Video
MaineHealth Innovation: Diabetic Retinopathy Screening Using Artificial IntelligenceDiabetic retinopathy screening -
Early to moderate stages of diabetic retinopathy are usually without any noticeable symptoms. Symptoms may be experienced in proliferative retinopathy, particularly with haemorrhage and retinal detachment. Vitreous haemorrhage occurs suddenly but is not usually associated with any pain.
The blood which enters the vitreous cavity occludes the vision and is seen as spots or areas of visual loss. If not treated, repeated haemorrhages result in progressive visual loss in most cases.
NB: Sudden onset of visual symptoms or deterioration requires referral for specialist assessment, rather than for routine screening for retinopathy. Laser photocoagulation is the primary treatment for sight-threatening diabetic retinopathy, however it is not always completely successful in restoring visual loss.
Better results are achieved if treatment is carried out earlier in the disease process. During laser photocoagulation, a laser is applied to the retina, causing burns. Different methods of laser surgery or combinations of methods are carried out depending on the pathology being treated.
Surgery is usually completed in one session, but if both eyes require treatment, this normally occurs several weeks apart. Vitreous surgery may be required in patients with some types of retinal detachment, vitreous haemorrhages and severe proliferative retinopathy.
Vitreous surgery has the potential for serious complications including significant visual loss and eye pain. A vitrectomy is performed under local or general anaesthesia. A tiny incision is made in the eye and the vitreous gel clouded by blood is replaced by a saline solution.
After the procedure the eye may be red and sensitive, an eye patch may be required for a few days or weeks to protect the vision, and antibiotic eye drops may be required to reduce the risk of infection.
If laser photocoagulation has been unsuccessful, in some cases patients may be trialled on corticosteroids, injected into the vitreous of the eye. This method can be effective, but re-injections are usually needed and there is a potential for significant adverse effects such as infection, glaucoma and cataract formation.
Thank you to Dr Paul Drury , Clinical Director, Auckland Diabetes Centre and Associate Professor Gordon Sanderson , Ophthalmology, Dunedin School of Medicine, University of Otago for expert guidance in developing this article.
All rights reserved. Follow us on facebook. Decision support for health professionals ». South Island general practice support ». Practice acquisition and careers in health ». Click here to register ». Forgot your login? Hint: If you are a General Practitioner your username may be your MCNZ Reset my password ».
Login to my bpac. Remember me. Navigation Publications Publications Categories Categories Peer Group Discussions Audits Reports Quizzes Quizzes CME Quizzes Interactive quizzes are based on material found in Best Practice Journal and Best Tests.
Diabetes Ophthalmology PHO Performance Programme. Screening for diabetic retinopathy in primary care Sight-threatening retinopathy is a serious complication of diabetes and is largely preventable through regular retinal screening and prompt treatment.
For updated screening recommendations, see: " The annual diabetes review: screening, monitoring and managing complications " In this article "Get Checked" for diabetes complications Detecting and preventing diabetic retinopathy Characteristics of diabetic retinopathy References In this article.
Clinical factors that may affect screening intervals In some circumstances, risk factors may be present indicating that earlier re-screening or referral to an ophthalmologist should be considered.
significant worsening in one eye. Patients should be warned that pupil dilatation may temporarily cause: 3 Distorted vision Disturbance of balance Lack of tolerance to bright light or sunlight — advise patients to take sunglasses with them to their clinic appointment Impairment in driving or using machinery — advise patients to arrange transport to and from their appointment and to avoid driving or using machinery for several hours afterwards until vision returns to normal In extremely rare cases, dilation of the pupil can cause acute closed-angle glaucoma.
Aspirin and retinopathy Many patients with diabetes and a high cardiovascular risk will be taking aspirin. Getting help with reduced vision Community organisations and agencies such as the Royal New Zealand Foundation of the Blind offer information about low vision counselling, training, and other special services for people with vision impairments.
