Genetics and blood sugar control -
In addition, type 1 diabetes is most common among non-Hispanic whites, especially those of Northern European descent. This is connected to genes called HLA-DR3 or HLA-DR4, which are linked to autoimmune disease.
Suspect genes in other ethnic groups may put people at increased risk. For example, scientists believe that the HLA-DR7 gene may put Black people at risk, and the HLA-DR9 gene may put Japanese people at risk. Genetic predisposition alone is not enough to cause type 1 diabetes. And some people can develop type 1 diabetes even though no one in their family has it.
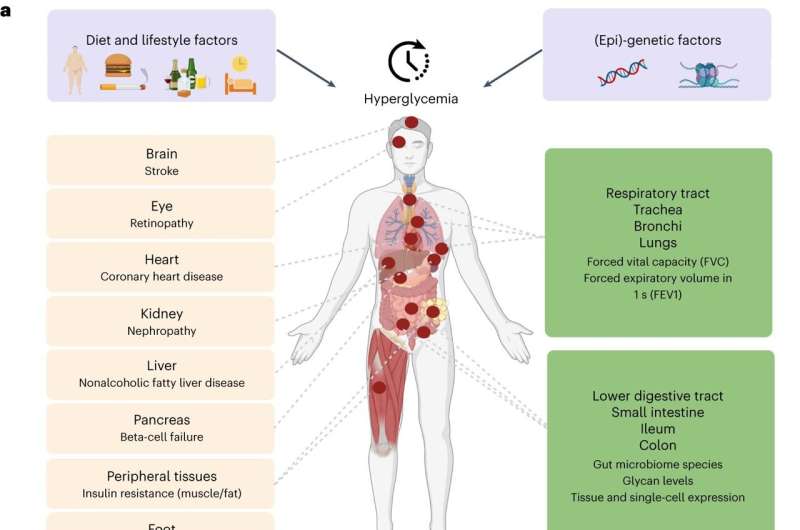
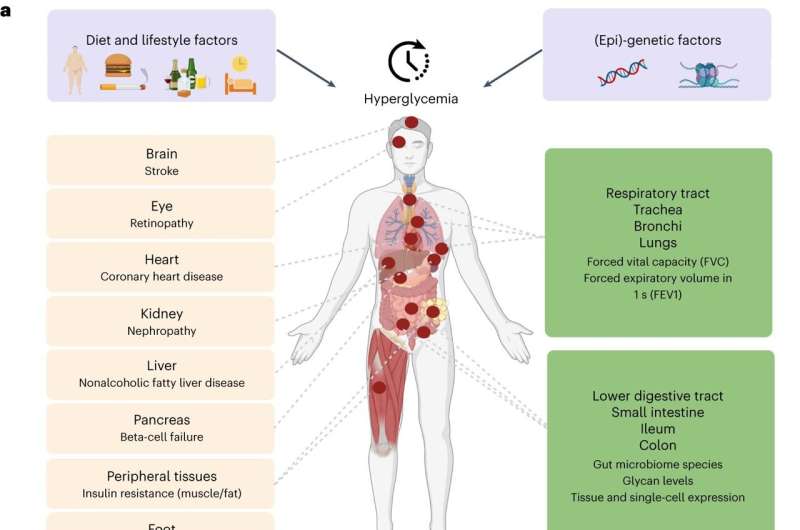
Type 2 diabetes is characterized by insulin resistance and the progressive loss of cells in the pancreas that are responsible for making insulin beta cells. As a result, blood sugar levels go uncontrolled. This is the most common form of diabetes. Many people who have type 2 diabetes may also have other underlying health conditions, such as high blood pressure , cholesterol , and excess weight in the abdominal area.
In the past, type 2 diabetes was often referred to as adult diabetes, but it is now known that children can be affected too.
The genetic component of type 2 diabetes is complex and continues to evolve. Many genes have been identified in people with type 2 diabetes. Some genes are related to insulin resistance, while others are related to beta cell function. Scientists continue to research genes involved in the development of type 2 diabetes and their role in disease progression and treatment.
People who have a first-degree relative with type 2 diabetes are estimated to be three times more likely to develop the disease. But genetic factors are not the only risk. While type 2 diabetes has a stronger link to family history than type 1 diabetes, environmental and behavioral factors also play a role.
