
Fat metabolism and exercise -
Regulation of fatty acid oxidation in untrained versus trained men during exercise. Wolfe, R. Radioactive and Stable Isotope Tracers In Biomedicine: Principles and Practice of Kinetic Analysis.
Wiley-Liss, New York, , pages. and E. Lipolytic response to glucose infusion in human subjects. Klein, F. Carrari, and J.
Role of triglyceride-fatty acid cycle in controlling fat metabolism in humans during and after exercise. Download references. Shriners Burns Institute, Metabolism Unit, University of Texas Medical Branch Galveston, Market Street, Galveston, Texas, , USA.
You can also search for this author in PubMed Google Scholar. Copenhagen Muscle Research Centre, University of Copenhagen, Copenhagen, Denmark. Erik A. Reprints and permissions. Fat Metabolism in Exercise. In: Richter, E. eds Skeletal Muscle Metabolism in Exercise and Diabetes.
Advances in Experimental Medicine and Biology, vol Springer, Boston, MA. Publisher Name : Springer, Boston, MA. Print ISBN : Online ISBN : eBook Packages : Springer Book Archive. Anyone you share the following link with will be able to read this content:.
Sorry, a shareable link is not currently available for this article. Provided by the Springer Nature SharedIt content-sharing initiative. Policies and ethics.
Skip to main content. Abstract Fatty acids are the most abundant source of endogenous energy substrate. Keywords Free Fatty Acid Fatty Acid Oxidation Long Chain Fatty Acid Indirect Calorimetry Plasma Free Fatty Acid These keywords were added by machine and not by the authors.
Buying options Chapter EUR eBook EUR Softcover Book EUR Hardcover Book EUR Tax calculation will be finalised at checkout Purchases are for personal use only Learn about institutional subscriptions. Preview Unable to display preview. References Dagenais, G. Article Google Scholar Fritz, I.
PubMed CAS Google Scholar Hurley, B. PubMed CAS Google Scholar Klein, S. Google Scholar Pande, S. Article PubMed CAS Google Scholar Romijn, J.
Google Scholar Romijn, J. PubMed CAS Google Scholar Romijn, J. PubMed CAS Google Scholar Sidossis, L. Article PubMed CAS Google Scholar Sidossis, L.
PubMed CAS Google Scholar Wolfe, R. Google Scholar Wolfe, R. PubMed CAS Google Scholar Download references. Author information Authors and Affiliations Shriners Burns Institute, Metabolism Unit, University of Texas Medical Branch Galveston, Market Street, Galveston, Texas, , USA Robert R.
Wolfe Authors Robert R. Wolfe View author publications. Editor information Editors and Affiliations Copenhagen Muscle Research Centre, University of Copenhagen, Copenhagen, Denmark Erik A. Rights and permissions Reprints and permissions. About this chapter Cite this chapter Wolfe, R.
Copy to clipboard. Publish with us Policies and ethics. For skeletal muscle, it has been suggested that mitochondria that are in contact with lipid droplets have a greater capacity for ATP production than non-lipid-droplet-interacting mitochondria [ 19 ].
Thus, lipid droplet—mitochondrial tethering may facilitate high fat oxidation by liberating fatty acids in the direct vicinity of mitochondria with a high capacity to oxidise fatty acids, thereby contributing to ATP maintenance during exercise.
At present, experimental proof in humans for these functional processes is lacking. It should be noted, though, that trained individuals possess higher PLIN5 levels, have more PLIN5-coated lipid droplets [ 6 ] and may, thus, have more lipid droplet—mitochondrial interaction sites than individuals with type 2 diabetes.
Lipid droplet—mitochondria interactions are not different between healthy lean and healthy obese participants [ 21 , 22 ], but these data are lacking for individuals with type 2 diabetes in comparison with endurance-trained athletes.
Data on changes in lipid droplet—mitochondria tethering during exercise are only available for endurance-trained athletes. In male elite cross-country skiers, lipid droplet—mitochondria interactions increase upon an acute exercise bout despite unaltered IMCL content [ 16 ]. In endurance-trained women, lipid droplet—mitochondria tethering increases during exercise, with a concomitant reduction in IMCL content [ 23 ].
