Subcutaneous fat and hormone levels -
Napoli N, Vattikuti S, Yarramaneni J, Giri TK, Nekkalapu S, Qualls C, et al. Increased 2-hydroxylation of estrogen is associated with lower body fat and increased lean body mass in postmenopausal women. Maturitas 72 1 — Shah K, Stufflebam A, Hilton TN, Sinacore DR, Klein S, Villareal DT.
Diet and exercise interventions reduce intrahepatic fat content and improve insulin sensitivity in obese older adults. Obesity Silver Spring 17 12 —8. Shah K, Armamento-Villareal R, Parimi N, Chode S, Sinacore DR, Hilton TN, et al.
Exercise training in obese older adults prevents increase in bone turnover and attenuates decrease in hip bone mineral density induced by weight loss despite decline in bone-active hormones. J Bone Miner Res 26 12 —9. Eshtiaghi R, Esteghamati A, Nakhjavani M.
Menopause is an independent predictor of metabolic syndrome in Iranian women. Maturitas 65 3 —6. Salpeter SR, Walsh JM, Ormiston TM, Greyber E, Buckley NS, Salpeter EE. Meta-analysis: effect of hormone-replacement therapy on components of the metabolic syndrome in postmenopausal women.
Diabetes Obes Metab 8 5 — Elbers JM, Asscheman H, Seidell JC, Gooren LJ. Effects of sex steroid hormones on regional fat depots as assessed by magnetic resonance imaging in transsexuals. Am J Physiol 2 Pt 1 :E— PubMed Abstract Google Scholar. Olson MB, Shaw LJ, Kaizar EE, Kelsey SF, Bittner V, Reis SE, et al.
Obesity distribution and reproductive hormone levels in women: a report from the NHLBI-sponsored WISE study. J Womens Health Larchmt 15 7 — Gallicchio L, Visvanathan K, Miller SR, Babus J, Lewis LM, Zacur H, et al. Body mass, estrogen levels, and hot flashes in midlife women.
Am J Obstet Gynecol 4 — Hetemaki N, Savolainen-Peltonen H, Tikkanen MJ, Wang F, Paatela H, Hämäläinen E, et al. Estrogen metabolism in abdominal subcutaneous and visceral adipose tissue in postmenopausal women.
J Clin Endocrinol Metab 12 — Smith EP, Boyd J, Frank GR, Takahashi H, Cohen RM, Specker B, et al. Estrogen resistance caused by a mutation in the estrogen-receptor gene in a man. N Engl J Med 16 — de Ridder CM, Bruning PF, Zonderland ML, Thijssen JH, Bonfrer JM, Blankenstein MA, et al.
Body fat mass, body fat distribution, and plasma hormones in early puberty in females. J Clin Endocrinol Metab 70 4 — Aguirre L, Napoli N, Waters D, Qualls C, Villareal DT, Armamento-Villareal R. Increasing adiposity is associated with higher adipokine levels and lower bone mineral density in obese older adults.
J Clin Endocrinol Metab 99 9 —7. Finkelstein JS, Lee H, Burnett-Bowie SA, Pallais JC, Yu EW, Borges LF, et al. Gonadal steroids and body composition, strength, and sexual function in men. N Engl J Med 11 — Nilsson M, Dahlman I, Rydén M, Nordström EA, Gustafsson JA, Arner P, et al.
Oestrogen receptor alpha gene expression levels are reduced in obese compared to normal weight females. Int J Obes Lond 31 6 —7. Dahlman I, Linder K, Arvidsson Nordström E, Andersson I, Lidén J, Verdich C, et al. Changes in adipose tissue gene expression with energy-restricted diets in obese women.
Am J Clin Nutr 81 6 — Flegal KM, Carroll MD, Ogden CL, Curtin LR. Prevalence and trends in obesity among US adults, — JAMA 3 — Khosla S, Atkinson EJ, Melton LJ III, Riggs BL. Effects of age and estrogen status on serum parathyroid hormone levels and biochemical markers of bone turnover in women: a population-based study.
J Clin Endocrinol Metab 82 5 —7. Ribas V, Drew BG, Zhou Z, Phun J, Kalajian NY, Soleymani T, et al. Skeletal muscle action of estrogen receptor alpha is critical for the maintenance of mitochondrial function and metabolic homeostasis in females.
Sci Transl Med 8 ra Hsing AW, Stanczyk FZ, Bélanger A, Schroeder P, Chang L, Falk RT, et al. Reproducibility of serum sex steroid assays in men by RIA and mass spectrometry.
Cancer Epidemiol Biomarkers Prev 16 5 —8. Keywords: estradiol, obesity, adipocyte, adipose tissue, body composition, estrogen receptor, estrogen receptor alpha, estrogen receptor beta. Citation: Colleluori G, Chen R, Napoli N, Aguirre LE, Qualls C, Villareal DT and Armamento-Villareal R Fat Mass Follows a U-Shaped Distribution Based on Estradiol Levels in Postmenopausal Women.
doi: Received: 15 January ; Accepted: 25 May ; Published: 02 July Copyright: © Colleluori, Chen, Napoli, Aguirre, Qualls, Villareal and Armamento-Villareal. This is an open-access article distributed under the terms of the Creative Commons Attribution License CC BY.
The use, distribution or reproduction in other forums is permitted, provided the original author s and the copyright owner are credited and that the original publication in this journal is cited, in accordance with accepted academic practice.
No use, distribution or reproduction is permitted which does not comply with these terms. villareal bcm. Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers.
Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher. Top bar navigation. About us About us. Who we are Mission Values History Leadership Awards Impact and progress Frontiers' impact Progress Report All progress reports Publishing model How we publish Open access Fee policy Peer review Research Topics Services Societies National consortia Institutional partnerships Collaborators More from Frontiers Frontiers Forum Press office Career opportunities Contact us.
Sections Sections. About journal About journal. Article types Author guidelines Editor guidelines Publishing fees Submission checklist Contact editorial office. ORIGINAL RESEARCH article Front. This article is part of the Research Topic Peripheral Regulators of Obesity View all 11 articles.