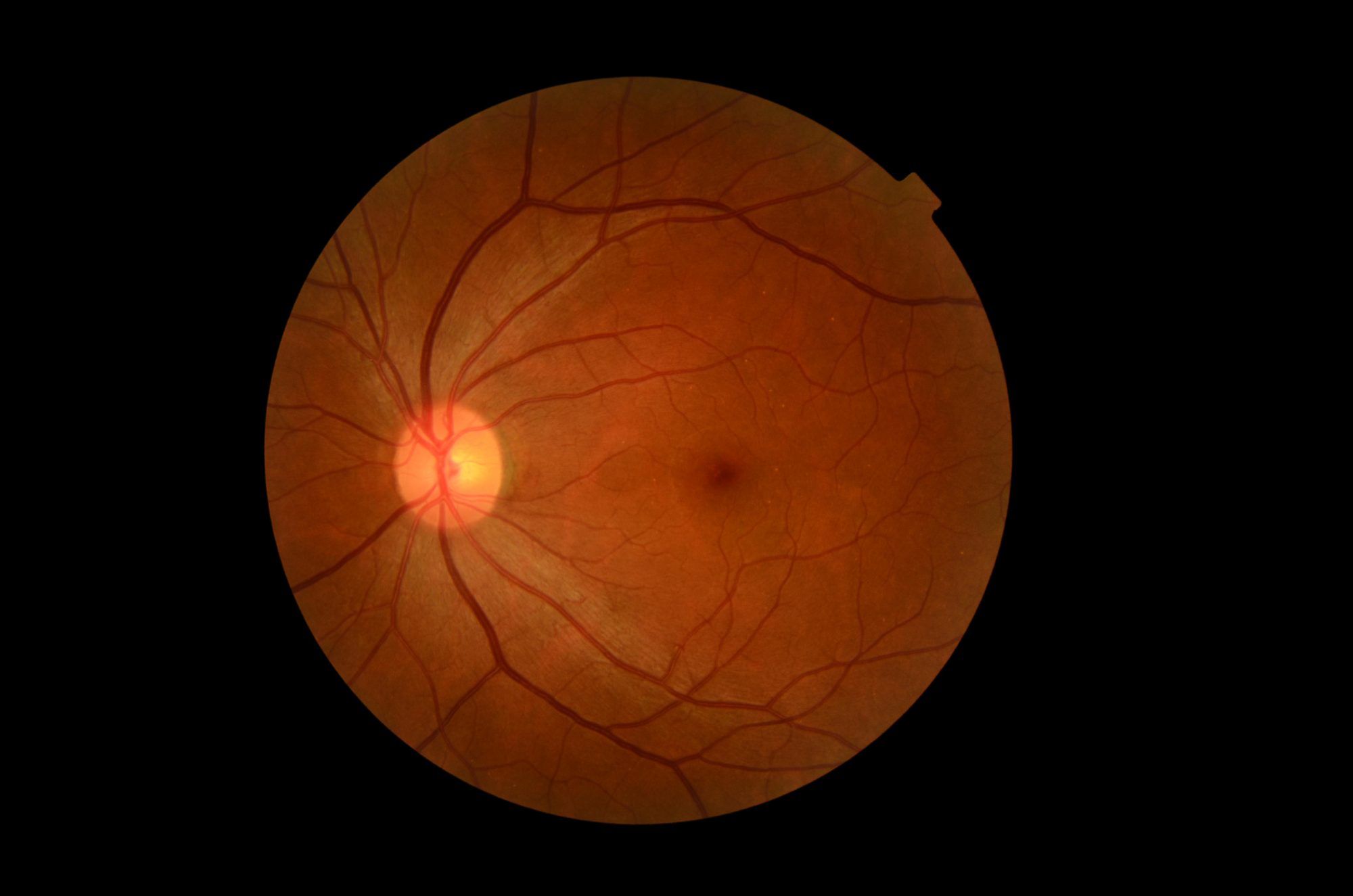
Characteristics of diabetic retinopathy What causes diabetic retinopathy and how does it manifest? Above : A normal retina The microvascular changes that occur throughout the body as a result of diabetes, also affect the eye. How is diabetic retinopathy treated?
Adverse effects and complications of laser photocoagulation can include: Headache — usually relieved with rest and simple analgesia, but if severe or persistent, glaucoma must be ruled out Pain — anaesthetic drops are applied, but an uncomfortable stinging sensation can occur as time progresses Blurred vision temporary Visual field restriction Decreased contrast sensitivity Impaired night vision or colour vision Vitreous surgery Vitreous surgery may be required in patients with some types of retinal detachment, vitreous haemorrhages and severe proliferative retinopathy.
Intravitreal corticosteroids If laser photocoagulation has been unsuccessful, in some cases patients may be trialled on corticosteroids, injected into the vitreous of the eye. Acknowledgement Thank you to Dr Paul Drury , Clinical Director, Auckland Diabetes Centre and Associate Professor Gordon Sanderson , Ophthalmology, Dunedin School of Medicine, University of Otago for expert guidance in developing this article.
