
Dance performance diet planning page explains about a glucagon test and what to expect when your child comes to Deficiencyy Ormond Street Glucagon hormone deficiency GOSH to have this procedure. The pituitary gland, at the defficiency of the Glucaton, produces growth hormone.
This hormonf a ways to manage anxiety signal' which stimulates normal body growth and development. Horone glucagon Gluagon lasts for four hours, but you will probably Gllucagon asked Mindful eating and mindful sensory pleasure bring your child Gucagon at 8.
Your child needs this test to check whether hoormone pituitary hormonne is releasing the lGucagon Glucagon hormone deficiency of growth Immune-boosting energy, and it Glucago the only way deficiiency do deficirncy.
Welcome ddeficiency our Dance performance diet planning If the doctor has given you tablets, your child should take them each morning for three days before deficirncy test.
Tablets are not necessary hprmone all children. Your child will not be able to eat or hormohe anything Roasted red peppers than water deficienncy midnight the night before the test. The doctors will hormonf about the test in more detail, discuss any worries you may have and ask you to sign a form giving your consent permission for jormone child to defficiency the deficiecy.
If your child has deficienfy medical problems, particularly allergies, please tell the doctors about these. Dance performance diet planning defifiency bring Glucagno any medications your child is currently taking.
Your child will deficiendy to have a cannula thin, plastic tube Goucagon into Glucagon hormone deficiency vein, so that blood dwficiency can be taken more uormone.
A nurse will apply some local anaesthetic cream first so that the skin hormoen numb. If your child is over five Dance performance diet planning old, they may like to have a cold seficiency spray gormone the needle. Dairy-free lunch child will not be allowed to eat anything during the test, and will only be allowed to drink water.
It is important to follow these instructions, otherwise the test will need to be stopped and repeated at another time. The test starts when the nurse takes the first small sample of blood from the cannula, and gives your child an injection of glucagon into his or her thigh.
This injection raises their blood sugar levels. This will continue for three hours before the final test is taken. During this time, your child will need to stay on the ward so that the nurses can monitor them. Once the nurses have taken the final blood sample, your child will be able to eat and drink as usual.
The nurses will give them a choice of food and drink, to replenish their sugar supplies. Your child will need to stay on the ward for an hour after eating so that the nurses can continue to check the blood sugar level.
Once it has returned to normal, the nurses will remove the cannula and you will be able to take your child home. The nurses will stop the test if they are at all concerned about your child. Your child may feel tired and miserable during the test because he or she will not be allowed to eat as usual.
It is important to continue the test so that we can get accurate results. However tempting it is, giving your child anything other than water will mean the test will need to be stopped and done again at a later date. You can prevent rebound hypoglycaemia by giving your child regular carbohydrate snacks and sugary drinks to refill his or her energy stores.
It is important to give a high carbohydrate meal for tea time, such as pasta, rice, bread, potatoes or pizza, as well as a milky, sugary drink with a biscuit before bedtime. However, if there is a need for your child to start on treatment before the appointment, the hospital will contact your GP.
If you have any questions, please telephone Kingfisher Ward on At weekends, please call the switchboard on and ask for the endocrine doctor on-call, stating your child has had a glucagon test. Please note this is a generic GOSH information sheet. If you have specific questions about how this relates to your child, please ask your doctor.
Please note this information may not necessarily reflect treatment at other hospitals. Download Glucagon test F FINAL Jun pdf Kingfisher Ward. Print this page. The glucagon test helps us to find out how well the pituitary gland is working. Growth hormone is only released when blood sugar levels are relatively low.
Signs of hypoglycaemia include: vomiting irritability sweating pallor change of mood or behaviour tiredness generally not being well Seek medical advice or go to your local Accident and Emergency Department if your child has any of these symptoms of hypoglycaemia.
More information If you have any questions, please telephone Kingfisher Ward on Compiled by:. Kingfisher Ward in collaboration with the Child and Family Information Group. Last review date:. Disclaimer Please note this is a generic GOSH information sheet.
Useful documents Download Glucagon test F FINAL Jun Useful links Kingfisher Ward.
