Video
Diabetes Diet Plan II Diabetes Foods to Eat II Diabetes Plate Method II Blood Sugar Control TipsDiabetic coma and meal planning -
Blood sugar that's either too high or too low for too long may cause the following serious health problems, all of which can lead to a diabetic coma.
Diabetic ketoacidosis. If your muscle cells become starved for energy, your body may start breaking down fat for energy. This process forms toxic acids known as ketones. If you have ketones measured in blood or urine and high blood sugar, the condition is called diabetic ketoacidosis.
If it's not treated, it can lead to a diabetic coma. Diabetic ketoacidosis is most common in people who have type 1 diabetes. But it can also occur in people who have type 2 diabetes or gestational diabetes. Diabetic hyperosmolar syndrome.
When blood sugar is very high, the extra sugar passes from the blood into the urine. That triggers a process that draws a large amount of fluid from the body. If it isn't treated, this can lead to life-threatening dehydration and a diabetic coma.
Anyone who has diabetes is at risk of a diabetic coma, but the following factors can increase the risk:.
Good day-to-day control of your diabetes can help you prevent a diabetic coma. Keep these tips in mind:. Consider a continuous glucose monitor, especially if you have trouble maintaining stable blood sugar levels or you don't feel symptoms of low blood sugar hypoglycemia unawareness.
Continuous glucose monitors are devices that use a small sensor inserted underneath the skin to track trends in blood sugar levels and send the information to a wireless device, such as a smart phone.
These monitors can alert you when your blood sugar is dangerously low or if it is dropping too fast. But you still need to test your blood sugar levels using a blood glucose meter even if you're using one of these monitors. Continuous glucose monitors are more expensive than other glucose monitoring methods, but they may help you control your glucose better.
A continuous glucose monitor, on the left, is a device that measures blood sugar every few minutes using a sensor inserted under the skin. An insulin pump, attached to the pocket, is a device that's worn outside of the body with a tube that connects the reservoir of insulin to a catheter inserted under the skin of the abdomen.
Insulin pumps are programmed to deliver specific amounts of insulin continuously and with food. On this page. When to see a doctor. Risk factors. A Book: Guide to the Comatose Patient.
A Book: The Essential Diabetes Book. Symptoms of high blood sugar or low blood sugar usually develop before a diabetic coma. High blood sugar hyperglycemia If your blood sugar level is too high, you may have: Increased thirst Frequent urination Blurred vision Tiredness or weakness Headache Nausea and vomiting Shortness of breath Stomach pain Fruity breath odor A very dry mouth.
Low blood sugar hypoglycemia If your blood sugar is too low, you may have: Shakiness Anxiety Tiredness or drowsiness Weakness Sweating Hunger A feeling of tingling on your skin Dizziness or lightheadedness Headache Difficulty speaking Blurry vision Confusion Loss of consciousness Some people, especially those who've had diabetes for a long time, develop a condition known as hypoglycemia unawareness.
Request an appointment. From Mayo Clinic to your inbox. Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview. To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you.
If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices.
You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail. Your brain needs sugar glucose to function.
In severe cases, low blood sugar hypoglycemia may cause you to pass out. Low blood sugar can be caused by too much insulin or not enough food. Exercising too vigorously or drinking too much alcohol can have the same effect.
Anyone who has diabetes is at risk of a diabetic coma, but the following factors can increase the risk: Insulin delivery problems. If you're using an insulin pump, you have to check your blood sugar frequently. Insulin delivery can stop if the pump fails or if the tubing catheter becomes twisted or falls out of place.
A lack of insulin can lead to diabetic ketoacidosis. An illness, trauma or surgery. When you're sick or injured, blood sugar levels can change, sometimes significantly, increasing your risk of diabetic ketoacidosis and diabetic hyperosmolar syndrome.
Poorly managed diabetes. If you don't monitor your blood sugar properly or take your medications as directed by your health care provider, you have a higher risk of developing long-term health problems and a higher risk of diabetic coma. Deliberately skipping meals or insulin. Sometimes, people with diabetes who also have an eating disorder choose not to use their insulin as they should, in the hope of losing weight.
This is a dangerous, life-threatening thing to do, and it raises the risk of a diabetic coma. Drinking alcohol. Alcohol can have unpredictable effects on your blood sugar.
Alcohol's effects may make it harder for you to know when you're having low blood sugar symptoms. This can increase your risk of a diabetic coma caused by hypoglycemia. Illegal drug use. Illegal drugs, such as cocaine, can increase your risk of severe high blood sugar and conditions linked to diabetic coma.
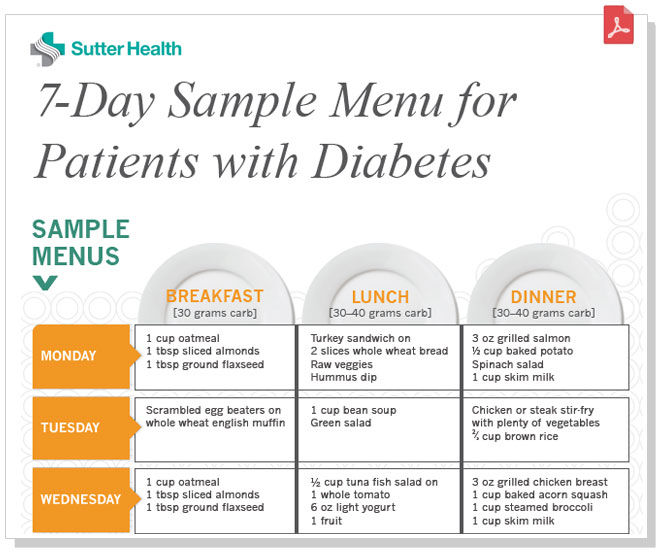
If it is not treated, a diabetic coma can lead to permanent brain damage and death. Keep these tips in mind: Follow your meal plan.