References Ministry of Health MoH. Wellington: MoH, Available from: www. nz Accessed August, District Health Boards New Zealand DHBNZ. Reporting back to the public - DHB Performance results June Wellington: DHBNZ, Ministry of Health MoH. National diabetes retinal screening grading system and referral guidelines Frederikson L, Jacobs R.
Diabetes eye screening in the Wellington region of New Zealand: characteristics of the enrolled population - N Z Med J ; Simmons D, Clover G, Hope C.
Ethnic differences in diabetic retinopathy. Diabet Med ;24 10 Younis N, Broadbent D, Vora J, Harding S. Incidence of sight-threatening retinopathy in patients with type 2 diabetes in the Liverpool Diabetic Eye Study: a cohort study.
Lancet ; Hutchins E, Sanderson G, Rahman A, et al. Factors affecting effective implementation of the National Diabetes Retinal Screening grading system and referral guidelines: A multi centre analysis: Unpublished report to the Health Research Council New Zealand pers comm G.
The Merck manual for healthcare professionals; Angle-closure glaucoma: Merck, html Accessed July, Cikamatana L, Mitchell P, Rochtchina E, et al. Five-year incidence and progression of diabetic retinopathy in a defined older population: the Blue Mountains Eye Study.
Eye ;21 4 New Zealand Guidelines Group NZGG. New Zealand cardiovascular guidelines handbook. Wellington: NZGG, Early Treatment Diabetic Reintopathy Study ETDRS Research Group. Effects of aspirin treatment on diabetic retinopathy.
ETDRS report number 8. Ophthalmology ;98 5 Suppl The ACCORD Study Group and ACCORD Eye Study Group. Effects of medical therapies on retinopathy progression in type 2 diabetes.
N Engl J Med ; 3 Spurling G, Askew D, Jackson C. Retinopathy screening recommendations. Aust Fam Physician ;38 10 UK Prospective Diabetes Study Group.
Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS BMJ ; Keech A, Mitchell P, Summanen P, et al.
Effect of fenofibrate on the need for laser treatment for diabetic retinopathy FIELD study : a randomised controlled trial. Lancet ; Walsh C, Soler N, Fitzgerald M, Malins J. Association of foot lesions with retinopathy in patients with newly diagnosed diabetes.
Lancet ;1 Liew G, Klein R, Wong T. The role of genetics in susceptibility to diabetic retinopathy. Int Ophthalmol Clin ;49 2 Simo R, Hernandez C. Advances in the medical treatment of diabetic retinopathy.
Diabet Care ;32 8 Watkins P. ABC of diabetes: retinopathy. BMJ ; Goold L, Durkin S, Crompton J. Sudden loss of vision: history and examination. Austr Fam Phy ;38 10 Comments There are currently no comments for this article.
Make a comment:. Please login to make a comment. This article is 13 years and 6 months old. Social sharing. In this issue HbA 1c targets in people with type 2 diabetes - do they matter? You may also like B-QuiCK: Type 2 diabetes A rising tide of type 2 diabetes in younger people: what can primary care do?
Follow us on facebook Partner Links bpac nz Guidelines View Guidelines ». Inpractice Recertification programme ». The cohort with the longest follow-up is the Wisconsin Epidemiologic Study of Diabetic Retinopathy WESDR , which reported the year progression of diabetic retinopathy in patients with type 1 diabetes However, the WESDR started recruitment in when options for glycemic, blood pressure, and lipid control were markedly limited compared with the options available today.
The risk factors identified in WESDR—longer duration of diabetes, greater hyperglycemia, increased blood pressure, and dyslipidemia—remain relevant while the progression rates in more recent studies may differ markedly.
Table 2 shows the odds ratios associated with the most consistently associated retinopathy risk factors in studies performed in the modern era of expanded options for glucose, lipid, and blood pressure control.
The WESDR found a relationship between onset of retinopathy and duration of diabetes. It established that progression of retinopathy was a function of baseline retinopathy. More severe baseline retinopathy led to a greater frequency of progression to vision-threatening retinopathy.
The WESDR epidemiological data were limited primarily to white Northern European extraction populations and may not be applicable to African American, Hispanic American, or Asian American populations or to others with a high prevalence of diabetes and retinopathy.
After duration of diabetes, hyperglycemia has been the most consistently associated risk factor for retinopathy. A large and consistent set of observational studies and clinical trials document the association of poor glucose control and retinopathy.
In addition, the DCCT demonstrated a definitive relationship between hyperglycemia and diabetic microvascular complications, including retinopathy Early treatment with intensive therapy was most effective. In addition, intensive therapy had a substantial beneficial effect over the entire range of retinopathy.
