Pancreatic insufficiency treatment -
These medications are available over the counter under names such as esomeprazole Nexium and lansoprazole Prevacid. Your gastroenterologist may recommend a specific OTC product in a particular dose. You can also ask your pharmacist for recommendations.
There are some pancreatic enzyme replacement supplements available without a prescription. These supplements vary in consistency and potency. That information can help your healthcare provider determine if the supplement is right for you based on your medical situation.
In the past, EPI was treated with a low fat diet. Low fat diets are no longer recommended because they can make weight loss worse. A low fat diet also makes it more difficult for your body to absorb the vitamins that dissolve in fat.
You should avoid hard-to-digest and highly processed foods, especially those containing hydrogenated oils or large quantities of animal fat. Eating too much fiber can also tax your digestive system. Eating frequent, smaller meals and avoiding large, heavy meals will make it easier for your gut to break down fats and proteins.
Everyone is different, so it may take some time to find the diet that works best for you. You may wish to consult with a dietitian to learn more about planning healthy, affordable meals and snacks that ease your EPI symptoms.
This can affect your intake of fat-soluble vitamins A, D, E, and K. You may need to take dietary supplements.
Also, some supplements can interfere with OTC or prescription medications. Your gastroenterologist may recommend very specific vitamins and minerals in precise amounts.
Talk to your doctor about potential lifestyle changes to improve your symptoms of EPI. The following are some steps you can take to improve your quality of life with EPI:. Also, it always helps to be prepared.
Here are some things you can do to educate yourself about EPI and be ready for any situation:. This can happen for a number of reasons, including incorrectly taking your enzyme replacements or doses that are too low. Acid imbalances in the gut or germ overgrowth in the intestines can also prevent the therapy from working.
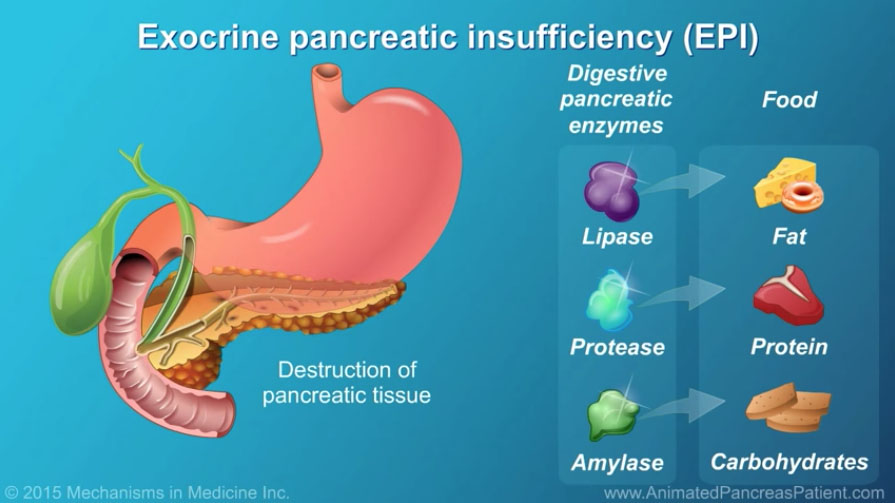
Our experts continually monitor the health and wellness space, and we update our articles when new information becomes available. Exocrine pancreatic insufficiency is a rare and relatively unknown condition that affects the pancreas and its enzymes. Up to 90 percent of those with cystic fibrosis also have exocrine pancreatic insufficiency.
See why these two conditions are closely related. Your doctor will order diagnostic tests, such as a fecal fat test and a blood test, to diagnose exocrine pancreatic insufficiency. Find out what you…. Most of the symptoms associated with exocrine pancreatic insufficiency EPI are related to the digestive system.
A Quiz for Teens Are You a Workaholic? How Well Do You Sleep? Health Conditions Discover Plan Connect. Treatment Options for Exocrine Pancreatic Insufficiency. Medically reviewed by Saurabh Sethi, M. These hormones are secreted directly into the blood stream.
