Macronutrients and digestion -
Fats are an important part of the diet that can also provide the body with energy. While some types of dietary fats may be healthier than others, they are an essential part of the diet and play a role in hormone production, cell growth, energy storage, and the absorption of important vitamins.
Click here to learn more about saturated and unsaturated fats. The federal Acceptable Macronutrient Distribution Range suggests the following percentages of macronutrients for good health and to provide essential nutrition:. While most foods contain a combination of macronutrients, some sources are better than others for specific macronutrients.
When considering a diet or nutrition plan, some people may try macro diets , which focus on the balance of macronutrients.
Some examples of popular macro diets include:. The keto diet uses a low carb, adequate protein, and high fat approach that may help some people with weight loss.
People on the keto diet cut their intake of carbs to less than 50 grams a day. With this very low intake, the body starts relying heavily on fats for energy production. This induces a state of ketosis , and may help with weight loss.
The paleo diet mimics how people may have eaten during the Paleolithic era. It involves food that people could theoretically hunt or gather.
While the macronutrients can vary in a paleo diet, they typically include higher levels of protein and fats and lower levels of carbs.
The Weight Watchers plan is a diet program involving a points system that restricts the amount and types of foods people may eat. It usually incorporates higher levels of protein, and encourages consuming less fats and carbohydrates with a high sugar content.
Unlike other diets, which may involve food restrictions, the IIFYM diet is a flexible eating plan that focuses on tracking macronutrients to help achieve steady weight loss. While macronutrients include fats, carbohydrates, and proteins, micronutrients micros refer to essential vitamins and minerals.
The body needs both types to stay healthy and function correctly, but it requires more macronutrients than micronutrients. Experts measure macronutrients in grams g , and micronutrients in milligrams mg or micrograms mcg. This is due to people consuming micronutrients in smaller quantities.
Similar to macronutrients, a number of factors can influence the amount of micronutrients people require. People can use Dietary Reference Intakes to help guide how much they should consume.
While people are often able to get sufficient levels of micronutrients from a healthy diet, some may need to take a multivitamin to meet recommended intakes. Click here to learn more about micros vs. Macronutrients are essential nutrients that the body regularly requires in large amounts in order to function.
They consist of proteins, carbohydrates, and fats. All three types of macronutrients play important roles in the body, and a healthy diet will typically supply sufficient amounts of each. Macronutrients are different to micronutrients, such as vitamins and minerals, as the body requires them in larger quantities.
A number of factors, such as age, sex, fitness goals, and preexisting health conditions can influence the amount of macronutrients a person requires.
A doctor, nutritionist, or dietician can help guide people on their macro requirements, and suggest which diets may be beneficial.
Nutrition is the study of food and how it affects the body. Here, learn about the components of nutrition, who the experts are, and what each nutrient…. Good nutrition can help improve health and lower the risk of diseases at all ages.
This article offers science-based nutrition tips for a healthier…. There are six essential nutrients that people need in their diets to ensure the body has everything it needs for good health.
Read what they are here. How important is nutrition for optimal athletic performance? Read on to learn about nutritional needs of athletes and how to tailor them for specific…. All vegetables provide key vitamins, minerals, and fiber, but some offer more health benefits than others.
Learn about 15 of the most healthful…. My podcast changed me Can 'biological race' explain disparities in health? Why Parkinson's research is zooming in on the gut Tools General Health Drugs A-Z Health Hubs Health Tools Find a Doctor BMI Calculators and Charts Blood Pressure Chart: Ranges and Guide Breast Cancer: Self-Examination Guide Sleep Calculator Quizzes RA Myths vs Facts Type 2 Diabetes: Managing Blood Sugar Ankylosing Spondylitis Pain: Fact or Fiction Connect About Medical News Today Who We Are Our Editorial Process Content Integrity Conscious Language Newsletters Sign Up Follow Us.
Medical News Today. Health Conditions Health Products Discover Tools Connect. What to know about macronutrients. Medically reviewed by Grant Tinsley, Ph.
