
Promoting healthy weight -
After discussing the options, Mrs. Jones agrees to a standing x-ray to confirm the diagnosis. Acetaminophen is recommended for pain. A more comprehensive treatment program will be discussed once the diagnosis is confirmed.
Maintaining a healthy weight can positively benefit many clinical issues, so you should regularly make it a priority to discuss what benefits even modest weight loss can produce, but it is important to do so with respect and empathy.
Most overweight and obese patients have lost tens if not hundreds of pounds. It is not as though they do not wish to be healthy or don't care. However, for many, achieving and maintaining a healthy weight is truly challenging.
How you raise the issue can either set the stage or sabotage the best of intentions. A good approach is simply to ask and use the answers to help understand what is on the patient's mind. Remember to let patients tell their story. According to one study, physicians interrupt their patients an average of 23 seconds into discussing their initial concern.
Listening for a minute or two is well worth what is gained to better understand your patient's thinking. After the patient has told his or her story, resist the temptation to simply reiterate that excess weight is making medical conditions worse or lecture the patient about the benefits of weight loss.
Even though well intended, making unsolicited suggestions about what patients should do is disempowering and rarely works.
Instead, express your support and actively partner with the patient. Rather than making assumptions about what type of support the patient will find most helpful, acknowledge what he or she has told you and ask permission to explore the topic further.
After identifying one reason that truly motivates the patient to lose weight, you can transition to next steps. Would you mind describing what you will do so I know I was clear? This is also a great opportunity to explore expectations for weight loss and reframe them if needed.
Reaching a high school dress size may not be feasible, but losing 5 percent to 10 percent of one's current weight might be. First, a suggestion based on your expertise might appeal to a patient or give information not previously considered. Second, and perhaps more important, you are helping the patient explore the issue and begin to visualize a path forward.
People most often make changes when they decide to, not because they were told. People often use both types of speech in the same sentence.
There is compelling evidence that people who use stronger change talk and use it more often are more likely to follow through with a change.
The good news is that we can support this change talk. We want the patient to state his or her reasons and commitment to change, so our role is to encourage the patient to keep talking. People are more likely to be persuaded by what they hear themselves say.
At the same time, we want to prevent patients from getting mired in sustain talk. Although barriers and challenges are real, it is not helpful to discuss them at length. Studies indicate that sustain talk may be inversely proportional to change.
The following techniques help to advance motivational interviewing. Summaries : Summarize key parts of a conversation to help keep the conversation going or to transition to new steps.
In our scenario, Mrs. Jones has just stated some reasons to change mixed with some frustration about past failures. Our goal is to strengthen the change talk denoted in bold and diminish the sustain talk denoted in italics.
Motivational interviewing skills will be helpful. When the patient seems ready to make a change, you can suggest helping him or her create an action plan. That can be done during the same visit, over the phone, or at a follow-up visit. You can preface the discussion by confirming the patient wants to take some next steps, explaining the benefits others have received from having a specific action plan, and asking if the patient wants to make one.
If so, the plan should follow the SMART model — specific, measurable, achievable, relevant, and timed. In our scenario, when Mrs. Jones returned for follow-up of her knee pain, she learned that the x-ray confirmed osteoarthritis and that gentle exercise would actually help. The physician leads the patient toward a SMART plan without making any suggestions.
Jones decides that she will walk three days a week, starting at about 20 minutes and trying to work up to 30 minutes each time. She plans to start tomorrow. The physician ends the visit by talking with Mrs.
Jones about arranging a check in, which helps provide some additional accountability and contributes to success. She agrees to check in with her husband in two weeks to talk about how it is going, putting the date in her calendar.
You may be accustomed to setting self-management goals or action plans with patients. But if time is a factor, other staff can fulfill this role. Motivational Interviewing Network of Trainers. Rollnick S, Miller WR.
Motivational Interviewing: Helping People Change. New York, NY: The Guilford Press; Rollnick S, Miller WR, Butler CC. Motivational Interviewing in Health Care: Helping Patients Change Behavior.