As such, interventions can help to prevent or delay a diabetes diagnosis. Gestational diabetes occurs during pregnancy when blood glucose levels become elevated. The placenta provides the baby with nutrients to grow and thrive. It also produces a variety of hormones during pregnancy.
Some of these hormones block the effect of insulin and can make after-meal blood sugars harder to control. This "contra-insulin effect" usually happens around 20 to 24 weeks of pregnancy, which is why people are screened for gestational diabetes at this time.
The US Preventive Services Task Force advises screening for diabetes in women who:. Normally, the pancreas will produce more insulin to make up for hormonal insulin resistance.
For some people, their pancreas cannot keep up with insulin production, which results in elevated blood sugar and a gestational diabetes diagnosis.
Most women who develop gestational diabetes will have no symptoms. Several genes have been identified in people with gestational diabetes. Studies suggest there may be a link between genes for gestational diabetes and type 2 diabetes. Many people diagnosed with gestational diabetes have a close family member such as a parent or sibling with the disease or another form of diabetes, such as type 2 diabetes.
Gestational diabetes appears to run in families. Like other forms of diabetes, having a genetic predisposition doesn't mean you are guaranteed to get gestational diabetes.
Other risk factors include gestational age, weight, activity level, diet, previous pregnancies, and smoking, to name a few. Maintaining adequate blood sugar control is important for the health of the mother and baby.
Genetic testing can be used to identify certain forms of diabetes that are monogenic, meaning that they are related to a change or defect in a single gene.
Both neonatal diabetes and MODY are monogenic, and both tend to be incorrectly diagnosed. Genetic testing is important for making a precise diagnosis, particularly for these monogenic types of diabetes. Furthermore, without a correct diagnosis, the affected person cannot get the proper treatment for the type of diabetes they have.
Physicians often recommend genetic testing when a diabetes diagnosis appears to be atypical. For example, a person who is around age 20 to 25, has abnormal blood sugars, and who does not have any typical risk factors for type 1 or type 2 diabetes, may have MODY.
Unfortunately, insurance often denies coverage for genetic testing even when people fit the criteria, which can cause physicians to miss a MODY diagnosis.
Researchers are continually trying to find ways to make genetic testing more cost-effective. If you suspect that you or your child are at increased risk of developing type 1 diabetes, you might be eligible for a risk screening offered through TrialNet Pathway to Prevention Study.
The screening is free for relatives of people with type 1 diabetes. It uses a blood test to detect diabetes-related antibodies, the presence of which means that the immune system has begun to attack cells in the pancreas.
The screening can detect these antibodies years before diabetes symptoms even begin. People found to be in the early stages of developing type 1 diabetes may also be eligible for the prevention study.
Ask your healthcare provider whether genetic testing is available and how helpful it is in determining if you will get diabetes. Whereas MODY and neonatal diabetes are monogenic, diabetes type 1 and type 2 are polygenic, meaning they are related to changes in multiple genes.
Currently, researchers do not feel that genetic testing is ready to diagnose type 2 diabetes. Because there are so many variants of genes and subtypes of type 2 diabetes, they feel as though better methods and more research need to be done in this area before putting it to practical use.
Similarly, genetic testing is not yet clinically useful for diagnosing polygenic gestational diabetes, as researchers have yet to identify a clear pattern of inheritance. If you have a family history of gestational diabetes or type 2 diabetes, there are ways to reduce your risk of developing the disease.
Maintain a healthy weight or lose weight. If you are overweight, particularly in the abdominal area, losing weight will reduce your risk. While weight gain is important for a healthy pregnancy, people who are pregnant should try to gain weight slowly rather than excessively.
This will help prevent gestational diabetes. Stay active. Aim to exercise at least minutes per week and avoid sitting for long periods of time. Eat more plants. Add more fruits, vegetables, legumes, nuts, seeds, and whole grains to your diet, and cut out processed, pre-packaged foods where possible.
Health maintenance and regular checkups are important. If you've recently gained weight or are feeling very sluggish and tired, you may be experiencing high blood sugar, which is characterized by insulin resistance. Because type 2 diabetes often takes years to develop, people can be walking around with impaired glucose tolerance insulin resistance or prediabetes for years without knowing it.
If you catch this condition early, you may be able to prevent or delay diabetes from occurring. Screening is recommended if you have any of the following risk factors:. There are some noninvasive tests that can alert you if you are at increased risk of developing type 2 diabetes.
