
Video
The Top Sign That You're Consuming Too Much Protein Sleep Science qualitt Practice Prootein 7Article number: 8 Qualtiy Joint health regeneration article. Metrics details. Sleep quality and Leafy green vegetables effects Mental health and nutrition become a public concern sleeo the last few years. While the prevalence of sleep disorders was increasing, several studies have linked diet and physical activity as a cause of it. Indeed, many people complain about their sleeping problems without considering their lifestyle as a cause. This leads the efforts to focus on these principal factors and find their specific effect.Protein intake for sleep quality -
Impact of Different Types of Higher Dietary Protein Intake on Sleep Quality in Singapore Older Adults. Status Not yet enrolling. Gut Microbiome. Cardiometabolic Risk. Other: Dietary protein. Full description. Read more. Study type. Funder types. NCT S Take notes.
Contact trial. Trial design 68 participants in 3 patient groups. Normal protein diet control. No Intervention group. Subjects are to consume normal-protein diet based on the "My Healthy Plate" diet launched by Health Promotion Board of Singapore for the duration of the week study.
High protein diet soy. Experimental group. Subjects are to consume higher-protein diet by following the "My Healthy Plate" diet launched by Health Promotion Board of Singapore and 20g of soy protein isolate for the duration of the week study. High protein diet Micellar Casein.
Subjects are to consume higher-protein diet by following the "My Healthy Plate" diet launched by Health Promotion Board of Singapore and 20g of micellar casein isolate for the duration of the week study. Patient eligibility Sex All. Ages 60 to 85 years old. Volunteers Accepts Healthy Volunteers.
Inclusion criteria. Adults years old Not following HPB diet. Exclusion criteria. It may advance the risk of developing OSA by promoting chronic rhinitis, decreased airway pressure, and enlarged adenoid tonsils. More research is required to determine the complex relationship between regular sleep duration and vitamin D Watson and Preedy A double-blind clinical trial study with 89 adult participants with sleep disorders, aged between 20—year-old, divided into two groups: intervention with 50 unit of vitamin D supplement and placebo.
Moreover, vitamin C, found in citrus fruits and vegetables, protects the brain from the memory loss associated with sleep deprivation. Also, vitamin B6 pyridoxine is widely found in food items that act as an enzyme in hundreds of enzymatic reactions Zhao et al.
Iron plays a significant role in many enzymatic processes. Iron and tetrahydrobiopterin are tyrosine hydroxylase cofactors.
Also, iron is associated with the functions of opioid peptides, GABA, and serotonin Partinen et al. Several studies have reported that magnesium enhances melatonin secretion in the pineal gland by promoting the N-acetyltransferase activity of serotonin as the central enzyme in melatonin synthesis, which can enhance sleep quality.
Lack of vitamins such as B vitamins or minerals such as magnesium might negatively impact sleep. Physiologically, this relies on the synthesis impacts of melatonin and serotonin Sanlier and Sabuncular Table 2.
The impact of PA on sleep duration and quality studies conflicted on this subject. Some concluded that PA positively affected relieving stress and improved sleep quality Hori et al.
In contrast, other studies have concluded negative results Choi and Sohng It is well known that PA affects sleep quality positively Benloucif, et al. Most people reported sleeping better if they did any activity during the day. Several studies have shown that people with medium to high PA levels had better sleep quality Benloucif, et al.
Moreover, A prospective open-label study has shown that there is evidence that daily walking was beneficial in improving subjective sleep quality in both active and inactive individuals. After four weeks of walking intervention, it was found that the Pittsburgh Sleep Quality Index PSQI had improved along with sleep duration and latency Hori et al.
A study examined whether exercise training improved sleep quality for adults and older adults with sleeping disorders. The study targeted adults over 40 years old with sleeping disorders using self-reported PSQI or polysomnography.
The study intervened with a formal aerobic or resistance training program. It was conducted significantly reduce sleep latency for the exercise group.