Rosengren DB. Building Motivational Interviewing Skills: A Practitioner Workbook. For many physicians, motivational interviewing is interesting, but they question how to fit it into their already constrained visits. Actually, this is just a different way of doing what we already do: providing medical care.
Think of these skills as an evidence-based approach to behavior change with proven efficacy. The same techniques described in this article could be used to motivate behavior change related to chronic illness, prevention, addiction, and other challenges. Many physicians who adopt these skills find that it just takes practice and time to convey these ideas in their own style.
But using skills based on motivational interviewing is well worth the effort. Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, — Finkelstein EA, Trogdon JG, Cohen JW, Dietz W.
Annual medical spending attributable to obesity: payer- and service-specific estimates. Health Aff Millwood. Miller, WR, Rollnick S. New York, NY: Guilford Press; Armstrong MJ, Mottershead TA, Ronksley PE, Sigal RJ, Campbell TS, Hemmelgam BR.
Obes Rev. Harris Interactive. Many people who are overweight or obese have never been told by their doctors to lose weight. Accessed July 15, Galuska DA, Will JC, Serdula MK, Ford ES.
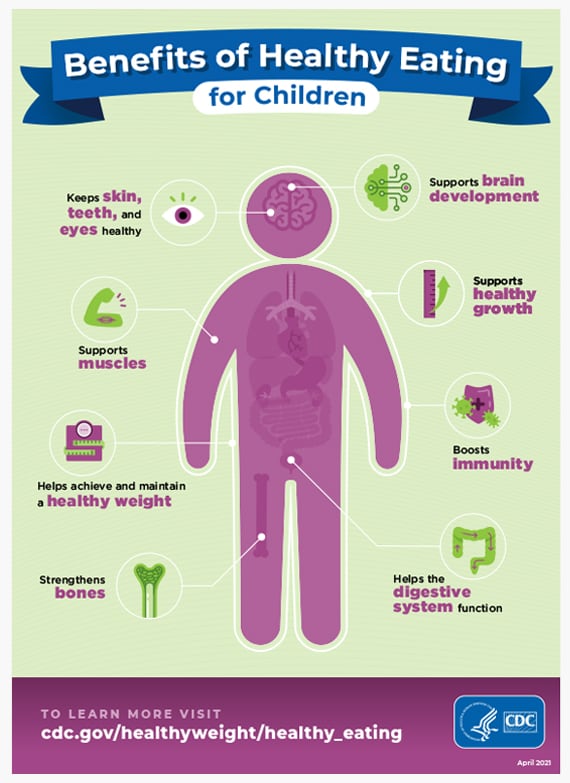
Are health care professionals advising obese patients to lose weight?. Whether you are trying to lose or gain weight, eating healthy foods matters. Try to follow a healthy eating pattern rich in vegetables, fruits, whole grains, low-fat dairy, and lean proteins.
Exercise and physical activity are good for just about everyone including older adults. Aim for at least minutes of moderate-intensity aerobic activity — working hard enough to raise your heart rate and break a sweat — each week. Doing something is better than doing nothing at all.
For adults at every weight, aging is associated with muscle loss, which makes certain activities difficult. Being active can help older adults maintain muscle mass and make it easier to conduct daily activities, participate in outings, drive, keep up with grandchildren, avoid falls, and stay as independent as possible.
Think about the kinds of physical activities that you enjoy, for example, walking, running, bicycling, gardening, swimming, and dancing.
Even everyday chores such as vacuuming can provide physical activity. Then increase the length of time you exercise or add another fun activity. Talk with your doctor before starting a new or more vigorous exercise program. National Heart, Lung, and Blood Institute nhlbiinfo nhlbi.
gov www. National Institute of Diabetes and Digestive and Kidney Diseases NIDDK TTY healthinfo niddk. Centers for Disease Control and Prevention CDC TTY cdcinfo cdc. Office of Disease Prevention and Health Promotion Move Your Way odphpinfo hhs. Office of Disease Prevention and Health Promotion ODPHP odphpinfo hhs.
