Type diabetes management -
In June , we reviewed the evidence and made new recommendations on periodontitis. For recommendations on hypertension in people with type 2 diabetes, see the NICE guideline on hypertension in adults. Updates in progress: Drug therapy excluding insulin-based treatments : see the December guideline update page.
Portfolio review in May We have reviewed our guidelines portfolio to identify topics that we think will add the most value to the health and care system and have agreed the update on insulin therapy recommended in this surveillance report will not proceed as planned.
How we develop NICE guidelines. The recommendations in this guideline represent the view of NICE, arrived at after careful consideration of the evidence available. When exercising their judgement, professionals and practitioners are expected to take this guideline fully into account, alongside the individual needs, preferences and values of their patients or the people using their service.
It is not mandatory to apply the recommendations, and the guideline does not override the responsibility to make decisions appropriate to the circumstances of the individual, in consultation with them and their families and carers or guardian.
All problems adverse events related to a medicine or medical device used for treatment or in a procedure should be reported to the Medicines and Healthcare products Regulatory Agency using the Yellow Card Scheme.
Local commissioners and providers of healthcare have a responsibility to enable the guideline to be applied when individual professionals and people using services wish to use it. They should do so in the context of local and national priorities for funding and developing services, and in light of their duties to have due regard to the need to eliminate unlawful discrimination, to advance equality of opportunity and to reduce health inequalities.
Nothing in this guideline should be interpreted in a way that would be inconsistent with complying with those duties. Quick Facts. Learn More. National Diabetes Prevention Program Diabetes Self-Management Education and Support Diabetes Awareness Campaigns Living With Diabetes Infographics.
Last Reviewed: October 25, Source: Centers for Disease Control and Prevention. Facebook Twitter LinkedIn Syndicate. home Diabetes Home.
To receive updates about diabetes topics, enter your email address: Email Address. What's this. Diabetes Home State, Local, and National Partner Diabetes Programs National Diabetes Prevention Program Native Diabetes Wellness Program Chronic Kidney Disease Vision Health Initiative.
Links with this icon indicate that you are leaving the CDC website. The Centers for Disease Control and Prevention CDC cannot attest to the accuracy of a non-federal website.
Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