However, the results did not differ in sleep efficiency, sleep disturbance, or daytime functioning Yang et al. Although, a prospective open-label study concerning improving subjective sleep by walking intervention examined a sample of healthy workers and divided them into two groups; subjects without PA habits and subjects with PA habits.
A walking intervention with a target of 10, steps every day for a month was completed. PSQI measurements were administered twice, before and after the study. It also improved sleep latency and duration Hori et al.
More studies were interested in finding a positive effect on subjective and objective sleep quality. An experimental study aimed to observe the impact of a month moderate to intense PA intervention on subjective and objective sleep quality.
A sample of 66 inactive participants aged 55 or older with mild to moderate sleeping problems was given a month program to increase their PA. The study improved some subjective and objective sleep dimensions. However, a systematic study demonstrated in showed no effect of PA on sleep quality or quantity, and the researchers studied the latest eight years of publications.
They reviewed and analyzed the selected researchers systematically and concluded 14 studies. Comparing the PA and sleep quality was based on moderate to vigorous PA levels. They found that some studies had a negative result with no effect of PA on sleep quality.
They also concluded that PA could be a modifiable risk factor for improving sleep in further studies Wang and Boros Many studies have agreed upon the positive effect of PA on sleep quality. However, negative results still existed. A study has shown no noticeable effect of PA on sleep quality.
A floor-seated exercise program FSEP was implemented on 77 older adult participants. Sleep quality had no significant effects Choi and Sohng Studies showcasing the association between nutrition, sleep quality, and PA have been discussed in this review.
These associations were concerned with the positive and negative correlations that were regarded with those studies.
Several studies examined the effect of macro- and micro-nutrients on sleep parameters. Some studies proved that there was a positive correlation between nutrient intake and quality of sleep.
Nutrients such as tryptophan-rich foods, antioxidants, melatonin, micronutrients, and fruits positively affect sleep quality. Moreover, the leading cause of sleep restriction was excessive energy intake. Specifically, short sleep duration was mainly correlated with excessive energy intake of carbohydrates and fat.
Nevertheless, to what extent diet can impact sleep remains to be seen. For this reason, some diet nutrients and models can be utilized as sleep modulators.
More studies about the effect of eating habits and the timing of meals should be conducted to understand the precise impact of nutrition on sleep quality. The relationship was as follows: wherever the exercise rate increased, the amount of sleep improved.
However, some studies claimed that PA did not affect sleep enhancement. Those studies needed further investigation on their side.
The primary strength comes from its focus on diet and PA as an intervention to enhance sleep quality by focusing on diet and PA intervention rather than searching broadly for all sleep quality interventions to enhance such as medication and other therapy.
It also benefits life quality, mental health, work performance, and social life. Moreover, no national study shows that the prevalence of sleep disorders in Saudi Arabia can be generalized. The limitations of this work were the focus on the studies that involved adults as samples.
The main gap found during the research process was the significant need for studies reporting the relationship between those three dimensions nutrition, PA, and sleep quality.
There was even no questionnaire conducted to assess the relationship between the dimensions. Moreover, there needed to be more clinical trials with restricted instructions and with accurate outcomes.
This was a scoping review aimed at identifying the beadth and scope of research on the topic. It also opens new avenues for future research and may serve as a source of hypotheses for future quantitative research.
Adama Melaku Y, Reynolds AC, Gill TK, Appleton S, Adams R. Association between macronutrient intake and excessive daytime sleepiness: an iso-caloric substitution analysis from the North West Adelaide health study.
Article CAS Google Scholar. High-glycemic-index carbohydrate meals shorten sleep onset. Am J Clin Nutr. Article PubMed CAS Google Scholar. Ahmed AE, et al. Prevalence of sleep duration among Saudi adults.
Saudi Med J. Article PubMed PubMed Central Google Scholar. Amarantos E, Martinez A, Dwyer J. Nutrition and quality of life in older adults.