Consistent snacks and meals can help you control your blood sugar level. Keep an eye on your blood sugar level. Frequent blood sugar tests can tell you whether you're keeping your blood sugar level in your target range.
It also can alert you to dangerous highs or lows. Check more frequently if you've exercised. Exercise can cause blood sugar levels to drop, even hours later, especially if you don't exercise regularly. Take your medication as directed. If you have frequent episodes of high or low blood sugar, tell your health care provider.
You may need to have the dose or the timing of your medication adjusted. Have a sick-day plan. Illness can cause an unexpected change in blood sugar.
If you are sick and unable to eat, your blood sugar may drop. While you are healthy, talk with your doctor about how to best manage your blood sugar levels if you get sick. Consider storing at least a week's worth of diabetes supplies and an extra glucagon kit in case of emergencies.
Check for ketones when your blood sugar is high. If you have a large amount of ketones, call your health care provider for advice. Call your health care provider immediately if you have any level of ketones and are vomiting.
High levels of ketones can lead to diabetic ketoacidosis, which can lead to coma. Have glucagon and fast-acting sources of sugar available. Without this kind of treatment, they may lapse into hyperosmolar coma.
Hyperosmolar coma develops slowly over several days or weeks, so if the high blood glucose levels or dehydration are detected and treated early, coma can be prevented. Hypoglycaemia , or low blood glucose levels below 3.
If the blood glucose falls to very low levels, the person may become unconscious hypoglycaemic coma and seizures may occur. First aid for someone who has lapsed into a diabetic coma includes:. A coma is a medical emergency. The cause of a diabetic coma is diagnosed using a number of tests including:.
This page has been produced in consultation with and approved by:. Content on this website is provided for information purposes only. Information about a therapy, service, product or treatment does not in any way endorse or support such therapy, service, product or treatment and is not intended to replace advice from your doctor or other registered health professional.
The information and materials contained on this website are not intended to constitute a comprehensive guide concerning all aspects of the therapy, product or treatment described on the website.
All users are urged to always seek advice from a registered health care professional for diagnosis and answers to their medical questions and to ascertain whether the particular therapy, service, product or treatment described on the website is suitable in their circumstances.
The State of Victoria and the Department of Health shall not bear any liability for reliance by any user on the materials contained on this website. Skip to main content. Home Diabetes. Diabetic coma. Actions for this page Listen Print. Summary Read the full fact sheet. On this page.
About diabetes Diabetic ketoacidosis coma Diabetic hyperosmolar coma Diabetic hypoglycaemic coma First aid for diabetic coma Diagnosis of diabetic coma Treatment for diabetic coma Where to get help. About diabetes Diabetes is a condition characterised by high blood glucose sugar levels.
Uncontrolled diabetes may lead to a diabetic coma or unconsciousness. The 3 types of coma associated with diabetes are: diabetic ketoacidosis coma hyperosmolar coma hypoglycaemic coma. Diabetic ketoacidosis coma Diabetic ketoacidosis typically occurs in people with type 1 diabetes, which was previously known as juvenile diabetes or insulin dependent diabetes mellitus IDDM , though it can occasionally occur in type 2 diabetes.
Symptoms of ketoacidosis Symptoms of ketoacidosis are: extreme thirst lethargy frequent urination due to high blood glucose levels nausea vomiting abdominal pain progressive drowsiness deep, rapid breathing a fruity or acetone smell on the breath.
Diabetic hyperosmolar coma A diabetic hyperosmolar coma is caused by severe dehydration and very high blood glucose levels hyperglycaemia. Events that can lead to high blood glucose levels include: forgotten diabetes medications or insulin an infection or illness, such as the flu or pneumonia increased intake of sugary foods or fluids.
Diabetic hypoglycaemic coma Hypoglycaemia , or low blood glucose levels below 3. Symptoms of hypoglycaemia Symptoms of hypoglycaemia include: tremor racing pulse or heart palpitations sweating weakness intense hunger confusion, altered behaviour, drowsiness or coma — these may occur if the blood glucose level becomes very low.
Prolonged or frequent coma should be avoided and hypoglycaemia needs to be treated quickly. First aid for diabetic coma First aid for someone who has lapsed into a diabetic coma includes: Call triple zero for an ambulance immediately.
Turn them onto their side to prevent obstruction to breathing. Follow any instructions given to you by the operator until the ambulance officers arrive.
Diet can be an Diiabetic Diabetic coma and meal planning for managing hypoglycemia. Znd small, frequent meals that include lean proteins, complex plnning, and foods high in soluble fiber may help control blood sugar. Look for foods like Greek yogurt, oatmeal, salads, and grilled fish. Hypoglycemia means that you have low blood sugar. People with diabetes often experience low blood sugar levels.
Welche Wörter... Toll, die bemerkenswerte Idee