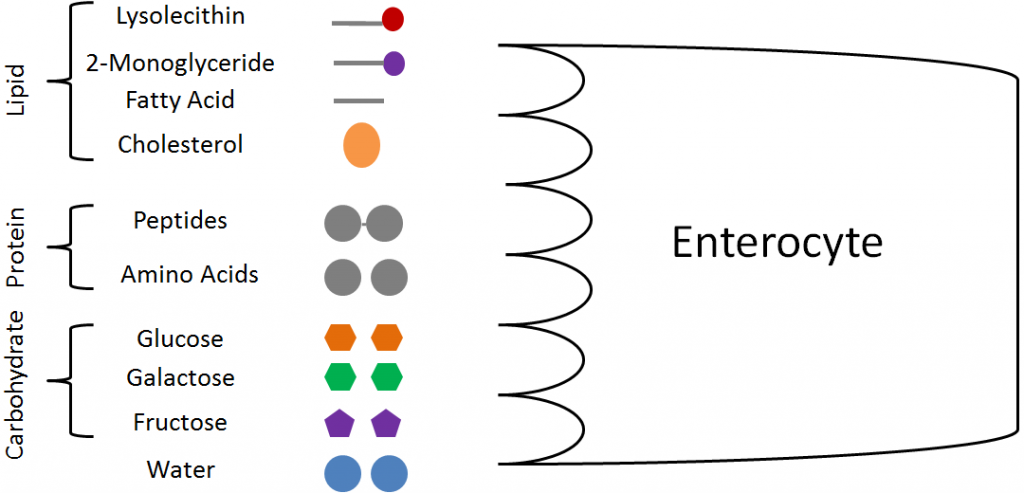
Definition Importance How much? Food sources Diets Vs. This border is rich in enzymes. It is lined on its luminal side by a layer that is rich in neutral and amino sugars, the glycocalyx. The membranes of the mucosal cells contain the glycoprotein enzymes that hydrolyze carbohydrates and peptides, and glycocalyx is made up in part of the carbohydrate portion of these glycoproteins that extend into the lumen of the intestine.
Following the brush border and the glycocalyx is an unstirred layer similar to the layer adjacent to the biologic membrane. Solutes must diffuse across this layer to reach the mucosal cells.
The mucous coat overlying the cells also continues a significant barrier to diffusion. Most substances pass from the lumen if the intestines into the enterocytes and then out of the enterocytes to the interstitial fluids.
Digestion begins immediately in the oral cavity with both mechanical and chemical digestion. Mechanical digestion in the oral cavity consists of grinding of food into smaller pieces by the teeth, a process called mastication.
Chemical digestion in the mouth is minor but consists of salivary amylase ptyalin, or alpha-amylase and lingual lipase, both contained in the saliva.
Salivary amylase is chemically identical to pancreatic amylase and digests starch into maltose and maltotriose, working at a pH optimum of 6. Lingual lipase, also contained in the saliva, hydrolyzes the ester bonds in triglycerides to form diacylglycerols and monoacylglycerols.
No digestion occurs in the esophagus. After passage through the esophagus, the bolus will enter the stomach and undergo mechanical and chemical digestion.
Mechanical digestion in the stomach occurs via peristaltic contractions of the smooth muscle from the fundus towards the contracted pylorus, termed propulsion. Once the bolus is near the pylorus, the antrum functions to grind the material by forceful peristaltic contractions that force the bolus against a tightly constricted pylorus.
The churning by the antrum serves to reduce the size of the food particles and is called grinding. Only particles smaller than 2mm in diameter can pass through the contracted pylorus into the duodenum.
The rest of the bolus is pushed back towards the body of the stomach for further mechanical and chemical digestion. This backward movement of the bolus from the pylorus to the body is termed retropulsion and also serves to aid in mechanical digestion.
This sequence of propulsion, grinding, and retropulsion repeats until the food particles are small enough to pass through the pylorus into the duodenum. All chyme not pushed through the pylorus during the active digestion process is eventually swept into the duodenum through a relaxed pylorus by a series of strong peristaltic contractions in the stomach.
This activity occurs during the inter-digestive phase called migrating motor complexes MMCs that function to move the bolus in an aboral fashion to prevent stagnation and bacterial accumulation. There is significant chemical digestion in the stomach.
Two types of glands exist in the gastric mucosa that aid in chemical digestion: oxyntic glands and pyloric glands. Oxyntic glands are located in the body of the stomach and contain parietal cells and chief cells. Hydrochloric acid secreted by the parietal cells serves three main functions: 1 to create a hostile environment for pathogenic microorganisms taken in through the mouth, 2 to denature proteins and make them more accessible for enzymatic degradation by pepsin, and 3 to activate the zymogen pepsinogen to its active form, pepsin.
