Bone health and smoking -
Smoking cessation and mental health. Smoking Cessation and Mental Health: A briefing for front-line staff. Smoking cessation and smokefree policies: Good practice for mental health services.
Smoking cessation and cannabis use. Stopping Smoking in Pregnancy: A briefing for maternity care providers. Stop smoking aids. Stop smoking aids resources. Stop smoking aids quick reference sheet. Vaping resources. Vaping: a guide for health and social care professionals.
Information for specialist stop-smoking services that are considering providing e-cigarette starter packs: recommendations from the Trial of Ecigarettes TEC.
Nicotine Replacement Therapy. Nicotine Gum. Unlicensed varenicline. Secondary care resources. How were these factsheets put together?
Interventions in Secondary Care - Orthopedic Patients Factsheet NHS Smokefree, Inpatient Tobacco Dependence Treatment Resources. Inpatient Tobacco Dependence Treatment: Best Practices and Key Messages. NHS Acute Inpatient Tobacco Dependence Advisor Training Resources.
NHS Mental Health Inpatient Tobacco Dependence Advisor Training Resources. Communicating with high-risk individuals about lung cancer screening. Communicating with high-risk individuals about lung cancer screening training module.
NHSE Competency frameworks for tobacco dependence treatment in secondary care. There was no difference in height, weight, or body mass index using an independent samples t test between these two cohorts, demonstrating that the GOOD cohort is representative of the general young male population of Gothenburg.
Baseline data of the whole GOOD cohort concerning bone parameters, anthropometrics, and smoking frequency have been published previously 1.
Height and weight were measured using standardized equipment. The CVs for the aBMD measurements ranged from 0. The CVs for total body lean mass and total body fat mass were 1.
A pQCT device, using single energy x-ray XCT; Stratec Medizintechnik, GmbH, Pforzheim, Germany was used to scan the distal leg tibia and the distal arm radius of the nondominant leg and arm, respectively. The pQCT was calibrated every week using a standard phantom and once every 30 d using a cone phantom provided by the manufacturer.
A 2-mm-thick single tomographic slice was scanned with a voxel size of 0. The cortical vBMD is the true cortical volumetric BMD, not including the marrow compartment. All the pQCT analyses were performed by one technician using one pQCT.
Analyses of serum levels of total estradiol, testosterone, and SHBG were performed as previously described Free testosterone and free estradiol were calculated according to the method previously described by Vermulen et al.
Serum levels of OH-vitamin D were measured by a competitive RIA DiaSorin, Stillwater, MN. This assay measures both OH-vitamin D3 and OH-vitamin D2. Serum levels of intact PTH were measured by an immunoluminometric assay Diagnostic Products Corp.
Values are given as mean ± sd unless otherwise indicated. All calculations were performed with the SPSS Statistical Software version Differences between smokers and nonsmokers were calculated using independent samples t test.
The independent predictors of the various bone parameters were tested using multiple linear regression analysis, including height, weight, age, calcium intake, smoking, and physical activity.
Smokers were coded as 1 and nonsmokers as 0. Standardized β-values were used. Bone parameters Figs. Lower aBMD of the total body A , lumbar spine B , femoral neck C , and the trochanter D in smokers than in nonsmokers.
Values are adjusted for calcium intake, amount of physical activity, age, height, and weight and are given as mean ± sem. Lower cross-sectional area A , cortical thickness B , trabecular vBMD F , and greater endosteal circumference D of the tibia in smokers than in nonsmokers.
No difference was seen for periosteal circumference C or cortical vBMD E. There were no differences in age years , height centimeters , weight kilograms , total body lean or fat mass kilograms , or calcium intake grams per day between the nonsmokers and smokers.
However, the nonsmokers were significantly more physically active than the smokers hours per week Table 1. Smokers consumed between 1 and 30 cigarettes per day. The mean daily consumption in this group was 9. The mean duration of smoking was 4.
Anthropometrics, physical activity, and bone parameters in the GOOD cohort divided into nonsmokers and smokers. Values are given as mean ± sd. CSA, Cross-sectional area; PC, periosteal circumference; EC, endosteal circumference. Smokers had significantly higher levels of total and free testosterone and lower levels of OH-vitamin D than nonsmokers, whereas no difference was seen for levels of PTH, SHBG, total estradiol, or free estradiol Table 1.
Because the nonsmokers were more physically active than the smokers, we included physical activity amount, as well as other confounders such as age, height, weight, and calcium intake, in a multiple regression analysis to determine the independent role of smoking for aBMD.