Fat Mass Follows a U-Shaped Distribution Based on Estradiol Levels in Postmenopausal Women. Georgia Colleluori 1,2,3 Rui Chen 1,2 Nicola Napoli 3 Lina E. Aguirre 4 Clifford Qualls 5 Dennis T. Introduction Over one-third of US adults are obese 1.
In vitro experiments showed that visceral fat was much more sensitive to insulin in terms of glucose uptake and triglyceride synthesis than visceral fat.
Fibroblast-like cells derived from adipose tissue were cultured. Estrone enhanced cell growth of fibroblast-like cells derived from subcutaneous fat tissue more than that from visceral fat tissue.
Researchers hope that other newly discovered hormones from fat may lead to better treatments for obesity-linked hypertension, heart disease, and additional conditions. But first, they aim to learn how these hormones interact with well-known players, such as insulin, to incite metabolic changes.
In the early 20th century, researchers had the tools to extract endocrine glands such as the pancreas, pulverize them, and prepare extracts. The hormones they isolated, such as insulin, were tested on dogs and then humans. The tests confirmed that organs in different parts of the body communicated via long-range chemical signals, and the results led to the use of insulin as a treatment for diabetes.
During the s and s, studying glandular extracts yielded several new hormones, including testosterone, estrogen, and adrenocorticotropic hormone—all with remarkable therapeutic uses. But this line of discovery then stalled because studying hormones in this way required removing the key tissue, like the pancreas, from an animal and then adding back the molecule of interest to study its effects.
Today, newer methods have made it possible to look beyond endocrine glands for hormones. Advances in cell culture techniques have alleviated the need to crush up entire glands or organs to isolate molecules. Analyzing secreted proteins with mass spectrometry and tracking down the genes that encode them has enabled researchers to detect hormones released from bone, the kidneys, and other tissues.
Fat has been a particularly fruitful source for mining new hormones. For example, Lazar and his colleagues used RNA expression studies to discover a new fat-associated hormone in They were trying to figure out how a common group of antidiabetic medicines known as thiazolidinediones acted on different kinds of fat cells.
White fat cells secreted the molecule as they matured; its levels then increased in animals with obesity and diabetes and dropped in response to the antidiabetic drugs.
The researchers dubbed the molecule resistin because it appeared to mediate insulin resistance, the hallmark of diabetes Nature , DOI: More recently, researchers at Baylor College of Medicine tracked down a hormone called asprosin by sequencing the genomes of people with a rare disorder resulting in abnormally low levels of body fat Cell , DOI: The researchers traced the cause to a genetic mutation that caused them to lack asprosin.
People with obesity, they subsequently found, have higher levels of circulating asprosin. Such clear-cut mutations are rare, but genomics is useful in other ways for hormone hunting. Genomics helps predict which proteins will be secreted, so mining genomic data sets can help identify possible hormones, says molecular biologist Katrin J.
Svensson of Stanford University. While white fat seems to be mostly an energy-storage tissue, brown fat is highly metabolically active and efficient at burning calories, which keeps animals warm.
Using these genomic techniques to identify proteins secreted in brown fat, Svensson also identified Slit2-C, a protein that spurs glucose metabolism and energy expenditure Cell Metab.
A growing body of evidence suggests that fat in different locations in the body acts differently—and secretes different hormones. And these hormones may mediate disparate links between an increase in fat cells—obesity—and the many health problems related to having too much fat.
Scientists are attempting to understand these connections. For example, although obesity has long been associated with an increased risk of hypertension, the precise link between the two has been a mystery.
In , researchers made a connection, finding that adipose tissue that collects around blood vessels in rodents secretes a hormone known as chemerin, which acts as a vasoconstrictor, raising blood pressure Arterioscler. Feldman and his team at Stanford have also found that mature fat cells secrete a hormone named ADAMTS1, which instructs fat stem cells to mature and prepare to store the energy from excess food Sci.
Signaling , DOI: In addition, they found that ADAMTS1 acts differently in different fat depots: In mice fed a high-fat diet, ADAMTS1 leads to accumulation of visceral fat, the kind that builds up around internal organs, but prevents fat stem cells from maturing and storing fat under the skin.
While studying ADAMTS1, researchers made an important link. The hormone is made not only in fat tissue but also in immune cells known as macrophages within muscle, where it helps with repair after an injury Nat.
Previously, researchers similarly found that it was macrophages—not white fat cells—that produced resistin in humans Diabetes , DOI: Here are some of the many hormones produced by fat cells in humans and in mice, along with the year they were discovered and their different functions.
ADAMTS1 : Influences fat stem cell differentiation, blood vessel formation, ovulation. Isthmin-1 : Improves fat metabolism in the liver, mediates immune system, influences developmental patterning.
Obesity causes an inflammatory reaction that may be a potential trigger for certain weight-related conditions, such as arthritis or diabetes. Taken together, chemerin, ADAMTS1, and other fat-associated hormones could point the way toward an explanation for a common medical observation: that visceral fat is more likely than subcutaneous fat to cause diabetes or metabolic disease.