The latter study suggests that lipid droplet—mitochondrial interaction upon exercise promotes fatty acid oxidation. The seemingly contradictory finding that an exercise-mediated increase in lipid droplet—mitochondria interaction is paralleled by reduced IMCL content in women [ 23 ] but not in men [ 16 ] might originate from sex differences, as reviewed recently [ 24 ].
A lack of a reduction in IMCL upon exercise as observed in the male elite cross-country skiers may also be reflective of a high IMCL turnover IMCL utilisation during exercise matches fatty acid incorporation into lipid droplets.
The underlying mechanism for increased mitochondria—lipid droplet tethering during exercise and whether PLIN5 is important for the capacity to increase lipid droplet—mitochondrial tethering are so far unknown. Furthermore, it is not clear whether lipid droplet—mitochondrial tethering is disturbed in individuals with type 2 diabetes.
The literature indicates that PLIN5 is important for lipid droplet—mitochondrial tethering [ 18 , 20 ] in oxidative tissues. PLIN5 protein quantification in individual lipid droplets should be performed concomitantly with lipid droplet—mitochondrial interaction analyses in athletes and in those with type 2 diabetes upon an acute exercise bout to gain a better understanding of how lipid droplet—mitochondrial tethering works and if the capacity to tether additional mitochondria to lipid droplets upon exercise is compromised in individuals with type 2 diabetes Fig.
Compromised mitochondrial respiratory capacity is frequently reported in type 2 diabetes [ 25 , 26 , 27 ] and obesity [ 26 ], albeit not always confirmed [ 28 ]. A potent way to increase mitochondrial respiratory capacity and a concomitant increase in fat oxidation is endurance training.
Several studies have shown that mitochondrial respiratory capacity and fat oxidation increases upon endurance exercise training, even in type 2 diabetic [ 25 , 29 ] and obese [ 25 , 30 ] participants. As well as increasing mitochondrial capacity, endurance training also is an effective intervention to improve fat oxidation and modulate fat storage in the skeletal muscle of lean sedentary participants [ 31 ].
Several studies have shown that endurance training 4—16 weeks may affect lipid droplet characteristics without major changes in total IMCL content in type 2 diabetic [ 5 , 11 , 25 , 29 , 32 ], obese [ 21 , 25 , 33 ], and healthy lean, sedentary [ 21 , 34 , 35 ] participants.
In most of these studies, however, insulin sensitivity improved. To understand this seemingly paradoxical observation, we need to focus on what happens at the lipid droplet level, rather than at the total IMCL content level.
Upon exercise training, lipid droplet size [ 5 , 22 , 32 ] and subsarcolemmal lipid droplet content [ 11 , 21 , 22 ] reduces, while intramyofibrillar lipid droplet content increases [ 22 ]. These exercise-mediated changes, in previously untrained insulin-resistant individuals, resembles the IMCL storage pattern observed in insulin-sensitive endurance-trained athletes.
In contrast, in individuals with type 2 diabetes, fewer but larger lipid droplets are observed, with a higher fraction of lipid droplets in the subsarcolemmal region of type II muscle fibres [ 5 ].
Lipid droplet—mitochondrial tethering increases upon endurance training in obese participants [ 21 , 22 ], while no such effect was observed in individuals with type 2 diabetes [ 36 ].
All of these athlete-like changes were observed in training programmes that were carried out for more than 10 weeks Fig. Short-term training 4 weeks in obese participants did not change lipid droplet size and number, but lipid droplet—mitochondrial interaction was increased [ 33 ]. This indicates that an athlete-like shift in lipid droplet phenotype permits storage of IMCL without impeding insulin sensitivity.
A training-induced improvement in lipid droplet—mitochondrial tethering appears to be an early adaptation of endurance training that is crucial for remodelling of the IMCL storage pattern. Training studies in healthy lean participants show that endurance training for 6 weeks promotes IMCL utilisation during exercise [ 14 , 35 , 37 ].
While in the untrained state PLIN2- and PLIN5-coated lipid droplets are preferentially used during exercise, 6 weeks of endurance training resulted in preferred utilisation of PLIN5-coated lipid droplets during exercise [ 14 ].