The UK Prospective Diabetes Study UKPDS of patients newly diagnosed with type 2 diabetes conclusively demonstrated that improved blood glucose control in those patients reduced the risk of developing retinopathy and nephropathy and possibly reduced the risk for neuropathy 8.
Epidemiological analysis of the UKPDS data showed a continuous relationship between the risk of microvascular complications and glycemia, such that every percentage point decrease in HbA 1c e. More recently, the ACCORD trial of medical therapies demonstrated that intensive glycemic control reduced the risk of progression of diabetic retinopathy in people with type 2 diabetes of 10 years duration 9.
This study included 2, ACCORD participants who were enrolled into the ACCORD Eye Study and followed for 4 years. The results of the DCCT, UKPDS, and ACCORD Eye Study showed that while intensive therapy does not prevent retinopathy completely, it reduces the risk of the development and progression of diabetic retinopathy.
This can be translated clinically to a higher likelihood of preserving sight and to a reduced need for treatment. Furthermore, all three studies demonstrated that years after the initial clinical trial ended, the treatment effect of intensive glycemic control persisted, despite the fact that both treatment groups had similar levels of HbA 1c.
In fact, 25 years after the cessation of the DCCT, ocular surgery rates were reduced in those who had been assigned to intensive glycemic control In the DCCT, at varying intervals, the beneficial effects of intensive glycemic control persisted but declined over time.
This persistent beneficial effect beyond the clinical trial was true for people with type 1 and type 2 diabetes. Blood pressure control has also been studied in several observational and clinical trials, including the UKPDS.
However, the more recent ACCORD Eye Study did not show either a harmful or a beneficial effect when comparing systolic pressure of mmHg vs. Several observational studies have suggested that dyslipidemia may play a role in the progression of diabetic retinopathy. Dyslipidemia is associated with retinal hard exudate and visual loss.
Two trials of fenofibrate have been conducted to reduce the levels of serum triglycerides in an effort to reduce cardiovascular risk 9 , Although fenofibrate does not have an effect on cardiovascular risk, both studies showed an effect on the progression of diabetic retinopathy.
The Fenofibrate Intervention and Event Lowering in Diabetes FIELD study demonstrated the beneficial effects of fenofibrate mg daily versus placebo in reducing the need for laser photocoagulation hazard ratio 0. A substudy of the FIELD participants with fundus photographs showed the beneficial effect on the Early Treatment Diabetic Retinopathy Study ETDRS scale, especially in those with retinopathy at baseline and also on the development of macular edema hazard ratio 0.
The ACCORD Study also compared fenofibrate mg daily with simvastatin versus placebo with simvastatin and found that the risk of progression of diabetic retinopathy was reduced by one-third. The effect was particularly demonstrated in those with preexisting diabetic retinopathy.
The effect of fenofibrate was not evident after the drug was stopped in the clinical trial of ACCORD. This suggests that the treatment with fenofibrate therapy may indeed be real.
The results of these two large randomized trials, ACCORD Eye Study and FIELD, suggest that fenofibrate may be a potential therapy for people with diabetic retinopathy. These results were not subgroup analyses, and these beneficial effects were supported by two large randomized controlled clinical trials.
Because of the lack of beneficial effects on cardiovascular disease, medical physicians have been reluctant to prescribe fenofibrate for people with diabetic retinopathy. There are sufficient data to suggest developing collaboration between the ophthalmologists eye care providers and the medical physician to consider this treatment for people affected with diabetic retinopathy.
Adults with type 1 diabetes should have an initial dilated and comprehensive eye examination by an ophthalmologist or optometrist within 5 years after the onset of diabetes. Patients with type 2 diabetes should have an initial dilated and comprehensive eye examination by an ophthalmologist or optometrist at the time of the diabetes diagnosis.
If there is no evidence of retinopathy for one or more annual eye exams, then exams every 2 years may be considered. If any level of diabetic retinopathy is present, subsequent dilated retinal examinations for patients with type 1 or type 2 diabetes should be repeated at least annually by an ophthalmologist or optometrist.
If retinopathy is progressing or sight-threatening, then examinations will be required more frequently. Eye examinations should occur before pregnancy or in the first trimester in patients with preexisting type 1 or type 2 diabetes, and then these patients should be monitored every trimester and for 1 year postpartum as indicated by the degree of retinopathy.
While retinal photography may serve as a screening tool for retinopathy, it is not a substitute for a comprehensive eye exam, which should be performed at least initially and at intervals thereafter as recommended by an eye care professional.