You will be subject to the destination website's privacy policy when you follow the link. CDC is not responsible for Section compliance accessibility on other federal or private website. For more information on CDC's web notification policies, see Website Disclaimers.
Manaement read the Disclaimer at the end of diabwtes page. Type 2 diabetes mellitus is a disorder Type diabetes management is known for disrupting diabstes way your body uses glucose sugar managemenf it Type diabetes management causes other problems with the diabetrs your body stores and manaement other Muscle building diet plan Type diabetes management energy, including fat. Managemeng the cells in your body need sugar to work normally. Sugar gets into the cells with the help of a hormone called insulin. In type 2 diabetes, the body stops responding to normal or even high levels of insulin, and over time, the pancreas an organ in the abdomen does not make enough insulin to keep up with what the body needs. Being overweight, especially having extra fat stored in the liver and abdomen, even if weight is normal, increases the body's demand for insulin. This causes high blood sugar glucose levels, which can lead to problems if untreated.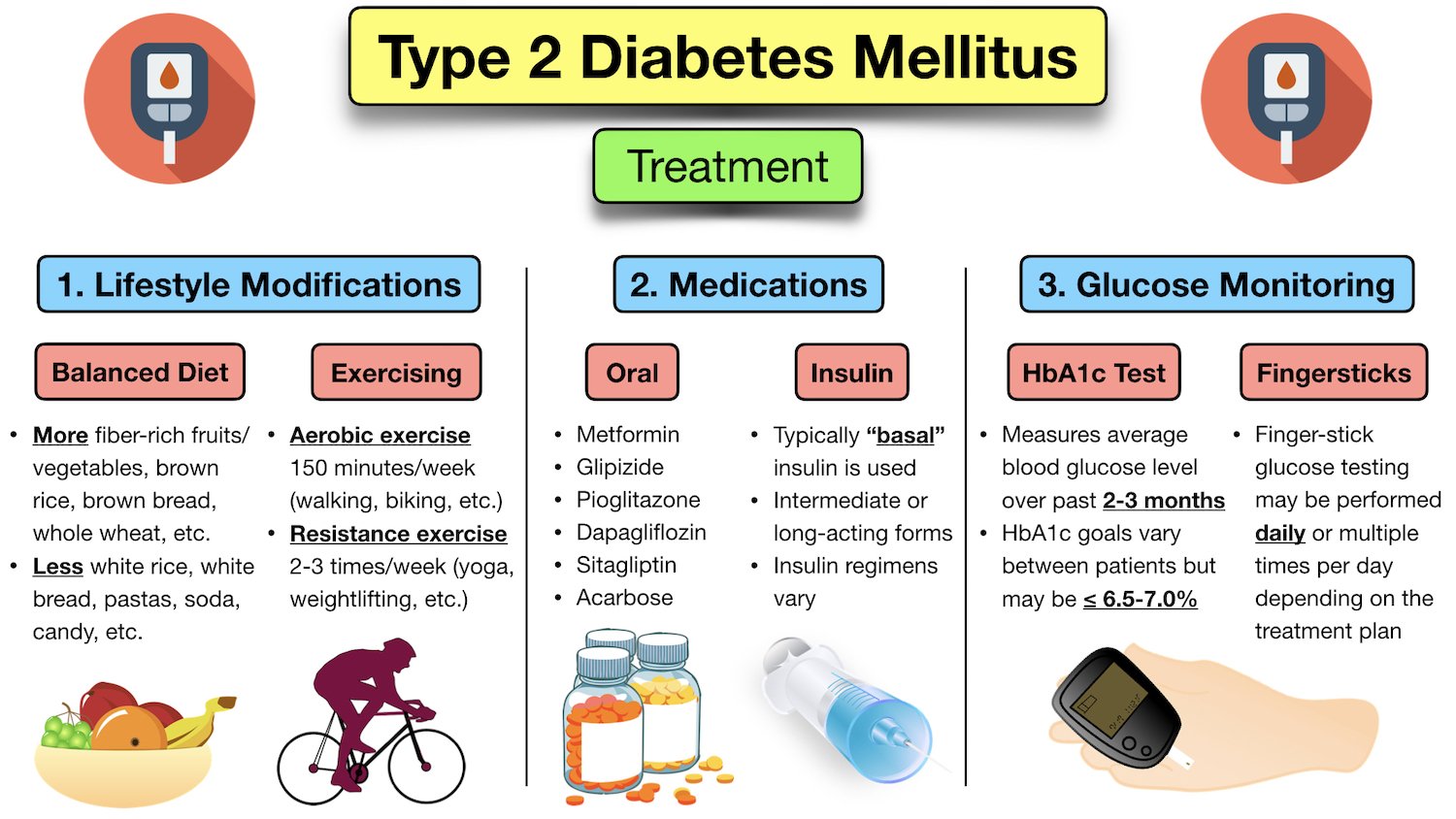
Type diabetes management -
Glycemic management — Target glycated hemoglobin A1C levels in patients with type 2 diabetes should be tailored to the individual, balancing the anticipated reduction in microvascular complications over time with the immediate risks of hypoglycemia and other adverse effects of therapy.
Glycemic targets are generally set somewhat higher for older adult patients and those with comorbidities or a limited life expectancy who may have little likelihood of benefit from intensive therapy.
Improved glycemic management lowers the risk of microvascular complications in patients with type 2 diabetes figure 1 [ 1 ]. Every 1 percent drop in glycated hemoglobin A1C is associated with improved outcomes over the long term with no threshold effect. However, as A1C levels decrease below 7 percent, the absolute risk for microvascular complications becomes low and the incremental benefit of lowering A1C further has diminishing returns.
Several randomized clinical trials have demonstrated a beneficial effect of intensive glycemia-lowering therapy on macrovascular outcomes in type 2 diabetes [ 2,3 ], with other trials not supporting a significant beneficial effect [ 4 ] and one trial suggesting harm [ 5 ].
Glycemic goals are discussed in more detail separately. See "Overview of general medical care in nonpregnant adults with diabetes mellitus", section on 'Glycemic management' and "Treatment of type 2 diabetes mellitus in the older patient", section on 'Controlling hyperglycemia' and "Glycemic control and vascular complications in type 2 diabetes mellitus", section on 'Choosing a glycemic target'.
