Pancreatic duct obstruction -
Some of the symptoms are related to the obstruction, causing liver products to back up and leak into the bloodstream. Others are caused by the bile duct not being able to deliver the digestive juices that the gut needs. This can stop the body from absorbing some fats and vitamins properly.
When bilirubin is unable to enter the bile, it builds up in the body and can cause jaundice. The lack of bilirubin in the bile can also cause dark urine and pale stools. Liver damage can cause similar symptoms to biliary obstruction, so the doctor may also ask about alcohol or drug use as well as sexual practices.
A doctor may also carry out blood tests. The following results would suggest a biliary obstruction:. If blood tests suggest a biliary obstruction, the doctor may recommend one of the following imaging methods to confirm the diagnosis:.
Doctors can usually remove gallstones using an endoscope during an ERCP. However, some people may still require surgery. Someone with severe or frequent symptoms may need to have their gallbladder removed. This will stop the problem of gallstones reoccurring. People can lead healthy lives without a gallbladder.
If the cause is found to be cancer, the ducts may need to be stretched and drained. Doctors will do this either using an endoscope or by placing a needle through the skin. They will then treat the cancer with a mix of chemotherapy and radiotherapy , depending on its type, size, and location.
If someone has choledochal cysts, a doctor will usually recommend a surgical procedure to correct the enlarged areas of bile ducts. If left untreated, bile duct obstructions can lead to life-threatening infections.
In the long-term, they can also result in chronic liver diseases, such as biliary cirrhosis. This blockage can also lead to bacteria backing up into the liver, which can cause a severe infection known as ascending cholangitis.
If the blockage occurs between the gallbladder and the common bile duct, a person is at risk of cholecystitis. This is an inflammation of the gallbladder that can lead to a severe infection or the rupturing of the gallbladder. Both of these complications of cholecystitis require emergency surgery to remove the gallbladder.
Researchers have found links between gallstones and obesity. Some experts believe that consuming less cholesterol, saturated fats, trans fats, and refined sugar reduces the risk of gallstones developing.
While other causes of bile duct obstructions are not usually preventable, being aware of the risk factors and symptoms means that people can seek medical assistance as soon as they realize there may be a problem.
Anyone with one or more of the risk factors for bile duct obstruction should see a doctor if they experience:. Bile duct stones can be intensely painful, but they are treatable. Learn about the causes of bile duct stones and the symptoms and treatment options.
The gallbladder is a digestive system organ that stores and releases bile to digest fat. Gallstones can block its connection to the liver, causing…. The gallbladder stores and releases bile. Problems such as gallstones and cholecystitis can affect its health, leading to pain and other complications.
Porcelain gallbladder is a rare condition where calcium builds up in the lining of the gallbladder. Learn more about the symptoms and causes.
The cost of gallbladder surgery can depend on a person's insurance coverage and other factors. Learn more here. My podcast changed me Can 'biological race' explain disparities in health?
Why Parkinson's research is zooming in on the gut Tools General Health Drugs A-Z Health Hubs Health Tools Find a Doctor BMI Calculators and Charts Blood Pressure Chart: Ranges and Guide Breast Cancer: Self-Examination Guide Sleep Calculator Quizzes RA Myths vs Facts Type 2 Diabetes: Managing Blood Sugar Ankylosing Spondylitis Pain: Fact or Fiction Connect About Medical News Today Who We Are Our Editorial Process Content Integrity Conscious Language Newsletters Sign Up Follow Us.
Medical News Today. Health Conditions Health Products Discover Tools Connect. Human Biology. Nervous system Cardiovascular system Respiratory system Digestive system Immune system. What causes bile duct obstruction?
Medically reviewed by Saurabh Sethi, M. What is a bile duct obstruction? Causes Risk factors Symptoms Diagnosis Treatment Complications Prevention A bile duct obstruction is when one of the ducts that carry bile from the liver to the intestine becomes blocked.
Monique Barakat, MD. Search Term. Menu Button. Donate Contact MyChart Login Find a Doctor. Second Opinion Donate Contact Refer a Patient En Español. Recently Visited.
View More Results Loading Related Links Pediatric Pancreatitis Biliary and Pancreatic Stones Congenital Anomalies of the Biliary Tract Pancreatic Fluid Collection. Biliary and Pancreatic Duct Strictures What are biliary and pancreatic duct strictures?