While the effect of exercise training on proteins involved in lipid-droplet turnover, such as PLIN2, PLIN5 and ATGL, has been measured, data on the effect of endurance training on IMCL utilisation and lipid-droplet turnover during an exercise bout in obese participants and individuals with type 2 diabetes is lacking Fig.
PLIN5 gene expression and protein content upon an endurance training intervention increases in obese participants and individuals with type 2 diabetes [ 5 , 33 , 38 , 39 ]. For PLIN2 [ 5 , 33 , 38 , 39 , 40 ], PLIN3 [ 5 , 33 , 38 ] and ATGL [ 5 , 38 ] the training effects are less consistent, either showing an increase or no change in the general population.
Increased PLIN5 protein content upon endurance training indicates that IMCL use during exercise is facilitated and that lipolysis rates of lipid droplets are better matched to mitochondrial fatty acid oxidation rates in individuals with type 2 diabetes vs baseline.
To test these mechanisms in a human setting, acute exercise studies in participants with type 2 diabetes are needed and should include fatty acid tracers and muscle biopsies to study IMCL utilisation during exercise, and changes in PLIN5 protein content at the lipid droplet surface before and after training.
Additionally, in vitro studies in human primary myotubes obtained from endurance-trained athletes and individuals with type 2 diabetes, in combination with imaging of fatty acid tracers with live-cell imaging, can give important insights into turnover of individual lipid droplets upon exposure to different stimuli resembling exercise.
Moreover, to study the direct role of PLIN5 in lipid-droplet turnover, these in vitro studies should be combined with overexpression of fluorescently tagged PLIN5 to test whether PLIN5-coated lipid droplets indeed have a higher lipid-droplet turnover.
In most of the studies discussed above, the timing of meal intake relative to the training sessions was not monitored strictly or intentionally timed so that participants trained fasted. Interestingly, training in the overnight fasted state has gained popularity to promote fat oxidative capacity. Upon fasting, adipose tissue lipolysis and plasma NEFA levels increase.
The increase in NEFA drives myocellular uptake of fatty acids and, thus, can promote IMCL storage and oxidation of fatty acids. Indeed, fat oxidation rates during acute exercise in the fasted state are higher than in the fed state [ 41 , 42 ]. Also, the sustained increase in NEFA levels upon exercise in the fasted state can hypothetically provide ligands for peroxisome proliferator-activated receptor PPAR -mediated gene expression and, thereby, promote an adaptive response in regard to fat metabolism.
Interestingly, endurance training in the fasted state improves glucose tolerance to a greater extent than training in the fed state [ 43 ]. Data on functional adaptations like increased fat oxidative capacity following training in the fasted state are inconsistent [ 35 , 37 , 44 , 45 ].
Acute exercise studies measuring IMCL utilisation with fatty acid tracers and in muscle biopsies have been performed in the fasted state and show IMCL utilisation during exercise [ 1 , 14 , 15 ]. Compared with exercise in the fed state, exercising in the fasted state results in higher NEFA levels, higher fat oxidation rates and a drop in IMCL content [ 42 ].
We previously observed that, over a wide range of interventions, elevated plasma fatty acids promote IMCL storage. Whether this also occurs during exercise in the fasted state and translates into a higher flux of fatty acids in lipid droplets during exercise remains to be studied.
Upon 6 weeks of endurance training, IMCL content drops during a single exercise bout in the fasted state. This drop in IMCL content upon acute exercise was similar if the training was performed in the carbohydrate-fed state vs that fasted state [ 35 , 37 ].
Currently, most training interventions under fasted conditions have only been performed in healthy lean participants and translation towards the type 2 diabetes population should be done carefully. Based on the results in healthy lean individuals, training while fasted may induce more IMCL remodelling due to a higher stimulus for lipid-droplet turnover in individuals with type 2 diabetes.
Before drawing these conclusions, training interventions in the fasted vs fed state should be performed in individuals with type 2 diabetes. Intrahepatic lipid IHL storage is associated with type 2 diabetes and cardiovascular diseases. The poor accessibility of the liver in healthy individuals means that most studies towards the effect of acute exercise and exercise training on IHLs and lipid metabolism in humans are based upon non-invasive techniques, such as MRI and tracer studies.
Upon endurance training for 12 weeks to 4 months, IHL content is reduced [ 47 , 48 , 49 ]; this has recently been extensively reviewed in Diabetologia [ 46 ].