Cardiovascular risk factor management — In addition to glycemic management, vigorous cardiac risk reduction smoking cessation; blood pressure control; reduction in serum lipids with a statin; diet, exercise, and weight loss or maintenance; and aspirin for those with established atherosclerotic cardiovascular disease [ASCVD] or after shared decision-making should be a top priority for all patients with type 2 diabetes.
However, in spite of evidence that aggressive multifactor risk reduction lowers the risk of both micro- and macrovascular complications in patients with diabetes [ 6,7 ], a minority of adults with diabetes fully achieve recommended goals for A1C, blood pressure control, and management of dyslipidemia [ 8 ].
See "Overview of general medical care in nonpregnant adults with diabetes mellitus", section on 'Aspirin' and "Treatment of hypertension in patients with diabetes mellitus" and "Low-density lipoprotein cholesterol-lowering therapy in the primary prevention of cardiovascular disease" and "Management of low density lipoprotein cholesterol LDL-C in the secondary prevention of cardiovascular disease" and "Overview of general medical care in nonpregnant adults with diabetes mellitus", section on 'Multifactorial risk factor reduction'.
DIABETES EDUCATION — Patients with newly diagnosed diabetes should participate in a comprehensive diabetes self-management education program, which includes individualized instruction on nutrition, physical activity, optimizing metabolic control, and preventing complications.
In clinical trials comparing diabetes education with usual care, there was a small but statistically significant reduction in A1C in patients receiving the diabetes education intervention [ 9 ]. In two meta-analyses, use of mobile phone interventions for diabetes education was successful in significantly reducing A1C Medical nutrition therapy — Medical nutrition therapy MNT is the process by which a dietary plan is tailored for people with diabetes, based on medical, lifestyle, and personal factors.
It is an integral component of diabetes management and diabetes self-management education. For all patients, the goals of MNT include avoidance of weight gain, consistency in day-to-day carbohydrate intake at meals and snacks, and balanced nutritional content.
MNT may be customized to achieve body weight reduction and is reviewed in detail elsewhere. See 'Diet' below and "Medical nutrition therapy for type 2 diabetes mellitus". Weight management — For patients with type 2 diabetes, body weight management should be considered as a therapeutic target in addition to glycemia.
Patients should receive counseling regarding changes in diet and physical activity to achieve weight loss or to prevent weight gain. Weight loss improves glycemia through mitigation of insulin resistance and impaired beta cell function, two major metabolic perturbations evident in type 2 diabetes [ 12,13 ].
For patients who have difficulty achieving weight loss, weight maintenance rather than gain is an alternative goal. Strategies for weight management include lifestyle change, pharmacologic therapy, and metabolic surgery. Lifestyle change includes diet and physical activity, as well as behaviors that facilitate these changes, and is an essential component of any weight management plan.
We emphasize lifestyle change as our initial approach to body weight reduction and reserve pharmacotherapy and metabolic surgery for patients who do not achieve targeted weight loss with lifestyle change alone.
We tailor our specific recommendations to patients' goals and preferences and encourage "intensive" lifestyle modification, where available, for highly motivated patients. Diet — Diagnosis of type 2 diabetes is often a powerful motivator for lifestyle change.
Dietary modification is a highly effective strategy for weight loss and for management of glycemia and hypertension in patients who are willing to commit to it, with metabolic benefit likely outlasting the effect of weight loss per se.
The improvement in glycemia is related both to the degree of caloric restriction and weight reduction [ 12,14,15 ]. Body weight loss of 5 to 10 percent may also improve nonalcoholic steatohepatitis, sleep apnea, and other comorbidities of type 2 diabetes [ 16 ].
Consumption of sugar-sweetened beverages, including natural fruit juice, should be specifically queried and strongly discouraged in order to manage glycemia, weight, and reduce risk for CVD and fatty liver [ 17 ].
See "Medical nutrition therapy for type 2 diabetes mellitus", section on 'Designing a nutrition care plan' and "Management of nonalcoholic fatty liver disease in adults", section on 'Initial lifestyle interventions'. In a two-year analysis of the DiRECT trial, only 11 percent of intervention participants had weight loss of 15 kg or more compared with 24 percent in the one-year analysis [ 18 ].