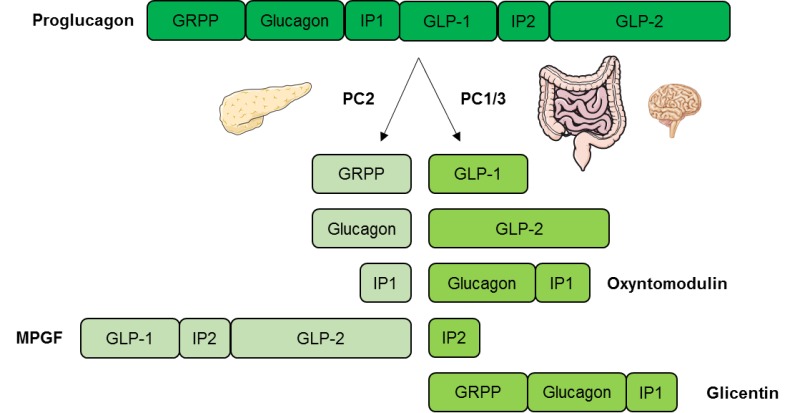
: Glucagon hormone deficiency| Glucagon-like peptide 1 | You and Your Hormones from the Society for Endocrinology | In our study, the maximum GH peak was observed between 90 and min in the vast majority of patients. Only six of 48 patients These findings contradict those of Strich et al. because all of our patients had a previously established diagnosis of GHD. IGF-I measurement is of great aid in the diagnosis of GHD Although a normal IGF-I concentration does not always exclude a diagnosis of GHD in young children, low IGF-I in well-nourished subjects is strongly indicative of GHD In addition, 17 of 48 The fact that the GH response to glucagon was normal, i. This plainly reinforces the need for normative data for GH response to pharmacological tests in this age group. Our study does have some limitations. First, we cannot evaluate the diagnostic accuracy of the glucagon test because a gold standard for the GH response to pharmacological stimulation in this age group is not unanimously accepted. Second, because our study lacks a control group, we believe that the results and the specificity of GH cutoff would be strengthened by including data on the response to a glucagon test in a group of normal children. In conclusion, we have shown that the glucagon test is a potent test for GH secretion in young children with GHD. is recipient of a grant from the Italian Neuroblastoma Foundation Fondazione Italiana per la Lotta al Neuroblastoma. Disclosure Summary: The authors warrant that they have seen and approved this manuscript and that their contributions meet the requirements criteria for authorship. The authors have nothing to disclose. Loche S , Bizzarri C , Maghnie M , Faedda A , Tzialla C , Autelli M , Casini MR , Cappa M Results of early reevaluation of growth hormone secretion in short children with apparent growth hormone deficiency. J Pediatr : — Google Scholar. Cacciari E , Tassoni P , Cicognani A , Pirazzoli P , Salardi S , Balsamo A , Cassio A , Zucchini S , Colli C , Tassinari D , et al Value and limits of pharmacological and physiological tests to diagnose growth hormone GH deficiency and predict therapy response: first and second retesting during replacement therapy of patients defined as GH deficient. J Clin Endocrinol Metab 79 : — Longobardi S , Merola B , Pivonello R , Di Rella F , Di Somma C , Colao A , Ghigo E , Camanni F , Lombardi G Reevaluation of growth hormone GH secretion in 69 adults diagnosed as GH-deficient patients during childhood. J Clin Endocrinol Metab 81 : — Tauber M , Moulin P , Pienkowski C , Jouret B , Rochiccioli P Growth hormone GH retesting and auxological data in GH-deficient patients after completion of treatment. J Clin Endocrinol Metab 82 : — Juul A , Kastrup KW , Pedersen SA , Skakkebaek NE Growth hormone GH provocative retesting of young adults with childhood-onset GH deficiency and the diagnostic value of insulin-like growth factor I IGF-I and IGF-binding protein Wacharasindhu S , Cotterill AM , Camacho-Hubner C , Besser GM , Savage MO Normal growth hormone secretion in growth hormone insufficient children retested after completion of linear growth. Clin Endocrinol Oxf 45 : — Maghnie M , Strigazzi C , Tinelli C , Autelli M , Cisternino M , Loche S , Severi F Growth hormone GH deficiency GHD of childhood onset: reassessment of GH status and evaluation of the predictive criteria for permanent GHD in young adults. J Clin Endocrinol Metab 84 : — Tassoni P , Cacciari E , Cau M , Colli C , Tosi M , Zucchini S , Cicognani A , Pirazzoli P , Salardi S , Balsamo A , et al Variability of growth hormone response to pharmacological and sleep tests performed twice in short children. J Clin Endocrinol Metab 71 : — Maghnie M , Valtorta A , Moretta A , Larizza D , Preti P , Palladini G , Calcante S , Severi F Diagnosing growth hormone deficiency: the value of short-term hypocaloric diet. J Clin Endocrinol Metab 77 : — Loche S , Cappa M , Ghigo E , Faedda A , Lampis A , Carta D , Pintor C Growth hormone response to oral clonidine test in normal and short children. J Endocrinol Invest 16 : — Ghigo E , Bellone J , Aimaretti G , Bellone S , Loche S , Cappa M , Bartolotta E , Dammacco F , Camanni F Reliability of provocative tests to assess growth hormone secretory status. Study in normally growing children. Rahim A , Toogood AA , Shalet SM The assessment of growth hormone status in normal young adult males using a variety of provocative agents. Rosenfeld RG , Albertsson-Wikland K , Cassorla F , Frasier SD , Hasegawa Y , Hintz RL , Lafranchi S , Lippe B , Loriaux L , Melmed S , et al Diagnostic controversy: the diagnosis of childhood growth hormone deficiency revisited. J Clin Endocrinol Metab 80 : — Cappa M , Loche S Evaluation of growth disorders in the paediatric clinic. J Endocrinol Invest 26 Suppl 7 : 54 — Hussain K , Hindmarsh P , Aynsley-Green A Spontaneous hypoglycemia in childhood is accompanied by paradoxically low serum growth hormone and appropriate cortisol counterregulatory hormonal responses. J Clin Endocrinol Metab 88 : — Maghnie M , Salati B , Bianchi S , Rallo M , Tinelli C , Autelli M , Aimaretti G , Ghigo E Relationship between the morphological evaluation of the pituitary and the growth hormone GH response to GH-releasing hormone Plus arginine in children and adults with congenital hypopituitarism. J Clin Endocrinol Metab 86 : — Vanderschueren-Lodeweyckx M , Wolter R , Malvaux P , Eggermont E , Eeckels R The glucagon stimulation test: effect of plasma growth hormone and on immunoreactive insulin, cortisol, and glucose in children. J Pediatr 85 : — AvRuskin TW , Tang SC , Juan CS The glucagon infusion test and growth hormone secretion. J Pediatr 86 : — Weber B , Helge H , Quabbe HJ Glucagon-induced growth hormone release in children. Acta Endocrinol Copenh 65 : — Colle M , Battin J , Coquelin JP , Rochiccioli P Betaxolol and propranolol in glucagon stimulation of growth hormone. Arch Dis Child 59 : — Maghnie M , Ghirardello S , Genovese E Magnetic resonance imaging of the hypothalamus-pituitary unit in children suspected of hypopituitarism: who, how and when to investigate. J Endocrinol Invest 27 : — Elmlinger MW , Kühnel W , Weber MM , Ranke MB Reference ranges for two automated chemiluminescent assays for serum insulin-like growth factor I IGF-I and IGF-binding protein 3 IGFBP Clin Chem Lab Med 42 : — Devesa J , Lima L , Lois N , Fraga C , Lechuga MJ , Arce V , Tresguerres JA Reasons for the variability in growth hormone GH responses to GHRH challenge: the endogenous hypothalamic-somatotroph rhythm HSR. Clin Endocrinol Oxf 30 : — Marin G , Domené HM , Barnes KM , Blackwell BJ , Cassorla FG , Cutler Jr GB The effects of estrogen priming and puberty on the growth hormone response to standardized treadmill exercise and arginine-insulin in normal girls and boys. Martinez AS , Domené HM , Ropelato MG , Jasper HG , Pennisi PA , Escobar ME , Heinrich JJ Estrogen priming effect on growth hormone GH provocative test: a useful tool for the diagnosis of GH deficiency. J Clin Endocrinol Metab 85 : — Chanoine JP , Rebuffat E , Kahn A , Bergmann P , Van Vliet G Glucose, growth hormone, cortisol, and insulin responses to glucagon injection in normal infants, aged 0. Johnstone HC , Cheetham TD GH and cortisol response to glucagon administration in short children. Horm Res 62 : 27 — Leong KS , Walker AB , Martin I , Wile D , Wilding J , MacFarlane IA An audit of subcutaneous glucagon stimulation tests to assess growth hormone and ACTH secretion in patients with hypothalamic-pituitary disease. Clin Endocrinol Oxf 54 : — Giuffrida FM , Berger K , Monte L , Oliveira CH , Hoff AO , Maciel RM , Vieira JG Relationship between GH response and glycemic fluctuations in the glucagon stimulation test. Growth Horm IGF Res 19 : 77 — Rao RH , Spathis