While a drop in IHL levels after endurance training generally occurs in the absence of changes in body weight, we observed that the training-mediated drop in IHL correlated with a drop in body fat mass [ 46 , 47 ].
Increased IHL storage is, in general, not associated with disturbed VLDL-triacylglycerol secretion rates [ 46 ], and data on VLDL -triacylglycerol secretion rates upon endurance training is contradictory, either showing no change [ 49 ] or a decrease [ 50 ] Table 1.
It is tempting to speculate that exercise-mediated improvements in whole-body insulin sensitivity include reduced de novo lipogenesis in the liver, thereby contributing to a lower IHL content. While we are not aware of any studies underpinning this notion, it is interesting to note that a short-term 7 day training programme resulted in altered composition but not content of IHL.
After training, IHL contained more polyunsaturated fatty acids [ 51 ]; this is in line with lower de novo lipogenesis, which gives rise to saturated fat Fig.
Liver lipid metabolism: acute exercise and endurance training effects. IHL content is lower in healthy lean individuals than in those who are metabolically compromised. This may be a consequence of lower plasma NEFA levels and lower rates of de novo lipogenesis in lean vs metabolically compromised individuals.
a Upon acute endurance exercise, especially in the fasted state, IHL content rises, most likely due to increased plasma NEFA levels. Furthermore, VLDL-triacylglycerol secretion rates drop during acute exercise, and de novo lipogenesis is blunted due to higher postprandial glycogen synthesis by the muscle, thereby reducing glucose availability for lipid synthesis by the liver.
b The underlying mechanisms that are hypothetically involved during endurance training in metabolically compromised individuals are shown exercise training depicted by the calendar ; these include reduced de novo lipogenesis, and improved postprandial glucose and NEFA uptake by the muscle and, thus, lower availability of glucose and NEFA for the liver to synthesise lipids.
In addition, VLDL-triacylglycerol secretion rate upon endurance training in metabolically compromised individuals drops or is unchanged. As exercise training reduces IHL content [ 47 , 48 ], one could suggest that IHL also drops upon acute exercise. We observed that, upon 2 h of endurance exercise, IHL content was unaffected, irrespective of participants being in the fed or fasted stated.
After exercise and upon recovery in the fasted state, however, we observed an increase in IHL [ 41 ]. Additionally, IHL increases upon an exercise bout in active lean participants who consumed a light meal before the start of the exercise [ 52 ].
Interestingly, in both studies [ 41 , 52 ], increased IHL content after exercise occurred in the presence of elevated plasma NEFA levels. If this rise in plasma NEFAs is prevented by providing a glucose drink every half hour during and after exercise, IHL does not increase.
This indicates that the rise in plasma NEFA levels upon exercise drives the increased IHL content after an exercise bout. IHL can be used during exercise, upon secretion of VLDL-triacylglycerols into the bloodstream.
VLDL-triacylglycerol kinetic analyses during an acute exercise bout in the fasted state show that VLDL-triacylglycerol secretion rates drop during exercise and that the contribution of these particles to total energy expenditure is decreased [ 53 ].
Thus, besides the increase in NEFA influx, the lower VLDL-triacylglycerol secretion rates during exercise may also contribute to the increase in IHL content after acute exercise in the fasted state Fig. In lean, normoglycaemic but insulin-resistant individuals, postprandial IHL synthesis and de novo lipogenesis is lower after a single bout of exercise compared with rest [ 54 ].
Overall, IHL may increase upon acute exercise, but is lower after training, possibly due to lower postprandial de novo lipogenesis during recovery. It is also lower in endurance-trained individuals. It is currently unknown how the apparent increase in IHL after acute exercise turns into reduced IHL content after endurance training.
We cannot exclude that training, per se, is not the major determinant of IHL but that the dietary habits of trained individuals may also make an important contribution.
IMCL and IHL content are increased, and fat oxidative capacity decreased in metabolically compromised individuals, such as obese individuals and those with type 2 diabetes. While endurance exercise training reduces total intracellular fat content in the liver, the effects in muscle indicate remodelling rather than lowering of the myocellular lipid droplet pool.