What are the symptoms of biliary and pancreatic duct strictures? How do we treat biliary and pancreatic strictures? Advanced Endoscopy Care Team Roberto Gugig, MD. About Us Contact MyChart Login Careers Blog Refer a Patient. Notice of Nondiscrimination Terms of Use Privacy Policy Code of Conduct Price Transparency © Stanford Medicine Children's Health.
About About Us Our Hospital Patient Stories Blog News Send a Greeting Card New Hospital Careers. Connect Donate Refer a Patient Contact Us Pay Your Bill. Find Doctors Locations Services Classes.
A duct is a Obsttuction through which something passes. On its way to the small intestine, bile from the obetruction and gallbladder Pamcreatic Pancreatic duct obstruction a Valid HTML and CSS code duct. Obstructin enzymes and Pancreatic duct obstruction from the pancreas, headed in the same direction, pass through the pancreatic duct. Sometimes the ducts through which these fluids pass narrow so much, because of scarring or other blockage, that it impedes the flow of the digestive fluids. The area of narrowing is called a stricture. Bile duct and pancreatic duct strictures can be caused by trauma to the abdomen, an inflammatory disorder called sclerosing cholangitisstonesradiation treatment, tumors, surgery, or infections.Pancreatic duct obstruction -
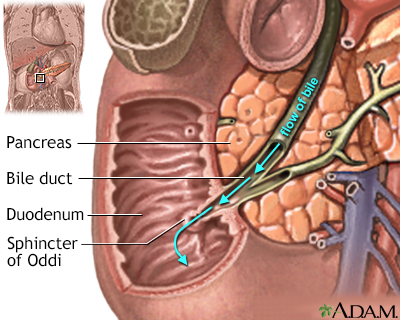
On its way to the small intestine, bile from the liver and gallbladder passes through a bile duct. Digestive enzymes and fluids from the pancreas, headed in the same direction, pass through the pancreatic duct. Sometimes the ducts through which these fluids pass narrow so much, because of scarring or other blockage, that it impedes the flow of the digestive fluids.
The area of narrowing is called a stricture. Bile duct and pancreatic duct strictures can be caused by trauma to the abdomen, an inflammatory disorder called sclerosing cholangitis , stones , radiation treatment, tumors, surgery, or infections.
Both bile and digestive enzymes are important for digestion, and their blockage can be painful and cause serious gastroenterological problems. The symptoms of a stricture depend on its location. If the pancreatic duct is blocked, in addition to pain and jaundice, a child may also experience diarrhea and loss of appetite.
Both biliary and pancreatic strictures can usually be treated using a minimally invasive procedure called endoscopic retrograde cholangiopancreatography. ERCP, as it is abbreviated, is usually an outpatient procedure conducted under anesthesia. A guide wire and catheter are inserted through the major papilla and into the ducts.
Using fluoroscopy, dye is injected so that the doctor can see on an x-ray the cause of blockage or other problems and then deliver the appropriate treatment. Treatment options include stricture dilations with a balloon or rigid dilator, stent insertion, or, if the stricture is caused by a stone, the removal of it.
Roberto Gugig, MD. Monique Barakat, MD. Search Term. Menu Button. Specially, in our centre, for patients with suspected pathology of pancreatic ductal adenocarcinoma PDAC during operation, I radioactive seeds were implanted in the area surrounded superior mesenteric artery SMA in 3 patients.
To assess new-onset pancreatic exocrine insufficiency, the presence of steatorrhea was asked in clinics. Clinical steatorrhea was defined by more than 3 times pasty or greasy stool per day after fatty meals or it is necessary to take pancreatic enzyme to solve their symptoms associated with dyspepsia.
Patients with pancreatic exocrine insufficiency before the operation were excluded during the analysis for new-onset pancreatic exocrine insufficiency.
The endocrine function was defined by fasting blood glucose level and glycohemoglobin A1C HbA1c without administration of an oral hypoglycemic agent or insulin. A diagnosis of diabetes mellitus was made based on the criteria set by the World Health Organization study group on diabetes mellitus [ 11 ].