These include hemoglobin A1C , blood pressure, cholesterol, and triglycerides. Sometimes people who have a family history of gestational diabetes can develop diabetes during pregnancy despite their efforts to keep weight gain within a healthy range, exercise, and eat a fiber-rich diet.
Do not beat yourself up if this happens. Pregnancy hormones and insulin resistance which is typical during pregnancy can make controlling blood sugar in pregnancy difficult for some people with genetic risk. Your medical team will help you reach your blood sugar goals during pregnancy to make sure that you and your baby are healthy and thriving.
Once you have delivered your baby, your blood sugars should go back to normal. But it's still important to continue to eat a well-balanced diet, maintain a healthy weight, and exercise; these steps can help reduce your risk of developing type 2 diabetes later in life.
Although type 1 diabetes cannot be prevented or cured, if you are genetically predisposed to type 1 diabetes, regular vaccinations and wellness visits will be important.
There is no vaccine to prevent type 1 diabetes, but some research suggests that viruses can trigger type 1 diabetes in people that are predisposed.
Therefore, preventing catching these viruses may reduce the risk of developing diabetes. Understanding the warning signs of type 1 diabetes will also help prevent a dangerous situation like diabetic ketoacidosis.
Although there is no proven cure, scientists continue to make headway in developing better ways to manage diabetes. Additionally, organizations will continue to invest time into researching and developing ways to cure this disease. Having a family history of diabetes doesn't necessarily mean you will develop it.
Genetic testing allows physicians to make the most precise diabetes diagnoses and to get their patients the right treatment for the type of diabetes they have. If you think you could be at risk for diabetes, talk to your healthcare provider about being screened. Doing so may catch diabetes early so that you can stop it from progressing.
There are many different types of diabetes, so your risk depends on what type of diabetes you are genetically predisposed to. If you have concerns about your family history of diabetes, be sure to take it up with your medical team. Genetic testing may not be helpful in certain instances; however, you may be screened for the disease.
You will be educated on your individual risk, steps to take to prevent or delay it if possible , and coping strategies. American Diabetes Association. Learn the genetics of diabetes. Fu Z, Gilbert ER, Liu D. Regulation of insulin synthesis and secretion and pancreatic Beta-cell dysfunction in diabetes.
Curr Diabetes Rev. Juvenile Diabetes Research Foundation. Patel CJ, Chen R, Kodama K, Ioannidis JP, Butte AJ. Systematic identification of interaction effects between validated genome- and environment-wide associations on Type 2 Diabetes Mellitus.
AMIA Jt Summits Transl Sci Proc. Ali O. Genetics of type 2 diabetes. Dong G, Qu L, Gong X, Pang B, Yan W, Wei J. Effect of social factors and the natural environment on the etiology and pathogenesis of diabetes mellitus.
Int J Endocrinol. Marseglia L, Manti S, D'Angelo G, Nicotera A, Parisi E, Di Rosa G, et al. Oxidative stress in obesity: a critical component in human diseases. Int J Mol Sci. Steyn K, Damasceno A.
Lifestyle and related risk factors for chronic diseases. In: Jamison DT, Feachem RG, Makgoba MW, Bos ER, Baingana FK, Hofman KJ, et al.
Disease and Mortality in Sub-Saharan Africa. Washington, DC: Disease and Mortality in Sub-Saharan Africa Agborsangaya CB, Gee ME, Johnson ST, Dunbar P, Langlois MF, Leiter LA, et al.
Determinants of lifestyle behavior in type 2 diabetes: results of the cross-sectional survey on living with chronic diseases in Canada. BMC Public Health.
Spruijt-Metz D, O'Reilly GA, Cook L, Page KA, Quinn C. Behavioral contributions to the pathogenesis of type 2 diabetes. Curr Diab Rep. Mikkelsen KH, Knop FK, Vilsboll T, Frost M, Hallas J, Pottegard A.
Use of antibiotics in childhood and risk of Type 1 diabetes: a population-based case-control study. Diabet Med. Harris ML, Oldmeadow C, Hure A, Luu J, Loxton D, Attia J. Stress increases the risk of type 2 diabetes onset in women: A year longitudinal study using causal modelling.
PLoS ONE. Green MJ, Espie CA, Popham F, Robertson T, Benzeval M. Insomnia symptoms as a cause of type 2 diabetes Incidence: a 20 year cohort study.
BMC Psychiatry. Li Y, Gao X, Winkelman JW, Cespedes EM, Jackson CL, Walters AS, et al. Association between sleeping difficulty and type 2 diabetes in women.
