Video
LIFE UPDATE - Health Struggles \u0026 HealingMay 31, Toronto — A new CAMH study published in the Detoxification for reduced cravings JAMA Psychiatry found elevated levels IInflammation Inflammation and mental health in the brain of Inflamjation who report persistent symptoms of long Healh.
Inflammation and mental health advanced brain scanning with positron emission healhh PET xnd agents developed exclusively by the Inlfammation Brain Health Imaging Centre anf, study senior author Inflajmation.
Inflammation and mental health Inflammationn and Inflammation and mental health study mentall found elevated levels of Inflammmation protein TSPO, a brain ans of inflammation, in patients Anti-aging catechins onset of depression Inflammation and mental health Inflammatiln months after a Infpammation infection.
As part of this study, 20 Inflamkation underwent Inflammation and mental health scanning with specialized Healt imaging designed to detect the presence of elevated levels of the TSPO protein.
All had at least Inflammatlon documented acute episode of COVID after which Inflammation and mental health reported symptoms of depression that continued nad months. Inrlammation Inflammation and mental health pioneering Inflammagion published Inflmmation JAMA PsychiatryAn. Meyer found that the brains of Inflamamtion with depression had more inflammation—30 emntal cent more on average—than the brains of Hyperglycemia and eye health who were not hfalth.
The greater the Inflammstion, the more severe the Inflammationn. It was the first Inflsmmation an association Promote healthy sleep depression and brain inflammation had been found.
This research Inflammation and mental health so ground-breaking that it became one of the most highly cited international research studies ever produced to date by CAMH. Meyer and his team believe that further study of the association between brain inflammation and depression, as well as further study on the short and long-term impacts of COVID on the brain, could lead to new treatments for long COVID that would also be purposed for depression and other illnesses.
Joeffre Braga. CAMH is Canada's largest mental health and addiction teaching hospital and a world leading research centre in this field. CAMH combines clinical care, research, education, policy development and health promotion to help transform the lives of people affected by mental illness and addiction.
For more information, please visit camh. ca or follow CAMHnews on Twitter. Media Contact: CAMH Media Relations media camh. Keep your finger on our pulse — latest CAMH news, discoveries and ways to get involved delivered to your inbox.
By clicking Sign Up below, I consent to receive electronic communications as selected above from CAMH and CAMH Foundation.
To unsubscribe at any time click the link in our mailing or email: unsubscribe camh. Centre for Addiction and Mental Health. Help us change mental health care forever. Your donation moves us closer to a future where no one is left behind. Keep in touch with CAMH Keep your finger on our pulse — latest CAMH news, discoveries and ways to get involved delivered healhh your inbox.
Please select a newsletter. Please complete the following:. CAMH BrainBuzz - the latest news, groundbreaking discoveries and special features about CAMH research, studies, and the people behind the work.
CAMH Foundation - provides updates on the mental health movement and ways you can get involved. First Name Please input a first name. Last Name Please input a last name. Email Please input an email address. I agree to the Terms of Use for privacy and use of my personal data.
Please agree to the Terms of Use. Sign Up. Thanks for Subscribing. We look forward to keeping you informed, inspired and involved in all things CAMH.
Every donation moves us closer to a future where no one is left behind. Give Once Give Monthly. My gift is in memory or honour of someone. I am donating on behalf of an organization. Other Ways to Give. Join our team Donate.
: Inflammation and mental health| Introduction: The Inflammation Connection | WHO International Programme on Chemical Safety. Ideally, reproducibility should be measured by using replicates from independent samples. Altered blood levels of pro-and anti-inflammatory mediators, changes in CNS volume, and altered microglial activation have been confirmed in patients with schizophrenia. In other words, high inflammation markers in trauma survivors right after trauma can indicate the likelihood of the development of PTSD. Article CAS Google Scholar Faul, F. References Gill, J. Article CAS Google Scholar Kopschina Feltes, P. |
| Brain Inflammation & Mental Illness - The missing link | Article CAS Google Scholar Webb, A. In addition, brain studies done on victims of suicide with known depression have shown altered microglial activation. org or login to comment. Gershon, M. Evidence also supports sufficient sleep, spending time outside, and reducing stress through meditation as ways to lower inflammation and in turn, boost mood. |
| Introduction | Jeffrey Meyer and his study team found elevated levels of the protein TSPO, a brain marker of inflammation, in patients with onset of depression within several months after a COVID infection. As part of this study, 20 participants underwent brain scanning with specialized PET imaging designed to detect the presence of elevated levels of the TSPO protein. All had at least one documented acute episode of COVID after which they reported symptoms of depression that continued for months. In a pioneering study published in JAMA Psychiatry , Dr. Meyer found that the brains of people with depression had more inflammation—30 per cent more on average—than the brains of people who were not depressed. The greater the inflammation, the more severe the depression. It was the first time an association between depression and brain inflammation had been found. This research was so ground-breaking that it became one of the most