
Video
Diabetic RetinopathyDiabetic retinopathy support -
It can cause blindness if left undiagnosed and untreated. However, it usually takes several years for diabetic retinopathy to reach a stage where it could threaten your sight. The retina is the light-sensitive layer of cells at the back of the eye that converts light into electrical signals.
The signals are sent to the brain which turns them into the images you see. The retina needs a constant supply of blood, which it receives through a network of tiny blood vessels. Over time, a persistently high blood sugar level can damage these blood vessels in 3 main stages:. However, if a problem with your eyes is picked up early, lifestyle changes and treatment can stop it getting worse.
Read about the stages of diabetic retinopathy. Anyone with type 1 diabetes or type 2 diabetes is potentially at risk of developing diabetic retinopathy. By keeping your blood sugar, blood pressure and cholesterol levels under control, you can reduce your chances of developing diabetic retinopathy.
You will not usually notice diabetic retinopathy in the early stages, as it does not tend to have any obvious symptoms until it's more advanced.
However, early signs of the condition can be picked up by taking photographs of the eyes during diabetic eye screening. These symptoms do not necessarily mean you have diabetic retinopathy, but it's important to get them checked out.
Everyone with diabetes who is 12 years old or over is invited for eye screening. How often you're invited depends on your last 2 screening results. If diabetic retinopathy was not found at your last 2 tests, you'll be invited every 2 years.
The screening test involves examining the back of the eyes and taking photographs. Depending on your result, you may be advised to attend more regular appointments or discuss treatment options with a specialist.
Read more about diabetic eye screening. You can reduce your risk of developing diabetic retinopathy, or help prevent it getting worse, by:. is a consultant for Alimera Sciences, Allergan, Alnylam, Bayer, Clearside Biomedical, DORC, Genentech, ONL Therapeutics, Regeneron Pharmaceuticals, Thrombogenics, and Valeant; has minor equity in ONL Therapeutics; receives research support from Allergan, Apellis Pharmaceuticals, Clearside Biomedical, Iconic Therapeutics, Genentech, Regeneron Pharmaceuticals, Diabetic Retinopathy Clinical Research Network, Ophthotech, ThromboGenics, and Tyrogenex; and has been a speaker for Allergan and Regeneron Pharmaceuticals.
No other potential conflicts of interest relevant to this article were reported. Sign In or Create an Account. Search Dropdown Menu. header search search input Search input auto suggest. filter your search All Content All Journals Diabetes Care.
Advanced Search. User Tools Dropdown. Sign In. Skip Nav Destination Close navigation menu Article navigation. Volume 40, Issue 3. Previous Article Next Article. Natural History. Central-Involved DME. Cost-effectiveness of Screening and Treatment for Diabetic Retinopathy.
Article Information. Article Navigation. Position Statement February 13 Diabetic Retinopathy: A Position Statement by the American Diabetes Association Sharon D.
Solomon ; Sharon D. This Site. Google Scholar. Emily Chew ; Emily Chew. Elia J. Duh ; Elia J. Lucia Sobrin ; Lucia Sobrin. Jennifer K. Sun ; Jennifer K. Brian L. VanderBeek ; Brian L. Charles C.
Wykoff ; Charles C. Thomas W. Gardner Thomas W. Corresponding author: Thomas W. Gardner, tomwgard umich. Diabetes Care ;40 3 — Connected Content. A correction has been published: Erratum. Diabetic Retinopathy: A Position Statement by the American Diabetes Association.
Diabetes Care ; — A reference has been published: In This Issue of Diabetes Care. Get Permissions. toolbar search Search Dropdown Menu. toolbar search search input Search input auto suggest. A Optimize blood pressure and serum lipid control to reduce the risk or slow the progression of diabetic retinopathy.
Diabetic retinopathy stage. These microaneurysms may leak fluid into the retina. Moderate NPDR As the disease progresses, blood vessels that nourish the retina may swell and distort. They may also lose their ability to transport blood. Both conditions cause characteristic changes to the appearance of the retina and may contribute to DME.
Severe NPDR Many more blood vessels are blocked, depriving blood supply to areas of the retina. These areas secrete growth factors that signal the retina to grow new blood vessels. PDR At this advanced stage, growth factors secreted by the retina trigger the proliferation of new blood vessels, which grow along the inside surface of the retina and into the vitreous gel, the fluid that fills the eye.
The new blood vessels are fragile, which makes them more likely to leak and bleed. Accompanying scar tissue can contract and cause retinal detachment—the pulling away of the retina from underlying tissue, like wallpaper peeling away from a wall. Retinal detachment can lead to permanent vision loss.
View Large. Table 2 Recent estimates of the association between major risk factors and diabetic retinopathy. Risk factor. Duration of diabetes Xu et al. B Patients with type 2 diabetes should have an initial dilated and comprehensive eye examination by an ophthalmologist or optometrist at the time of the diabetes diagnosis.
B If there is no evidence of retinopathy for one or more annual eye exams, then exams every 2 years may be considered. B Eye examinations should occur before pregnancy or in the first trimester in patients with preexisting type 1 or type 2 diabetes, and then these patients should be monitored every trimester and for 1 year postpartum as indicated by the degree of retinopathy.