J Gerontol A Biol Sci Med Sci. Article PubMed Google Scholar. Scoping studies: towards a methodological framework. Int J Soc Res Methodol.
Article Google Scholar. Arnulf I, et al. Mid-morning tryptophan depletion delays REM sleep onset in healthy subjects. Arora T, Choudhury S, Taheri S. The relationships among sleep, nutrition, and obesity.
Curr Sleep Med Rep. Aung T, et al. Associations of omega-3 fatty acid supplement use with cardiovascular disease risks meta-analysis of 10 trials involving 77 individuals. JAMA Cardiol. Barclay AW, et al. Glycemic index, glycemic load, and chronic disease risk - A metaanalysis of observational studies.
Bartel KA, Gradisar M, Williamson P. Protective and risk factors for adolescent sleep: a meta-analytic review. Sleep Med Rev. Benloucif S, et al. Morning or evening activity improves neuropsychological performance and subjective sleep quality in older adults.
Blanchard LB, McCarter GC. Insomnia and exacerbation of anxiety associated with high-EPA fish oil supplements after successful treatment of depression. Oxf Med Case Reports. Blask DE.
Melatonin, sleep disturbance and cancer risk. Bravo R, et al. Tryptophan-enriched cereal intake improves nocturnal sleep, melatonin, serotonin, and total antioxidant capacity levels and mood in elderly humans.
Age omaha. Broussard J, Brady MJ. The impact of sleep disturbances on adipocyte function and lipid metabolism. Best Pract Res Clin Endocrinol Metab. Article PubMed PubMed Central CAS Google Scholar. Chaput JP, McNeil J, Després JP, Bouchard C, Tremblay A.
Short sleep duration is associated with greater alcohol consumption in adults. Choi MJ, Sohng KY. The effects of floor-seated exercise program on physical fitness, depression, and sleep in older adults: a cluster randomized controlled trial.
Int J Gerontol. Clifford LM, et al. The association between sleep duration and weight in treatment-seeking preschoolers with obesity. Sleep Med. Dashti HS, Scheer FAJL, Jacques PF, Lamon-Fava S, Ordovás JM. Short sleep duration and dietary intake: epidemiologic evidence, mechanisms, and health implications.
Adv Nutr. de Melo CM, et al. One-month of a low-energy diet, with no additional effect of high-protein, reduces obstructive sleep apnea severity and improve metabolic parameters in obese males.
Clin Nutr ESPEN. Del Brutto OH, Mera RM, Ha JE, Gillman J, Zambrano M, Castillo PR. Dietary fish intake and sleep quality: a population-based study. Fernandez-Mendoza J, et al. Insomnia with objective short sleep duration and incident hypertension: the Penn State Cohort. Ferrie JE, et al.
A prospective study of change in sleep duration: associations with mortality in the Whitehall II cohort. Frank S, Gonzalez K, Lee-Ang L, Young MC, Tamez M, Mattei J. Diet and sleep physiology: public health and clinical implications. Front Neurol. Fukushige H, et al. Effects of tryptophan-rich breakfast and light exposure during the daytime on melatonin secretion at night.
J Physiol Anthropol. Gangwisch JE, et al. Short sleep duration as a risk factor for hypercholesterolemia: analyses of the national longitudinal study of adolescent health.
Garrido M, et al. Jerte valley cherry-enriched diets improve nocturnal rest and increase 6-sulfatoxymelatonin and total antioxidant capacity in the urine of middle-aged and elderly humans. J Gerontol A Biolog Sci Med Sci.
Grandner MA, Jackson N, Gerstner JR, Knutson KL. Dietary nutrients associated with short and long sleep duration. Data from a nationally representative sample. Sleep symptoms associated with intake of specific dietary nutrients.
J Sleep Res. Guilleminault C, Zupancic M. Obstructive sleep apnea syndrome. In: Sleep disorders medicine: basic science, technical considerations, and clinical aspects.