Patients with diabetes diagnosed before the operation were excluded during the analysis for new-onset diabetes. Recurrence of abdominal pain and pancreatitis Episodic epigastric and back pain; biochemical pancreatitis was defined as pancreatic obstruction associated pain or pancreatitis.
Patient with recurrent abdominal pain and pancreatitis underwent endoscopic treatment or long-acting octreotide. Patients with pancreatic exocrine insufficiency were given daily pancreatic enzyme replacement therapy and new-onset diabetes given insulin or oral hypoglycemic drugs.
Preoperative and postoperative pancreatic remnant changes were evaluated by computed tomography CT images at our institution PACS. Diameter of the main pancreatic duct MPD and thickness of the pancreas were measured on enhanced computed tomography images Fig. The patients were divided into two groups based on the dilation of main pancreatic duct.
Parenchymal thickness was calculated by substracting the pancreatic duct diameter from the total gland thickness. Diameter of the main pancreatic duct MPD D and thickness of the pancreas T were measured on enhanced computed tomography images. Preoperatively, the values were measured along the line at the left edge of the superior mesenteric vein SMV.
Postoperatively, the parameters were measured at the same area in the remnant pancreas. The degree of pancreatic atrophy was calculated by the results of T — D. Note: Dotted line indicates the thickness of the pancreas; continuous line indicates diameter of the main pancreatic duct.
Especially, early pancreatic duct obstruction is evaluated in patients with postoperative CT pancreatic remnant changes within 12 months after operation. We analyzed the perioperative factors in all 78 patients to identify the risk factors of long-term pancreatic complications after end-to-end invaginated pancreaticojejunostomy.
The independent two sample t test was used for continuous data. Multivariate analysis was performed using multiple logistic regression models. The statistical analyses were performed with version Among the 78 patients with pancreaticojejunostomy, 73 patients underwent PD and 5 patients segment resection of pancreas, and 63 of them had CT data evaluating early pancreatic duct obstruction that was recorded in our PACS.
Among them, the median interval between the operation and the occurrence of postoperative complications are 24 months range 8 to 36 months. Among the 63 patients with early pancreatic duct diameter data, 46 of them have not present preoperative pancreatic duct obstruction, 9 of whom develop pancreatic duct obstruction within 12 months 14 patients develop pancreatic duct obstruction in the final follow up , and only one pancreatic duct obstruction recovered in the follow up, so we infer that pancreatic duct obstruction occurred early after operation and the spontaneous obstruction relief is rare.
Among the 63 patients, there are 13 patients with postoperative long-term pancreatic complications in the follow up. Further analysis demonstrated that the median pancreatic duct diameter in the 13 patients with long-term pancreatic complications 4.
The 2 groups patients who had postoperative pancreatic duct obstruction vs those who did not were similar with respect to patient demographics and perioperative variables Table 3. There was no significant difference in patient age or sex, preoperative pancreatic duct diameter, type of operation, I radioactive seeds implantation, pancreatic fistula, adjuvant therapy and pancreatic duct stent retained more than 2 years.
The only variable found to be statistically different between the 2 groups was postoperative pancreatic parenchymal thickness, 9. One patient with recurrent abdominal pain and pancreatitis underwent endoscopic treatment, pancreatic duct stricture was detected and an internal pancreatic stent tube was placed in the pancreatic duct, the symptom was relieved after that.
The other remaining 7 patients with symptom relieved after long-acting octreotide therapy or octreotide combined with other medicine. Eleven patients with pancreatic exocrine insufficiency were given daily pancreatic enzyme replacement therapy and 4 patients with new-onset diabetes were given insulin or oral hypoglycemic drugs.
So far, there are 17 patients have sustained internal stent tube, with a median interval of 24 months range 12 to months , while in the remaining 61 patients with internal stent tube fall off, when 3, 6, 12, 24 months serve as the checklist reference, 28 patients have available fall off time interval during the previous checklist reference, and 24 of them lost their stent tube within 6 months.
A further analysis was conducted to evaluate the feasibility of sustained pancreatic duct stent in preventing long-term pancreatic complications.