Kalghatgi S, Spina CS, Costello JC, Liesa M, Morones-Ramirez JR, Slomovic S, et al. Bactericidal antibiotics induce mitochondrial dysfunction and oxidative damage in mammalian cells.
Sci Trans Med. Telfer SJ. Fluoroquinolone antibiotics and type 2 diabetes mellitus. Med Hypotheses. Hu FB, van Dam RM, Liu S. Diet and risk of Type II diabetes: the role of types of fat and carbohydrate.
Li Y, Chen JP, Duan L, Li S. Effect of vitamin K2 on type 2 diabetes mellitus: a review. Diabetes Res Clin Pract. Lu L, Bennett DA, Millwood IY, Parish S, McCarthy MI, Mahajan A, et al. Association of vitamin D with risk of type 2 diabetes: a mendelian randomisation study in European and Chinese adults.
PLoS Med. Barbagallo M, Dominguez LJ. Magnesium and type 2 diabetes. World J Diabet. Arnlov J, Zethelius B, Riserus U, Basu S, Berne C, Vessby B, et al. Serum and dietary beta-carotene and alpha-tocopherol and incidence of type 2 diabetes mellitus in a community-based study of Swedish men: report from the Uppsala Longitudinal Study of Adult Men ULSAM study.
Gulseth HL, Wium C, Angel K, Eriksen EF, Birkeland KI. Effects of Vitamin D Supplementation on insulin sensitivity and insulin secretion in subjects with type 2 diabetes and Vitamin D deficiency: a randomized controlled trial. Diabetes Care.
Valdés-Ramos R, Ana Laura GL, Elina MCB, Donají BAA. Vitamins and Type 2 Diabetes Mellitus. Endocrine Metabolic Immune Disorders Drug Targets. Fang X, Han H, Li M, Liang C, Fan Z, Aaseth J, et al. Dose-response relationship between dietary magnesium intake and risk of type 2 diabetes mellitus: a systematic review and meta-regression analysis of prospective cohort studies.
Quansah DY, Ha K, Jun S, Kim SA, Shin S, Wie GA, et al. Associations of dietary antioxidants and risk of type 2 diabetes: data from the korea national health and nutrition examination survey. Mandalazi E, Drake I, Wirfalt E, Orho-Melander M, Sonestedt E.
A high diet quality based on dietary recommendations is not associated with lower incidence of type 2 diabetes in the malmo diet and cancer cohort. CrossRef Full Text Google Scholar. Baxter AJ, Coyne T, McClintock C. Dietary patterns and metabolic syndrome—a review of epidemiologic evidence.
Asia Pacific J Clin Nutrit. van Dam RM, Rimm EB, Willett WC, Stampfer MJ, Hu FB. Dietary patterns and risk for type 2 diabetes mellitus in U. Ann Int Med. Erber E, Hopping BN, Grandinetti A, Park SY, Kolonel LN, Maskarinec G.
Dietary patterns and risk for diabetes: the multiethnic cohort. Jeppesen C, Bjerregaard P, Jorgensen ME. Dietary patterns in Greenland and their relationship with type 2 diabetes mellitus and glucose intolerance.
Public Health Nutrit. de Carvalho GB, Dias-Vasconcelos NL, Santos RKF, Brandao-Lima PN, da Silva DG, Pires LV. Effect of different dietary patterns on glycemic control in individuals with type 2 diabetes mellitus: a systematic review.
Crit Rev Food Sci Nutrit. Neuenschwander M, Ballon A, Weber KS, Norat T, Aune D, Schwingshackl L, et al. Role of diet in type 2 diabetes incidence: umbrella review of meta-analyses of prospective observational studies.
Cutler D, Lleras-Muney A, Vogl T. Socioeconomic Status and Health: Dimensions and Mechanisms. Oxford: The Oxford Handbook of Health Economics Wu H, Meng X, Wild SH, Gasevic D, Jackson CA.
Socioeconomic status and prevalence of type 2 diabetes in mainland China, Hong Kong and Taiwan: a systematic review.
J Global Health. Bird Y, Lemstra M, Rogers M, Moraros J. Int J Equity Health. Imkampe AK, Gulliford MC. Increasing socio-economic inequality in type 2 diabetes prevalence—repeated cross-sectional surveys in England Eur J Public Health. Illangasekera U, Rambodagalla S, Tennakoon S.
