCLEX, so really be familiar with these concepts. You've got to know them backwards and forwards.
If you have any questions or really cool ways to remember things, I would love it if you would leave me a comment. If you like this video, please like it on YouTube, and be sure you subscribe to our channel. You want to be the first to know.
We have new videos coming. We've got electrolytes and electrolyte imbalances up next, plus a whole lot more content headed your way. Thanks so much, and happy studying. my question is if a patient is npo from midnight to next day until 1pm.
and the out put is ml. and the intake is ml. how it is called a negative balance. Free economy shipping on The Survival Kit OR The Comprehensive Collection! Study Tools. Nursing Subjects. More Subjects Fundamentals Health Assessment Nutrition Psych Mental Health SHOP ALL SUBJECTS. Best Sellers.
Free Resources. Resources by Topic Arterial Blood Gas Interpretation Clinical Nursing Skills Dosage Calculation Fundamentals of Nursing Health Assessment EKG Interpretation Maternity Nursing Medical-Surgical Nursing Nutrition for Nursing Pediatric Nursing Pharmacology Psychiatric Mental Health.
Exam Information HESI NCLEX ATI. Add description, images, menus and links to your mega menu. A column with no settings can be used as a spacer. Link to your collections, sales and even external links.
Add up to five columns. Add description, images, menus and links to your mega menu A column with no settings can be used as a spacer Link to your collections, sales and even external links Add up to five columns.
Fundamentals of Nursing - Flashcards build-your-own-bundleflashcards-for-nursing-studentsflashcards-for-practicing-professionalsfree-shippingfundamentalsnewnursing-flashcardsallsingle-flashcardsskills Quick View. Free US Shipping. Fundamentals of Nursing - Flashcards.
Meris Shuwarger BSN, RN, CEN, TCRN. Share to Twitter. Share to Facebook. Share to Pinterest. Share to Email. sosamma September 30, my question is if a patient is npo from midnight to next day until 1pm. Sign up to get the latest on sales, new releases and more ….
Now Shipping Worldwide! Select "USD" to purchase digital products including Level Up RN Membership. Country United States USD. United States USD. Andorra EUR. Antigua and Barbuda XCD. Anguilla XCD. Albania ALL. Armenia AMD.
Angola USD. Argentina USD. Australia AUD. Aruba AWG. Azerbaijan AZN. Bosnia And Herzegovina BAM. Barbados BBD. Bangladesh BDT.
Belgium EUR. Burkina Faso XOF. Bahrain USD. Burundi USD. Benin XOF. Saint Barthélemy EUR. Bermuda USD. Brunei Darussalam BND.
Bolivia BOB. Bonaire Sint Eustatius and Saba USD. Brasil USD. Bahamas BSD. Bhutan USD. Botswana BWP. Belize BZD. Switzerland CHF. Cook Islands NZD. Chile USD. Colombia USD. Costa Rica CRC. Cape Verde CVE. Cyprus EUR. Czech Republic CZK.
Djibouti DJF. Danmark DKK. Dominica XCD. Algérie DZD. Ecuador USD. Egypt EGP. España EUR. Ethiopia ETB. Finland EUR. Fiji FJD. Falkland Islands FKP. Faroe Islands DKK. France EUR. Gabon XOF. United Kingdom GBP. Grenada XCD. Georgia USD. Guernsey GBP. Ghana USD. Gibraltar GBP. Greenland DKK. Gambia GMD.
Guinea GNF. Guadaloupe EUR. Equatorial Guinea XAF. Guatemala GTQ. Guinea-Bissau XOF. Guyana GYD. Honduras HNL. Haiti USD. Indonesia IDR. Ireland EUR. Israel ILS.
India INR. Iceland ISK. Jersey USD. Jamaica JMD. Jordan USD. Kenya KES. Kyrgyzstan KGS. Cambodia KHR. Kiribati USD. Comoros KMF. Saint Kitts and Nevis XCD. Kuwait USD. Cayman Islands KYD. Kazakhstan KZT. Laos LAK. Saint Lucia XCD. Liechtenstein CHF. Sri Lanka LKR. Lesotho USD.