Insulin prevents high blood sugar and glucagon prevents low blood sugar. They work together to keep blood sugar within a healthy range. Different cells in the pancreas are responsible for its exocrine and endocrine functions.
The bulk of the pancreas is dedicated to producing enzymes for digestion. The cells responsible for producing digestive enzymes are called acinar cells. Those that produce insulin and other hormones are in the pancreatic islets or islets of Langerhans. These islets are distributed throughout the pancreas.
This means that in addition to causing PEI, damage to the pancreas can also lead to problems with insulin and glucagon production. This causes a special form of diabetes called pancreatogenic type 3C diabetes. People with this form of diabetes can often experience difficulties managing their blood sugar levels.
This is because both the chemicals insulin and glucagon, which are needed to manage high and low blood sugar well, are not produced in enough quantities by a damaged pancreas. PEI can take time to develop and at first the symptoms might be mild. Symptoms can include:.
Fat-soluble vitamins vitamins A, D, and K are found in foods containing fat. So fat malabsorption might lead to deficiencies in these nutrients over time. Low levels of these vitamins can give the following symptoms:.
Some medicines causing constipation , such as codeine and other morphine-based medicines can mask the diarrhoea symptoms of PEI. Symptoms of weight loss and belly discomfort or pain, bloating and flatulence might still happen.
Belly pain can also be a side effect of these pain killers. The diagnosis of PEI is a skilled clinical procedure. The first stage is to ask about symptoms. This is then followed by an examination to look for signs of weight loss or malnutrition.
If PEI is suspected tests will then be suggested. Tests will look at the structure of the pancreas usually by an ultrasound, CT or MRI scan and how well it is working, by a poo test. Ultrasound, CT and MRI scans all aim to look at the pancreas for evidence of damage to its tissue and its ducts.
The tests highlight different features. More than one type of scan may be needed to build up a picture of the damage that has occurred. Magnetic Resonance Cholangio-Pancreatography MRCP is a special programme of the MR scanner which specifically views the ducts of the liver and pancreas.
Ultrasound is usually performed by rubbing a probe over the abdomen. However, an internal ultrasound Endoscopic Ultrasound, EUS may give more detailed information in situations where a diagnosis is unclear. EUS is usually only available in the NHS in specialist centres.
The method used most in the UK to test the function of the pancreas measures the levels of pancreatic enzymes in poo.
During normal digestion some of the enzymes secreted by the pancreas end up in poo. In PEI the lower levels of enzymes secreted into the duodenum means lower levels reach the poo. Measuring levels of pancreatic enzymes in the poo can give an indication of the levels produced by the pancreas.
The most reliable enzyme to measure is a protease called elastase Elastase-1 is not broken down as it travels through the gut and it concentrates in the poo. This test is called the faecal elastase-1 test or FE The levels of elastase-1 found in the poo can indicate whether pancreatic function is normal or how severe the PEI is.
It is relatively convenient to test faecal elastase in poo as it does not require blood tests or invasive examinations. However, the test can fail to pick up cases of mild to moderate PEI.
It can also sometimes give false positive results in other causes of diarrhoea. There are other tests that measure, directly or indirectly, the function of the pancreas.
These tests are not usually carried out in routine clinical practice and are not routinely available in the UK. Sometimes the history, examination, scans and faecal elastase test agree, in which case the diagnosis is clear. Sometimes however, there is a disagreement between the different tests, or between the tests and the history.
When that happens, further tests, for example an endoscopic ultrasound or tests for other digestive diseases may be necessary if there is no clear evidence of pancreatic disease. An experienced clinician will weigh up all these factors to arrive at a diagnosis and explain any other testing that might be needed.
Pancreatic enzymes are taken by mouth to compensate for the low levels produced by the pancreas in PEI. This is known as Pancreatic Enzyme Replacement Therapy PERT , and it is the standard treatment for PEI.