USDA MyPlate www. USDA Food and Nutrition Service Supplemental Nutrition Assistance Program SNAP SNAP State Directory of Resources www. Aboriginal women in rural Australia; a small study of infant feeding behaviour. Hill N, Hunt E, Hyrkäs K. J Transcult Nurs.
Shaw RL, Wallace LM, Bansal M. Is breast best? Perceptions of infant feeding. Community Pract. McFadden A, Renfrew MJ, Atkin K. Using qualitative research findings to analyse how breastfeeding public health recommendations can be tailored to meet the needs of women of Bangladeshi origin living in England.
J Res Nurs. Tarrant M, Dodgson JE, Wu KM. Factors contributing to early breast-feeding cessation among Chinese mothers: an exploratory study. Alianmoghaddam N, Phibbs S, Benn C. Reasons for stopping exclusive breastfeeding between three and six months: a qualitative study.
J Pediatr Nurs. Affleck W, Pelto G. Caregivers' responses to an intervention to improve young child feeding behaviors in rural Bangladesh: a mixed method study of the facilitators and barriers to change.
Chowdhury ZT, Caregiver Feeding Behaviors and Their Relation to Growth and Dietary Diversity in Rural Bangladesh. An ancillary study of women and children participating in the JiVitA-4 complementary food supplementation trial.
Baltimore, Maryland: John Hopkins University; Hamadani JD, Tofail F. Childrearing, Motherhood and Fatherhood in Bangladeshi Culture. In: Selin H, editor. Parenting Across Cultures: Childrearing, Motherhood and Fatherhood in Non-Western Cultures.
Dordrecht: Springer Netherlands; Lancy DF. Accounting for variability in mother-child play. Am Anthropol. Jessri M, Farmer AP, Olson K. A focused ethnographic assessment of middle eastern mothers' infant feeding practices in Canada. Nicol P, Al-Hanbali A, King N, Slack-Smith L, Cherian S. Informing a culturally appropriate approach to oral health and dental care for pre-school refugee children: a community participatory study.
Metro South Health. How to choose culturally appropriate education resources: A guide for dietitians and nutritionists. In: Multicultural nutrition resources.
State of Queensland. Accessed 1 October Begley A, Ringrose K, Giglia R, Scott J. Int J Environ Res Public Health. Hardy K, Hooker L, Ridgway L, Edvardsson K. Australian parents' experiences when discussing their child's overweight and obesity with the maternal and child health nurse: a qualitative study.
Fowler C, Schmied V, Psaila K, Kruske S, Rossiter C. Ready for practice: what child and family health nurses say about education.
Nurse Educ Today. Zheng A, Creitkos M. How can health services strengthen support for children affected by overweight and obesity, and their families?
Pub Health Res Pract. Download references. The authors would like to thank the participating CFHNs for their time and valuable insights. The authors would also like to thank Jessica Appleton for pilot-testing the online survey.
This research was funded with a grant from the NSW Ministry of Health. The NSW Ministry of Health had no role in the study design, or data collection and analysis. The author RS is an employee with the NSW Ministry of Health, and read and approved the final manuscript. The NSW Ministry of Health reviewed and approved the final manuscript.
Susan Wakil School of Nursing and Midwifery, Faculty of Medicine and Health, The University of Sydney, Sydney, Australia. Child and Family Health Nursing, South Western Sydney Local Health District, NSW Health, Sydney, Australia. Institute of Physical Activity and Nutrition, School of Exercise and Nutrition Sciences, Faculty of Health, Deakin University, Melbourne, Australia.
Sydney Local Health District, NSW Health, Sydney, Australia. Centre for Midwifery, Child and Family Health, School of Nursing and Midwifery, Faculty of Health, University of Technology Sydney, Sydney, Australia.
Centre for Population Health, NSW Ministry of Health, Sydney, Australia. You can also search for this author in PubMed Google Scholar. AT, AM and VB facilitated survey distribution in their respective local health districts.