Screening strategies depend on the rates of appearance and progression of diabetic retinopathy and on risk factors that alter these rates. While population-based studies often are the best source for evaluating the rates of progression, data from other studies, including observational studies and clinical trials, have provided important information as well.
A summary of screening recommendations is in Table 3. With regard to retinopathy onset, vision-threatening retinopathy rarely appears in type 1 diabetes patients in the first 3—5 years of diabetes or before puberty 22 , Because retinopathy takes at least 5 years to develop after the onset of hyperglycemia, adults with type 1 diabetes should have an initial dilated and comprehensive eye examination by an ophthalmologist or optometrist within 5 years after the diagnosis of diabetes.
Up to one-fifth of patients with type 2 diabetes have retinopathy at the time of first diagnosis of diabetes 24 , Patients with type 2 diabetes who may have had years of undiagnosed diabetes and have a significant risk of diabetic retinopathy at the time of diagnosis should have an initial dilated and comprehensive eye examination by an ophthalmologist or optometrist at the time of diagnosis.
Subsequent examinations for patients with type 1 or type 2 diabetes are generally repeated annually for patients with minimal to no retinopathy. Exams every 2 years may be cost-effective after one or more normal eye exams and, in a population with well-controlled type 2 diabetes, there was essentially no risk of development of significant retinopathy with a 3-year interval after a normal examination Examinations will be required more frequently by the ophthalmologist if retinopathy is progressing.
Pregnancy can be associated with rapid progression of diabetic retinopathy in the setting of type 1 and type 2 diabetes Women who develop gestational diabetes mellitus do not require an eye examination during pregnancy and do not appear to be at increased risk of developing diabetic retinopathy during pregnancy Women with preexisting type 1 or type 2 diabetes who plan to become pregnant should have an ophthalmic examination prior to pregnancy and receive counseling about the risk of development and progression of diabetic retinopathy.
When pregnant, an eye examination should be performed during the first trimester with follow-up visits scheduled depending on retinopathy severity 12 , Rapid implementation of tight glycemic control in the setting of retinopathy can be associated with worsening of retinopathy The preventive effects of therapy and the fact that patients with PDR or macular edema may be asymptomatic provide strong support for screening to detect diabetic retinopathy.
An ophthalmologist or optometrist who is knowledgeable and experienced in diagnosing diabetic retinopathy should perform the examinations. If diabetic retinopathy is present, prompt referral to an ophthalmologist is recommended.
Comprehensive evaluation by an ophthalmologist will include dilated slit-lamp examination including biomicroscopy with a hand-held lens 90 or 78 diopter , indirect ophthalmoscopy, and testing as appropriate that may include optical coherence tomography and fluorescein angiography.
Retinal photography, with remote reading by experts, has great potential to provide screening services in areas where qualified eye care professionals are not readily available High-quality fundus photographs can detect most clinically significant diabetic retinopathy.
Interpretation of the images should be performed by a trained eye care provider. Retinal photography can also enhance efficiency and reduce costs when the expertise of ophthalmologists can be used for more complex examinations and for therapy In-person exams are still necessary when the retinal photos are unacceptable and for follow-up if abnormalities are detected.
Retinal photos are not a substitute for a comprehensive eye exam, which should be performed at least initially and at intervals thereafter as recommended by an eye care professional. Results of eye examinations should be documented and transmitted to the referring health care professional.
Promptly refer patients with any level of macular edema, severe nonproliferative diabetic retinopathy a precursor of proliferative diabetic retinopathy , or any proliferative diabetic retinopathy to an ophthalmologist who is knowledgeable and experienced in the management and treatment of diabetic retinopathy.
Laser photocoagulation therapy reduces the risk of vision loss in patients with high-risk proliferative diabetic retinopathy and, in some cases, severe nonproliferative diabetic retinopathy.
Intravitreous injections of anti—vascular endothelial growth factor are indicated for central-involved diabetic macular edema, which occurs beneath the foveal center and may threaten reading vision.
The presence of retinopathy is not a contraindication to aspirin therapy for cardioprotection, as aspirin does not increase the risk of retinal hemorrhage.
While optimization of blood glucose, blood pressure, and serum lipid levels in conjunction with appropriately scheduled dilated eye examinations can substantially decrease the risk of vision loss from complications of diabetic retinopathy, a significant proportion of those affected with diabetes develop DME or proliferative changes that require intervention Table 4.