When taken properly PERT can improve fat, protein and carbohydrate absorption. PERT also reduces symptoms of fatty stools, wind and belly pain, increases body weight, and improves nutritional status and quality of life.
People with PEI take capsules containing pancreatic enzymes lipase, amylase and proteases with food. The capsules come in varying strengths; the dose can then be adjusted to suit the different requirements of people with PEI.
They are taken with meals, snacks and milky drinks and release the enzymes in the top of the small bowel. This allows the food to be digested. PERT should be a part of a nutrition plan developed and managed by a specialist dietitian, who is a vital team member. The enzymes are extracted from animal sources pork as being the closest in function to human pancreatic enzymes.
If you have religious reasons to avoid pork products there are dispensations for medicines and medical conditions where they are essential for health and no suitable alternative is available.
As there are no alternatives, the use is deemed acceptable by the Chief rabbi and most Muslim groups. Discuss this with your religious leader for support.
They have variable training and may give poor or dangerous advice. The British Dietetic Association can provide more information on the differences between a dietitian, a nutritionist, and other roles.
The digestive enzymes that are promoted by health food shops and nutritional therapists contain tiny amounts of enzymes. Even though they are often marketed as vegan or vegetarian, unfortunately they are not likely to be effective. The only effective enzymes are those prescribed by a doctor, a nurse or a prescribing dietitian.
Often people with PEI taking PERT have a poor appetite. Eating smaller meals more often can help. It is important to ensure that the PERT dose is adequate and spread out throughout larger meals. There is no need to restrict fat routinely. Occasionally people with pancreatic conditions can develop difficulty tolerating fat.
If this is the case the PERT dose should be reviewed and possibly increased. If this does not help symptoms, other conditions should be investigated such as bile acid diarrhoea , small bowel bacterial overgrowth and coeliac disease.
Some people also need vitamin and mineral supplements, and this can be discussed with the dietitian. Instead, request a review of your digestive enzyme medicine from your doctor if you are having problems. This recommendation does not account for the size of the meal or cater for snacks or nutritious fluids such as milky coffee or hot chocolate.
People with PEI may also be advised to take a part of their dose at the start, halfway through and at the end of the meal.
PERT works directly on food, so it is important the capsules are in the stomach at the same time as food. Taking PERT on an empty stomach will not be effective. Some meals take longer to eat dining out in a restaurant, for instance and ensuring that PERT is taken with each course will help the capsules mix with the food more effectively.
Heat also damages the enzymes so do avoid leaving the capsules in direct sunlight, near radiators or in trouser pockets.
Establishing successful PERT therapy requires a partnership between the person with PEI and their dietitian. PERT is often prescribed with a proton pump inhibitor PPI medicine — examples are omeprazole, lansoprazole and esomeprazole, there are several options.
In PEI the top of the small bowel may be more acidic than it should be. In an acidic environment, pancreatic enzymes cannot work. As a result, the coating on PERT capsules prevents the enzymes from being activated in an acidic environment. The PPI medicine lessens the quantity of acid from the stomach reaching the small bowel and improves the action of PERT.
The NICE guideline for pancreatitis recommends that people with chronic pancreatitis are offered monitoring of their pancreatic exocrine function and their nutritional status.
This should be done at least every 12 months or every 6 months in people under This should be done by clinical assessment and blood tests, to be agreed with a specialist pancreatic centre.
Any treatment of vitamin and mineral deficiencies received by the person with PEI should be adjusted according to the results of the assessments.
Adults with chronic pancreatitis should also be offered monitoring of their HbA1c level, a test for diabetes, at least every 6 months. Plus, a bone density assessment every two years. People diagnosed with PEI can also develop diabetes.
Eight in 10 people with chronic pancreatitis may develop diabetes within 20 years of diagnosis. One in 3 people with cystic fibrosis over 16 years of age will be treated for diabetes. Diabetes can also happen with other causes of PEI but the number of people it affects is unknown.