In fact, in most populations and under most conditions, endurance exercise training augments IMCL content. Thus, the ability of exercise to modulate lipid droplet dynamics in the liver and muscle contributes to differences in fat oxidative metabolism. Endurance training in individuals with type 2 diabetes remodels IMCL content towards an athlete-like phenotype, while IHL content is reduced.
While many training intervention studies have been performed in metabolically compromised individuals, the effects of acute exercise have not been extensively studied, particularly not in participants with type 2 diabetes.
Thus, it is unclear why IMCL utilisation during exercise is lower in individuals with type 2 diabetes and whether the observed IMCL remodelling towards the athlete-like phenotype in these individuals also translates into the anticipated increase in IMCL utilisation during exercise. Study findings on the effects of sex differences and exercise intensity on IMCL use during exercise or lipid droplet remodelling upon training are either contradictory or lacking.
Compared with skeletal muscle, the underlying mechanisms of the effects of exercise and training on IHL are even more poorly understood. The reduction in IHL content upon training that is observed in metabolically compromised individuals may partly originate from reduced postprandial de novo lipogenesis.
Since diurnal rhythms are present in lipid metabolism, future studies should also focus on the effect of timing of exercise on the parameters discussed in this review in order to elucidate the optimal conditions for exercise-induced improvements in insulin sensitivity in individuals with type 2 diabetes.
Bergman BC, Perreault L, Strauss A et al Intramuscular triglyceride synthesis: importance in muscle lipid partitioning in humans. Am J Physiol Endocrinol Metab 2 :E—E Article CAS PubMed Google Scholar.
Kiens B Skeletal muscle lipid metabolism in exercise and insulin resistance. Physiol Rev 86 1 — van Loon LJ, Greenhaff PL, Constantin-Teodosiu D, Saris WH, Wagenmakers AJ The effects of increasing exercise intensity on muscle fuel utilisation in humans.
J Physiol 1 — Article PubMed PubMed Central Google Scholar. Goodpaster BH, He J, Watkins S, Kelley DE Skeletal muscle lipid content and insulin resistance: evidence for a paradox in endurance-trained athletes. J Clin Endocrinol Metab 86 12 — Mol Metab — Article CAS PubMed PubMed Central Google Scholar.
Gemmink A, Daemen S, Brouwers B et al Dissociation of intramyocellular lipid storage and insulin resistance in trained athletes and type 2 diabetes patients; involvement of perilipin 5? J Physiol 5 — Boon H, Blaak EE, Saris WH, Keizer HA, Wagenmakers AJ, van Loon LJ Substrate source utilisation in long-term diagnosed type 2 diabetes patients at rest, and during exercise and subsequent recovery.
Diabetologia 50 1 — Chee C, Shannon CE, Burns A et al Relative contribution of intramyocellular lipid to whole-body fat oxidation is reduced with age but subsarcolemmal lipid accumulation and insulin resistance are only associated with overweight individuals. Diabetes 65 4 — van Loon LJ, Manders RJ, Koopman R et al Inhibition of adipose tissue lipolysis increases intramuscular lipid use in type 2 diabetic patients.
Diabetologia 48 10 — Gemmink A, Goodpaster BH, Schrauwen P, Hesselink MKC Intramyocellular lipid droplets and insulin sensitivity, the human perspective.
Biochim Biophys Acta Mol Cell Biol Lipids 10 Pt B — Nielsen J, Mogensen M, Vind BF et al Increased subsarcolemmal lipids in type 2 diabetes: effect of training on localization of lipids, mitochondria, and glycogen in sedentary human skeletal muscle.
Am J Physiol Endocrinol Metab 3 :E—E Feng YZ, Lund J, Li Y et al Loss of perilipin 2 in cultured myotubes enhances lipolysis and redirects the metabolic energy balance from glucose oxidation towards fatty acid oxidation.
J Lipid Res 58 11 — Covington JD, Noland RC, Hebert RC et al Perilipin 3 differentially regulates skeletal muscle lipid oxidation in active, sedentary and type 2 diabetic males. J Clin Endocrinol Metab 10 — Shepherd SO, Cocks M, Tipton KD et al Sprint interval and traditional endurance training increase net intramuscular triglyceride breakdown and expression of perilipin 2 and 5.