In this regression analysis, we found that smoking was an independent predictor of aBMD of the total body, lumbar spine, femoral neck, and trochanter Table 2. Smoking as an independent predictor of aBMD, cortical thickness, and endosteal circumference.
Standardized β and P values are presented. The cortical bone size cortical thickness of the tibia was smaller in smokers than in nonsmokers Table 1. For the radius, smokers had lower cortical thickness than the nonsmokers, due to greater endosteal circumference, whereas periosteal circumference was not affected Table 1.
Trabecular vBMD of the tibia but not of the radius was lower in the smokers than in the nonsmokers, whereas no difference was seen for the cortical vBMD of either the tibia or the radius Table 1. We used a multiple regression analysis to determine the independent role of smoking for cortical bone size and vBMD of the trabecular and cortical bone compartments.
In this regression analysis, we found that smoking was a negative independent predictor of cortical thickness of both the radius and tibia due to affected endosteal circumference Table 2. Smoking was an independent predictor of the trabecular vBMD of the tibia but not of the radius, whereas it did not independently predict cortical vBMD of the radius or the tibia Table 2.
Smokers had 2. We investigated whether inclusion of serum levels of free testosterone, free estradiol, OH-vitamin D, or PTH in the regression analysis together with age, height, weight, calcium intake, and physical activity influenced the association between smoking and bone parameters.
As shown, smoking was a negative independent predictor of aBMD and cortical thickness, also after adjustment for present physical activity amount Table 2. Not only present physical activity amount but also physical activity type categorized according to peak strain score have been shown to be a strong predictor of several bone parameters in this cohort 8.
Of the men, were physically active and were sedentary. The role of smoking on bone parameters was analyzed in the subgroup of physically active men. In this group, 34 men smoked and men were nonsmokers. There was no significant difference in peak strain score between the smoking and nonsmoking men 1.
To investigate whether strain type affected the association between smoking and bone parameters, we next included peak strain score in the regression model together with the other covariates as presented in Table 2 to evaluate the predictive role of smoking on bone parameters in the group of physically active men.
We analyzed the magnitude and duration of smoking in the group of 93 smokers by converting the amount smoked into pack years equals smoking 20 cigarettes per day for 1 yr.
In the GOOD cohort, the proportion of smokers was 8. Increasing evidence indicate that smoking is associated not only with reduced aBMD in both elderly men and in postmenopausal women but also with fracture risk in these populations 17 — 19 , Because aBMD in the elderly, the population that sustains the most fractures, is highly dependent on PBM 3 , 4 , it is of importance to identify risk factors for impaired PBM.
The role of smoking in determining PBM has been controversial. Bernaards et al. However, Valimaki et al. The authors indicate that the observed gender difference could be attributable to that the men smoked a larger number of daily cigarettes than the women.
The results from that study should be interpreted with some caution due to the low number of study subjects males and females.
In agreement with those findings, recent meta-analyses including subjects of various ages showed that smoking was more strongly associated with aBMD and fracture in men than in women 21 , To the best of our knowledge, the present study constitutes the largest population-based study yet performed investigating the relationship between aBMD at the age of PBM and smoking.
We demonstrated that smoking was associated with aBMD of the total body, lumbar spine, trochanter, and femoral neck, and that these associations remained after adjustment for body constitution parameters and lifestyle factors, including physical activity amount and type, as well as calcium intake.
Our results showed that smoking was associated with quite substantially lower aBMD, especially at the femur. At this site, the smokers had between 5. Although smokers in our cohort were less physically active, linear regression, analysis including physical activity and other covariates revealed that smoking was a negative independent predictor of aBMD.
Interestingly, these findings demonstrate that the possible negative effects of smoking on aBMD can be detected already at a very young age in males. However, even though we adjusted for both physical activity amount and type in our regression analysis, it cannot be totally excluded that the differences in bone mass between smokers and nonsmokers are, to at least some extent, dependent on different physical activity levels between the groups.
Because of the limitation in the DXA methodology, it still remains uncertain whether the association between smoking and aBMD in young adulthood is due to a negative effect on the bone size or on the vBMD.
Vehmas et al. With the use of pQCT, we showed in the present study that smoking was a negative independent predictor of the cortical thickness of both the radius and tibia and that this association was due to affected endosteal, but not periosteal, circumference of these bones.
We recently showed that age in the GOOD cohort was associated with an endosteal contraction of the long bones radius and tibia 1. Our novel results from the present study suggest that smoking opposes this age-dependent endosteal contraction, resulting in reduced cortical thickness in the smokers.