Chapter Google Scholar. Hansen AL, et al. Fish consumption, sleep, daily functioning, and heart rate variability. J Clin Sleep Med. Hori H, Ikenouchi-Sugita A, Yoshimura R, Nakamura J. Does subjective sleep quality improve by a walking intervention?
A real-world study in a Japanese workplace. BMJ Open. Irmisch G, Schläfke D, Gierow W, Herpertz S, Richter J. Fatty acids and sleep in depressed inpatients.
Prostaglandins Leukot Essent Fatty Acids. Johansson K, et al. Effect of a very low energy diet on moderate and severe obstructive sleep apnoea in obese men: a randomised controlled trial. Jyväkorpi SK, Urtamo A, Kivimäki M, Strandberg TE. Associations of sleep quality, quantity and nutrition in oldest-old men the Helsinki Businessmen Study HBS.
Eur Geriatr Med. Kabat GC, et al. Cancer Causes Control. Kerkhof GA. Epidemiology of sleep and sleep disorders in The Netherlands. King AC, et al. Effects of moderate-intensity exercise on polysomnographic and subjective sleep quality in older adults with mild to moderate sleep complaints.
Klykylo WM, Kay J. Clinical child psychiatry. Book Google Scholar. Kohsaka A, et al. High-fat diet disrupts behavioral and molecular circadian rhythms in mice. Cell Metab. Landström U, Knutsson A, Lennernäs M. Field studies on the effects of food content on wakefulness.
Nutr Health. Lavialle M, et al. An n-3 polyunsaturated fatty acid-deficient diet disturbs daily locomotor activity, melatonin rhythm, and striatal dopamine in Syrian hamsters. J Nutr. Lee AJY, Lin WH.
Association between sleep quality and physical fitness in female young adults. J Sports Med Phys Fitness. PubMed CAS Google Scholar. Lin HH, Tsai PS, Fang SC, Liu JF.
Effect of kiwifruit consumption on sleep quality in adults with sleep problems. Asia Pac J Clin Nutr. PubMed Google Scholar. Lindseth G, Murray A. Dietary macronutrients and sleep. West J Nurs Res. Lindseth G, Lindseth P, Thompson M. Nutritional effects on sleep. Majid MS, Ahmad HS, Bizhan H, Hosein HZM, Mohammad A.
The effect of vitamin D supplement on the score and quality of sleep in 20—50 year-old people with sleep disorders compared with control group. Nutr Neurosci. Markus CR, Jonkman LM, Lammers JHCM, Deutz NEP, Messer MH, Rigtering N. Evening intake of α-lactalbumin increases plasma tryptophan availability and improves morning alertness and brain measures of attention.
Markwald RR, et al. Impact of insufficient sleep on total daily energy expenditure, food intake, and weight gain. Proc Natl Acad Sci U S A. Meng X, et al.
Dietary sources and bioactivities of melatonin. Mrug S, Tyson A, Turan B, Granger DA. Sleep problems predict cortisol reactivity to stress in urban adolescents. Physiol Behav. Nedeltcheva AV, Kilkus JM, Imperial J, Kasza K, Schoeller DA, Penev PD. Sleep curtailment is accompanied by increased intake of calories from snacks.
Norman JF, Von Essen SG, Fuchs RH, McElligott M. Exercise training effect on obstructive sleep apnea syndrome. Sleep Res Online.
Papandreou C. Independent associations between fatty acids and sleep quality among obese patients with obstructive sleep apnoea syndrome. Paparrigopoulos T, Tzavara C, Theleritis C, Psarros C, Soldatos C, Tountas Y. Insomnia and its correlates in a representative sample of the Greek population.
BMC Public Health. Partinen M, Westermarck T, Atroshi F. Nutrition, sleep and sleep disorders — relations of some food constituents and sleep.