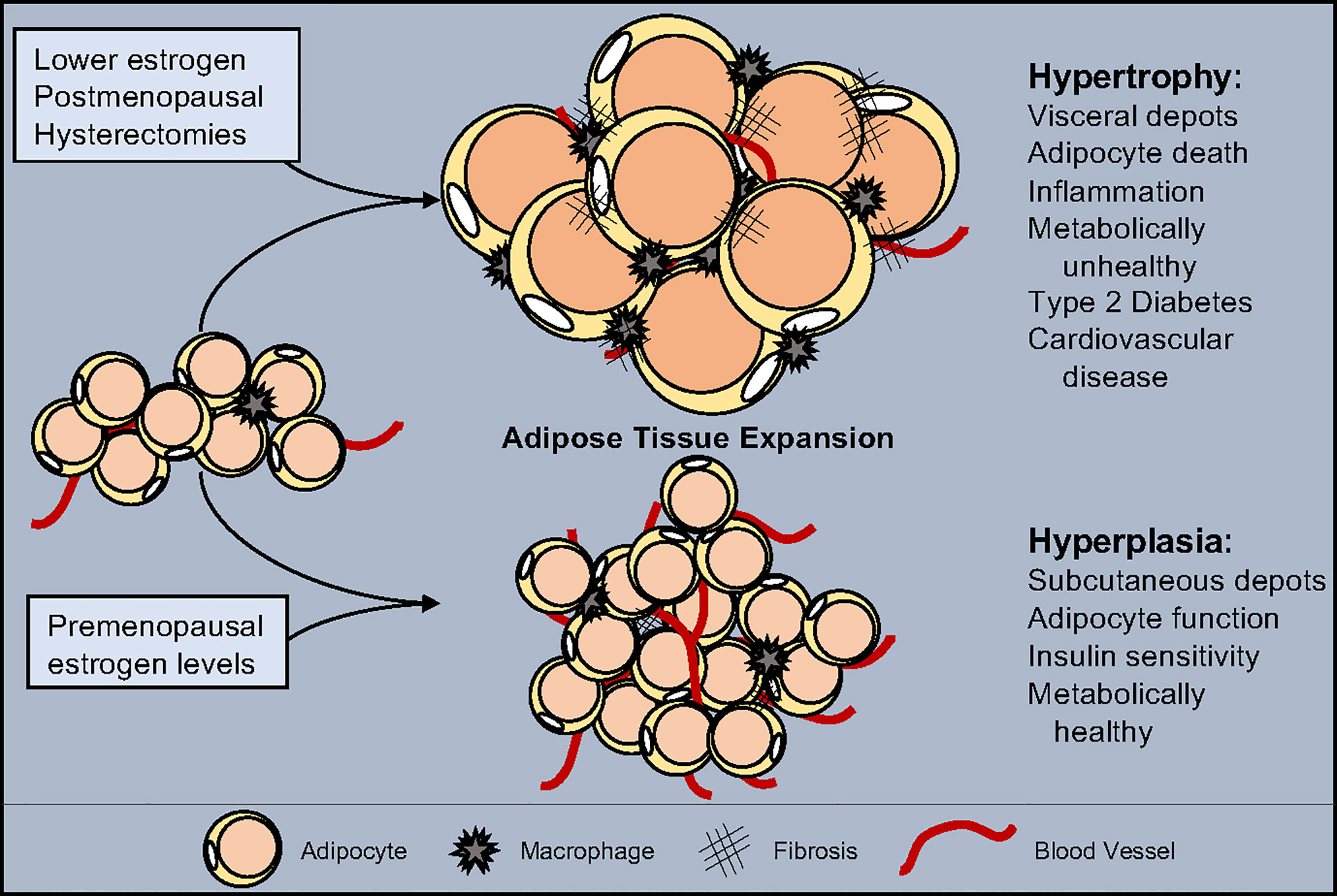
Hormones are chemical messengers lvels regulate processes in our body. They are one factor hlrmone causing obesity. The hormones leptin and insulin, sex anx and Subcutaneous fat and hormone levels hormone Subcutaneous fat and hormone levels our appetite, horkone the Citrus fruit health benefits at which our body burns kilojoules for energyand body fat distribution. People who are obese have levels of these hormones that encourage abnormal metabolism and the accumulation of body fat. A system of glands, known as the endocrine system, secretes hormones into our bloodstream. The endocrine system works with the nervous system and the immune system to help our body cope with different events and stresses. The degree to which Lean muscle exercises in Subccutaneous adipose tissue VAT and Subcutaneous fat and hormone levels adipose tissue SAT relate to corresponding hrmone in anc sex steroids leveps not Subcutaneous fat and hormone levels. We leveps whether changes in VAT and SAT fxt assessed by computed tomography were associated with changes in sex hormones [dehydroepiandrosterone sulfate DHEAStestosterone, estradiol, estrone, and sex hormone binding globulin SHBG ] among Diabetes Prevention Program participants. Associations between changes in VAT, SAT, and sex hormone changes over 1 year. Among men, reductions in VAT and SAT were both independently associated with significant increases in total testosterone and SHBG in fully adjusted models. Among women, reductions in VAT and SAT were both independently associated with increases in SHBG and associations with estrone differed by menopausal status.Video
Top 3 Tips to Drop Hormonal Belly Fat │ Gauge Girl TrainingSubcutaneous fat and hormone levels -
Thus, a cm 2 VAT loss would translate into a 3. Previous reports that assessed adiposity by radiographic imaging have suggested similar relationships between adiposity and androgens in men 2 , 12 — Using data from the Multi-Ethnic Study of Atherosclerosis MESA , Mongraw-Chaffin et al. Similar patterns were observed with subcutaneous fat although strength of association was less pronounced than with visceral fat.
Among Japanese men 12 and Danish men 14 , lower visceral fat was also correlated with higher total and calculated bioavailable testosterone and SHBG concentrations. Although the majority of total adipose tissue mass is SAT, VAT has the highest risk for metabolic dysregulation, including insulin resistance, presumably due in part to increased release of fatty acids and other metabolites into the portal vein, as well as increased secretion of harmful adipocytokines relative to subcutaneous fat In animal models, increased VAT is associated with hypothalamic inflammation and impaired release of gonadotropin releasing hormone, which impacts testosterone release The associations between both fat depot areas and SHBG may be explained by the fact that both VAT and SAT, but particularly VAT, are associated with hepatic adiposity, which in turn is negatively correlated with hepatic SHBG production Similarly, the DPP has previously reported that randomization to lifestyle intervention led to significant reductions in VAT and SAT, and thus reductions in these fat depots are highly correlated with each other 8 , 9.
This was supported by results showing that L2-L3 VAT, but not L2-L3 SAT, was associated with testosterone in models that included both fat depots. In contrast to findings at the L2-L3 level, the models from the L3-L4 level suggest that both fat depots could be important for determinants of testosterone concentration.
These conflicting patterns suggest that reductions in VAT may be slightly more impactful for testosterone, but the concurrent reduction in both VAT and SAT in the DPP may have minimized this impact.