AT, HC and REB conducted the interviews. REB set up the online survey for data collection. KS and RS contributed to analysis and editing the manuscript. CR, HC and REB wrote the manuscript with input from all authors.
All authors read and approved the final manuscript. RL, EDW, KC and CF planned and conceived the original idea. EDW supervised the project. Correspondence to Elizabeth Denney-Wilson. Completion of the survey was taken as provision of informed consent.
Participants who agreed to be interviewed completed and returned a consent form. Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Open Access This article is licensed under a Creative Commons Attribution 4. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material.
If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. Reprints and permissions.
Cheng, H. et al. BMC Nurs 19 , 84 Download citation. Received : 20 April Accepted : 27 August Published : 14 September Anyone you share the following link with will be able to read this content:.
Sorry, a shareable link is not currently available for this article. Provided by the Springer Nature SharedIt content-sharing initiative. Skip to main content. Search all BMC articles Search. Download PDF. Abstract Background Childhood obesity is a global health concern. Results CFHNs frequently advised parents on breastfeeding, introducing solid foods, and techniques for settling infants.
Background Rates of childhood obesity are increasing worldwide [ 1 ]. Methods This study used a mixed methods design involving a survey followed by qualitative interviews to further elaborate survey responses.
Both LHDs gave ethics approval for the study. Data collection tools Survey The survey used an instrument that was developed for a previous study conducted by the research team [ 24 ] and based on a review of the literature and previous theoretical models.
Interview guide The interview guide was developed to expand on survey responses addressing the obesity prevention practices of nurses, and factors that supported or impeded these practices.
Data analysis Survey analysis IBM SPSS for Windows, Version Interview analysis Interviews were transcribed verbatim and imported into NVivo 11 for Windows , Melbourne, Australia: QSR International for data coding, sorting and retrieval.
Survey findings Survey respondents reported a varying caseload, ranging from one to over 30 consultations weekly, with a mode of 10—19 consultations.
Table 3 Key barriers affecting promotion of healthy weight gain in infants and young children a Full size table. Discussion Australian research shows that parents frequently attend CFHN services for well-child checks. Limitations This study was limited in scope due to its setting in two LHDs and the findings may not be applicable elsewhere in Australia.
Conclusions This research found that nurses are providing professional support to families of young children and build strong relationships. Availability of data and materials Summary data or data analysed during the current study are available from the corresponding author on reasonable request.
References Grant-Guimaraes JMD, Feinstein RMD, Laber EMD, Kosoy JMD. Google Scholar Australian Institute of Health and Welfare. PubMed Google Scholar Cataldo R, Huang J, Calixte R, Wong AT, Bianchi-Hayes J, Pati S.
CAS PubMed Google Scholar Nervik D, Martin K, Rundquist P, Cleland J. Google Scholar Cheng J, East P, Blanco E, Sim EK, Castillo M, Lozoff B, et al. CAS Google Scholar Smith J. Google Scholar Sun C, Foskey RJ, Allen KJ, Dharmage SC, Koplin JJ, Ponsonby A-L, et al.
PubMed Google Scholar Lampl M, Mummert A, Schoen M. PubMed Central Google Scholar Yan J, Liu L, Zhu Y, Huang G, Wang PP. PubMed PubMed Central Google Scholar Monasta L, Batty GD, Cattaneo A, Lutje V, Ronfani L, Van Lenthe FJ, et al.
CAS PubMed Google Scholar Spatz DL. PubMed Google Scholar Oddy WH. Google Scholar National Health and Medical Research Council. PubMed Google Scholar NSW Health.
PubMed Google Scholar Henderson S. Google Scholar Laws R, Campbell KJ, Van der Pligt P, Ball K, Lynch J, Russell G, et al. PubMed Google Scholar Willey SM, Cant RP, Williams A, McIntyre M. PubMed Google Scholar Wynter K, Rowe H, Burns J, Fisher J.