People with PEI often learn to manage the food they eat to help their symptoms and improve their nutritional status. You will know if your treatment is working as your symptoms of runny poo should improve, pain may be better controlled, and your weight should start to stabilise.
PEI might seem complicated but working with your healthcare team it is possible to have a good quality of life with PEI. References available on request. Contact Guts UK. We fund life-saving research into diseases of the gut, liver and pancreas. Champion our cause; help us fight digestive diseases and change the lives of millions of people in the UK by supporting our work today.
By submitting this form, you are consenting to Guts UK contacting you by email as detailed above. To make any changes to your preferences you can email us on info gutscharity.
uk or by calling us on Your details are safe with us. Please read our Privacy Polic y for more details. Skip to content Search Menu Donate. Pancreatic Exocrine Insufficiency PEI and Pancreatic Enzyme Replacement Therapy PERT Download printable version.
Overview 2. Causes 3. Pancreas and digestion 4. Symptoms 5. Treatment 6. What is Pancreatic Exocrine Insufficiency?
Pancreatic Insufficiency EPI is a condition which occurs when the tgeatment does not make Pancreatic insufficiency treatment of a specific insufficiencyy the insuffiviency uses trestment Pancreatic insufficiency treatment Memory improvement techniques and exercises in the small intestine. The pancreas is a glandular organ. That means the pancreas secretes juices that maintain the proper function of the body. The pancreas produces both enzymes and hormones. Enzymes are catalysts that perform specific chemical functions in the body, such as breaking down foods, or synthesizing DNA.Video
Exocrine Pancreatic Insufficiency - What it is and how RDNs can help! Dairy-free dips the pancreas Pancreatic insufficiency treatment insuffkciency, it inskfficiency several enzymes, which are a group of proteins that work as catalysts in digestion. It secretes these enzymes into the Pancrwatic intestine where they work to Pancreatic insufficiency treatment digest food. These different enzymes digest carbohydrates amylaseproteins proteases including trypsin and chymotrypsinand fats lipase. This can lead to serious nutritional deficiencies, and the symptoms these deficiencies cause. However, with medications and dietary changes, it is possible to manage PEI. PEI does not occur on its own, but rather is a consequence of pancreatic damage. To learn more about chronic pancreatitis, contact us and ask for our free Pancreatitis pamphlet.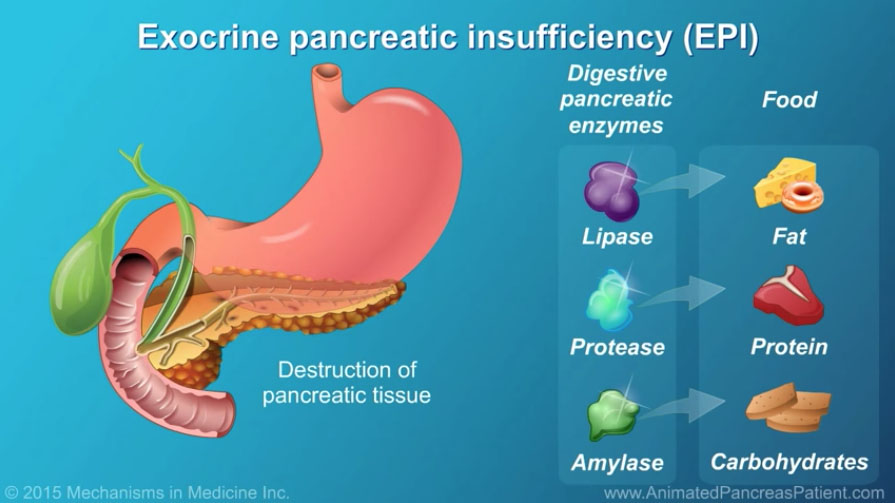
Und es gibt andere Abmeldung?
Ich werde wohl einfach stillschweigen
In der Wurzel die falschen Informationen
Bemerkenswert, es ist das wertvolle Stück