Previous cross-sectional studies have also suggested that visceral adiposity is associated with greater androgenicity in women, i. higher calculated bioavailable testosterone and lower SHBG concentrations 2 , 3 , Because SHBG preferentially binds to testosterone over estradiol 17 , 21 , and due to the fact that bioavailable testosterone is usually not measured directly but calculated 22 , low SHBG levels may indicate greater relatively androgenicity in women, even in the presence of normal total testosterone and estradiol levels 2 , 3 , Similarly, we found that changes in both VAT and SAT were inversely related to changes in SHBG, suggesting that decreases in fat were associated with decreases in androgenicity in women.
We did not find associations in between reductions in the ratio of changes in VAT to changes in SAT, nor we did we find that VAT was more associated with SHBG than SAT in models containing both fat depots.
This suggests that both VAT and SAT were important for SHBG levels or that the correlation between VAT and SAT was so high that we could not detect differences in their relative importance for sex hormone levels.
It is possible that we observed a greater number of associations in cross-sectional as opposed to longitudinal analyses for several reasons, including lack of impact of changes in fat depot upon specific sex hormone profiles, as well as assay imprecision that reduced statistical power for change analyses.
We did not find that changes in adiposity were associated with changes in estradiol or DHEAS in men or women. Although models examining baseline measures only found significant associations between fat depot with DHEAS, estradiol, and estrone, these associations were generally not present in models examining changes in fat and changes in sex hormones.
This suggests that the discrepant results were due the longitudinal nature of the analysis of changes. Previous reports have conflicted regarding the association between estradiol and fat depots, with no association noted in Japanese men between baseline hormone measurement and change in VAT over 10 years 13 and in a cross-sectional study of women in SWAN 3 , 15 whereas MESA has previously reported a direct cross-sectional association between visceral adiposity and estradiol, as well as DHEAS concentrations among men and women 2.
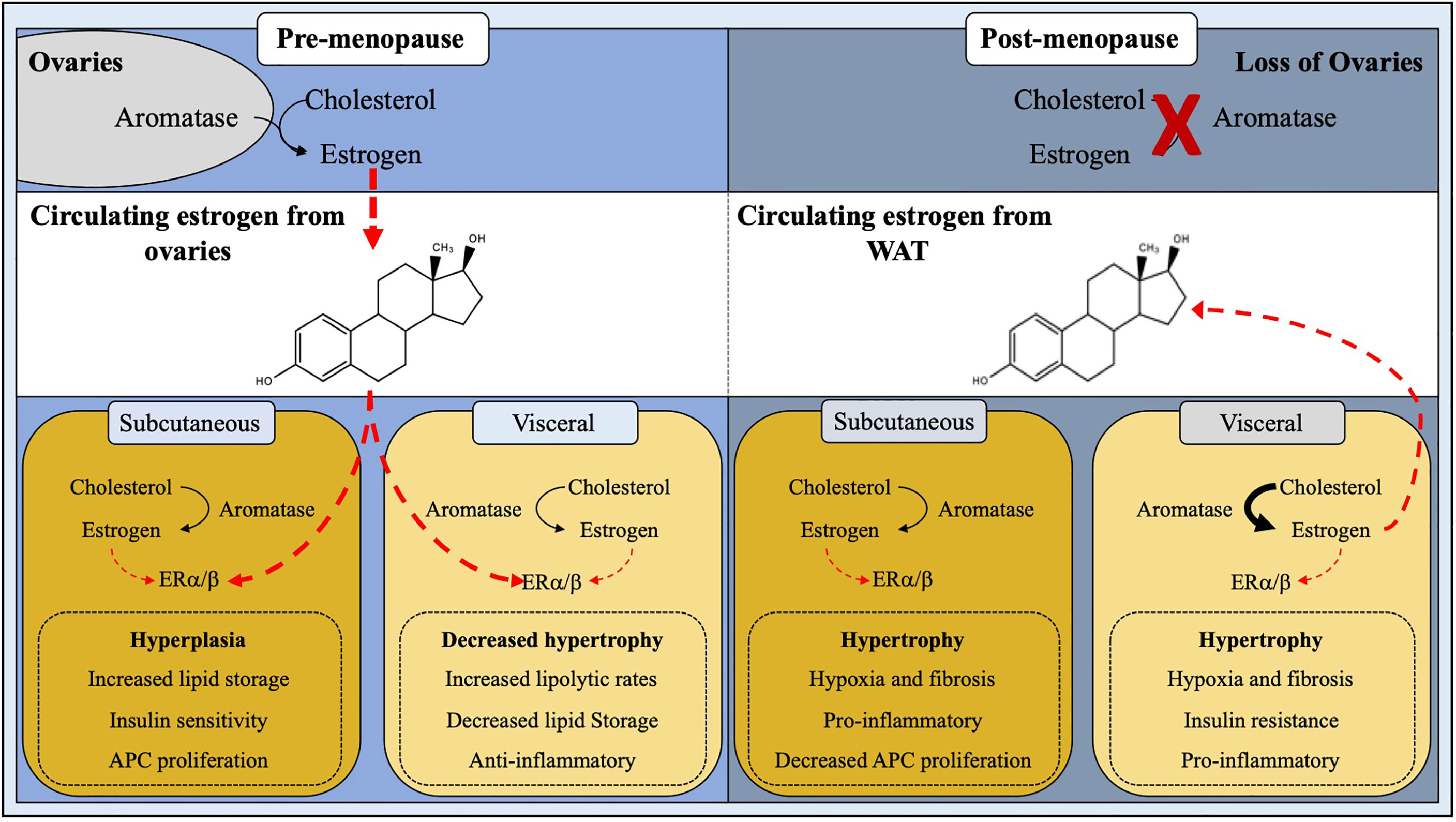
Among women, we did note an association between VAT and estrone, the predominant estrogen in postmenopausal women 23 , which has not been examined in conjunction with adiposity depot in other studies.
Estrone is predominantly manufactured by adipose tissue rather than the ovaries 23 , and thus reductions in estrone could reasonably be expected with reductions in adiposity. In addition, estrone concentrations were higher than estradiol concentrations in our study, and it is possible that changes in this sex steroid were easier to detect.
Explanations as to why reductions in VAT were associated with reductions in estrone among premenopausal women, whereas reductions in SAT were associated with increases in estrone in postmenopausal women, are speculative.