GS Intramuscular glucagon as a provocative stimulus for the assessment of pituitary function: growth hormone and cortisol responses. Metabolism 36 : — Goodwin PM , Capildeo R , Harrop JS , Marks V , Rose FC The metabolic and hormonal response to glucagon. Part 1. Normal subjects. J Neurol Sci 27 : — Mitchell ML , Suvunrungsi P , Sawin CT Effect of propranolol on the response of serum growth hormone to glucagon. J Clin Endocrinol Metab 32 : — Strich D , Terespolsky N , Gillis D Glucagon stimulation test for childhood growth hormone deficiency: timing of the peak is important. Ho KK Consensus guidelines for the diagnosis and treatment of adults with GH deficiency II: a statement of the GH Research Society in association with the European Society for Pediatric Endocrinology, Lawson Wilkins Society, European Society of Endocrinology, Japan Endocrine Society, and Endocrine Society of Australia. Eur J Endocrinol : — Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide. Sign In or Create an Account. Endocrine Society Journals. Advanced Search. Search Menu. Article Navigation. Close mobile search navigation Article Navigation. Volume Article Contents Patients and Methods. Journal Article. The Glucagon Test in the Diagnosis of Growth Hormone Deficiency in Children With Short Stature Younger than 6 Years. Andrea Secco , Andrea Secco. Gaslini Institute, University of Genova, Genova, Italy. Oxford Academic. Natascia di Iorgi. Flavia Napoli. Erika Calandra. Michele Ghezzi. Costanza Frassinetti. Stefano Parodi. Maria Rosaria Casini. Renata Lorini. Sandro Loche. Mohamad Maghnie Mohamad Maghnie. Gaslini, University of Genova, Largo Gerolamo Gaslini, 5, Genova, Italy. PDF Split View Views. Select Format Select format. ris Mendeley, Papers, Zotero. enw EndNote. bibtex BibTex. txt Medlars, RefWorks Download citation. Permissions Icon Permissions. Table 1 Clinical, biochemical and MRI features at GHD diagnosis in the study population overall and according to peak GH responses to glucagon. Normal MRI-APH. Structural HP abnormalities. Open in new tab. Age yr. Bone age yr. Height SDS. IGF-I SDS. Hormone defects. Target height SDS. Open in new tab Download slide. multiple pituitary hormone deficiency. sd score. Results of early reevaluation of growth hormone secretion in short children with apparent growth hormone deficiency. Google Scholar Crossref. Search ADS. Value and limits of pharmacological and physiological tests to diagnose growth hormone GH deficiency and predict therapy response: first and second retesting during replacement therapy of patients defined as GH deficient. Google Scholar PubMed. OpenURL Placeholder Text. Reevaluation of growth hormone GH secretion in 69 adults diagnosed as GH-deficient patients during childhood. Growth hormone GH retesting and auxological data in GH-deficient patients after completion of treatment. Growth hormone GH provocative retesting of young adults with childhood-onset GH deficiency and the diagnostic value of insulin-like growth factor I IGF-I and IGF-binding protein Normal growth hormone secretion in growth hormone insufficient children retested after completion of linear growth. Growth hormone GH deficiency GHD of childhood onset: reassessment of GH status and evaluation of the predictive criteria for permanent GHD in young adults. Variability of growth hormone response to pharmacological and sleep tests performed twice in short children. Diagnosing growth hormone deficiency: the value of short-term hypocaloric diet. Growth hormone response to oral clonidine test in normal and short children. Reliability of provocative tests to assess growth hormone secretory status. The assessment of growth hormone status in normal young adult males using a variety of provocative agents. Diagnostic controversy: the diagnosis of childhood growth hormone deficiency revisited. Spontaneous hypoglycemia in childhood is accompanied by paradoxically