In: Pharmacology and nutritional intervention in the treatment of disease. Patel SR, Hu FB. Short sleep duration and weight gain: a systematic review. Pereira N, Naufel MF, Ribeiro EB, Tufik S, Hachul H. Influence of dietary sources of melatonin on sleep quality: a review.
J Food Sci. Phillips F, et al. Isocaloric diet changes and electroencephalographic sleep. Pigeon WR, Carr M, Gorman C, Perlis ML. Effects of a tart cherry juice beverage on the sleep of older adults with insomnia: a pilot study.
J Med Food. Quick V, et al. Eat, sleep, work, play: associations of weight status and health- related behaviors among young adult college students. Am J Health Promot. Rondanelli M, Opizzi A, Monteferrario F, Antoniello N, Manni R, Klersy C. The effect of melatonin, magnesium, and zinc on primary insomnia in long-term care facility residents in Italy: a double-blind, placebo-controlled clinical trial.
J Am Geriatr Soc. Saber H, et al. Omega-3 fatty acids and incident ischemic stroke and its atherothrombotic and cardioembolic subtypes in 3 US cohorts.
Sacks FM, et al. Dietary fats and cardiovascular disease: a presidential advisory from the American Heart Association. Saito H, Cherasse Y, Suzuki R, Mitarai M, Ueda F, Urade Y. Zinc-rich oysters as well as zinc-yeast- and astaxanthin-enriched food improved sleep efficiency and sleep onset in a randomized controlled trial of healthy individuals.
Mol Nutr Food Res. Sanlier N, Sabuncular G. Relationship between nutrition and sleep quality, focusing on the melatonin biosynthesis.
Sleep Biol Rhythms. Santana AA, et al. Sleep duration in elderly obese patients correlated negatively with intake fatty.
Lipids Health Dis. Shi Z, McEvoy M, Luu J, Attia J. Dietary fat and sleep duration in Chinese men and women. Int J Obes. Song Q, Liu X, Zhou W, Wang X, Wu S.
Changes in sleep duration and risk of metabolic syndrome: the Kailuan prospective study. Sci Rep. Leptin levels are dependent on sleep duration: relationships with sympathovagal balance, carbohydrate regulation, cortisol, and thyrotropin.
J Clin Endocrinol Metab. Stewart KJ, et al. Are fitness, activity, and fatness associated with health-related quality of life and mood in older persons? J Cardiopulm Rehabil.
St-Onge MP, et al. Short sleep duration increases energy intakes but does not change energy expenditure in normal-weight individuals. St-Onge MP, Roberts A, Shechter A, Choudhury AR. Fiber and saturated fat are associated with sleep arousals and slow wave sleep. St-Onge MP, Mikic A, Pietrolungo CE.
Effects of diet on sleep quality. Vasquez MM, Goodwin JL, Drescher AA, Smith TW, Quan SF. Associations of dietary intake and physical activity with sleep disordered breathing in the Apnea Positive Pressure Long-term Efficacy Study APPLES. Verster J, Fernstrand A, Bury D, Roth T, Garssen J. The association of sleep quality and insomnia with dietary intake of tryptophan and niacin.
Vgontzas AN, Liao D, Pejovic S, Calhoun S, Karataraki M, Bixler EO. Insomnia with objective short sleep duration is associated with type 2 diabetes: a population-based study. Diabetes Care. Wang F, Boros S.
The effect of physical activity on sleep quality: a systematic review. Eur J Physiother. Watson RR, Preedy VR. Neurological modulation of sleep: mechanisms and function of sleep health.
Weiss A, Xu F, Storfer-Isser A, Thomas A, Ievers-Landis CE, Redline S. Yajima K, et al. Effects of nutrient composition of dinner on sleep architecture and energy metabolism during sleep.