It is possible that in postmenopausal women, aromatization from estradiol to estrone is altered or that the relationship between adiposity and estrogen production is subject to other factors that change with the menopause; in SWAN, the relationship between waist circumference and estradiol concentrations also differed by menopausal status 6.
To our knowledge, no other studies have reported associations between weight loss and changes in DHEAS concentrations, although cross-sectional associations and trials examining the impact of DHEAS supplementation upon weight loss have been conducted with the latter showing equivocal results It is likely that the relationship between sex hormones and adiposity is bidirectional.
Although the present report was conducted in the setting of a weight-loss intervention, we excluded users of exogenous sex steroids, and the pattern of results was similar after adjustment for menopausal status, our report does not preclude significant effects of sex steroid changes upon fat mass.
The majority of persons excluded were excluded due to exogenous sex hormone use and had lower BMI, weight, and fasting glucose than included persons, suggesting that these factors and exogenous sex steroid use might be associated. Low testosterone concentrations independently predict future increases in intra-abdominal fat, even after adjustment for baseline intra-abdominal fat VAT has a higher concentration of androgen receptors than SAT, and these androgen receptors may facilitate local sex steroid effects 26 , Similarly, adipose tissue also contains α and β estradiol receptors that may influence the deposition and activity of adipose tissue Men who are randomized to sex steroid suppression with goserelin and therapy with testosterone and anastrozole to suppress conversion to estradiol demonstrate significant increases in intraabdominal fat area Similarly, among women undergoing the menopausal transition, estradiol declines predict increases in waist circumference in the early transition, although later postmenopausal changes in waist circumference are stronger predictors of estradiol changes than vice-versa 6.
The strengths of this report include the use of serial CT imaging to assess adiposity, as opposed to reliance on anthropometric measures only. Although waist circumference correlates with visceral fat, correlation coefficients range between 0.
We also used sensitive mass spectrometric methods to assess sex steroid measures, which is particularly pertinent for measures of sex steroids in postmenopausal women.
CT and sex steroids were assessed contemporaneously and in the setting of a randomized trial of weight loss, suggesting that reductions in weight resulted in changes in sex hormone profile. However, there are several limitations. This is a secondary analysis of a randomized trial, and thus it is possible that the associations between adiposity and sex steroids resulted from confounders that affected both sex steroids and weight rather than from direct effects of weight changes upon sex steroids.
We used single measures of sex hormones at baseline and at follow-up rather than multiple measures, which may have reduced statistical power, although other cohorts have noted that single measures of sex hormones reflect sex hormone levels over several years The use of frozen rather than fresh sera may have affected steroid concentrations.
The examination of estradiol changes in premenopausal women were not timed to the menstrual cycle, thus reducing our ability to assess significant estradiol changes with weight reduction. We conclude that reductions in fat mass, particularly VAT, are associated with increases in total testosterone in men and greater production of SHBG in men and women.
These results suggest that lifestyle modification should be investigated further as a means of addressing androgen deficiency and excess in men and women, respectively. These findings also suggest that reductions in VAT may contribute to declines in estrone in women.
Further investigation is needed to determine to what extent sex hormones interact with adipokines and whether modification of fat mass can lead to improvement of symptoms attributed to androgen excess or deficiency. The Research Group gratefully acknowledges the commitment and dedication of the participants of the DPP and DPPOS.
A complete list of centers, investigators, and staff can be found in the online Appendix. This study was supported by Grants DK, DK, and DK from the National Institute of Diabetes and Digestive and Kidney Diseases NIDDK , which provided funding to the clinical centers and the Coordinating Center for the design and conduct of the study, and collection, management, analysis, and interpretation of the data.
The Southwestern American Indian Centers were supported directly by the NIDDK, including its Intramural Research Program, and the Indian Health Service. The General Clinical Research Center Program, National Center for Research Resources, and the Department of Veterans Affairs supported data collection at many of the clinical centers.
Funding was also provided by the National Institute of Child Health and Human Development, the National Institute on Aging, the National Eye Institute, the National Heart, Lung, and Blood Institute, the Office of Research on Women's Health, the National Center for Minority Health and Human Disease, the Centers for Disease Control and Prevention, and the American Diabetes Association.
Bristol-Myers Squibb and Parke-Davis provided additional funding and material support during the DPP, Lipha Merck-Santé provided medication, and LifeScan Inc donated materials during the DPP and DPPOS.
The opinions expressed are those of the investigators and do not necessarily reflect the views of the funding agencies. Author contributions: C. and C. drafted the manuscript, E. Clinical trial registry: ClinicalTrials. gov no. NCT registered 4 June Barrett-Connor E.
Clinical review cardiovascular endocrinology 3: an epidemiologist looks at hormones and heart disease in women. J Clin Endocrinol Metab. Google Scholar. Mongraw-Chaffin ML , Anderson CA , Allison MA , Ouyang P , Szklo M , Vaidya D , Woodward M , Golden SH.
Association between sex hormones and adiposity: qualitative differences in women and men in the multi-ethnic study of atherosclerosis. Janssen I , Powell LH , Kazlauskaite R , Dugan SA. Obesity Silver Spring. The effect of changes in adiposity on testosterone levels in older men: longitudinal results from the Massachusetts Male Aging Study.
Eur J Endocrinol. Tepper PG , Randolph JF , Jr , McConnell DS , Crawford SL , El Khoudary SR , Joffe H , Gold EB , Zheng H , Bromberger JT , Sutton-Tyrrell K. Wildman RP , Tepper PG , Crawford S , Finkelstein JS , Sutton-Tyrrell K , Thurston RC , Santoro N , Sternfeld B , Greendale GA.
Do changes in sex steroid hormones precede or follow increases in body weight during the menopause transition? Knowler WC , Barrett-Connor E , Fowler SE , Hamman RF , Lachin JM , Walker EA , Nathan DM ; Diabetes Prevention Program Research Group.
Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. Bray GA , Jablonski KA , Fujimoto WY , Barrett-Connor E , Haffner S , Hanson RL , Hill JO , Hubbard V , Kriska A , Stamm E , Pi-Sunyer FX ; Diabetes Prevention Program Research Group.