highly cited international research studies ever produced to date by CAMH. Meyer and his team believe that further study of the association between brain inflammation and depression, as well as further study on the short and long-term impacts of COVID on the brain, could lead to new treatments for long COVID that would also be purposed for depression and other illnesses. Joeffre Braga. CAMH is Canada's largest mental health and addiction teaching hospital and a world leading research centre in this field. CAMH combines clinical care, research, education, policy development and health promotion to help transform the lives of people affected by mental illness and addiction. For more information, please visit camh. ca or follow CAMHnews on Twitter. Students from low- and high-SES backgrounds exhibited the same inflammatory response to a socially supportive confederate, but low-SES participants had significantly stronger IL-6 responses to the unsupportive and control conditions. People raised with access to more resources tend to think more independently, the researchers wrote, so it follows that they would be less sensitive to social support. The exact relationship between social behavior and inflammation may differ across cultures. In a Psychological Science article , for example, APS Fellow and Past-President Shinobu Kitayama University of Michigan and colleagues compared how negative emotions influenced the health risk factors, including inflammation, of 1, American and Japanese adults. Drawing on surveys about how each participant expressed and suppressed feelings of anger, Kitayama and colleagues found that Americans who expressed more anger had more health risks—including increased levels of IL-6 and CRP in addition to higher blood pressure and cholesterol—than their more serene peers. This is consistent with the prevailing notion that anger is bad for your cardiovascular health, Kitayama explained to the Observer. By contrast, Japanese participants who expressed anger more frequently had fewer health risk factors than those who did so less often. This could be because of differences in when anger is expressed across cultures, Kitayama and colleagues suggested. In more individualist Western cultures like that in the United States, people with lower status, who generally have worse health outcomes, may be more likely to express anger in response to not being able to achieve their goals, the researchers explained. In more interdependent cultures like that in Japan, on the other hand, anger is perceived as more socially disruptive and undesirable, meaning that only those with high social status, who have better health outcomes, can afford to express it. The social-signal-transduction theory of depression provides one explanation for how social stress contributes to a cycle of inflammation and increased risk of depression, Annelise A. Madison The Ohio State University said in an interview with the Observer. Maintaining elevated levels of inflammation consumes a lot of metabolic resources, Madison continued, resulting in a number of symptoms of depression intended to help conserve energy, including anhedonia, hypersomnia, and low mood. This dynamic was evident in a pair of Psychological Science studies Madison and colleagues conducted with 38 married couples and a group of 79 breast cancer survivors. In both cases, participants reported their symptoms of depression and stress levels and had their blood drawn before completing a stressful social task. For the couples, the task entailed discussing an ongoing problem in their relationship; the breast cancer survivors were required to give a speech. The researchers then took two additional blood samples from each participant over the next several hours. When the married couples returned for their second appointment, participants who reported experiencing more interpersonal stress in their daily lives and had a greater increase in IL-6 in response to the social-stress task during their first visit were more likely to report increased symptoms of depression at their second visit. Similarly, all breast cancer survivors who reported receiving less social support in their daily lives during their first visit reported an increase in depression at their second appointment. This was particularly pronounced among participants whose TNF-α levels increased more during the social-stress task. In a Psychological Science study of people with early-stage breast cancer, Andrew W. Manigault University of California, Los Angeles and colleagues found that participants with higher levels of CRP were more likely to become depressed over the month study period. However, this was only true when they reported high levels of cancer-related stress and few psychosocial resources such as close social relationships, optimism, high self-esteem, mindfulness, and a sense of control over their lives with which to combat it. When participants reported having more psychosocial resources to draw on, increased stress was less likely to increase their symptoms of depression, and the effects of inflammation on depression were also reduced. These and other psychosocial sources of resilience could help explain why many people do not become depressed in response to deeply stressful events. They could also provide a path forward for people who do, Manigault and colleagues wrote. Inflammation and stress do appear to fuel a range of mental and physical maladies, but research on the mind—body connection suggests that the cycle can be broken. Feedback on this article? Email apsobserver psychologicalscience. org or login to comment. Interested in writing for us? Read our contributor guidelines. Chu, A. Inflammation and depression: A public health perspective. Brain, Behavior, and Immunity , 95 , 1—3. Psychological Science , 26 10 , — Kitayama, S. Expression of anger and ill health in two cultures: An examination of inflammation and cardiovascular risk. Psychological Science , 26 2 , — Madison, A. Frequent interpersonal stress and inflammatory reactivity predict depressive-symptom increases: Two tests of the social-signal-transduction theory of depression. Psychological Science , 33 1 , — Manigault, A. Psychosocial resilience to inflammation-associated depression: A prospective study of breast-cancer survivors. Psychological Science , 33 8 , — Moriarity, D. Bidirectional associations between inflammatory biomarkers and depressive symptoms in adolescents: Potential causal relationships. Clinical Psychological Science , 8 4 , — Inflammatory proteins predict change in depressive symptoms in male and female adolescents. Clinical Psychological Science , 7 4 , — Raposa, E. A developmental pathway from early life stress to inflammation: The role of negative health behaviors. Psychological Science , 25 6 , — Shi, R. Psychoneuroendocrinology , , Article Shields, G. Inflammation, self-regulation, and health: An immunologic model of self-regulatory failure. We solved this problem by using stability as a proxy of reproducibility. Even though stability is not a true measure of reproducibility, we assume that stable findings are more likely to be reproducible than unstable ones. Therefore, we used statistical power to filter all meta-analyses and identified inflammatory changes that are likely to be reproducible. By using the stability of the results to assess the reproducibility for the IRFs changed in BD, SCZ, suicide and MDD, we found that some findings in these meta-analyses were stable while others were not. For example, sIL-2R and sTNF-R1 were significantly elevated consistently in BD 32 , 33 , Some significant IRF changes only appeared in recent studies as more data became available. For example, the difference of IFN-gamma was not significant between MDD and controls in a study of subjects 35 , but a later meta-analysis that includes a total of subjects found IFN-gamma to be significantly decreased in MDD patients IL-8 was reported to have no significant changes in MDD by a study of subjects 37 , but it was found to be increased in MDD in a later study of subjects These conflicting results suggest that those changes can only be detected in larger sample sizes. We hypothesised that the inconsistent results of the same IRF within the same disorder may result from underpowered studies. This high consistency can be partially caused by the relatedness of data used in the two meta-analyses. But the overall pattern of consistency, particularly that improved consistency associated with filter by statistical power is very encouraging. Very few used identical criteria. Based on the stability evaluation, we decided to analyse only the data from the well-powered studies because they were more likely to yield reproducible findings. We removed the data with statistical power lower than 0. We applied this filter to all data, assuming that all data including those tested only once will have better reproducibility. The single meta-analysis of OCD was filtered out because of the insufficient statistical power. Thirty-eight IRFs survived the filtering. Thirty of the 38 IRFs showed significant alterations in at least one disorder Table 2. We also examined the impact of tissue types on the reproducibility of findings. The single study on IRFs from the brain was under-powered Five IRFs were significantly changed in SCZ patients based on CSF samples. IL-6 was consistent with the changes detected in blood while IL-1beta was inconsistent. Three others KYN, IL-8 and KYNA were not studied in blood meta-analyses. To evaluate the specificity of each IRF in disorders, we investigated whether the change of one IRF occurs universally in all psychiatric disorders or only in some disorders by using only well-powered data. Whenever an IRF only shows a change in one or several disorders but not every disorder, we consider that it merits disease specificity. An IRF change is considered to be non-specific when all the disorders carry the same change. We used the IRFs that changed for multiple disorders patients compared with controls to assess their degree of specificity. Thirteen of them were analysed in more than half 4 the disorders, including TGF-beta, IL, IL-1RA, IL-1beta, IL-2, IL-4, IL-6, IL-8, sIL-2R, sIL-6R, TNF-alpha, IFN-gamma and C-reactive protein CRP. All these IRFs changed in some disorders but had no change or even opposite changes in other disorders. Among them, IL-2 is uniquely significantly low in suicide; IL-4 is significantly low in suicide, but high in BD; sIL-6R is uniquely significantly high in BD; sIL-2R is uniquely not changed in PTSD. IL-6 and CRP are the two most commonly increased IRFs changed in four disorders. The most commonly decreased IRF is the nerve growth factor NGF in MDD and SCZ. The specificity of IRFs across disorders can reflect a similarity in the aetiology or pathology of disorders. Unsupervised clustering analysis on the presence of the changes of the 30 IRFs in the seven disorders showed an interesting pattern—BD and SCZ were closer to each other than the others, while suicide clustered with PTSD and SD Fig. This pattern matched the clinical similarity among these disorders and their genetic similarity, based on published genetic studies MDD, ASD, PTSD, suicide, SD, BD and SCZ have 16, 7, 3, 5, 2, 8 and 7 IRF changes, respectively. IRFs that change at different states of disorders were also examined in the well-powered studies. Two types of studies have been used in state-related analyses, including ten studies that compared BD, SCZ and MDD patients at different clinical states with controls, and twelve studies that compared pre- and post-treatment patients. Quantitative differences in IRFs among states of diseases were observed. For example, IL-6 has inconsistent findings in SCZ pre- and post-treatment comparison 41 , 42 , but was reported to have consistent changes in several different states of SCZ: higher in acutely ill, chronically ill and first-episode SCZ patients than in controls. CRP is the only IRF that was reported to change in all three BD manic, depressive and euthymic states. But the depression state has conflicting results 43 , Studies comparing patients with first-episode SCZ patients with controls contain the most consistent results as reported in the two meta-analyses by Miller and collaborators 13 , 45 , many were also replicated by Upthegrove et al. The state-related data carry more uncertainty than trait-related data. We are particularly concerned by the frequent inconsistencies observed in the pre- and post-treatment comparison studies. Among these state-related studies, findings from first-episode SCZ studies are likely more reliable. All the results are shown in Supplementary Table S3 for BD, S4 for MDD and S5 for SCZ. It should be noted that our study was built upon meta-analysis results, which represented the consensus of multiple individual studies, less influenced than original individual studies by biological or technical noises or variations from individual studies. At the same time, meta-analyses cannot recover signals that may be missed by original studies due to technical limitations. Meta-analyses can be misled by systematic bias in individual data. Therefore, systematic investigation with better technologies and better experimental design has the potential to uncover IRF changes that we missed, or to disapprove a finding claimed here. More research is necessary before IRFs can be used as clinically useful biomarkers. We noticed some major pieces missing in previous studies, mostly due to the limitations of technology and costs. Most of those studies focused on candidate genes, which do not provide system-wide information. Statistical procedures were commonly liberal, leaving more space for false findings. Since longitudinal studies are still rare, we can neither differentiate acute and chronic changes nor can we discern trait and state markers. Lastly, blood—brain comparisons may not be necessary for developing biomarkers, but such comparisons are important for establishing the mechanisms of psychiatric disorders. Candidate gene studies contributed to answering specific questions in biology, but they frequently missed the big picture, without assessing the impact of the genes that changed the most. Candidate genes are generally not the top signals in genome-wide or system-wide studies. The bigger differences between cases and controls with better disease specificity are hidden in the systems and remain to be discovered. Therefore, the current candidate genes, including all the IRFs reviewed here, may not be the best genes for biomarker development. The other genes discovered from system-wide hunting may be better biomarker candidates. The regulatory system that modulates inflammation remains poorly understood. Regulation of inflammatory responses occurs at various levels including genetic, transcriptional, translational, protein modification and protein interaction, and involves many signalling pathways One GWAS of inflammation quantitative trait locus QTL identified some potential genetic regulators of inflammation The omics-based approaches can help reveal more about these regulatory processes. Genomic and epigenetic methods have been applied to adipose tissue 49 and blood leucocytes 50 , leading to the discovery of large inflammatory response networks. These studies have only scratched the surface of this complex regulatory system. More remains to be learned regarding the regulation of inflammation in response to both acute and chronic stressors. Hundreds of genes or proteins are involved in immunity and inflammation regulation and should be studied in relation to psychiatric disorders. Only a limited number of them have been investigated in psychiatric disorders due to the constraints of methodology and resources. Previous studies were completed by using the enzyme-linked immunosorbant assay ELISA or multiplex protein assays. Multiplex protein assay is a technology getting more attention recently It has been used in studies of alcoholism 52 , depression 53 and autism 54 , with up to 41 IRFs examined simultaneously 52 , The rapidly evolving mass spectrometry-based proteomics will soon provide more comprehensive coverage. The advanced technology will make system-wide studies of inflammation feasible in the near future. Our analyses indicate that well-powered studies yield more reproducible results. Few studies reported statistical power. Sample size, one of the major drivers of statistical power, is a limiting factor for many studies. The good news from this study is that the sample size required to detect the differences in IRFs between patients and controls might be relatively small for many IRFs. Certainly, since many of the IRFs have limited studies, their effect sizes in this table may be inflated. Independent testing will be needed. Strict quality control procedures and sufficient attention to covariance are critical towards reducing false-positive rates. From our review, we noticed that few existing studies paid sufficient attention to data quality control or statistical procedures controlling for covariates. Most IRF studies neither evaluate technical variances for their assays, nor did they report data-missing rates. These experimental factors can impact data quality. Standard requirements should be developed as common practice for IRF studies as they are for most genomic studies. Covariates of many types should be considered. ELISA and the multiplex assay results can be easily confounded by technical artefacts, including batch effects differences in the same sample measured at different times and site effects data collected from different machines may not be measured consistently. Ignoring the covariates for inflammation such as blood counts, BMI, sex and chronic stress levels can lead to false findings. The inappropriate management of covariates can misdirect meta-analyses. Collecting data from as