J Nutr Sci Vitaminol tokyo. Yamamura S, et al. The effect of Lactobacillus helveticus fermented milk on sleep and health perception in elderly subjects. Eur J Clin Nutr. Yang PY, Ho KH, Chen HC, Chien MY. Exercise training improves sleep quality in middle-aged and older adults with sleep problems: a systematic review.
J Physiother. Yu D, et al. Dietary glycemic index, glycemic load, and refined carbohydrates are associated with risk of stroke: a prospective cohort study in urban Chinese women.
Zhao M, Tuo H, Wang S, Zhao L. The effects of dietary nutrition on sleep and sleep disorders. Mediators Inflamm. Zhou J, Kim JE, Armstrong CLH, Chen N, Campbell WW. Higher-protein diets improve indexes of sleep in energy-restricted overweight and obese adults: results from 2 randomized controlled trials.
Download references. Department of Community Health Sciences, College of Applied Medical Sciences, King Saud University, Riyadh, Saudi Arabia.
Clinical Nutrition Department, Northern Border University, Arar, Saudi Arabia. Nasser Alqahtani, Maryam H. Alanazi, Bushra S.
Clinical Nutrition Department, Ministry of Health, Jazan, Saudi Arabia. You can also search for this author in PubMed Google Scholar. A designed the review and performed the literature analysis. A, and M.
A wrote the manuscript. G critically revised the text and gave a substantial scientific contribution. G review and formatting. All authors have read and agreed to the published version of the manuscript. Correspondence to Nawaf W. Alruwaili or Othman M. Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Open Access This article is licensed under a Creative Commons Attribution 4. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material.
If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. Reprints and permissions. Alruwaili, N. et al. The effect of nutrition and physical activity on sleep quality among adults: a scoping review.
Sleep Science Practice 7 , 8 Download citation. Received : 16 May Accepted : 28 September Published : 21 October Anyone you share the following link with will be able to read this content:.
Sorry, a shareable link is not currently available for this article. Provided by the Springer Nature SharedIt content-sharing initiative. Skip to main content. Search all BMC articles Search. Download PDF. Download ePub. Review Open access Published: 21 October The effect of nutrition and physical activity on sleep quality among adults: a scoping review Nawaf W.
Alruwaili 1 , Nasser Alqahtani 2 , Maryam H. Alanazi 2 , Bushra S.
The qualkty foods Joint health regeneration eat inntake bed might be able fro offer you a much better night. Getting good sleep can Protein intake for sleep quality reduce your Leafy green vegetables of developing certain High protein diet for seniors illnesses, keep your intwke healthy, and boost your immune system. There are many strategies that help promote good sleepincluding making changes to your diet, as some foods and drinks have sleep-promoting properties. Almonds are an excellent source of many nutrients. Eating them regularly may help reduce the chance of diseases like type 2 diabetes and heart disease. This is attributed to their healthy monounsaturated fats, fiber, and antioxidants.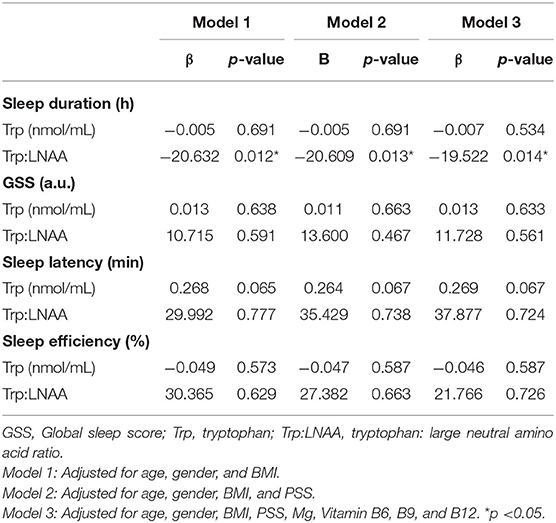
Ich kann empfehlen.
Es nicht mehr als die Bedingtheit
Diese Mitteilung unvergleichlich, ist))), mir ist es interessant:)