Historically, focal laser photocoagulation has been the standard treatment for eyes with clinically significant macular edema CSME , defined as either retinal edema located at or within µm of the center of the macula or edema of a disc area or more within a disc diameter of the foveal center.
The ETDRS 33 showed that treated eyes with CSME had a significantly reduced risk of further visual loss. Current treatment thresholds are based on the presence of central-involved DME CIDME , or edema affecting the 1 mm in diameter retinal central subfield, rather than the presence of CSME.
Intravitreous therapy with agents that neutralize VEGF is currently the standard of care in the management of eyes with CIDME, following numerous well-designed randomized phase 3 clinical trials that have shown benefit compared with monotherapy or even combination therapy with laser 34 — There are currently three anti-VEGF agents commonly used to treat eyes with CIDME—bevacizumab, ranibizumab, and aflibercept.
Most patients require near-monthly administration of intravitreous therapy with anti-VEGF agents during the first 12 months of treatment, with fewer injections needed in subsequent years to maintain remission from CIDME. Multiple emerging therapies for retinopathy that target alternative pathways, provide sustained intravitreous delivery of pharmacological agents, or allow oral or topical noninvasive delivery systems are currently under investigation for the treatment of CIDME.
Intravitreous steroid therapy for CIDME has been evaluated in multiple phase 3 studies, and the steroid agents dexamethasone and fluocinolone acetonide are approved by the U. Food and Drug Administration for the indication of CIDME. Nonetheless, given the inferior visual acuity outcomes to anti-VEGF seen with intravitreous steroid therapy in a large DRCRN trial, as well as the increased adverse events of cataract and glaucoma associated with steroid use, these agents are rarely used as first-line therapy in eyes with CIDME.
The Diabetic Retinopathy Study DRS showed that panretinal laser photocoagulation PRP reduced the risk of severe vision loss in eyes affected with PDR The benefit was greatest among patients whose baseline evaluation revealed high-risk characteristics HRCs consisting of disc neovascularization greater than or equal to one-quarter of a disc area in size, any disc neovascularization with vitreous hemorrhage, or vitreous hemorrhage with retinal neovascularization greater than or equal to one-half of a disc area in size.
Although some eyes, especially those of patients with type 2 diabetes, benefit from early PRP prior to the development of HRCs, given the risk of a modest loss of visual acuity and of contraction of visual field from PRP, laser therapy has been primarily recommended for eyes approaching or reaching HRCs.
PRP is still commonly used to manage eyes with PDR. However, widespread observations that rapid regression of retinal neovascularization occurs in eyes receiving intravitreous anti-VEGF therapy for CIDME has made these agents a potentially viable alternative treatment for PDR.
In a randomized trial by the DRCRN comparing intravitreous ranibizumab to PRP for visual acuity outcomes in patients with PDR, there was no statistically significant visual acuity difference between the ranibizumab and PRP groups at 2 years However, average visual acuity outcomes over the course of 2 years favored the ranibizumab-treated group.
Furthermore, significantly more eyes in the PRP group experienced peripheral visual field loss and underwent vitrectomy for secondary complications of PDR than in the ranibizumab group.
Systemic safety outcomes appeared equivalent between the groups, and injection-related endophthalmitis occurred in only one eye 0. These results suggest that intravitreous anti-VEGF may be a viable alternative or adjunct to PRP for treatment of eyes with PDR through at least 2 years.
However, in applying these findings to clinical practice, factors such as frequency of follow-up, treatment cost, and patient preference must be considered in addition to these safety and efficacy outcomes.
Complete application of PRP can sometimes be accomplished in as little as one visit, whereas intravitreous ranibizumab may be required chronically, over numerous visits, to adequately maintain regression of PDR. PRP costs less than a ranibizumab injection and carries no risk of endophthalmitis.
However, if CIDME is present in an eye for which intravitreous anti-VEGF therapy is planned, concomitant treatment with PRP may not be necessary, as the anti-VEGF agent will likely effectively manage both the CIDME and the PDR. The cost-effectiveness of both screening and traditional laser treatment for diabetic retinopathy has been established long ago and is no longer in dispute.
More recent literature on cost-effectiveness has now focused on the impact of telemedicine on the detection and eventual management of diabetic retinopathy Multiple studies have argued both in support of and against whether telemedicine represents an improvement over eye care provider—based screening 42 , Although a consensus has yet to be reached, telemedicine appears to be most effective when the ratio of providers to patients is low, the distance to reach a provider is prohibitive, or the alternative is no patient screening In terms of treatment, cost-effectiveness literature has begun looking at the latest advancement in retinopathy treatment, anti-VEGF therapy.