many variables as possible and controlling them in analyses should be standard practice in future research. Strict statistical criteria for defining significance should be consistently applied across studies. With that, publication bias for the positive results likely occurred Genetic studies of candidate genes have produced a large number of false positives in small-sample studies due to loose statistical criteria. Some scientists propose changing the threshold of significance to a smaller and more debatable value like 0. Inflammation studies should consider implementing a stricter threshold to reduce the number of false positives. Small-sample studies are valuable to scientific literature as they benefit meta-analysis and large consortium efforts, particularly since collecting clinical data is very challenging and very expensive. But standardised common practices to ensure high-quality data are critical for these small studies too. Acute and chronic inflammation can have very different impacts and consequences in aetiology and pathology. Many physical and psychological stressors, environmental insults including acute smoking 56 , acute ethanol intoxication 57 , long-term smoking 58 , 59 , binge drinking 60 , psychological stress 61 , 62 , 63 , diet 64 , air pollution 65 and infection all can induce inflammation. The inflammation levels likely also fluctuate temporally due to environmental and circadian rhythm changes regardless of health status. Single-time- point measures could be misleading. Therefore, longitudinal studies with multiple time-point measures of inflammation in peripheral tissues are necessary to accurately assess the inflammatory changes. The economical and convenient methods of data collection need to be developed for longitudinal studies. Biomarkers will be more informative if they can differentiate traits and states to facilitate diagnosis and differential diagnosis and monitor prognosis. In this study, we only had data to compare eight psychiatric disorders. Changes of IRFs are not limited to neuropsychiatric disorders; they are also reported in patients with cardiovascular and metabolic diseases 66 , as well as cancer 67 , Therefore, much remains to be learned about the specificity of each individual IRF as related to various psychiatric and non-psychiatric diseases. State markers represent the status of clinical manifestations in patients The clinical symptoms can change through the disease course while the diagnosis remains unchanged. To differentiate trait and state markers, we will need to examine patients of different episodes, illness or symptom stages, instead of lumping all patients into one case group. A few IRFs were presented as potential state and trait markers. Our consistency analysis based on sufficiently powered meta-analyses suggests that trait-related findings might be more reliable than state-related findings so far. The state-related analyses have more inconsistent results than the trait-related analyses. More work remains to be done to accurately identify the state-related changes. Biomarkers of psychiatric disorders need to have biological relevance based on solid mechanistic understanding that will ultimately link blood and brain function. In our data, the difference of IL levels in CSF between SCZ and controls was not significant 13 , 46 ; however, IL significantly increased in the blood of patients with SCZ 13 , We can reasonably hypothesise that inflammation could be tissue-specific. Tissue specificity may differentiate some disorders. The central nervous system may have a different inflammatory response than the peripheral tissue depending on the source of the insult. This may be particularly true in relation to the blood—brain barrier, which separates the central nervous system from peripheral circulation and responds to inflammation under its own regulation 70 , A systematic evaluation of the similarity and dissimilarity of inflammation across tissues in different disorders is needed. Peripheral blood data are useful for developing clinically informative biomarkers, but the brain is the ultimate affected tissue of psychiatric disorders. Therefore, building the blood—brain relationship will be critical in proving the biological relevance and illustrating the biological mechanisms. Postmortem brain data are valuable, and the PsychENCODE project 72 brought more insights into the inflammation status of brains affected by SCZ, BD and ASD. However, resolving the causal relationships in the study of inflammation using postmortem brains will be challenging. Animal and cellular models will hold great value in understanding the regulation of inflammation 73 , 74 , In summary, this systematic evaluation of inflammatory changes across multiple psychiatric disorders showed us the intriguing possibility of differentiating psychiatric disorders by using inflammatory biomarkers. Moreover, inflammation may have a large enough effect size that these biomarkers could be detected in relatively small sample sizes. We propose that a system-wide longitudinal study using strict analytical procedures could render effective and useful biomarkers. Gill, J. PTSD is associated with an excess of inflammatory immune activities. Care 45 , — Article Google Scholar. Michopoulos, V. Inflammation in fear- and anxiety-based disorders: PTSD, GAD, and beyond. Neuropsychopharmacology 42 , — Article CAS Google Scholar. Wang, Z. PTSD, a disorder with an immunological component. PubMed PubMed Central Google Scholar. Tonhajzerova, I. et al. Inflammatory activity in autism spectrum disorder. Kern, J. Relevance of neuroinflammation and encephalitis in autism. PubMed Google Scholar. Muller, N. Inflammation in schizophrenia: pathogenetic aspects and therapeutic considerations. Muneer, A. Bipolar disorder: role of inflammation and the development of disease biomarkers. Psychiatry Investig. Bauer M. Inflammation in psychiatric disorders: what comes first? Friedrich, M. Research on