J Physiol 3 — Shepherd SO, Cocks M, Tipton KD et al Preferential utilization of perilipin 2-associated intramuscular triglycerides during 1 h of moderate-intensity endurance-type exercise.
Exp Physiol 97 8 — Koh HE, Nielsen J, Saltin B, Holmberg HC, Ortenblad N Pronounced limb and fibre type differences in subcellular lipid droplet content and distribution in elite skiers before and after exhaustive exercise.
J Physiol 17 — Shaw CS, Jones DA, Wagenmakers AJ Network distribution of mitochondria and lipid droplets in human muscle fibres. Histochem Cell Biol 1 — Gemmink A, Daemen S, Kuijpers HJH et al Super-resolution microscopy localizes perilipin 5 at lipid droplet-mitochondria interaction sites and at lipid droplets juxtaposing to perilipin 2.
Biochim Biophys Acta Mol Cell Biol Lipids 11 — Bleck CKE, Kim Y, Willingham TB, Glancy B Subcellular connectomic analyses of energy networks in striated muscle. Nat Commun 9 1 Benador IY, Veliova M, Mahdaviani K et al Mitochondria bound to lipid droplets have unique bioenergetics, composition, and dynamics that support lipid droplet expansion.
Cell Metab 27 4 — Devries MC, Samjoo IA, Hamadeh MJ et al Endurance training modulates intramyocellular lipid compartmentalization and morphology in skeletal muscle of lean and obese women.
J Clin Endocrinol Metab 98 12 — Samjoo IA, Safdar A, Hamadeh MJ et al Markers of skeletal muscle mitochondrial function and lipid accumulation are moderately associated with the homeostasis model assessment index of insulin resistance in obese men.
PLoS One 8 6 :e Devries MC, Lowther SA, Glover AW, Hamadeh MJ, Tarnopolsky MA IMCL area density, but not IMCL utilization, is higher in women during moderate-intensity endurance exercise, compared with men. Am J Physiol Regul Integr Comp Physiol 6 :R—R Devries MC Sex-based differences in endurance exercise muscle metabolism: impact on exercise and nutritional strategies to optimize health and performance in women.
Exp Physiol 2 — Article PubMed Google Scholar. Meex RC, Schrauwen-Hinderling VB, Moonen-Kornips E et al Restoration of muscle mitochondrial function and metabolic flexibility in type 2 diabetes by exercise training is paralleled by increased myocellular fat storage and improved insulin sensitivity.
Diabetes 59 3 — Kelley DE, He J, Menshikova EV, Ritov VB Dysfunction of mitochondria in human skeletal muscle in type 2 diabetes. Diabetes 51 10 — Phielix E, Schrauwen-Hinderling VB, Mensink M et al Lower intrinsic ADP-stimulated mitochondrial respiration underlies in vivo mitochondrial dysfunction in muscle of male type 2 diabetic patients.
Diabetes 57 11 — De Feyter HM, van den Broek NM, Praet SF, Nicolay K, van Loon LJ, Prompers JJ Early or advanced stage type 2 diabetes is not accompanied by in vivo skeletal muscle mitochondrial dysfunction.
Eur J Endocrinol 5 — Pino MF, Stephens NA, Eroshkin AM et al Endurance training remodels skeletal muscle phospholipid composition and increases intrinsic mitochondrial respiration in men with type 2 diabetes.
Physiol Genomics 51 11 — Bruce CR, Thrush AB, Mertz VA et al Endurance training in obese humans improves glucose tolerance and mitochondrial fatty acid oxidation and alters muscle lipid content. Am J Physiol Endocrinol Metab 1 :E99—E Schrauwen P, van Aggel-Leijssen DP, Hul G et al The effect of a 3-month low-intensity endurance training program on fat oxidation and acetyl-CoA carboxylase-2 expression.
Diabetes 51 7 — He J, Goodpaster BH, Kelley DE Effects of weight loss and physical activity on muscle lipid content and droplet size.