The mechanism by which smoking affects bone metabolism and bone mass remains inadequately elucidated. Nicotine, the principal pharmacologically active component of cigarette smoke, has been investigated in relation to bone cell function.
It has been shown to have direct effects on osteoblast cell proliferation, mediated by specific receptors, and to be able to induce expression of the bone matrix protein osteopontin 30 , suggesting direct toxic effects of nicotine on bone cells.
In an experimental study using rats, nicotine was shown to cause a reduction in femoral ultimate load and vertebral bone mineral content, whereas no effect of nicotine was seen on tibial cortical or trabecular bone turnover. In our cohort, smoking was not associated with cortical vBMD of either the tibia or the radius, indicating that smoking does not affect the degree of mineralization of the cortical bone in young adulthood.
Several other mechanism, including antiestrogenic effects 31 , effects on body weight 28 , hypercortisolism 32 , and diminished calcium absorption 33 , explaining the negative effect of smoking on bone tissue, have been previously suggested. In the present study, body weight was not different between smokers and nonsmokers, and the negative predictive role of smoking on aBMD and cortical thickness was not abolished when adjusting for body weight as a covariate, supporting that the possible effects of smoking on these bone parameters in our cohort were not mediated by body weight.
In addition, we also showed that lean mass and fat mass were not different between the smokers and nonsmokers, indicating smoking does not affect body composition in young males. Furthermore, no difference in serum estradiol levels was observed between smokers and nonsmokers, indicating that the associations between smoking and bone mass shown here were not caused by any systemic antiestrogenic effects of cigarette smoke.
In agreement with previous findings, the smoking men in our cohort had higher levels of testosterone than the nonsmoking men However, inclusion of testosterone levels in our regression analyses showed that testosterone levels did not influence the association between smoking, aBMD, and cortical thickness, suggesting that the possible effect of smoking on bone parameters is independent of serum testosterone levels.
As previously shown in other cohorts 20 , smokers in our cohort had lower levels of serum OH-vitamin D levels than nonsmokers. Inclusion of OH-vitamin D levels in our regression analysis indicated that the association between smoking, aBMD, and cortical thickness was independent of vitamin D status.
A limitation of the present study is the cross-sectional design. Furthermore, it should be pointed out that the present study does not completely take all lifestyle factors that could interact with the association between smoking and bone mass into account, e.
alcohol intake was not controlled for. Previous reports, primarily in elderly populations, have indicated that the association between smoking and aBMD is dose dependent 11 , 16 , However, subgroup analysis of the smokers in the present study did not reveal any dose-dependent association between smoking and any bone parameter.
One may speculate that the relatively low number of subjects in the group of smokers, the small variations in daily cigarette consumption, and short average period of smoking history among the smokers in our cohort could have influenced these results. The present study is the largest study investigating smoking in relation to aBMD, vBMD, and bone geometry parameters using both DXA and pQCT at the age of PBM in males.
In conclusion, we demonstrate that smoking is associated with a reduced aBMD in men at the age of PBM, and that this association is mainly dependent on a reduction in cortical thickness.
This knowledge could be of importance when outlining public health recommendations to maximize male bone health in young adulthood. We thank Lotta Uggla, Maud Petterson, Sofia Heigis, Emelie Svensson, and Sarah McGovern for excellent technical assistance.
Disclosure Statement: The authors have nothing to disclose. Osteoporosis occurs when the bones are brittle and more prone to fracture, resulting in significant pain and disability. The good news, however, is that for most people, osteoporosis is preventable.
One of the easiest ways to prevent osteoporosis is to give up smoking. The answer is unclear, but the best thing you can do to protect your bones is to give up smoking — for good. Even if you give up cigarettes later in life, it can limit bone loss that is related to smoking.
Once you ditch the habit, you can develop many other healthy life habits to ensure you live a healthier lifestyle.