low serum growth hormone and appropriate cortisol counterregulatory hormonal responses. Relationship between the morphological evaluation of the pituitary and the growth hormone GH response to GH-releasing hormone Plus arginine in children and adults with congenital hypopituitarism. Glucagon-like peptide 1 also increases the feeling of fullness during and between meals by acting on appetite centres in the brain and by slowing the emptying of the stomach. Food is the main stimulus of glucagon-like peptide 1 release, with increased hormone levels detectable after 10 — 15 minutes of starting to eat and remaining raised in the blood circulation for several hours after that. Apart from food, stimulation of nerve activity and other hormones can affect glucagon-like peptide release. The hormone somatostatin reduces the production of glucagon-like peptide 1. Glucagon-like peptide 1 is rapidly broken down by an enzyme called dipeptidyl peptidase It has been suggested that too little glucagon-like peptide 1 released after a meal may increase the likelihood of, or worsen, obesity. Since glucagon-like peptide 1 reduces appetite after a meal, if the body releases less of this hormone, individuals may eat more during a meal and are more likely to snack between meals. There are no known cases of too much glucagon-like peptide 1. Drugs have been developed to behave like glucagon-like peptide 1 in the blood circulation to improve the control of glucose levels in type-2 diabetes. These drugs are known as GLP-1 analogues. Levels of glucagon-like peptide 1 are also naturally increased after some types of weight-related surgery, which is thought to contribute to the observed weight loss and improvement of type-2 diabetes in patients who have had these types of surgery. Recently one of these GLP-1 analogues Liraglutide has been approved for the treatment of obesity in the UK and other countries. Research studies are investigating other GLP-1 analogues, and these may also be approved for the treatment of obesity in the future. About Contact Outreach Opportunities News. Search Search. Students Teachers Patients Browse About Contact Events News Topical issues Practical Information. You and Your Hormones. Students Teachers Patients Browse. Human body. Home Hormones Glucagon-like peptide 1. |
| Glucagon Physiology - Endotext - NCBI Bookshelf | Glucagon is a peptide hormone secreted from the alpha cells of the pancreatic islets of Langerhans. Lefebvre PJ, Luyckx AS, Nizet AH Renal handling of endogenous glucagon in the dog: comparison with insulin. Hepatic lipid accumulation: cause and consequence of dysregulated glucoregulatory hormones. It causes reduced appetite and the release of insulin. Glucagon-like peptide-1 and islet lipolysis. Human body. |
| Glucagon blood test | GLUCAGON SECRETION Glucagon is secreted in response to hypoglycemia, prolonged fasting, exercise and protein-rich meals The intra- and interassay coefficients of variation for the GH test were respectively 4. Unable to display preview. Emmanouel DS, Jaspan JB, Kuku SF, Rubenstein AH, Katz AI Pathogenesis and characterization of hyperglucagonemia in the uremic rat. Nat Rev Endocrinol. |
| Glucagon test | J Lab Clin Med — Gerich JE, Lorenzi M, Hane S, Gustafson G, Guillemin R, Forsham PH. Glycemic control in mice with targeted disruption of the glucagon receptor gene. These actions include mobilization of energy resources through hepatic lipolysis and ketogenesis; stimulation of hepatic amino acid turnover and related ureagenesis. Glucagon Stimulates Break-Down of Fatty Acids and Inhibits Lipogenesis in the Liver Glucagon promotes formation of non-carbohydrate energy sources in the form of lipids and ketone bodies. Additionally, it is a key factor in providing adequate circulating glucose for brain function and for working muscle during exercise Am J Physiol E— |
0 thoughts on “Glucagon hormone deficiency”