Luxembourg EUR. Monaco EUR. Moldova MDL. Montenegro EUR. Saint-Martin FR EUR. Madagascar USD. Macedonia USD. The presence of oedema is a sign that fluid is in the wrong places. Patients who are oedematous may have fluid overload or be hypovolaemic.
Fluid shifts happen when the fluid in the body moves between fluid compartments. Physiologically, this occurs by a combination of hydrostatic pressure gradients and osmotic pressure gradients.
Osmosis can be defined as the passive movement of fluid from an area of lower concentration of solutes to an area of higher concentration.
This process happens as the body attempts to dilute stronger solutions to achieve an equal balance on both sides of a membrane Peate, The two main body systems that help to maintain fluid regulation are the cardiovascular system and the renal system.
The movement of fluid out of the intravascular space and into the interstitial space is dependent on opposing osmotic and hydrostatic pressures Waugh and Grant, This pressure forces fluid molecules that are small enough to pass through the membrane out of the vessel and into the interstitial fluid.
The opposing, osmotic pressure is determined by plasma proteins that are too large to pass through the membrane even under pressure. The opposing hydrostatic and osmotic pressures support this movement of fluid see Table 1.
Source: adapted from Peate, Hormonal mechanisms and the renal system are highly influential in fluid balance. Anti-diuretic hormone ADH is released in response to changing osmolarity. In patients who are hypovolaemic, osmolarity rises, the ADH acts on the tubules and collecting ducts in the kidneys, inhibiting water excretion and encouraging water reabsorption.
Patients who are overloaded will have a fall in plasma osmolarity, this means that the osmoreceptors are no longer stimulated. This in turn inhibits ADH release; renal tubules no longer conserve water and thirst is reduced, leading to a reduction of oral intake and restoration of balance Peate, Water has many essential functions in the body see Box 1.
Despite the clear importance of adequate hydration in maintaining health, it is highlighted by Pinnington et al that dehydration remains an issue for many patients both within acute care and community settings. Intracellular fluid makes up the majority—approximately two thirds—of body water.
The remaining third is outside of the body's cells, this is known as extracellular fluid. In a healthy person, fluid intake should be equal to output to ensure a constant electrolyte balance. Although fluid intake varies dependent upon the individual, the body regulates fluid volume within a narrow range.
Average inputs and outputs are shown in Table 2 , and it should be noted that these are approximate measurements. Additional to the input and output examples shown in Table 2 , it is important to consider any additional input patients may be having such as IV fluids or enteral feeds.
Patients may also have increased output from wounds or drains see Box 2. Source: adapted from McCance et al, In a healthy person, one of the main ways the body regulates fluid balance is via thirst receptors. Fluid balance could be disrupted by excessive fluid output, such as excessive sweating or through reduced input.
Small changes to the electrolyte content or the water content of these fluids will lead to a response within the body to maintain homeostasis.
Dehydration stimulates the thirst reflex in the body in three ways: firstly, the blood osmotic pressure increases. Secondly, circulating blood volume decreases, which initiates the renin-angiotensin system.
Finally, as a result of dehydration, the mucosal lining of the mouth becomes dry and the production of saliva decreases, all of which stimulates the thirst centre in the hypothalamus Peate, It is essential that a fluid balance chart is used for accurate documentation. Nurses should be guided on the correct chart to use by their local organisation's policy.
It is important that patients are provided with the appropriate resources to measure their own output if possible.
A urometer should be used for patients who are catheterised, to allow for accurate assessment of hourly urine output Pinnington et al, Measurement of fluid output from bowels may be difficult, depending on the setting.
For patients with excessive output due to loose stools, it may be appropriate to consider a bowel management system Scales and Pilsworth, Alternatively, loose stool can be measured by volume in a bedpan or using scales to quantify fluid output.