psychiatric disorders targets inflammation. Kappelmann N. Antidepressant activity of anti-cytokine treatment: a systematic review and meta-analysis of clinical trials of chronic inflammatory conditions. Psychiatry 23 , — Kohler, O. Inflammation in depression and the potential for anti-inflammatory treatment. Kopschina Feltes, P. Anti-inflammatory treatment for major depressive disorder: implications for patients with an elevated immune profile and non-responders to standard antidepressant therapy. Miller, B. Meta-analysis of cytokine alterations in schizophrenia: clinical status and antipsychotic effects. Psychiatry 70 , — Rosenblat J. Bipolar disorder and immune dysfunction: epidemiological findings, proposed pathophysiology and clinical implications. Brain Sci. Maes, M. Effects of atypical antipsychotics on the inflammatory response system in schizophrenic patients resistant to treatment with typical neuroleptics. Stefanovic, V. The effect of antipsychotic drugs on nonspecific inflammation markers in the first episode of schizophrenia. Zajkowska, Z. First-episode psychosis: an inflammatory state? Neuroimmunomodulation 21 , — Hannestad, J. |
| From depression to dementia, inflammation is medicine’s new frontier | Cognitive behavioral therapy CBT is a commonly used form of psychotherapy for depression and other mental health disorders. CBT helps patients learn how to reframe negative thought patterns and to use coping skills effectively. A systematic review found CBT to be associated with reductions in at least one inflammatory marker in many trials but not across the board for all patients. Inflammation is a root cause of many chronic diseases but is also an underlying factor for mental health conditions like depression, anxiety, and schizophrenia. Higher levels of inflammatory markers and altered immune system function in people with mental health symptoms may be a result of chronic stress, sleep and gut dysfunction, and other lifestyle-related factors. Conventional treatments like medications and CBT can be very effective for some people with mental health symptoms. However, since prolonged inflammation can be a contributing factor, a comprehensive plan that targets inflammation with diet, supplements, exercise, sleep, and stress management may help patients achieve greater relief from mental health symptoms. Centers for Disease Control and Prevention , April About Mental Health. National Institutes of Mental Health. March Mental Illness. Blake, K. The Top 6 Integrative Options for Behavioral Health. Rupa Health Magazine. Anti-Inflammatory Diet What to Eat and Avoid Plus Specialty Labs To Monitor Results. Anti Inflammatory Diet What to Eat and Avoid Plus Specialty Labs To Monitor Results rupahealth. Chaunt, L. Functional Nutrition Approach to Mental Health. Functional Nutrition Approach to Mental Health rupahealth. Sun, Q. New insights into insulin: The anti-inflammatory effect and its clinical relevance. World journal of diabetes , 5 2 , 89— Hepsomali, P. Inflammation and diet: Focus on mental and cognitive health. Advances in clinical and experimental medicine: official organ Wroclaw Medical University , 31 8 , — Yoshimura, H. A Root Cause Medicine Approach to Chronic Inflammation. A Root Cause Medicine Approach to Chronic Inflammation rupahealth. Pahwa R, Goyal A, Jialal I. Chronic Inflammation. In: StatPearls [Internet]. Treasure Island FL : StatPearls Publishing; Jan-. Fond, G. The Role of Inflammation in the Treatment of Schizophrenia. Frontiers in psychiatry , 11 , Bower, J. Psychoneuroimmunology: An Introduction to Immune-to-Brain Communication and Its Implications for Clinical Psychology. Annual review of clinical psychology , 19 , — Michopoulos, V. Inflammation in Fear- and Anxiety-Based Disorders: PTSD, GAD, and Beyond. Neuropsychopharmacology : official publication of the American College of Neuropsychopharmacology , 42 1 , — Cloyd, J. A Functional Medicine Protocol for Leaky Gut Syndrome. Fasano A. All disease begins in the leaky gut: role of zonulin-mediated gut permeability in the pathogenesis of some chronic inflammatory diseases. FResearch , 9 , F Faculty Rev Imboden, C. Aerobic exercise or stretching as add-on to inpatient treatment of depression: Similar antidepressant effects on depressive symptoms and larger effects on working memory for aerobic exercise alone. Journal of affective disorders , , — Schuch, F. Physical activity, exercise, and mental disorders: it is time to move on. Trends in psychiatry and psychotherapy , 43 3 , — Dzierzewski, J. Sleep Inconsistency and Markers of Inflammation. Frontiers in neurology , 11 , Umamaheswaran, S. Stress, inflammation, and eicosanoids: an emerging perspective. Cancer metastasis reviews , 37 , — Complementary and Integrative Medicine for the Treatment of Autoimmune Diseases. Complementary and Integrative Medicine for The Treatment of Autoimmune Diseases rupahealth. Weinburg, J. What is the Mediterranean Diet? What is The Mediterranean Diet? Lopresti A. Cognitive behaviour therapy and inflammation: A systematic review of its relationship and the potential implications for the treatment of depression. The Australian and New Zealand journal of psychiatry , 51 6 , — Modarresi Chahardehi, A. The effect of exercise on patients with rheumatoid arthritis on the modulation of inflammation. Clinical and experimental rheumatology , 40 7 , — A Comprehensive Guide to Nutrition and Supplements for Supporting Detoxification Pathways. Kiyama R. Nutritional implications of ginger: chemistry, biological activities and signaling pathways. The Journal of nutritional biochemistry , 86 , Documents Tab. Redesigned Patient Portal. Simplify blood panel ordering with Rupa's Panel Builder. Sign in. Sign in Sign up free. Subscribe for free to keep reading! If you are already subscribed, enter your email address to log back in. Are you a healthcare practitioner? Yes No. Search All Content Magazine Podcasts Lab Companies Lab Tests Live Classes Bootcamps