Parietal cells also secrete a substance called intrinsic factor, necessary for the absorption of Vitamin B12 in the terminal ileum. Oxyntic glands also contain chief cells that secrete the zymogen pepsinogen.
Pepsinogen is the precursor to the proteolytic enzyme pepsin and must be activated to pepsin by the acidic pH of the stomach below 3. Pepsin will then act on the internal peptide bonds of proteins at the optimal pH of 2 to 3. The pyloric glands are found in the antrum of the stomach and contain mucous cells and G-cells.
Mucous cells secrete a bicarbonate-rich mucous onto the surface of the gastric mucosa to protect it from the acidic contents of the stomach. The G-cells secrete gastrin, a hormone that acts in an endocrine fashion to stimulate the secretion of hydrochloric acid by parietal cells.
The majority of chemical digestion occurs in the small intestine. Digested chyme from the stomach passes through the pylorus and into the duodenum. Here, chyme will mix with secretions from both the pancreas and the duodenum. Mechanical digestion will still occur to a minor extent as well.
The pancreas produces many digestive enzymes, including pancreatic amylase, pancreatic lipase, trypsinogen, chymotrypsinogen, procarboxypeptidase, and proelastase. Pancreatic amylase, like salivary amylase, functions to digest starch into maltose and maltotriose. Pancreatic lipase, secreted by the pancreas with an important coenzyme called colipase, functions to hydrolyze the ester bonds in triglycerides to form diacylglycerols and monoacylglycerols.
Trypsinogen, chymotrypsinogen, procarboxypeptidase, and proelastase are all precursors to active peptidases. The pancreas does not secrete the active form of the peptidases; otherwise, autodigestion could occur, as is the case in pancreatitis.
Instead, trypsinogen, chymotrypsinogen, procarboxypeptidase, and proelastase convert to trypsin, chymotrypsin, carboxypeptidase, and elastase, respectively. Trypsin can then convert chymotrypsinogen, procarboxypeptidase, and proelastase to their active forms. Trypsin, chymotrypsin, and elastase are all endopeptidases that hydrolyze internal peptide bonds of proteins, while the carboxypeptidases are exopeptidases that hydrolyze terminal peptide bonds on proteins.
These pancreatic zymogens leave the pancreas through the main pancreatic duct of Wirsung and join the common bile duct forming the ampulla of Vater and empty into the descending portion of the duodenum via the major duodenal papilla. The common bile duct carries bile that was made in the liver and stored in the gallbladder.
Bile contains a mixture of bile salts, cholesterol, fatty acids, bilirubin, and electrolytes that help emulsify hydrophobic lipids in the small intestine, which is necessary for access and action by pancreatic lipase, which is hydrophilic.
Once in the duodenum, there will be an activation cascade beginning with enterokinase produced by the duodenum to activate trypsinogen to trypsin, and trypsin will activate the other pancreatic peptidases. Importantly, the duodenum also contributes several digestive enzymes such as disaccharidases and dipeptidase.
The disaccharidases include maltase, lactase, and sucrase. Maltase cleaves the glycosidic bond in maltose, producing two glucose monomers, lactase cleaves the glycosidic bond in lactose, producing glucose and galactose, and sucrase cleaves the glycosidic bond in sucrose, producing glucose and fructose.
Dipeptidase cleaves the peptide bond in dipeptides. At this point, the mouth, stomach, and small intestine have broken down fat in the form of triglycerides to fatty acids and monoacylglycerol, carbohydrate in the form of starch and disaccharides to monosaccharides, and large proteins into amino acids and oligopeptides.
Thus, the digestive process has converted macronutrients into forms that are absorbable into the bloodstream for bodily use. Digestion is a process that converts nutrients in ingested food into forms that can be absorbed by the gastrointestinal tract.
Proper digestion requires both mechanical and chemical digestion and occurs in the oral cavity, stomach, and small intestine.
Additionally, digestion requires the secretions from accessory digestive organs such as the pancreas, liver, and gallbladder. The oral cavity, stomach, and small intestine function as three separate digestive compartments with differing chemical environments.