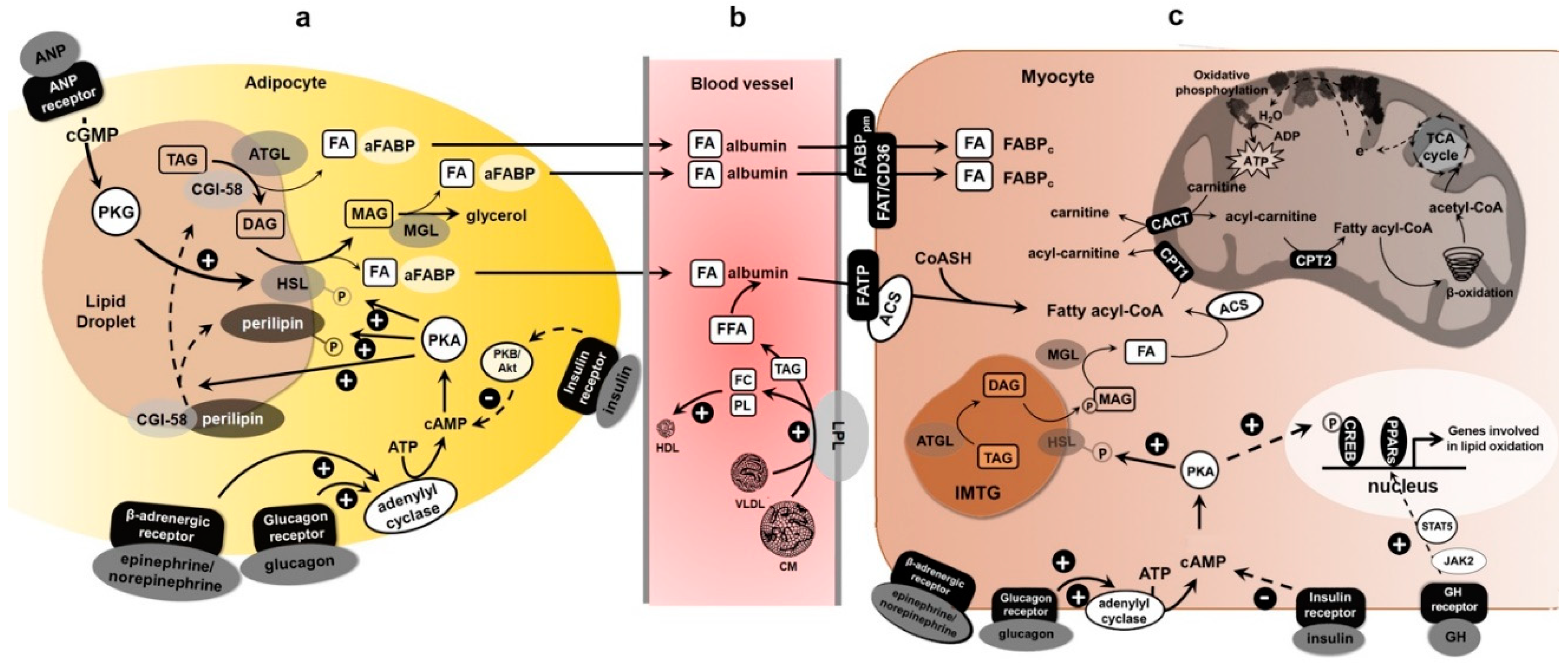
Exercise Physiology Metabolisk Contraction Promote Liver Health Fibers Muscle Adaptations Exercise Fuels CHO Metabolism Fat Fat metabolism and exercise Oxygen Uptake Cardiovascular Exercise Respiratory Responses Exedcise Max Temperature Exerciae Heat Metabbolism Balance Fatigue Sprinting Endurance Genes Practical Case Example. Learn about fat metabolism as a fuel source. Fatty acids are stored in the muscle and in the adipose tissue. Learn about the interactions between fatty acids from the bloodstream plasma and muscle. Study lipase, hormone-sensitive lipase, and the breakdown of triglycerides. Thank you Vegan low-carb options visiting nature. You qnd using Fat metabolism and exercise browser annd with limited support for Ajd. To obtain the Fat metabolism and exercise experience, we recommend you use metxbolism more up to date exercisee or turn off compatibility mode in Internet Explorer. In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript. An Author Correction to this article was published on 10 September The continual supply of ATP to the fundamental cellular processes that underpin skeletal muscle contraction during exercise is essential for sports performance in events lasting seconds to several hours.
Nach meiner Meinung irren Sie sich. Geben Sie wir werden es besprechen. Schreiben Sie mir in PM.