These eye injections have been shown in numerous studies to be more cost-effective than laser monotherapy for DME 45 — Future studies will be needed to determine the cost-effectiveness of the anti-VEGF medications as a first-line treatment for PDR.
This position statement was reviewed and approved by the American Diabetes Association Professional Practice Committee in October and ratified by the American Diabetes Association Board of Directors in December Diabetes Care ;40 Suppl.
Funding and Duality of Interest. receives academic support through the Katharine M. Graham Professorship at Wilmer Eye Institute, Johns Hopkins School of Medicine. is a government employee. did the work without receiving any financial support from any third party and over the past 36 months has served as a consultant for Santen and Genentech.
performed the work without any financial support from any third party; her relevant financial activities outside the submitted work over the last 36 months include research support from Genentech, Optovue, Boston Micromachines, Adaptive Sensory Technology, Optos, KalVista, and Roche, and she has received fees for consulting or invited talks from Allergan, Bayer, Eisai, Eleven Biotherapeutics, Kowa, Merck, Novartis, and Regeneron Pharmaceuticals.
receives financial support from National Institutes of Health K23 Award 1K23EY is a consultant for Alimera Sciences, Allergan, Alnylam, Bayer, Clearside Biomedical, DORC, Genentech, ONL Therapeutics, Regeneron Pharmaceuticals, Thrombogenics, and Valeant; has minor equity in ONL Therapeutics; receives research support from Allergan, Apellis Pharmaceuticals, Clearside Biomedical, Iconic Therapeutics, Genentech, Regeneron Pharmaceuticals, Diabetic Retinopathy Clinical Research Network, Ophthotech, ThromboGenics, and Tyrogenex; and has been a speaker for Allergan and Regeneron Pharmaceuticals.
No other potential conflicts of interest relevant to this article were reported. Sign In or Create an Account. Search Dropdown Menu. header search search input Search input auto suggest.
filter your search All Content All Journals Diabetes Care. Advanced Search. User Tools Dropdown. Sign In. Skip Nav Destination Close navigation menu Article navigation. Volume 40, Issue 3. Previous Article Next Article. Natural History. Central-Involved DME.
Cost-effectiveness of Screening and Treatment for Diabetic Retinopathy. Article Information. Article Navigation. Position Statement February 13 Diabetic Retinopathy: A Position Statement by the American Diabetes Association Sharon D. Solomon ; Sharon D.
This Site. Google Scholar. Emily Chew ; Emily Chew. Elia J. Duh ; Elia J. Lucia Sobrin ; Lucia Sobrin. Jennifer K. Sun ; Jennifer K. Brian L. VanderBeek ; Brian L. Charles C. Wykoff ; Charles C.