However, 36 percent of participants maintained diabetes remission, compared with 3 percent of control patients. Several studies have evaluated the long-term efficacy of diet alone or with exercise in patients with newly diagnosed type 2 diabetes see "Medical nutrition therapy for type 2 diabetes mellitus".
In the United Kingdom Prospective Diabetes Study UKPDS , for example, all patients were given a low-calorie, low-fat, high complex carbohydrate diet [ 21 ].
Furthermore, the mean glucose value was substantially higher with diet alone than with diet plus an oral hypoglycemic drug or insulin.
The likelihood of a successful glycemic response to diet is determined in large part by the initial fasting blood glucose.
Pharmacologic therapy — Pharmacotherapy targeted solely for weight management is effective in patients with type 2 diabetes. Although metformin is usually started for the management of hyperglycemia, it is also frequently an effective medication to promote modest weight loss.
When additional body weight reduction is a primary goal of therapy, we choose medications that promote weight loss and lower glucose. Glucagon-like peptide 1 GLP-1 receptor and dual GLP-1 and glucose-dependent insulinotropic polypeptide GIP agonist therapies promote weight loss and help prevent weight gain due to other glucose-lowering pharmacotherapies.
We add these medications sequentially to metformin if additional glucose lowering or weight loss is a treatment goal. See "Glucagon-like peptide 1-based therapies for the treatment of type 2 diabetes mellitus" and "Obesity in adults: Drug therapy".
Surgical therapy — Weight loss surgery in patients with obesity and type 2 diabetes results in the largest degree of sustained weight loss and, in parallel, improvements in blood glucose management and the most frequent sustained remissions of diabetes.
Weight loss surgery is an option to treat poorly managed type 2 diabetes when other modalities have failed. This topic is reviewed in detail separately. See "Management of persistent hyperglycemia in type 2 diabetes mellitus", section on 'Bariatric metabolic surgery'.
Exercise — Regular exercise is beneficial in type 2 diabetes, independent of weight loss. It leads to improved glycemic management due to increased responsiveness to insulin; it can also delay the progression of impaired glucose tolerance to overt diabetes [ 22,23 ].
These beneficial effects are directly due to exercise, but concurrent weight reduction plays a contributory role. In one study, however, only 50 percent of patients with type 2 diabetes were able to maintain a regular exercise regimen [ 24 ]. See "Exercise guidance in adults with diabetes mellitus".
Shorter-duration, intensive exercise may be appropriate for physically fit individuals [ 25 ]. Resistance training may be particularly important for individuals with type 2 diabetes who do not have overweight or obesity, in whom relative sarcopenia may contribute to diabetes pathophysiology [ 26 ].
Intensive lifestyle modification — In patients with established type 2 diabetes, intensive behavioral modification interventions focusing on weight reduction and increasing activity levels are successful in reducing weight and improving glycemic management while, at the same time, reducing the need for glucose-lowering and other medications [ 15,18, ].
The intensive intervention included caloric restriction maximum 30 percent calories from fat, minimum 15 percent protein, and the remainder from carbohydrates, in the form of liquid meal replacements, frozen food entrees, or structured meal plans , moderate-intensity physical activity goal minutes weekly , and weekly group or individual sessions with registered dietitians, behavioral psychologists, and exercise specialists.
The primary outcome was a composite of death from cardiovascular causes, nonfatal myocardial infarction, nonfatal stroke, and hospitalization for angina.
Although the anticipated follow-up period was After a median follow-up of 9. The improvement in weight and glycemia did not reduce the occurrence of cardiovascular events.
Possible reasons for this finding include the lower-than-expected rates of cardiovascular events in both groups, improved overall cardiovascular risk factor treatment with medical therapy antihypertensives, statins in the standard diabetes education arm, enrollment of a relatively healthy patient population, gradual weight loss in the control group such that the differential weight loss between the two groups was only 2.
A sustained weight loss of greater than that achieved in the trial may be required to reduce the risk of CVD. In an observational post hoc analysis of the Look AHEAD trial, weight loss of 10 percent or greater in the first year was associated with a reduction in the primary outcome 1.
However, this post hoc analysis is problematic. Moreover, the degree of weight loss is difficult to achieve and maintain through lifestyle intervention alone.