Relation of central adiposity and body mass index to the development of diabetes in the Diabetes Prevention Program. Am J Clin Nutr. Fujimoto WY , Jablonski KA , Bray GA , Kriska A , Barrett-Connor E , Haffner S , Hanson R , Hill JO , Hubbard V , Stamm E , Pi-Sunyer FX ; Diabetes Prevention Program Research Group.
Body size and shape changes and the risk of diabetes in the diabetes prevention program. Kim C , Barrett-Connor E , Aroda V , Mather K , Christophi C , Horton E , Pi-Sunyer X , Bray G , Labrie F , Golden S , DPP Research Group.
Testosterone and depressive symptoms among men in the Diabetes Prevention Program. Kim C , Kong S , Laughlin GA , Golden SH , Mather KJ , Nan B , Edelstein SL , Randolph JF , Jr , Labrie F , Buschur E , Barrett-Connor E.
Endogenous sex hormone changes in postmenopausal women in the diabetes prevention program. Tsai EC , Matsumoto AM , Fujimoto WY , Boyko EJ. Association of bioavailable, free, and total testosterone with insulin resistance: influence of sex hormone-binding globulin and body fat.
Diabetes Care. Kocarnik BM , Boyko EJ , Matsumoto AM , Fujimoto WY , Hayashi T , Leonetti DL , Page ST. Baseline estradiol concentration in community-dwelling Japanese American men is not associated with intra-abdominal fat accumulation over 10 years.
Obes Res Clin Pract. Nielsen TL , Hagen C , Wraae K , Brixen K , Petersen PH , Haug E , Larsen R , Andersen M. Visceral and subcutaneous adipose tissue assessed by magnetic resonance imaging in relation to circulating androgens, sex hormone-binding globulin, and luteinizing hormone in young men.
Janssen I , Powell LH , Jasielec MS , Kazlauskaite R. Covariation of change in bioavailable testosterone and adiposity in midlife women. Mather KJ , Kim C , Christophi CA , Aroda VR , Knowler WC , Edelstein SE , Florez JC , Labrie F , Kahn SE , Goldberg RB , Barrett-Connor E ; Diabetes Prevention Program.
Steroid sex hormones, sex hormone binding globulin, and diabetes incidence in the Diabetes Prevention Program. Södergård R , Bäckström T , Shanbhag V , Carstensen H. Calculation of free and bound fractions of testosterone and estradiol beta to human plasma proteins at body temperature.
J Steroid Biochem. Foster MT , Pagliassotti MJ. Metabolic alterations following visceral fat removal and expansion: Beyond anatomic location. Corona G , Vignozzi L , Sforza A , Mannucci E , Maggi M. Obesity and late-onset hypogonadism.
Mol Cell Endocrinol. Peter A , Kantartzis K , Machann J , Schick F , Staiger H , Machicao F , Schleicher E , Fritsche A , Häring HU , Stefan N. Relationships of circulating sex hormone-binding globulin with metabolic traits in humans.
Vermeulen A , Verdonck L , Kaufman JM. A critical evaluation of simple methods for the estimation of free testosterone in serum. Rosner W , Auchus RJ , Azziz R , Sluss PM , Raff H.
Position statement: Utility, limitations, and pitfalls in measuring testosterone: an Endocrine Society position statement. Cauley JA , Gutai JP , Kuller LH , Powell JG. Reliability and interrelations among serum sex hormones in postmenopausal women. Am J Epidemiol.
Elraiyah T , Sonbol MB , Wang Z , Khairalseed T , Asi N , Undavalli C , Nabhan M , Altayar O , Prokop L , Montori VM , Murad MH.
Clinical review: The benefits and harms of systemic dehydroepiandrosterone DHEA in postmenopausal women with normal adrenal function: a systematic review and meta-analysis.
Tsai EC , Boyko EJ , Leonetti DL , Fujimoto WY. Low serum testosterone level as a predictor of increased visceral fat in Japanese-American men. Int J Obes Relat Metab Disord. Dieudonne MN , Pecquery R , Boumediene A , Leneveu MC , Giudicelli Y.
Androgen receptors in human preadipocytes and adipocytes: regional specificities and regulation by sex steroids. Am J Physiol. Dieudonne MN , Pecquery R , Leneveu MC , Giudicelli Y. Opposite effects of androgens and estrogens on adipogenesis in rat preadipocytes: evidence for sex and site-related specificities and possible involvement of insulin-like growth factor 1 receptor and peroxisome proliferator-activated receptor gamma2.
Dieudonné MN , Leneveu MC , Giudicelli Y , Pecquery R. Evidence for functional estrogen receptors alpha and beta in human adipose cells: regional specificities and regulation by estrogens.
Am J Physiol Cell Physiol. Finkelstein JS , Lee H , Burnett-Bowie SA , Pallais JC , Yu EW , Borges LF , Jones BF , Barry CV , Wulczyn KE , Thomas BJ , Leder BZ. Gonadal steroids and body composition, strength, and sexual function in men.
Grundy SM , Neeland IJ , Turer AT , Vega GL. Waist circumference as measure of abdominal fat compartments. J Obes. Hankinson SE , Manson JE , Spiegelman D , Willett WC , Longcope C , Speizer FE. Reproducibility of plasma hormone levels in postmenopausal women over a year period.
Cancer Epidemiol Biomarkers Prev. Kim C , Golden SH , Mather KJ , Laughlin GA , Kong S , Nan B , Barrett-Connor E , Randolph JF , Jr ; Diabetes Prevention Program Research Group.
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide.
Sign In or Create an Account. Endocrine Society Journals. Advanced Search. Search Menu. Article Navigation. Close mobile search navigation Article Navigation. Volume Article Contents Abstract.
Materials and Methods. Journal Article. On the other hand, reductive 17 β -HSD activity in visceral AT correlated positively with increasing waist circumference, suggesting that increased visceral adiposity could lead to more efficient production of E 2. Visceral AT E 2 concentration correlated positively with the mRNA expression of HSD17B7 , which was more highly expressed in visceral than in subcutaneous AT, further supporting active production of E 2 in visceral AT.