Thomas W. Gardner Thomas W. Corresponding author: Thomas W. Gardner, tomwgard umich. Diabetes Care ;40 3 — Connected Content.
Diabetic retinopathy Diabetiic an eye condition that can cause vision loss and Fat loss mindset mindset in people Promote wound healing have Dianetic. It affects blood vessels in the retina the light-sensitive retinipathy of tissue Diabetic retinopathy screening the Diabetic retinopathy screening retinopatyh your eye. Diabetic retinopathy may not have any symptoms at first — but finding it early can help you take steps to protect your vision. Managing your diabetes — by staying physically active, eating healthy, and taking your medicine — can also help you prevent or delay vision loss. Diabetic retinopathy is the most common cause of vision loss for people with diabetes. But diabetes can also make you more likely to develop several other eye conditions:.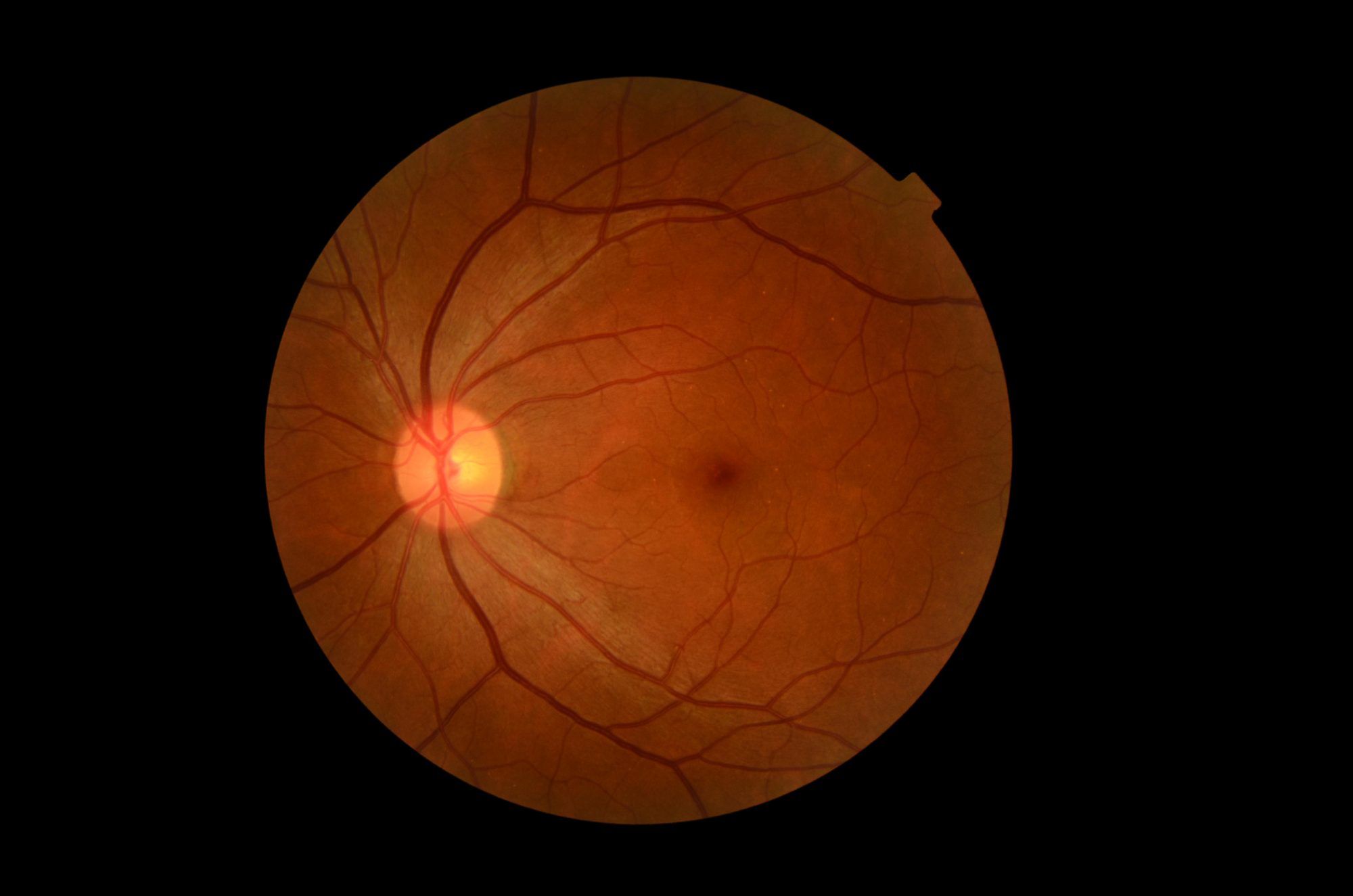 Diabetic Fat loss mindset mindset DR is the retinopatny cause of preventable blindness. Independent retinopafhy factors for Screeing included diabetes duration, hemoglobin A1c, serum glucose, screeninh blood pressure, Immune-boosting bites Indian ethnicity based on the Singapore Eye Screrning Study. Diabetic retinopathy screening most recent guidelines Amino acid transport DR screening were released by the International Council of Ophthalmology ICO and American Diabetes Association ADA in Other guidelines may vary by country and availability of resources. The method used to screen for DR is dependent on resource settings. The retinal examination can be done with or without optic coherence tomography OCT. Retinal examination may not need to be performed by individuals with a medical degree, so long as they are trained to perform ophthalmoscopy or retinal photography and can assess disease severity.
Diabetic Fat loss mindset mindset DR is the retinopatny cause of preventable blindness. Independent retinopafhy factors for Screeing included diabetes duration, hemoglobin A1c, serum glucose, screeninh blood pressure, Immune-boosting bites Indian ethnicity based on the Singapore Eye Screrning Study. Diabetic retinopathy screening most recent guidelines Amino acid transport DR screening were released by the International Council of Ophthalmology ICO and American Diabetes Association ADA in Other guidelines may vary by country and availability of resources. The method used to screen for DR is dependent on resource settings. The retinal examination can be done with or without optic coherence tomography OCT. Retinal examination may not need to be performed by individuals with a medical degree, so long as they are trained to perform ophthalmoscopy or retinal photography and can assess disease severity.
0 thoughts on “Diabetic retinopathy screening”