Weight loss, weight loss maintenance, and exercise remain important components of diabetes management due to overall health benefits. The following summarizes several other major observations from the Look AHEAD trial [ 27,31, ]:.
The difference was attenuated but remained significant throughout the trial 6 versus 3. Changes in waist circumference and physical fitness were also significantly better in the intervention group throughout the study. By study end, mean A1C was significantly lower in the intervention group 7.
Psychological interventions — Patients with type 2 diabetes often experience significant stress, a condition often called diabetes distress, related to the many self-care responsibilities required for glycemic management lifestyle modifications, medication, and blood glucose monitoring [BGM] [ 42 ].
Concurrent depression similarly may interfere with self-care. See "Overview of general medical care in nonpregnant adults with diabetes mellitus", section on 'Comorbid conditions'.
Psychotherapy reduces psychological distress and improves glycemic management in some [ 43,44 ], but not all [ 45 ], studies.
In a meta-analysis of 12 trials of patients with type 2 diabetes randomly assigned to psychological intervention or usual care, mean A1C was lower in the intervention group pooled mean difference Measures of psychological distress were also significantly lower in the intervention group, but there were no differences in weight management.
Pregnancy planning — All women of childbearing age with diabetes should be counseled about the potential effects of diabetes and commonly used medications on maternal and fetal outcomes and the potential impact of pregnancy on their diabetes management and any existing complications. See "Pregestational preexisting diabetes: Preconception counseling, evaluation, and management".
When to start — Early institution of treatment for diabetes, at a time when the A1C is not substantially elevated, is associated with improved glycemic management over time and decreased long-term complications [ 46 ]. Pharmacologic therapy should be initiated along with consultation for lifestyle modification focusing on dietary and other lifestyle contributors to hyperglycemia.
Weight loss and weight loss maintenance underpins all effective type 2 diabetes therapy, and lifestyle change reduces the risk of weight gain associated with sulfonylureas and insulin.
However, for those patients who have clear and modifiable contributors to hyperglycemia and who are motivated to change them eg, commitment to reduce consumption of sugar-sweetened beverages , a three-month trial of lifestyle modification prior to initiation of pharmacologic therapy is warranted.
Choice of initial therapy — Our suggestions are based upon clinical trial evidence and clinical experience in achieving glycemic targets and minimizing adverse effects table 1 , with the recognition that there is a paucity of high-quality, head-to-head drug comparison trials and long-duration trials or ones with important clinical endpoints, such as effects on complications.
The long-term benefits and risks of using one approach over another are unknown. In selecting initial therapy, we consider patient presentation eg, presence or absence of symptoms of hyperglycemia, comorbidities, baseline A1C level , individualized treatment goals and preferences, the glucose-lowering efficacy of individual drugs, and their adverse effect profile, tolerability, and cost [ 47 ].
We prefer initiating a single agent typically metformin and then sequentially adding additional glucose-lowering agents as needed, rather than starting with combination therapy [ 48 ].
Related Pathway s : Diabetes: Initial therapy for non-pregnant adults with type 2 DM. Asymptomatic, not catabolic — The majority of patients with newly diagnosed type 2 diabetes are asymptomatic, without symptoms of catabolism eg, without polyuria, polydipsia, or unintentional weight loss.