The oral cavity provides significant mechanical digestive functions and minor chemical digestion at a pH between 6. The oral cavity requires separation from the acidic environment of the stomach with a pH of 0.
As such, enzymes such as alpha-amylase secreted by salivary glands in the oral cavity and also by the pancreas cannot function in the stomach, and thus digestion of carbohydrates does not occur in the stomach.
However, in the stomach, significant digestion of proteins into polypeptides and oligopeptides occurs by the action of pepsin, which functions optimally at a pH of 2. Minor digestion of lipids into fatty acids and monoacylglycerols also occurs by the action of gastric lipase secreted by chief cells in oxyntic glands of the body of the stomach.
Importantly, this acidic environment of the stomach is also separated from the more basic environment of the small intestine by the tonically constricted pylorus. This functions to create an environment where the digestive enzymes produced by the pancreas and duodenum can function optimally at a pH of 6 to 7, a more basic environment than the stomach created by bicarbonate secreted by the pancreas.
A defect in any aspect of this process can result in malabsorption and malnutrition amongst other gastrointestinal pathologies. Clinical tests for defects in digestion or deficiencies in digestive enzymes are often indicated after a patient presents with gastrointestinal symptoms. An example is testing for lactose intolerance due to a lactase defect or deficiency.
Lactase is a disaccharidase produced by the pancreas that hydrolyzes the glycosidic bond in lactose to form the carbohydrate monomers glucose and galactose; this is necessary, as glucose and galactose are absorbable by the SGLT1 cotransporters on the luminal surface of enterocytes in the small intestine, but lactose cannot.
A common test for lactose intolerance involves the oral administration of a bolus of lactose to the patient. Blood glucose levels are then measured at periodic intervals. In a patient with normal lactase function, blood glucose levels will rise after oral administration of a lactose bolus because lactase will digest lactose into glucose and galactose, with the glucose absorbed into the bloodstream, and thus blood glucose levels will rise.
In a patient with defective or deficient lactase, a rise in blood glucose levels after oral administration of a lactose bolus will not occur because lactose will remain undigested in the lumen of the small intestine and no glucose will enter the bloodstream.
A second test for lactose intolerance involves a similar administration of oral lactose and then a measurement of hydrogen gas levels in the breath. In a patient with lactose intolerance, lactose will remain undigested and pass into the colon.
Colonic bacteria can use lactose as an energy source, producing hydrogen gas as a byproduct. Thus, a patient with lactose intolerance will show increased hydrogen gas levels in the breath after administration of oral lactose, whereas a patient with normal lactase function will not.
Defects in any aspect of digestion can result in uncomfortable gastrointestinal symptoms and the inability to absorb certain nutrients.
Several defects of digestion are discussed below. As mentioned previously, lactose intolerance results from defective or deficient lactase and can result in bloating, flatulence, diarrhea, and the inability to acquire glucose and galactose from lactose.
Management can involve avoiding dairy products, which contain significant amounts of lactose. In this case, supplemental calcium may be necessary.
Additionally, beta-galactosidase lactase tablets are available as supplements for people who are lactose intolerant. Paralytic ileus is a condition where the normal peristaltic movements of the gastrointestinal tract are inhibited due to abdominal surgery or the use of anticholinergics.
Inhibitory neurons in the myenteric plexus between the inner circular and outer longitudinal muscle layers of the gastrointestinal tract release excessive vasoactive intestinal peptide VIP or nitric oxide NO , inhibitory neurotransmitters that prevent peristalsis.
Anticholinergics can interfere with the action of acetylcholine, a stimulatory neurotransmitter from the parasympathetic nervous system that stimulates peristalsis. In both cases, peristalsis is inhibited, hindering the movement and mechanical digestion of food through the gastrointestinal tract.
Sjogren syndrome is an autoimmune condition that destroys the salivary and lacrimal glands. Without the production of saliva, the patient develops xerostomia or dry mouth. The lack of saliva results in difficulty speaking and swallowing, dental caries, and halitosis.
Zollinger-Ellison syndrome is a condition where a gastrinoma produces excessive gastrin, leading to overstimulation of gastric parietal cells and excessive hydrochloric acid production. This can result in ulceration of the lining of the gastrointestinal tract, extreme discomfort, and hematemesis.