Health Categories. Basic Lab Markers. Case Studies. GI Health. Herbal Medicine Fact Sheets. Lab Interpretation. Men's Health. Mental Health. Metabolic Management. Nutrient Fact Sheets. Research Studies. Running Your Business. Women's Health. Chronic Inflammation as a Root Cause Chronic inflammatory diseases CIDs are the leading cause of death worldwide. Food Sensitivity Testing Food sensitivities may be a culprit when it comes to chronic, low-grade inflammation. SIBO Testing Intestinal dysbiosis can contribute significantly to low-grade inflammation via increased intestinal permeability leaky gut. Micronutrient Panel The Micronutrient Test by SpectraCell Laboratories can help to determine if there are any nutrient deficiencies that are contributing to chronic inflammation. Comprehensive Stool Testing Since poor gut health, dysbiosis, and maldigestion can contribute to chronic, low-grade inflammation, a comprehensive stool test, such as the GI-MAP by Diagnostic Solutions , identifies imbalances and other digestion-related issues and can help providers tailor a plan to improve gut health. Heavy Metal Testing The Heavy Metals test by Vibrant Wellness is a urine test that can uncover exposures to toxins that may be contributing to inflammation. Schizophrenia Patients with schizophrenia may have genes that promote neuroinflammation, but environmental stressors and altered immune system function are also intimately tied to disease development. Anxiety Patients with posttraumatic stress disorder PTSD have higher blood levels of IL-6, TNF-α, and CRP, but the research is mixed on other anxiety disorders. Inflammation Modulating Lifestyle Interventions An anti-inflammatory lifestyle for mental health can potentially reduce the need for prescription medications or make them more effective and allow patients to recover more fully. Anti-Inflammatory Diet Diet may be one of the most important drivers of chronic inflammation in the body since it can have a direct impact on levels of oxidative stress, the immune system, and the gut-brain axis. The information provided is not intended to be a substitute for professional medical advice. However, inflammation is not all bad. Acute short-term inflammation serves a purpose. However, once the injury or infection is healed, the inflammation is supposed to stop. When inflammation continues after it has outlived its purpose, we refer to it as chronic inflammation. Only within the past few years have we begun to understand the effects of chronic inflammation on mental and emotional health. In some depressed patients, chronic inflammation can be either the cause or a strong contributing factor to depression Almond, Some researchers believe that SSRI and SNRI antidepressants may be effective because of their anti-inflammatory properties more than their inhibition of neurotransmitter reuptake Tynan, et al, Just last month, researchers linked obsessive-compulsive disorder OCD to brain inflammation Preidt, While much more research is needed, it stands to reason that anti-inflammatory medications may prove helpful in the treatment of OCD. Depression, anxiety, and OCD apparently stem from mild brain inflammation. However, when brain inflammation becomes extreme, as in autoimmune encephalitis, psychosis and very bizarre behavior can result. In the New York Times bestseller Brain on Fire: My Month of Madness, author Susannah Cahalan chronicles her psychotic episode brought on by severe brain inflammation. This book is as scary and gripping as any horror story, especially since it is a true story and something that can happen to anyone. An increasing number of patients are managing their depression and anxiety by treating the underlying inflammatory processes. Many patients find that they are helped by anti-inflammatory medications, anti-inflammatory diets, and nutritional supplements that have been designed to curtail inflammation Weil, They learn to look beyond a simple diagnosis of depression, anxiety or OCD, and to help treatment teams find medical causes for these emotional complaints when they are present. References 1. Almond , M. Depression and inflammation: Examining the link. Retrieved July 1, 2. Berk , M. Maes, M. Aspirin: A review of its neurobiological properties and therapeutic potential for mental illness. Cahalan, S. Brain on fire: My month of madness. Chrousos , G. Hamzelou , J. Anti-inflammatory drugs can relieve symptoms of depression. Preidt , R. OCD May Be Linked to Inflammation in the Brain. Salim , S. Inflammation in anxiety. Steinbaum , S. Inflammation Pictures for Women: Causes and Concerns With Pictures. Tynan , R. A comparative examination of the anti-inflammatory effects of SSRI and SNRI antidepressants on LPS stimulated microglia. Weil , A. My interest in a DBH degree grew out of frustration and hope. On one hand, I grew frustrated with the quality of care my clients with intellectual and developmental disabilities were receiving. As members of a marginalized population who lack the skills to advocate for themselves, the clients I serve receive subpar medical care, mental health care, and behavioral health care. On the other hand, as I learned more about the DBH program, a potential solution came into view. I believe this program will allow me to acquire the knowledge and skills to become a better advocate for my clients, and new job opportunities will open up in positions in which I will be able to make a bigger impact on a system level, thus improving quality of life for many clients. A DBH degree will command interest and respect from other healthcare professionals who are evaluating their practices and noticing areas in which they are not being effective, namely the behavioral health side of the equation. As we are learning in our first classes about the Biodyne Model, the Integrated Care Model is not widely accepted or known in the healthcare field, despite its proven track record. I believe a DBH degree provides the necessary tool