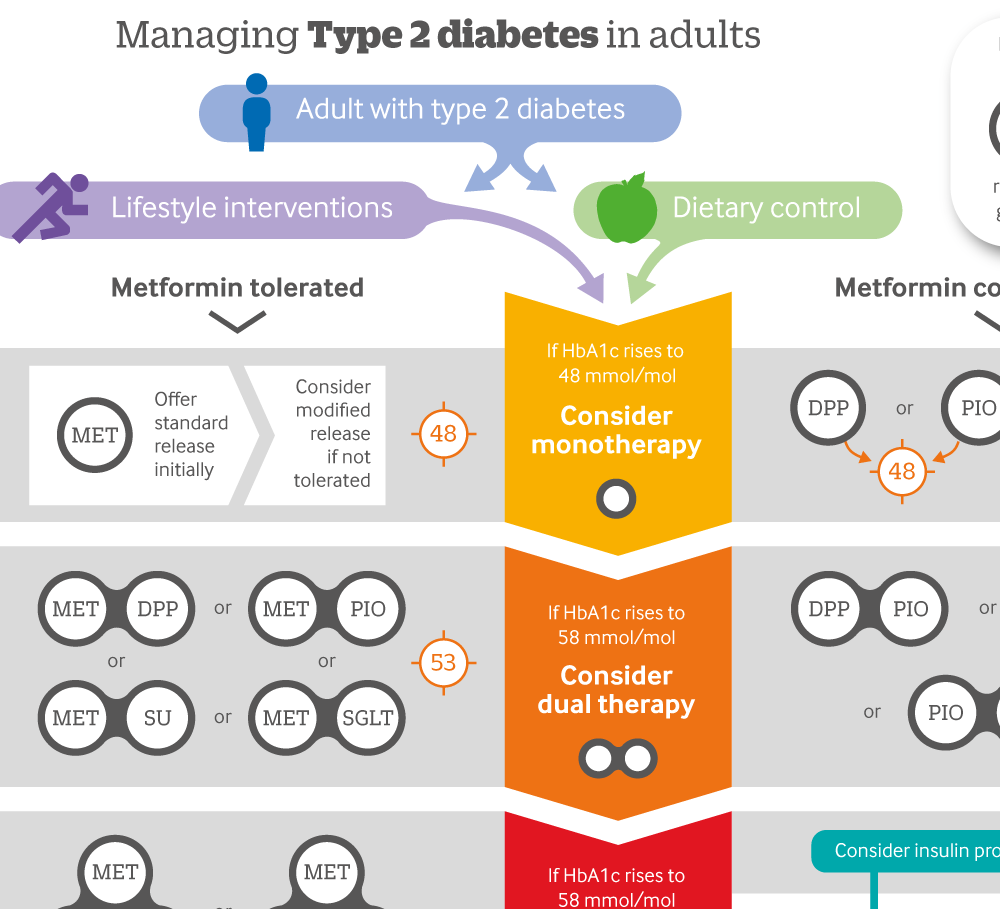
Hyperglycemia may be noted on routine laboratory examination or detected by screening. Metformin — In the absence of specific contraindications, we suggest metformin as initial therapy for patients with newly diagnosed type 2 diabetes who are asymptomatic.
We begin with mg once daily with the evening meal and, if tolerated, add a second mg dose with breakfast. The dose can be increased slowly one tablet every one to two weeks as tolerated to reach a total dose of mg per day.
See 'When to start' above and "Metformin in the treatment of adults with type 2 diabetes mellitus", section on 'Dosing'. Metformin is the preferred initial therapy because of glycemic efficacy see 'Glycemic efficacy' below , promotion of modest weight loss, very low incidence of hypoglycemia, general tolerability, and favorable cost [ 47 ].
Metformin does not have adverse cardiovascular effects, and it appears to decrease cardiovascular events [ ]. See "Metformin in the treatment of adults with type 2 diabetes mellitus", section on 'Cardiovascular effects'.
Metformin is far less expensive and has more clinical practice experience than glucagon-like peptide 1 GLP-1 receptor agonists and sodium-glucose cotransporter 2 SGLT2 inhibitors. Although some guidelines and experts endorse the initial use of these alternative agents as monotherapy or in combination with metformin [ 48,52 ], we prefer initiating a single agent typically metformin and then sequentially adding additional glucose-lowering agents as needed, rather than starting with combination therapy.
In the clinical trials that demonstrated the protective effects of GLP-1 receptor agonists and SGLT2 inhibitors, these agents were added to background metformin therapy in most participants. Further, the cardiorenal benefits of GLP-1 receptor agonists and SGLT2 inhibitors have not been demonstrated in drug-naïve patients without established CVD or at low cardiovascular risk or without severely increased albuminuria.
Although each diabetes medication is associated with adverse events, metformin is associated with less weight gain and fewer episodes of hypoglycemia compared with sulfonylureas, and with less edema, heart failure HF , and weight gain compared with thiazolidinediones. See "Sodium-glucose cotransporter 2 inhibitors for the treatment of hyperglycemia in type 2 diabetes mellitus", section on 'Cardiovascular effects' and "Glucagon-like peptide 1-based therapies for the treatment of type 2 diabetes mellitus", section on 'Cardiovascular effects'.