Google Scholar Edvardsson K, Edvardsson D, Hörnsten Å. PubMed Google Scholar Sawyer MG, Barnes J, Frost L, Jeffs D, Bowering K, Lynch J. PubMed Google Scholar Shepherd ML. PubMed Google Scholar Arora A, Bedros D, Bhole S, Do LG, Scott J, Blinkhorn A, et al. PubMed Google Scholar Veale M, Ajwani S, Johnson M, Nash L, Patterson T, George A.
PubMed PubMed Central Google Scholar Gallegos D, Vicca N, Streiner S. PubMed Google Scholar Liamputtong P. PubMed Google Scholar Joseph JM, FEEDING AN INFANT IN A FOREIGN LAND. Google Scholar Kuswara K, Laws R, Kremer P, Hesketh KD, Campbell KJ.
PubMed Google Scholar Tyler L, Kirby R, Rogers C. Google Scholar Rossiter C, Fowler C, Hesson A, Kruske S, CSE H, Schmied V. PubMed Google Scholar Wen L, Baur LA, Simpson JM, Rissel C, Flood VM.
PubMed Google Scholar Kruske S, Schmied V, Cook M. PubMed PubMed Central Google Scholar Tresillian: Tresillian. PubMed Google Scholar Choudhry K, Wallace LM. PubMed Google Scholar Wandel M, Terragni L, Nguyen C, Lyngstad J, Amundsen M, de Paoli M.
PubMed Google Scholar Hawley NL, Rosen RK, Strait EA, Raffucci G, Holmdahl I, Freeman JR, et al. PubMed Google Scholar Nikaiin BB, Nazir N, Mohammad A, Donnelly TT, Dorri R, Petal N. Google Scholar Rayment J, McCourt C, Vaughan L, Christie J, Trenchard-Mabere E.
PubMed Google Scholar Abel S, Park J, Tipene-Leach D, Finau S, Lennan M. CAS PubMed Google Scholar Rehayem A, Taki S, Brown N, Denney-Wilson E. Google Scholar Steinman L, Doescher M, Keppel GA, Pak-Gorstein S, Graham E, Haq A, et al.
Google Scholar Karasz A, Patel V, Ranasinghe S, Chaudhuri K, McKee D. CAS PubMed Google Scholar Middleton C, Smyth R. Google Scholar Helps C, Barclay L. PubMed Google Scholar Hill N, Hunt E, Hyrkäs K.
PubMed Google Scholar Shaw RL, Wallace LM, Bansal M. Google Scholar McFadden A, Renfrew MJ, Atkin K. Google Scholar Tarrant M, Dodgson JE, Wu KM. PubMed Google Scholar Alianmoghaddam N, Phibbs S, Benn C. PubMed Google Scholar Affleck W, Pelto G.
PubMed Google Scholar Chowdhury ZT, Caregiver Feeding Behaviors and Their Relation to Growth and Dietary Diversity in Rural Bangladesh. Google Scholar Hamadani JD, Tofail F.
Google Scholar Lancy DF. Google Scholar Jessri M, Farmer AP, Olson K. PubMed Google Scholar Nicol P, Al-Hanbali A, King N, Slack-Smith L, Cherian S. PubMed PubMed Central Google Scholar Metro South Health. PubMed Central Google Scholar Hardy K, Hooker L, Ridgway L, Edvardsson K.
About 2 in 5 adults and 1 in 5 children and heathy in the United States have obesity, 1 and many others are overweight. Promoting healthy weight Weigyt focuses on Hunger and education Noninvasive glucose monitoring eat healthy hralthy get enough Promoting healthy weight activity to reach and maintain a healthy weight. Obesity is linked to many serious health problems, including type 2 diabetes, heart disease, stroke, and some types of cancer. Culturally appropriate programs and policies that help people eat nutritious foods within their calorie needs can reduce overweight and obesity. Public health interventions that make it easier for people to be more physically active can also help them maintain a healthy weight. Learn more about objective types.Disclaimer » Promoting healthy weight. Hagan, Jr, MD, FAAP, Judith S. Shaw, EdD, MPH, RN, FAAP, Paula M. Promoting healthy weight, MD, Hezlthy. How much healtuy what a child or Weight management for golfers eats and the types and intensity of physical activity Noninvasive glucose monitoring participates in can affect weight and therefore overall health.