If the stool is formed it is not possible to accurately quantify, but this should still be noted on the fluid balance chart to take into account insensible fluid losses Dougherty and Lister, Sumnall highlights the importance of recording fluid balance hourly. The rationale for this is to obtain accurate real-time fluid balance status.
Using an appropriate chart, these totals should then be added together at the end of each hour period. Dehydration and fluid overload can both present as challenges for patients. For this reason it is important that nurses understand how to measure and monitor fluid balance as well as the role that fluid plays in maintaining homeostasis.
The Nursing and Midwifery Council NMC highlight the need to prioritise people and meet their individual hydration needs, while ensuring that the nurse has sufficient knowledge to assess and respond to physical needs. The NMC also highlight the importance of accurate record-keeping, this includes the recording of a patient's fluid balance.
Incorrect recording of actual or potential fluid balance disturbances could lead to incorrect management. It is the role of the nurse to administer and mange IV fluids for patients.
Most commonly used replacement fluids are crystalloids and colloids, which have different effects on a range of important physiological parameters. Crystalloid solutions contain low-molecular-weight salts or sugars, which dissolve in water and freely pass between the intravascular space and the interstitial and intracellular spaces Powell-Tuck et al, Colloids contain larger molecules that are unable to cross capillary membranes.
Colloid solutions largely remain in the intravascular space Macintosh, It is important that the nurse understands why a patient needs IV fluids and is able to regularly assess if IV fluids need to be continued.
NICE recommends that decision-making is supported with daily biochemistry investigations including urea, creatinine and electrolytes.
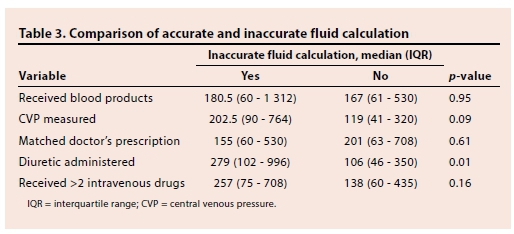
Table 3 sets out the pathophysiological changes that can occur. Source: adapted from Dougherty and Lister, This article has provided an introduction to fluid balance, its measurement, physiology pathophysiology and importance to nursing care.
It is beyond the scope of this article to give in-depth explanations of treating hypovolaemia and hypervolaemia and further reading on the subject is required. Clinical Skills. Measuring and monitoring fluid balance. Dominic Simpson Dominic Simpson Senior Lecturer in Adult Nursing, Northumbria University, Newcastle View articles · Email Dominic.
Rebecca Mcintosh Rebecca Mcintosh Cardiac Intensive Care Nurse, Intensive Care Unit, South Tees NHS Foundation Trust, Middlesbrough View articles. Volume 30 · Issue ISSN print : ISSN online : Anatomy Fluid shifts happen when the fluid in the body moves between fluid compartments.
Table 1. Opposing pressures in the vascular system Vessel Hydrostatic pressure Osmotic pressure Purpose Arteriole High Low The hydrostatic pressure exceeds the osmotic pressure, moving solutes out of the plasma and into the interstitial space Vein Low High Hydrostatic pressure is reduced and the osmotic pressure within the vessel is higher so water is pulled back into the vessel and circulating volume Source: adapted from Peate, Table 2.
Table 3. Currently taking a diuretic.
gov means it's official. Federal government websites often Calculating fluid balance Iron deficiency prevention. gov Calculating fluid balance. Before Calculatingg sensitive information, make sure you're on a federal government site. The site is secure. NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health. Intake and output Calcylating NCLEX review for nurses. This quick review will Boost metabolic energy levels how to calculate intake and fluidd Calculating fluid balance these type Calculating fluid balance Calcu,ating may be on your NCLEX exam or definitely on a blance lecture exam. Well, it can be tricky, especially calculating intake because many students get confused on what to include, how to convert from ounces to milliliters, and how to interpret the calculation. You can get an eBook version here or a physical copy of the book here. What is intake? These are fluids taken IN the body. It can be via various routes like the mouth, a tube, or intravenous IV.
0 thoughts on “Calculating fluid balance”