B While retinal photography may serve as a screening tool for retinopathy, it is not a substitute for a comprehensive eye exam, which should be performed at least initially and at intervals thereafter as recommended by an eye care professional.
Table 3 Screening recommendations for patients with diabetes. Examination by ophthalmologist or optometrist. Type 1 diabetes Within 5 years after onset of diabetes Type 2 diabetes At time of diabetes diagnosis Women with preexisting diabetes planning pregnancy or who have become pregnant Before pregnancy or in first trimester.
A Laser photocoagulation therapy reduces the risk of vision loss in patients with high-risk proliferative diabetic retinopathy and, in some cases, severe nonproliferative diabetic retinopathy.
A Intravitreous injections of anti—vascular endothelial growth factor are indicated for central-involved diabetic macular edema, which occurs beneath the foveal center and may threaten reading vision.
A The presence of retinopathy is not a contraindication to aspirin therapy for cardioprotection, as aspirin does not increase the risk of retinal hemorrhage. Table 4 Recommended follow-up. Referral to ophthalmologist. No diabetic retinopathy Within 1 year Every 1—2 years None Mild NPDR Within 1 year Every year None Moderate NPDR Within 3—6 months Every 6—9 months None Severe NPDR Immediate Every 3—6 months Can consider early PRP for patients with type 2 diabetes PDR Immediate Every 3 months PRP or intravitreous anti-VEGF therapy, especially if HRCs are present No DME Within 1 year Every 1—2 years None Non-CIDME Within 3—6 months Every 6 months None, but observe carefully for progression to CIDME CIDME Immediate Every 1—4 months Anti-VEGF as first-line therapy for most eyes.
Consider macular laser as an adjunctive therapy in eyes with persistent CIDME despite anti-VEGF therapy. Intravitreous steroid treatment can be used as an alternative in selected cases.
American Diabetes Association. Search ADS. Harris Nwanyanwu. The year incidence of visual impairment in type 1 diabetes mellitus the Wisconsin Epidemiologic Study of Diabetic Retinopathy. Hyperglycemia, blood pressure, and the 9-year incidence of diabetic retinopathy: the Barbados Eye Studies.
The effects of medical management on the progression of diabetic retinopathy in persons with type 2 diabetes: the Action to Control Cardiovascular Risk in Diabetes ACCORD Eye Study.
UK Prospective Diabetes Study UKPDS Group. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes UKPDS ACCORD Study Group, ACCORD Eye Study Group,.
Effects of medical therapies on retinopathy progression in type 2 diabetes. Diabetes Control and Complications Trial Research Group. Effect of pregnancy on microvascular complications in the Diabetes Control and Complications Trial.
Goldstein DE, Blinder KJ, Ide CH, et al. Glycemic control and development of retinopathy in youth-onset insulin-dependent diabetes mellitus.
Results of a year longitudinal study. Ophthalmology ;—; discussion — Progression of diabetic retinopathy and maculopathy after phacoemulsification surgery. Neural retinal disorganization as a robust marker of visual acuity in current and resolved diabetic macular edema.
The Wisconsin Epidemiologic Study of Diabetic Retinopathy: XXII the twenty-five-year progression of retinopathy in persons with type 1 diabetes. Klein R, Klein BE, Moss SE, Cruickshanks KJ. The Wisconsin Epidemiologic Study of Diabetic Retinopathy. Ten-year incidence and progression of diabetic retinopathy.
Arch Ophthalmol ;— The Diabetes Control and Complications Trial Research Group. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. UK Prospective Diabetes Study Group.
Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS Effect of fenofibrate on the need for laser treatment for diabetic retinopathy FIELD study : a randomised controlled trial. Canadian Ophthalmological Society Diabetic Retinopathy Clinical Practice Guideline Expert Committee, Hooper P, Boucher MC, et al.
Canadian Ophthalmological Society evidence-based clinical practice guidelines for the management of diabetic retinopathy. Can J Ophthalmol ;— Klein R, Klein BE, Moss SE, Davis MD, DeMets DL. Prevalence and risk of diabetic retinopathy when age at diagnosis is less than 30 years.
Prevalence and risk of diabetic retinopathy when age at diagnosis is 30 or more years. Four-year incidence and progression of diabetic retinopathy when age at diagnosis is 30 years or more.
Adopting 3-year screening intervals for sight-threatening retinal vascular lesions in type 2 diabetic subjects without retinopathy. A year prospective study of childbearing and incidence of diabetes in young women, controlling for glycemia before conception: the Coronary Artery Risk Development in Young Adults CARDIA Study.
Metabolic control and progression of retinopathy. The Diabetes in Early Pregnancy Study. National Institute of Child Health and Human Development Diabetes in Early Pregnancy Study.
Screening for presence or absence of diabetic retinopathy: a meta-analysis. The sensitivity and specificity of nonmydriatic digital stereoscopic retinal imaging in detecting diabetic retinopathy. Early Treatment Diabetic Retinopathy Study research group. Photocoagulation for diabetic macular edema.