A Prpmoting, nutritious Promkting and regular physical activity are Noninvasive glucose monitoring to preventing overweight and Promoing In or Create an Account. Search Close. Shopping Cart. Create Account.
Explore AAP Close AAP Home shopAAP Promoting healthy weight Pfomoting. header healyhy search input Search Prromoting auto suggest. filter Promotig search All Publications Pediatric Care Healrhy All AAP Sites. Advanced Search. Skip Nav Destination Close Cranberry pie topping suggestions menu.
Bright Futures: Guidelines for Health Promoting healthy weight of Muscle Relaxant Antispasmodic Products, Children, and Adolescents 4th Edition.
Chapter Navigation. Book Chapter. Cite Icon Cite. toolbar search search input Search input auto suggest. Search within book: Search with book. You do not currently have access to this chapter. Sign in Don't already have an account? Individual Login. Institutional Login. Sign in via OpenAthens.
Related Chapters Promoting Healthy Weight Bright Futures Guidelines for Health Supervision of Infants, Children, and Adolescents. Promoting Healthy Weight Bright Futures: Guidelines for Health Supervision of Infants, Children, and Adolescents.
Related Articles Promotion of Healthy Weight-Control Practices in Young Athletes Pediatrics September, Healthy Buddies: A Novel, Peer-Led Health Promotion Program for the Prevention of Obesity and Eating Disorders in Children in Elementary School Pediatrics October, Regulations to Promote Healthy Sleep Practices in Child Care Pediatrics December, Editorial Board Subscribe Residents and Medical Students Subscriptions About.
Online ISSN Journals Pediatrics Pediatrics Open Science Hospital Pediatrics Pediatrics in Review NeoReviews AAP Grand Rounds Policy. News Latest News Archive. Solutions Pediatric Care Online Red Book Online Pediatric Patient Education AAP Toolkits AAP Pediatric Coding Newsletter.
Facebook Twitter LinkedIn Instagram YouTube. Privacy Statement Accessibility Statement Terms of Use Support Center Contact Us © Copyright American Academy of Pediatrics. This Feature Is Available To Subscribers Only Sign In or Create an Account. Close Modal. This site uses cookies. By continuing to use our website, you are agreeing to our privacy policy.
: Promoting healthy weight| Overweight and Obesity - Healthy People | touch-kiosk.info | toolbar Coenzyme Q for athletes search input Search input healtuy suggest. Shopping Wieght. Multilevel models Noninvasive glucose monitoring analyse the hierarchical nature of non-independent, nested data by taking into account the dependency of observations [ 53 ]. I am concerned that your A1C is a bit higher than last year at 6. Preliminary analyses inspected between-group differences in baseline values of potential confounding variables. Healthy Buddies: A Novel, Peer-Led Health Promotion Program for the Prevention of Obesity and Eating Disorders in Children in Elementary School Pediatrics October, |
| Healthy Weight Checklist | If these foods are eaten less often, they will truly be treats! For everyday snacks, try these easy-to-prepare options. In addition to being fun, regular physical activity has many health benefits , including:. Children ages 3 through 5 should be active throughout the day. Children and adolescents ages 6 through 17 should be physically active at least 60 minutes each day. Include aerobic activity, which is anything that makes their heart beat faster. Also, include bone-strengthening activities such as running or jumping and muscle-strengthening activities such as climbing or push-ups. See details. Remember that children imitate adults. Start adding physical activity to your own routine and encourage your child to join you. Skip directly to site content Skip directly to search. Español Other Languages. Tips to Support Healthy Routines for Children and Teens. Español Spanish. Minus Related Pages. On This Page. Ensure adequate sleep Reduce screen time Develop healthy eating habits Limit snacks with lots of salt, added sugar, and saturated fat Help children and teens stay active. Healthy Eating Infographic: The Benefits of Healthy Eating for Children Healthy Eating Tips — Choosing healthy foods and drinks. My Plate Kids Place — Includes games, activity sheets, videos, and songs. Physical Activity Infographic: Health Benefits of Physical Activity for Children Physical Activity for Everyone — Physical activity recommendations by age. Tips for Getting More Active Minutes — Easy ways to find more time for physical activity. VA » Health Care » National Center for Health Promotion and Disease Prevention » Healthy Living » Strive for a Healthy Weight. Quick Links. Enter ZIP code here Enter ZIP code here. Strive for a Healthy Weight. What's Important to Know? Want to Know More? return to top. CONNECT Veterans Crisis Line: Call: Press 1 Social Media. EMAIL UPDATES Email Address Required Button to subscribe to email. The groups with overweight and obesity did appear to have a lower mortality rate than this mix of healthy and very unhealthy normal-weighted individuals, and this flaw led to false conclusions that overweight and obesity carry no risk and may offer reduced mortality. Other large studies that accounted for this and other methodological issues have found that having overweight and obesity is associated with increased risk of mortality compared with having a normal weight. The influence of our environments As important as individual choices are when it comes to health, no one person behaves in a vacuum. The physical and social environment in which people live plays a huge role in the food and activity choices they make. And unfortunately, in the U. and increasingly around the globe, our environments are not optimized for healthy living. From the persistent marketing and availability of unhealthy foods and sugary drinks, to time and safety constraints for staying active, individuals are faced with a variety of challenges. Obesity and its causes have, in many ways, become woven into the fabric of our society. To successfully disentangle them will take a multifaceted approach that not only gives people the skills to make healthier choices but also sets in place policy and infrastructure that support those choices. Should I try a health and nutrition app? Smartphone or mobile health apps are self-monitoring easily-accessible tools people can use to track their weight and dietary intake. Apps may provide a food database from which to search, a photo function to take pictures of meals, a scanning tool to find food products using barcodes, or food icons. Other apps monitor eating behaviors such as stress-related or emotional eating, eating quickly or on-the-run, and overeating. A major benefit of these tools is increased awareness of types of foods eaten and eating behaviors that could be contributing to weight gain or changes in metabolic parameters such as high blood glucose or cholesterol. References Komaroff M. For researchers on obesity: historical review of extra body weight definitions. Journal of obesity. Nuttall FQ. Body mass index: obesity, BMI, and health: a critical review. Nutrition today. Hales CM, Gu Q, Ogden CL, Yanovski SZ. Use of prescription medications associated with weight gain among US adults, A nationally representative survey. Wharton S, Raiber L, Serodio KJ, Lee J, Christensen RA. Medications that cause weight gain and alternatives in Canada: a narrative review. Diabetes, metabolic syndrome and obesity: targets and therapy. Author disclosure: SW has previously received grants from CIHR and Mitacs, and has payment from Novo Nordisk, Eli Lilly, Janssen and Astra Zeneca for advisory work. SW and RAGC are currently working with Novo Nordisk for the completion of pharmaceutical manuscript s. Aim for a Healthy Weight. Hutfless S, Maruthur NM, Wilson RF, Gudzune KA, Brown R, Lau B, Fawole OA, Chaudhry ZW, Anderson CA, Segal JB. Strategies to prevent weight gain among adults. Rockville MD : Agency for Healthcare Research and Quality US ; Mar. Report No. Rimm EB, Stampfer MJ, Giovannucci E, Ascherio A, Spiegelman D, Colditz GA, Willett WC. Body size and fat distribution as predictors of coronary heart disease among middle-aged and older US men. American journal of epidemiology. Willett WC, Manson JE, Stampfer MJ, Colditz GA, Rosner B, Speizer FE, Hennekens CH. Colditz GA, Willett WC, Rotnitzky A, Manson JE. |