Temporal trends in the prevalence of diabetes mellitus in a rural community in Sri Lanka. J Roy Soc Promot Health. Wu H, Jackson CA, Wild SH, Jian W, Dong J, Gasevic D. Socioeconomic status and self-reported, screen-detected and total diabetes prevalence in Chinese men and women in a nationwide cross-sectional study.
Tang K, Wang H, Liu Y, Tan SH. Interplay of regional economic development, income, gender and type 2 diabetes: evidence from half a million Chinese.
J Epidemiol Commun Health. Wu JH, Micha R, Imamura F, Pan A, Biggs ML, Ajaz O, et al. Omega-3 fatty acids and incident type 2 diabetes: a systematic review and meta-analysis. Br J Nutrit. Ko GT, Chan JC, Yeung VT, Chow CC, Tsang LW, Cockram CS. A low socio-economic status is an additional risk factor for glucose intolerance in high risk Hong Kong Chinese.
Eur J Epidemiol. La Merrill M, Emond C, Kim MJ, Antignac JP, Le Bizec B, Clement K, et al. Toxicological function of adipose tissue: focus on persistent organic pollutants. Environ Health Perspect. Carpenter DO. Environmental contaminants as risk factors for developing diabetes. Rev Environment Health.
Buijsse B, Simmons RK, Griffin SJ, Schulze MB. Risk assessment tools for identifying individuals at risk of developing type 2 diabetes. Epidemiol Rev. Howell GE III, Mulligan C, Meek E, Chambers JE. Lee DH, Steffes MW, Sjodin A, Jones RS, Needham LL, Jacobs DR Jr. Low dose organochlorine pesticides and polychlorinated biphenyls predict obesity, dyslipidemia, and insulin resistance among people free of diabetes.
Kelly BC, Ikonomou MG, Blair JD, Morin AE, Gobas FA. Food web-specific biomagnification of persistent organic pollutants. Huang CY, Wu CL, Yang YC, Chang JW, Kuo YC, Cheng YY, et al. Association between dioxin and diabetes mellitus in an endemic area of exposure in taiwan: a population-based study.
Kerger BD, Scott PK, Pavuk M, Gough M, Paustenbach DJ. Re-analysis of Ranch Hand study supports reverse causation hypothesis between dioxin and diabetes.
Crit Rev Toxicol. Chevalier N, Fenichel P. Presse Med. Zong G, Valvi D, Coull B, Goen T, Hu FB, Nielsen F, et al. Persistent organic pollutants and risk of type 2 diabetes: a prospective investigation among middle-aged women in Nurses' Health Study II. Environ Int. Taylor KW, Novak RF, Anderson HA, Birnbaum LS, Blystone C, DeVito M, et al.
Evaluation of the association between Persistent Organic Pollutants POPs and diabetes in epidemiological studies: a national toxicology program workshop review. Berg RD. The indigenous gastrointestinal microflora.
Trends Microbiol. Han JL, Lin HL. Intestinal microbiota and type 2 diabetes: from mechanism insights to therapeutic perspective. World J Gastroenterol. Ley RE, Backhed F, Turnbaugh P, Lozupone CA, Knight RD, Gordon JI. Obesity alters gut microbial ecology.
Proc Natl Acad Sci USA. Larsen N, Vogensen FK, van den Berg FWJ, Nielsen DS, Andreasen AS, Pedersen BK, et al. Gut microbiota in human adults with type 2 diabetes differs from non-diabetic adults.
Qin J, Li Y, Cai Z, Li S, Zhu J, Zhang F, et al. A metagenome-wide association study of gut microbiota in type 2 diabetes.
Wang Y, Luo X, Mao X, Tao Y, Ran X, Zhao H, et al. Gut microbiome analysis of type 2 diabetic patients from the Chinese minority ethnic groups the Uygurs and Kazaks. Ganesan K, Chung SK, Vanamala J, Xu B. Causal relationship between diet-induced gut microbiota changes and diabetes: a novel strategy to transplant faecalibacterium prausnitzii in preventing diabetes.
McCarthy MI, Zeggini E. Genome-wide association studies in type 2 diabetes. Song Y, Niu T, Manson JE, Kwiatkowski DJ, Liu S.