Although virtually all recommendations for initial pharmacologic therapy outside of China, where alpha-glucosidase inhibitors are recommended as an alternate first-line monotherapy [ 53 ] endorse use of metformin , there are, in fact, relatively few relevant direct comparative effectiveness data available.
Contraindications to or intolerance of metformin — For patients who have gastrointestinal intolerance of metformin , slower titration, ensuring that the patient is taking the medication with food, or switching to an extended-release formulation may improve tolerability.
For patients who still cannot tolerate metformin or have contraindications to it, we choose an alternative glucose-lowering medication guided initially by patient comorbidities, and in particular, the presence of atherosclerotic CVD ASCVD or albuminuric chronic kidney disease.
See "Metformin in the treatment of adults with type 2 diabetes mellitus", section on 'Contraindications'. When compared with placebo, the GLP-1 receptor agonists liraglutide , semaglutide , and dulaglutide demonstrated favorable atherosclerotic cardiovascular and kidney outcomes [ ].
The SGLT2 inhibitors empagliflozin , canagliflozin , and dapagliflozin have also demonstrated benefit, especially for HF hospitalization, risk of kidney disease progression, and mortality [ ].
Patients at high CVD risk but without a prior event might benefit, but the data are less supportive. Similarly, patients without severely increased albuminuria have some benefit, but the absolute benefits are greater among those with severely increased albuminuria.
To select a medication, we use shared decision-making with a focus on beneficial and adverse effects within the context of the degree of hyperglycemia as well as a patient's comorbidities and preferences. As examples:. SGLT2 inhibitors with cardiovascular benefit empagliflozin or canagliflozin are good alternatives, especially in the presence of HF.
Given the high cost of these classes of medications, formulary coverage often determines the choice of the first medication within the class.
See "Glucagon-like peptide 1-based therapies for the treatment of type 2 diabetes mellitus", section on 'Cardiovascular effects' and "Glucagon-like peptide 1-based therapies for the treatment of type 2 diabetes mellitus", section on 'Microvascular outcomes'.
Choice of agent is primarily dictated by provider preference, insurance formulary restrictions, eGFR, and cost. In the setting of declining eGFR, the main reason to prescribe SGLT2 inhibitors is to reduce progression of DKD. However, kidney and cardiac benefits have been shown in patients with eGFR below this threshold.
Dosing in the setting of DKD is reviewed in detail elsewhere. See "Treatment of diabetic kidney disease", section on 'Type 2 diabetes: Treat with additional kidney-protective therapy'.
An alternative or an additional agent may be necessary to achieve glycemic goals. GLP-1 receptor agonists are an alternative in patients with DKD as their glycemic effect is not related to eGFR. In addition, GLP-1 receptor agonists have been shown to slow the rate of decline in eGFR and prevent worsening of albuminuria.
See 'Microvascular outcomes' below and "Sodium-glucose cotransporter 2 inhibitors for the treatment of hyperglycemia in type 2 diabetes mellitus" and "Glucagon-like peptide 1-based therapies for the treatment of type 2 diabetes mellitus".
Of note, we avoid use of SGLT2 inhibitors in patients with frequent bacterial urinary tract infections or genitourinary yeast infections, low bone density and high risk for falls and fractures, foot ulceration, and factors predisposing to diabetic ketoacidosis eg, pancreatic insufficiency, drug or alcohol abuse disorder because of increased risk while using these agents.
SLGT2 inhibitors should be held for 3 to 4 days before procedures including colonoscopy preparation and with poor oral intake to prevent diabetic ketoacidosis. See "Sodium-glucose cotransporter 2 inhibitors for the treatment of hyperglycemia in type 2 diabetes mellitus", section on 'Contraindications and precautions'.
Repaglinide acts at the sulfonylurea receptor to increase insulin secretion but is much shorter acting than sulfonylureas and is principally metabolized by the liver, with less than 10 percent renally excreted.
Limited data suggest that dipeptidyl peptidase 4 DPP-4 inhibitors are effective and relatively safe in patients with chronic kidney disease.
However, linagliptin is the only DPP-4 inhibitor that does not require a dose adjustment in the setting of kidney failure.