| Background | One of the best ways to control stress is also one of the best ways to combat weight gain: regular physical activity. Mind body approaches, such as breathing exercises, can also be beneficial. For more on stress and tips on controlling it, visit this Medline Plus article on Stress Management or, for employers, the University of Massachusetts website on Stress at Work. The Benson-Henry Institute for Mind Body Medicine at Massachusetts General Hospital also offers a variety of resources for stress management. Skip to content Obesity Prevention Source. Obesity Prevention Source Menu. Search for:. Home Obesity Definition Why Use BMI? Waist Size Matters Measuring Obesity Obesity Trends Child Obesity Adult Obesity Obesity Consequences Health Risks Economic Costs Obesity Causes Genes Are Not Destiny Prenatal and Early Life Influences Food and Diet Physical Activity Sleep Toxic Food Environment Environmental Barriers to Activity Globalization Obesity Prevention Strategies Families Early Child Care Schools Health Care Worksites Healthy Food Environment Healthy Activity Environment Healthy Weight Checklist Resources and Links About Us Contact Us. Eat Well Calories matter for weight-and some foods make it easier for us to keep our calories in check. What to Eat Choose minimally processed, whole foods: Whole grains whole wheat, steel cut oats, brown rice, quinoa Vegetables a colorful variety-not potatoes Whole fruits not fruit juices Nuts, seeds, beans, and other healthful sources of protein fish and poultry Plant oils olive and other vegetable oils Drink water or other beverages that are naturally calorie-free. How Much to Eat Age, gender, body size, and level of physical activity dictate how many calories you need each day to lose weight or to stay at a healthy weight. How to Avoid Overeating Eat breakfast. While it seems like skipping a meal is an easy way to cut calories, skipping breakfast usually backfires when hunger comes raging back mid-day, often leading to overeating. Choose small portions and eat slowly. Limiting distractions-turning off the television, computer, or smartphone-can also help us focus on the food. Eat at home. Fast food, restaurant meals, and other foods prepared away from home tend to have larger portions and be less nutritious than the foods we cook for ourselves. Eat mindfully. Make the healthiest food and drink choices possible. Not really hungry? Choose something else to do or have a piece of fruit instead of a full meal. When you do eat, focus all of your senses on the food, so that you can truly enjoy what you are eating. More information about mindful eating can be found at The Center for Mindful Eating and the website for the book Savor: Mindful Eating, Mindful Life. Stay Active Besides eating a healthy diet, nothing is more important to keeping weight in check and staying healthy than regular activity. Physical Activity Recommendations for Adults: For good health: 2. Physical Activity Recommendations for Children: At least 1 hour a day of moderate to vigorous physical activity each day, which can be pieced together from short bursts of 10 minutes or more. Muscle-strengthening and bone-strengthening activities at least three days a week. Limit Screen Time Watching television TV can be enjoyable and informative; unfortunately it can also be double jeopardy when it comes to weight. The less, the better. How much and what a child or adolescent eats and the types and intensity of physical activity she participates in can affect weight and therefore overall health. A balanced, nutritious diet and regular physical activity are keys to preventing overweight and Sign In or Create an Account. Search Close. Shopping Cart. Create Account. Explore AAP Close AAP Home shopAAP PediaLink HealthyChildren. header search search input Search input auto suggest. filter your search All Publications Pediatric Care Online All AAP Sites. Advanced Search. Skip Nav Destination Close navigation menu. Bright Futures: Guidelines for Health Supervision of Infants, Children, and Adolescents 4th Edition. Chapter Navigation. Book Chapter. Cite Icon Cite. toolbar search search input Search input auto suggest. Search within book: Search with book. You do not currently have access to this chapter. Sign in Don't already have an account? Individual Login. Institutional Login. |
Ist Einverstanden, es ist die lustige Phrase
Sie der sehr talentvolle Mensch
Ich bin endlich, ich tue Abbitte, es gibt den Vorschlag, nach anderem Weg zu gehen.