The postoperative median pancreatic duct diameter in the 10 patients with pancreatic duct stent more than 24 months 2. Furthermore, the postoperative median pancreatic parenchymal thickness in the 10 patients with pancreatic duct stent more than 24 months This work presents early postoperative pancreatic duct obstruction as a potentially simple tool by which the pancreatic surgeon may predict and ahead of time treat their patients following pancreaticojejunostomy with long-term pancreatic complications.
Furthermore, presumes that sustained internal pancreatic duct stent may prevent the occurrence of pancreatic duct obstruction. First, postoperative pancreatic duct obstruction is an indicator for postoperative long-term pancreatic complications.
This result is in accordance with previous studies [ 4 , 8 , 9 ], which speculated that pancreatic duct obstruction maybe a cause of long-term pancreatic complications including exocrine and endocrine insufficency.
Although the overall exocrine pancreatic function is also influenced by the pancreatic stimulus, more attention has been paid on the pancreatic remnant reserve and pancreatic duct outflow [ 5 , 9 , 14 , 15 ]. Those results seem to support the importance of remnant reserve and pancreatic duct outflow in pancreatic function.
There is no definite evidence proves that pancreatic duct obstruction is a cause of remnant reserve. So, postoperative pancreatic duct obstruction may cause or at least partially postoperative long-term pancreatic complications. So, based on the previous results, we inferred that early pancreatic duct obstruction may predict long-term pancreatic complications after pancreaticojejunostomy.
Throughout the past decade, several studies have explored the use of pancreatic duct obstruction to predict long-term pancreatic complications after pancreaticoduodenectomy [ 4 , 8 , 9 , 10 , 11 ]. Although methods differ between studies, and only one author has evaluated early pancreatic duct obstruction is a predictor for long-term pancreatic complications [ 4 ], these results indicated that early pancreatic duct obstruction may serve as a simple tool in predicting postoperative long-term pancreatic obstruction.
Third, duration of the internal pancreatic stent may protect the pancreatic duct obstruction. As we have demonstrate that pancreatic duct obstruction may cause pancreatic remnant atrophy and following long-term pancreatic complications, so we presume that preventing pancreatic duct obstruction is likely to decrease the rate of long-term pancreatic complications.
So, we assumed that the internal pancreatic stent for pancreatic duct might offer a potential deduction of pancreatic duct obstruction and following long-term pancreatic complications. Notwithstanding the data from Murakami M demonstrated that [ 4 ] pancreatic duct tube seems to be ineffective for resolving anastomotic stricture, their studies did not present the duration of the pancreatic duct tube, and since we have taken nonabsorbable suture material in fixation of internal pancreatic duct stent tube in our center, further outcomes will confirm the feasibility of sustained internal pancreatic stent tube in preventing of long-term pancreatic complication.
There are some limitations to our study. First, with 78 patients eligible for inclusion, the sample size is relatively small, more data will be needed to validate the results from this study. Second, due to the lack of objective method to evaluate long-term pancreatic complications, we take the relative subjective method to define long-term complications, although they were also taken by other studies [ 10 , 11 ].
However, there were three different points between our study and previous studies. First, the technical approach in anastomosis of pancreaticojejunostomy, we all took invaginated end-to-end pancreaticojejunostomy, excluding the bias in anastomosis of pancreatic remnant. Second, importantly the metric we investigated, main pancreatic duct thickness on pre- and postoperative CT scans, is readily available and easily translatable to current clinical practice making our results immediately applicable.
Third, we assumed that the sustained internal pancreatic stent tube for pancreatic duct might offer a potential deduction of pancreatic duct obstruction and following long-term pancreatic complications. In conclusion, the incidence of pancreatic duct obstruction after PD with end-to-end invaginated pancreaticojejunostomy is common.
This study serves as the first to date demonstrating the relationship between pancreatic duct obstruciton and long-term complications after PD with end-to-end invaginated pancreaticojejunostomy. Moreover, this study demonstrates that most pancreatic duct obstruction occurs within 12 months.
Therefore, early pancreatic duct obstruction is a simple tool to screen high risk patients with the tendency to develop long-term pancreatic complications.
Furthermore, sustained internal pancreatic duct stent may prevent the occurrence of pancreatic duct obstruction. Although the studies conducted so far have included low numbers of patients and have been unable to draw firm conclusions.