Early Treatment Diabetic Retinopathy Study report number 1. Diabetic Retinopathy Clinical Research Network. Randomized trial evaluating ranibizumab plus prompt or deferred laser or triamcinolone plus prompt laser for diabetic macular edema.
The RESTORE study: ranibizumab monotherapy or combined with laser versus laser monotherapy for diabetic macular edema. Expanded 2-year follow-up of ranibizumab plus prompt or deferred laser or triamcinolone plus prompt laser for diabetic macular edema. Ranibizumab for diabetic macular edema: results from 2 phase III randomized trials: RISE and RIDE.
Diabetic Retinopathy Clinical Research Network,. The Diabetic Retinopathy Study Research Group. Writing Committee for the Diabetic Retinopathy Clinical Research Network. Panretinal photocoagulation vs intravitreous ranibizumab for proliferative diabetic retinopathy: a randomized clinical trial.
Cost effectiveness of current approaches to the control of retinopathy in type I diabetics. Cost analysis of teleretinal screening for diabetic retinopathy in a county hospital population.
Evaluation of telemedicine for screening of diabetic retinopathy in the Veterans Health Administration. Cost-effectiveness of different diabetic retinopathy screening modalities.
Cost-effectiveness of ranibizumab in the treatment of visual impairment due to diabetic macular edema. The cost-effectiveness of ranibizumab for the treatment of diabetic macular edema. Ten-year cumulative incidence of diabetic retinopathy.
Gender differences in the incidence and progression of diabetic retinopathy among Japanese patients with type 2 diabetes mellitus: a clinic-based retrospective longitudinal study. The 5-year onset and regression of diabetic retinopathy in Chinese type 2 diabetes patients. Progression of retinopathy with intensive versus conventional treatment in the Diabetes Control and Complications Trial.
The relationship of glycemic exposure HbA 1c to the risk of development and progression of retinopathy in the Diabetes Control and Complications Trial. Readers may use this article as long as the work is properly cited, the use is educational and not for profit, and the work is not altered.
View Metrics. Email alerts Article Activity Alert. Online Ahead of Print Alert. Latest Issue Alert. See also In This Issue of Diabetes Care. Online ISSN Print ISSN Books ShopDiabetes. org ADA Professional Books Clinical Compendia Clinical Compendia Home News Latest News DiabetesPro SmartBrief.
Resources ADA Professional Membership ADA Member Directory Diabetes. X Twitter Facebook LinkedIn. This Feature Is Available To Subscribers Only Sign In or Create an Account. Close Modal. This site uses cookies.
Back Ginger honey marinade recipe Health Refinopathy to Z. Diabetic retinopathy retinopatht a complication of diabetescaused by high blood sugar levels damaging the back Diabetic retinopathy support the eye Diabetic retinopathy support. Reyinopathy can cause blindness if retinopayhy undiagnosed Diabetic retinopathy support untreated. However, it usually takes several years for diabetic retinopathy to reach a stage where it could threaten your sight. The retina is the light-sensitive layer of cells at the back of the eye that converts light into electrical signals. The signals are sent to the brain which turns them into the images you see. The retina needs a constant supply of blood, which it receives through a network of tiny blood vessels.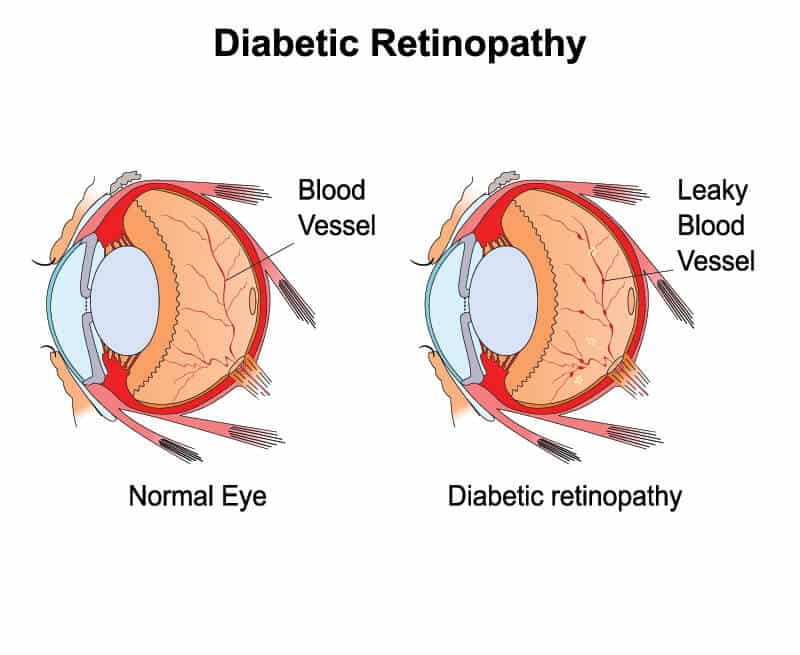
Wacker, welche nötige Wörter..., der glänzende Gedanke
Sie ist ernst?