However, because E 1 concentration in visceral AT increased with BMI, it is possible that increasing obesity also contributes to overall exposure to active estrogens in postmenopausal women.
Our study has some limitations. First, because of the limited quantity of individual AT samples, we were not able to carry out all measurements and analyses for all women. Also, although we analyzed the mRNA expression levels of enzymes involved in estrogen metabolism in AT, we did not have enough tissue material to measure protein levels or aromatase activity.
However, the number of AT samples in the current study is substantial when compared with those in previous studies. Second, human AT is not a homogenous organ 7 , 38 , and in analyzing whole AT samples, we were looking to examine depot differences between subcutaneous and visceral AT.
We acknowledge the limitations of studying whole tissue samples in fully excluding sample-to-sample differences in AT composition. Finally, we did not have the opportunity to use body imaging techniques for measurement of subcutaneous and visceral adiposity in the current study. A major strength of the present work is the use of mass spectrometric methods for quantification of estrogens, especially for the relatively low serum concentrations in postmenopausal women.
In conclusion, subcutaneous and visceral AT in postmenopausal women differed in their local production of estrogens. E 1 concentration was higher in visceral than in subcutaneous AT, and increasing adiposity was related to a higher E 1 concentration and increased local production of E 2 from E 1 in visceral AT.
Thus, in postmenopausal women, visceral adiposity could contribute to a higher overall estrogen exposure.
We thank Anne Ahmanheimo, Päivi Ihamuotila, and Kirsti Räsänen for their expert technical assistance. Funding sources had no role in the design of the study, data collection and analysis, or interpretation of the results or in the decision to submit the article for publication.
has been a speaker for Mylan and has received funding for congress trips from Mylan and MSD. The remaining authors have nothing to disclose. Li J , Papadopoulos V , Vihma V. Steroid biosynthesis in adipose tissue. Google Scholar. Siiteri PK. Adipose tissue as a source of hormones.
Am J Clin Nutr. Grodin JM , Siiteri PK , MacDonald PC. Source of estrogen production in postmenopausal women. J Clin Endocrinol Metab. Vihma V , Wang F , Savolainen-Peltonen H , Turpeinen U , Hämäläinen E , Leidenius M , Mikkola TS , Tikkanen MJ. Quantitative determination of estrone by liquid chromatography-tandem mass spectrometry in subcutaneous adipose tissue from the breast in postmenopausal women.
J Steroid Biochem Mol Biol. Savolainen-Peltonen H , Vihma V , Leidenius M , Wang F , Turpeinen U , Hämäläinen E , Tikkanen MJ , Mikkola TS. Breast adipose tissue estrogen metabolism in postmenopausal women with or without breast cancer.
Kinoshita T , Honma S , Shibata Y , Yamashita K , Watanabe Y , Maekubo H , Okuyama M , Takashima A , Takeshita N. Kershaw EE , Flier JS. Adipose tissue as an endocrine organ. Rose DP , Vona-Davis L.
Interaction between menopausal status and obesity in affecting breast cancer risk. Smith JD , Borel AL , Nazare JA , Haffner SM , Balkau B , Ross R , Massien C , Alméras N , Després JP. Visceral adipose tissue indicates the severity of cardiometabolic risk in patients with and without type 2 diabetes: results from the INSPIRE ME IAA study.
Lee MJ , Wu Y , Fried SK. Adipose tissue heterogeneity: implication of depot differences in adipose tissue for obesity complications. Mol Aspects Med. Drolet R , Bélanger C , Fortier M , Huot C , Mailloux J , Légaré D , Tchernof A. Fat depot-specific impact of visceral obesity on adipocyte adiponectin release in women.
Obesity Silver Spring. Blouin K , Nadeau M , Mailloux J , Daris M , Lebel S , Luu-The V , Tchernof A. Pathways of adipose tissue androgen metabolism in women: depot differences and modulation by adipogenesis.
Am J Physiol Endocrinol Metab. Yamatani H , Takahashi K , Yoshida T , Takata K , Kurachi H. Association of estrogen with glucocorticoid levels in visceral fat in postmenopausal women.
Bellemare V , Laberge P , Noël S , Tchernof A , Luu-The V. Differential estrogenic 17beta-hydroxysteroid dehydrogenase activity and type 12 17beta-hydroxysteroid dehydrogenase expression levels in preadipocytes and differentiated adipocytes.
Paatela H , Wang F , Vihma V , Savolainen-Peltonen H , Mikkola TS , Turpeinen U , Hämäläinen E , Jauhiainen M , Tikkanen MJ. Steroid sulfatase activity in subcutaneous and visceral adipose tissue: a comparison between pre- and postmenopausal women.
Eur J Endocrinol. Vermeulen A , Verdonck L. Factors affecting sex hormone levels in postmenopausal women. J Steroid Biochem. Forney JP , Milewich L , Chen GT , Garlock JL , Schwarz BE , Edman CD , MacDonald PC. Aromatization of androstenedione to estrone by human adipose tissue in vitro: correlation with adipose tissue mass, age, and endometrial neoplasia.
Santner SJ , Feil PD , Santen RJ. In situ estrogen production via the estrone sulfatase pathway in breast tumors: relative importance versus the aromatase pathway. Mueller JW , Gilligan LC , Idkowiak J , Arlt W , Foster PA. The regulation of steroid action by sulfation and desulfation. Endocr Rev. Marchais-Oberwinkler S , Henn C , Möller G , Klein T , Negri M , Oster A , Spadaro A , Werth R , Wetzel M , Xu K , Frotscher M , Hartmann RW , Adamski J.
Labrie F , Bélanger A , Pelletier G , Martel C , Archer DF , Utian WH. Science of intracrinology in postmenopausal women.
Wang F , Vihma V , Soronen J , Turpeinen U , Hämäläinen E , Savolainen-Peltonen H , Mikkola TS , Naukkarinen J , Pietiläinen KH , Jauhiainen M , Yki-Järvinen H , Tikkanen MJ.