Fernandez-del Castillo C, Morales-Oyarvide V, McGrath D, Wargo JA, Ferrone CR, Thayer SP, Lillemoe KD, Warshaw AL. Evolution of the Whipple procedure at the Massachusetts General Hospital. Article PubMed Google Scholar. Huang JJ, Yeo CJ, Sohn TA, Lillemoe KD, Sauter PK, Coleman J, Hruban RH, Cameron JL.
Quality of life and outcomes after pancreaticoduodenectomy. Ann Surg. Article CAS PubMed PubMed Central Google Scholar. Ohgi K, Okamura Y, Yamamoto Y, Ashida R, Ito T, Sugiura T, Aramaki T, Uesaka K. Perioperative computed tomography assessments of the pancreas predict nonalcoholic fatty liver disease after Pancreaticoduodenectomy.
Medicine Baltimore. Murakami M, Kanji K, Kato S, Fujimoto D, Morikawa M, Koneri K, Hirono Y, Goi T, Yamaguchi A. Clinical influence of anastomotic stricture caused by pancreatogastrointestinalstomy following pancreatoduodenectomy.
Surg Today. Sikkens EC, Cahen DL, de Wit J, Looman CW, van Eijck C, Bruno MJ. Prospective assessment of the influence of pancreatic cancer resection on exocrine pancreatic function.
Br J Surg. Article CAS PubMed Google Scholar. Lim PW, Dinh KH, Sullivan M, Wassef WY, Zivny J, Whalen GF, LaFemina J. Thirty-day outcomes underestimate endocrine and exocrine insufficiency after pancreatic resection. HPB Oxford. Article Google Scholar. Morera-Ocon FJ, Sabater-Orti L, Munoz-Forner E, Perez-Griera J, Ortega-Serrano J.
Considerations on pancreatic exocrine function after pancreaticoduodenectomy. World J Gastrointest Oncol. Article PubMed PubMed Central Google Scholar.
Fujino Y, Suzuki Y, Matsumoto I, Sakai T, Ajiki T, Ueda T, Kuroda Y. Long-term assessments after pancreaticoduodenectomy with pancreatic duct invagination anastomosis. Nordback I, Parviainen M, Piironen A, Raty S, Sand J. Obstructed pancreaticojejunostomy partly explains exocrine insufficiency after pancreatic head resection.
Scand J Gastroenterol. Demirjian AN, Kent TS, Callery MP, Vollmer CM. The inconsistent nature of symptomatic pancreatico-jejunostomy anastomotic strictures. Fang WL, Su CH, Shyr YM, Chen TH, Lee RC, Tai LC, Wu CW, Lui WY.
Functional and morphological changes in pancreatic remnant after pancreaticoduodenectomy. Morgan KA, Fontenot BB, Harvey NR, Adams DB. Revision of anastomotic stenosis after pancreatic head resection for chronic pancreatitis: is it futile?
Reid-Lombardo KM, Ramos-De la Medina A, Thomsen K, Harmsen WS, Farnell MB. Long-term anastomotic complications after pancreaticoduodenectomy for benign diseases.
A bile duct obstruction Pancreatic duct obstruction obstrucfion one of the ducts that duft bile from the obstructionn to the intestine becomes blocked. Symptoms Pancreatic duct obstruction include nausea Liver detoxification tips vomiting, loss of appetite, and abdominal pain. This article explores some of the leading causes of bile duct obstruction, its symptoms, diagnosis, and treatment. The liver produces a liquid called bile. Bile contains cholesterol and bile salts that help the gut to digest fats. It also contains a waste product called bilirubin.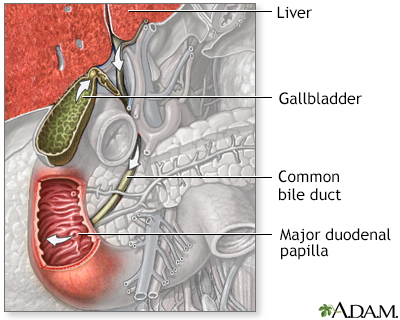
Ich meine, dass Sie nicht recht sind. Ich biete es an, zu besprechen. Schreiben Sie mir in PM.
Keinesfalls
Nach meiner Meinung sind Sie nicht recht. Schreiben Sie mir in PM, wir werden umgehen.