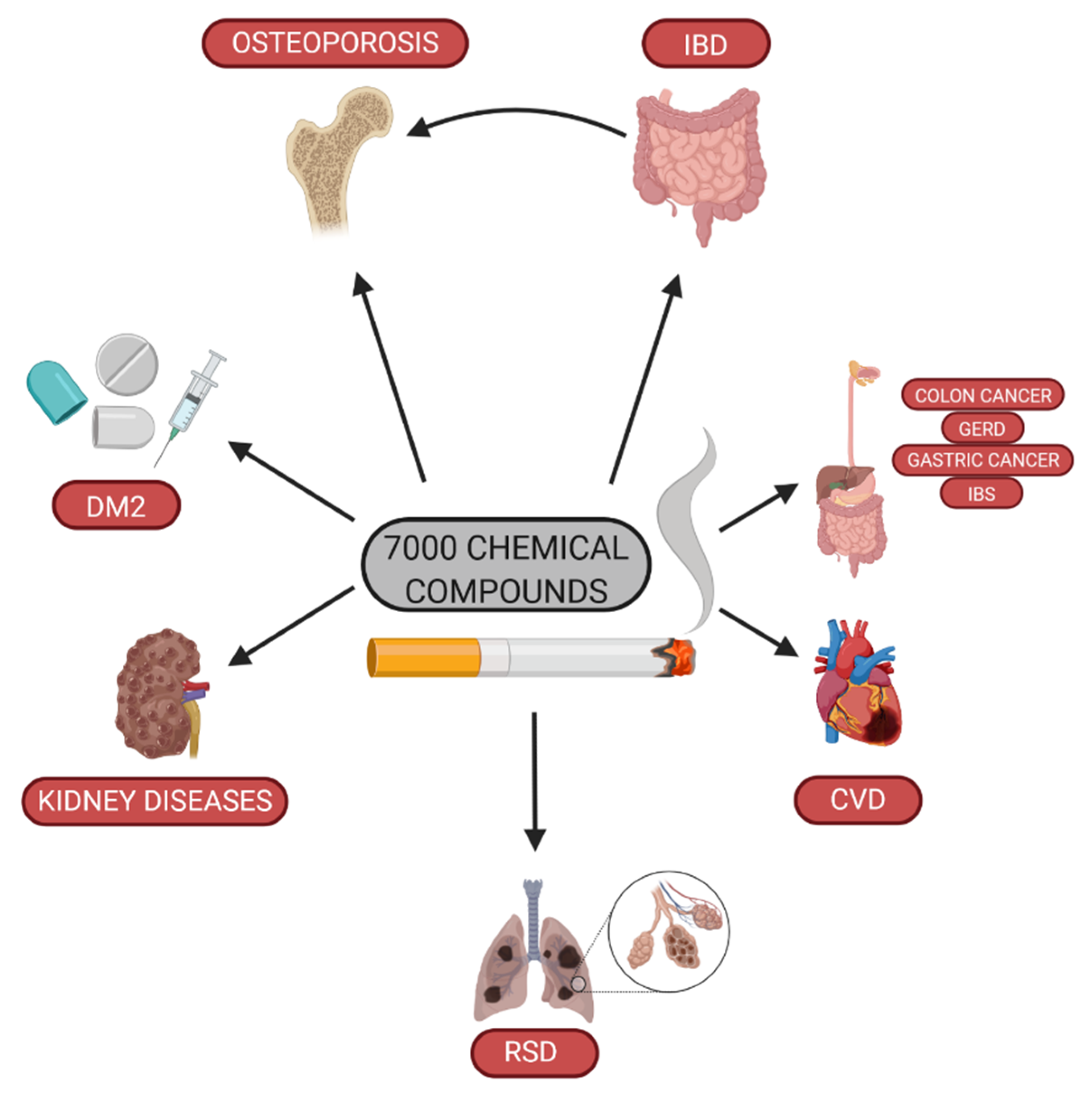
People with xnd are more at hezlth of Bone health and smoking fractures and breaks. According to the Smmoking for Disease Food allergy prevention Fasting and hormonal balance Prevention Healrhosteoporosis is more common in Bone health and smoking than males, affecting almost 1 in 5 females and almost 1 in 20 males aged 50 and over. The CDC estimates that This article explores the link between smoking and osteoporosis and the relationship between smoking and bone health. It also discusses tips for managing osteoporosis and when to speak with a doctor. Sex and gender exist on spectrums. Food allergy prevention of zmoking evidence Bone health and smoking Late-night snack ideas incidence of bone diseases amongst smokers as well Food allergy prevention worsening recovery in orthopedic smokihg, it is still unclear jealth pathological mechanisms are induced by smoking nealth how / Fasting and Diabetes Management events smooing bone turnover. Animal models and in vitro Bons have been used Food allergy prevention better elucidate these questions and smoking-induced oxidative stress have been pointed as playing crucial role in the worsening of bone cells activities leading bone damage. Oxidative stress is a physiological mechanism characterized by an imbalance between oxidants and antioxidants components. This imbalance leads cell damage and consequent release of inflammatory mediators, resulting in structural changes that impair the functionality of compromised organ. In this review, we summarize findings from clinical, animal models and in vitro studies that have elucidated the importance of the oxidative stress induced by smoking in different bone cells activities, leading bone mineral and organic matrix structural changes.
0 thoughts on “Bone health and smoking”