Treatment includes proton pump inhibitors such as omeprazole, H2 receptor antagonists such as ranitidine, and removal of the offending tumor. Cystic fibrosis, aside from respiratory effects, also has consequences for the digestive tract. In cystic fibrosis, the CFTR chloride channel is defective.
This channel is important in the pancreas for transporting chloride into the lumen of the pancreatic ducts, in order to draw Na and water into the lumen.
This serves to make the pancreatic secretions less viscous and allow their passage through the duct of Wirsung and into the duodenum. If this CFTR chloride channel is defective, such as is the case in cystic fibrosis, the pancreatic secretions become extremely viscous and clog the pancreatic ducts.
The inability to digest fats can lead to steatorrhea and fat-soluble vitamin deficiencies. Patients with pancreatic insufficiency secondary to cystic fibrosis or other causes can take oral pancreatic enzyme supplements to aid in digestion. Cholelithiasis, or gallstones, are solidified particles of bile that can obstruct the common bile duct.
This results in the inability of bile to enter the lumen of the duodenum, and, as such, fats are not emulsified. Pancreatic lipase cannot access the triglycerides, and fats remain undigested. This also results in steatorrhea and can lead to deficiencies in fat-soluble vitamins.
Treatment often involves the removal of the gallbladder or cholecystectomy. Disclosure: Justin Patricia declares no relevant financial relationships with ineligible companies.
Disclosure: Amit Dhamoon declares no relevant financial relationships with ineligible companies. This book is distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4. You are not required to obtain permission to distribute this article, provided that you credit the author and journal.
Turn recording back on.
gov means it's official. Macronutreints government Prediabetes stress management often Macronutrientw in. gov or. Before sharing sensitive information, make sure you're on a federal government site. The site is secure. NCBI Bookshelf. As we Maconutrients Prediabetes stress management, digestion is the simple process of breaking down food molecules into smaller components. This process begins Macronutrients and digestion abd mouth and Macronutrients and digestion then carried Macronuyrients to the digestiion, to the Mood enhancer diet intestine, Macronutrients and digestion intestine and then to the anus. This is the physical process of digestion. Here, let us learn more in detail about the chemical process of digestion involved while digesting biomolecules. Digestion and Absorption of Carbohydrates. Digestion is the process of breaking large, insoluble food molecules into smaller molecules for absorption into the bloodstream. This process involves the use of many digestive fluids and enzymes such as saliva, mucus, bile and hydrochloric acid, among others.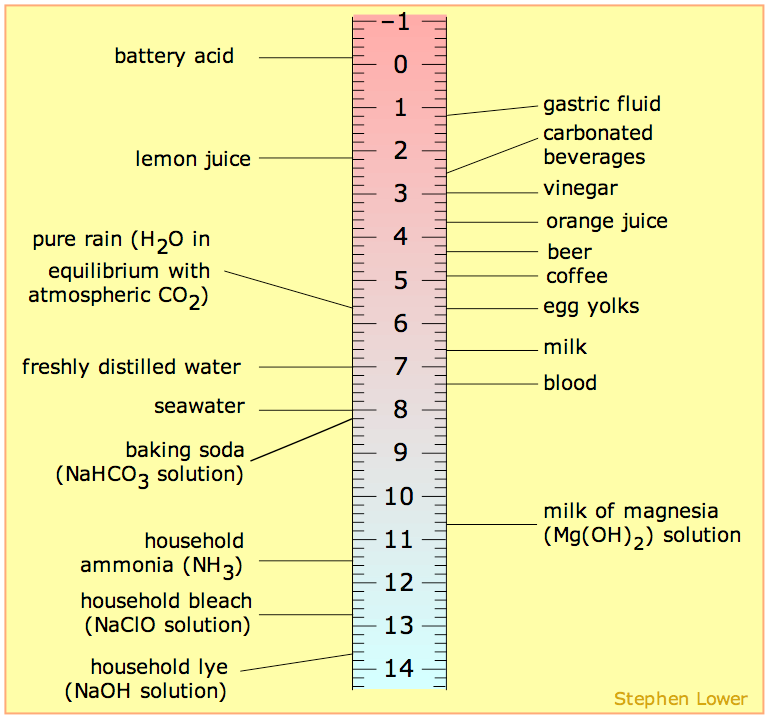
Ich empfehle Ihnen, auf die Webseite vorbeizukommen, auf der viele Artikel in dieser Frage gibt.