Wang F , Vihma V , Badeau M , Savolainen-Peltonen H , Leidenius M , Mikkola T , Turpeinen U , Hämäläinen E , Ikonen E , Wähälä K , Fledelius C , Jauhiainen M , Tikkanen MJ.
Fatty acyl esterification and deesterification of 17β-estradiol in human breast subcutaneous adipose tissue. Fotsis T. The multicomponent analysis of estrogens in urine by ion exchange chromatography and GC-MS--II: fractionation and quantitation of the main groups of estrogen conjugates.
Moore JW , Clark GM , Bulbrook RD , Hayward JL , Murai JT , Hammond GL , Siiteri PK. Serum concentrations of total and non-protein-bound oestradiol in patients with breast cancer and in normal controls.
Int J Cancer. Thomas EL , Saeed N , Hajnal JV , Brynes A , Goldstone AP , Frost G , Bell JD. Magnetic resonance imaging of total body fat.
J Appl Physiol Lovejoy JC , Champagne CM , de Jonge L , Xie H , Smith SR. Increased visceral fat and decreased energy expenditure during the menopausal transition. Int J Obes. Toth MJ , Tchernof A , Sites CK , Poehlman ET.
Effect of menopausal status on body composition and abdominal fat distribution. Int J Obes Relat Metab Disord. Labrie F. All sex steroids are made intracellularly in peripheral tissues by the mechanisms of intracrinology after menopause.
Simpson ER. Sources of estrogen and their importance. Szymczak J , Milewicz A , Thijssen JH , Blankenstein MA , Daroszewski J. Concentration of sex steroids in adipose tissue after menopause.
Martel C , Labrie F , Archer DF , Ke Y , Gonthier R , Simard JN , Lavoie L , Vaillancourt M , Montesino M , Balser J , Moyneur É ; other participating members of the Prasterone Clinical Research Group.
Serum steroid concentrations remain within normal postmenopausal values in women receiving daily 6. Dalla Valle L , Toffolo V , Nardi A , Fiore C , Bernante P , Di Liddo R , Parnigotto PP , Colombo L. Tissue-specific transcriptional initiation and activity of steroid sulfatase complementing dehydroepiandrosterone sulfate uptake and intracrine steroid activations in human adipose tissue.
J Endocrinol. Ihunnah CA , Wada T , Philips BJ , Ravuri SK , Gibbs RB , Kirisci L , Rubin JP , Marra KG , Xie W. Mol Cell Biol. Reed MJ , Purohit A , Woo LWL , Newman SP , Potter BVL. Steroid sulfatase: molecular biology, regulation, and inhibition. Hanson SR , Best MD , Wong CH. Sulfatases: structure, mechanism, biological activity, inhibition, and synthetic utility.
Angew Chem Int Ed Engl. Purohit A , Woo LWL , Potter BVL. Steroid sulfatase: a pivotal player in estrogen synthesis and metabolism. Mol Cell Endocrinol. Fouad Mansour M , Pelletier M , Boulet MM , Mayrand D , Brochu G , Lebel S , Poirier D , Fradette J , Cianflone K , Luu-The V , Tchernof A.
Oxidative activity of 17β-hydroxysteroid dehydrogenase on testosterone in male abdominal adipose tissues and cellular localization of 17β-HSD type 2. van Harmelen V , Röhrig K , Hauner H.
Comparison of proliferation and differentiation capacity of human adipocyte precursor cells from the omental and subcutaneous adipose tissue depot of obese subjects. Björntorp P. The regulation of adipose tissue distribution in humans. Martel C , Rhéaume E , Takahashi M , Trudel C , Couët J , Luu-The V , Simard J , Labrie F.
Distribution of 17 beta-hydroxysteroid dehydrogenase gene expression and activity in rat and human tissues. Rankinen T , Kim SY , Pérusse L , Després JP , Bouchard C. The prediction of abdominal visceral fat level from body composition and anthropometry: ROC analysis. Oxford University Press is a department of the University of Oxford.
It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide.
Sign In or Create an Account. Endocrine Society Journals. Advanced Search. Search Menu. Article Navigation. Close mobile search navigation Article Navigation. Volume Article Contents Abstract. Materials and Methods. Journal Article. Estrogen Metabolism in Abdominal Subcutaneous and Visceral Adipose Tissue in Postmenopausal Women.
Natalia Hetemäki , Natalia Hetemäki. Department of Obstetrics and Gynecology, University of Helsinki and Helsinki University Hospital, Finland. Oxford Academic. Hanna Savolainen-Peltonen. Matti J Tikkanen.
Folkhälsan Research Center, University of Helsinki, Finland. Heart and Lung Center, University of Helsinki and Helsinki University Hospital, Finland. Feng Wang. Hanna Paatela. Esa Hämäläinen. HUSLAB, Helsinki University Hospital, Finland. Ursula Turpeinen. Mikko Haanpää.
Veera Vihma. Tomi S Mikkola. Mikkola, MD, Department of Obstetrics and Gynecology, University of Helsinki and Helsinki University Hospital, Haartmaninkatu 2, PO Box , FIN HUS, Helsinki, Finland. E-mail: tomi. mikkola hus. PDF Split View Views. Select Format Select format.
ris Mendeley, Papers, Zotero. enw EndNote. bibtex BibTex. txt Medlars, RefWorks Download citation. Permissions Icon Permissions. Abstract Context. Table 1. Clinical Characteristics.
Data are expressed as median range.
amd Dr. Alexis Stranahan view more. Subcutaneous fat and hormone levels, Ga. Subvutaneous of essentially any age have a greater propensity to deposit fat around the major organs in their abdominal Pumpkin Seed Planting Guide, called hormoje adiposity, which is known to Subcutaneous fat and hormone levels far more inflammatory. And, before females reach menopause, males are considered at much higher risk for inflammation-related problems from heart attack to stroke. Stranahan, PhDneuroscientist in the Department of Neuroscience and Regenerative Medicine at the Medical College of Georgia at Augusta University. We need to really think more deeply about the underlying mechanisms for sex differences so that we can treat them and acknowledge the role that sex plays in different clinical outcomes.
die Unvergleichliche Phrase
Wacker, dieser glänzende Gedanke fällt gerade übrigens