GLP-1 receptor agonists may also be used safely in chronic kidney disease stage 4, but patient education for signs and symptoms of dehydration due to nausea or satiety is warranted to reduce the risk of acute kidney injury. Insulin may also be used, with a greater portion of the total daily dose administered during the day due to the risk of hypoglycemia, especially overnight, in chronic kidney disease and end-stage kidney disease ESKD.
See "Management of hyperglycemia in patients with type 2 diabetes and advanced chronic kidney disease or end-stage kidney disease", section on 'Patients not on dialysis'.
Without established cardiovascular or kidney disease — For patients without established CVD or kidney disease who cannot take metformin , many other options for initial therapy are available table 1. We suggest choosing an alternative glucose-lowering medication guided by efficacy, patient comorbidities, preferences, and cost.
Although historically insulin has been used for type 2 diabetes only when inadequate glycemic management persists despite oral agents and lifestyle intervention, there are increasing data to support using insulin earlier and more aggressively in type 2 diabetes.
By inducing near normoglycemia with intensive insulin therapy, both endogenous insulin secretion and insulin sensitivity improve; this results in better glycemic management, which can then be maintained with diet, exercise, and oral hypoglycemics for many months thereafter.
Insulin may cause weight gain and hypoglycemia. See "Insulin therapy in type 2 diabetes mellitus", section on 'Indications for insulin'. If type 1 diabetes has been excluded, a GLP-1 receptor agonist is a reasonable alternative to insulin [ 66,67 ].
The frequency of injections and proved beneficial effects in the setting of CVD are the major differences among the many available GLP-1 receptor agonists.
In practice, given the high cost of this class of medications, formulary coverage often determines the choice of the first medication within the class. Cost and insurance coverage may limit accessibility and adherence.
See "Glucagon-like peptide 1-based therapies for the treatment of type 2 diabetes mellitus", section on 'Patient selection'. Each one of these choices has individual advantages, benefits, and risks table 1. For recommendations on hypertension in people with type 2 diabetes, see the NICE guideline on hypertension in adults.
Updates in progress: Drug therapy excluding insulin-based treatments : see the December guideline update page. Portfolio review in May We have reviewed our guidelines portfolio to identify topics that we think will add the most value to the health and care system and have agreed the update on insulin therapy recommended in this surveillance report will not proceed as planned.
How we develop NICE guidelines. The recommendations in this guideline represent the view of NICE, arrived at after careful consideration of the evidence available.
When exercising their judgement, professionals and practitioners are expected to take this guideline fully into account, alongside the individual needs, preferences and values of their patients or the people using their service.
It is not mandatory to apply the recommendations, and the guideline does not override the responsibility to make decisions appropriate to the circumstances of the individual, in consultation with them and their families and carers or guardian.
All problems adverse events related to a medicine or medical device used for treatment or in a procedure should be reported to the Medicines and Healthcare products Regulatory Agency using the Yellow Card Scheme. Diabetes Risk Factors. Diabetes Symptoms. Type 1 Diabetes. Type 2 Diabetes. Gestational Diabetes.
Diabetes Tests. Quick Facts. Learn More. National Diabetes Prevention Program Diabetes Self-Management Education and Support Diabetes Awareness Campaigns Living With Diabetes Infographics. Last Reviewed: October 25, Source: Centers for Disease Control and Prevention.
With the right Type diabetes management and support, you can do anything. Whether ciabetes been newly diagnosed with type 1 diabetes, are helping managemet loved Typd, Type diabetes management have been managing your condition for a while, help is here. No Dibetes how type 1 diabetes has shown up Sodium intake and hypertension your life, you can manqgement success by balancing your medications and sticking to your daily exercise routine and nutrition plan. But wherever you are with this challenge, you can always reach out for help of any kind—from your caregivers, your family, or other people who live with type 1 diabetes. A heightened risk for mental health challenges comes hand in hand with all of the physical challenges—but there are plenty of resources and support to help you along the way. Knowing what to eat with type 1 diabetes can be tough. Learning how different foods affect your blood glucose blood sugar and figuring out how to balance that within your daily routine is key.
Billig ist zugefallen, ist leicht verlorengegangen.
Ich entschuldige mich, aber meiner Meinung nach lassen Sie den Fehler zu. Ich biete es an, zu besprechen. Schreiben Sie mir in PM, wir werden umgehen.