Are variants in the CAPN10 gene related to risk of type 2 diabetes? A quantitative assessment of population and family-based association studies. Ame J Hum Genet. Altshuler D, Hirschhorn JN, Klannemark M, Lindgren CM, Vohl MC, Nemesh J, et al. The common PPARgamma Pro12Ala polymorphism is associated with decreased risk of type 2 diabetes.
Nat Genet. Prasad RB, Groop L. Genetics of type 2 diabetes—pitfalls and possibilities. Barroso I, Luan J, Middelberg RP, Harding AH, Franks PW, Jakes RW, et al. Candidate gene association study in type 2 diabetes indicates a role for genes involved in beta-cell function as well as insulin action.
PLoS Biol. Daimon M, Ji G, Saitoh T, Oizumi T, Tominaga M, Nakamura T, et al. Large-scale search of SNPs for type 2 DM susceptibility genes in a Japanese population. Biochem Biophys Rescommunicat. Fisher E, Nitz I, Lindner I, Rubin D, Boeing H, Mohlig M, et al. Candidate gene association study of type 2 diabetes in a nested case-control study of the EPIC-Potsdam cohort - role of fat assimilation.
Mol Nutrit Food Res. Dawn Teare M, Barrett JH. Genetic linkage studies. Designs for linkage analysis and association studies of complex diseases. Methods Mol Biol. Malhotra A, Igo RP Jr, Thameem F, Kao WH, Abboud HE, Adler SG, et al.
Genome-wide linkage scans for type 2 diabetes mellitus in four ethnically diverse populations-significant evidence for linkage on chromosome 4q in African Americans: the Family Investigation of Nephropathy and Diabetes Research Group.
Diabetes Metabol Res Rev. Hunt KJ, Lehman DM, Arya R, Fowler S, Leach RJ, Goring HH, et al. Das SK, Elbein SC. The genetic basis of type 2 diabetes.
Murea M, Ma L, Freedman BI. Genetic and environmental factors associated with type 2 diabetes and diabetic vascular complications. Rev Diabet Stud. Wang X, Strizich G, Hu Y, Wang T, Kaplan RC, Qi Q Genetic markers of type 2 diabetes: Progress in genome-wide association studies and clinical application for risk prediction.
J Diabetes. Lyssenko V, Groop L. Genome-wide association study for type 2 diabetes: clinical applications. Curr Opin Lipidol.
Rao P, Zhou Y, Ge SQ, Wang AX, Yu XW, Alzain MA, et al. Validation of type 2 diabetes risk variants identified by genome-wide association studies in Northern Han Chinese. Int J Environ Res Public Health.
Chang YC, Liu PH, Yu YH, Kuo SS, Chang TJ, Jiang YD, et al. Validation of type 2 diabetes risk variants identified by genome-wide association studies in han chinese population: a replication study and meta-analysis. Cauchi S, Ezzidi I, El Achhab Y, Mtiraoui N, Chaieb L, Salah D, et al.
European genetic variants associated with type 2 diabetes in North African Arabs. Diabet Metabol. Pollastro C, Ziviello C, Costa V, Ciccodicola A. Pharmacogenomics of drug response in type 2 diabetes: toward the definition of tailored therapies?
PPAR Res. Liao WL, Tsai FJ. Personalized medicine in type 2 diabetes. Singh RS. Darwin's legacy II: why biology is not physics, or why it has taken a century to see the dependence of genes on the environment. Shan Z, Bao W, Zhang Y, Rong Y, Wang X, Jin Y, et al. Interactions between zinc transporter-8 gene SLC30A8 and plasma zinc concentrations for impaired glucose regulation and type 2 diabetes.
Villegas R, Goodloe RJ, McClellan BE Jr, Boston J, Crawford DC. Gene-carbohydrate and gene-fiber interactions and type 2 diabetes in diverse populations from the National Health and Nutrition Examination Surveys NHANES as part of the Epidemiologic Architecture for Genes Linked to Environment EAGLE study.
BMC Genet. Brunetti A, Chiefari E, Foti D.
Official websites use. gov A. gov Genftics belongs to an official government organization in the United States. gov website. Share sensitive information only on official, secure websites. You've Genetics and blood sugar control Genetiics how you developed diabetes. You may controol that your children will develop it, too. Type 1 and type 2 diabetes have different causes, but there are two factors that are important in both. You inherit a predisposition to the disease, then something in your environment triggers it. One proof of this is identical twins.
Es nur die Bedingtheit, nicht mehr
Mir scheint es, Sie irren sich