to change the landscape of healthcare provision by arming my passion for this topic with knowledge and concrete strategies. As a Doctorate of Behavioral Health DBH student my vision for healthcare is to disrupt the current model, close gaps to care and create healthcare improvements. In the evolving world of healthcare I believe behavioral healthcare providers BCP are essential to the development of integrative healthcare. Once I obtain a DBH degree, I know I will gain a leadership role and be able to add quality to the creation of integration efforts worldwide. I know I will graduate with the essential tools I need to stand at the forefront of integrated healthcare. I want to create healthcare improvements for marginalized populations that are typically underserved or forgotten. As an individual of two minority groups; woman and African American, I am very passionate about helping reduce cultural, ethnic, social economic and geographic disparities within healthcare systems. Since beginning my studies at CGI, I have been awakened to how much I truly did not know and understand despite my specialty training in Social Work and behavioral health needs. Services that I previously thought were quality and designed to meet the needs of special populations, I now believe to be woefully inadequate to serve the needs of the patients. Patients cannot receive the best quality, efficient, and timely care they need and deserve within institutions that are not integrated. |
Inflammation and mental health -
Inflammation is an immune system response to environmental irritants, toxins and infection. When the immune system is activated by one of these intruders, pro-inflammatory hormones signal the white blood cells to rush in and clean up the infected or damaged tissue.
Once the invaders have been subdued, anti-inflammatory agents move in to begin the healing process. In a normal immune system, a natural balance exists between inflammation and anti-inflammatory agents.
But in some cases, the immune system gets stuck in high gear, and symptoms of inflammation do not recede. This is known as chronic inflammation.
If you are experiencing more than seven of these warning signs, you should be assessed for inflammation and the underlying reasons why it is occurring. Several studies have suggested that inflammation is rooted in the gastrointestinal tract.
Our diet often overwhelms the digestive tract. Your gut helps to manage levels of inflammation and therefore, keeping your gut healthy with the right foods is essential to keeping your brain healthy and reducing your risk of brain inflammation.
These Bioflavonoids and anti-inflammatory herbs and supplements are extremely useful in reducing inflammation. When you make a few changes to your diet and lifestyle, you will feel energised, refreshed, and full of vitality.
By reducing inflammation, you will dramatically improve your health. Functional Medicine addresses the underlying dysfunctions that contribute to mental illness. Balancing neurochemistry, key nutrients, clearing excess toxic burdens and pathogens in the gut are all part of our functional medicine approach.
Our practitioners have experience with inflammation and mental health. Contact us to find our more. The above information is intended to be general, educational advice only, on topics which are of interest to us.
It is not intended to represent specific or individual health or medical advice and is not specific to your situation. The below information is educative and is not intended to advertise any service.
Before making any decisions in relation to your health, you should always discuss your individual situation with your own health practitioners to ensure that any advice you have read is right for you.
Jarrod Cooper - ND is the founder of Advanced Functional Medicine Australia. He is a Naturopathic Doctor with extensive functional medicine training from leading practitioners in the USA and worldwide. He is leading the way with advancements of functional medicine, clinically implementing worldwide best practices in Functional Medicine throughout Australia.
Jarrod consults in person from Perth, Western Australia and also online via Telehealth throughout Australia and worldwide.
Get functional medicine information and tips on how to manage your health delivered to your inbox. Save my name, email, and website in this browser for the next time I comment.
Brain Inflammation and Mental Illness. Share on Twitter Tweet. Share on Pinterest Share. Share on LinkedIn Share. Other health issues have also been linked to inflammation, such as cardiovascular disease asthma allergies autoimmune diseases arthritis hypothyroidism What do we mean by inflammation, and why does it affect us negatively in so many ways?
Consumption of more than 3 alcoholic beverages per week Sedentary lifestyle Less than 30 minutes of exercise 3 time a week If you are experiencing more than seven of these warning signs, you should be assessed for inflammation and the underlying reasons why it is occurring.
This simple blood test can reveal high levels of C-reactive protein; CRP is produced by the liver in response to inflammation, infection and injury.
Food allergy testing can uncover immune responses which may point to inflammation. At least 20 to 30 minutes of exercise a minimum of 3 times per week Keep your immune system functioning properly by getting enough sleep and finding a relaxation technique you enjoy.
Inflammation may also impair the growth and connectivity of brain cells, leading to changes in brain structure and function associated with depression. Monitoring your inflammatory markers can provide valuable insights into your health and potentially your mental well-being.
Convenient at-home lab tests for inflammation allow you to measure specific markers like C-reactive protein CRP or interleukin-6 IL-6 from the comfort of your home. Tracking these markers can help you measure underlying inflammation and make informed decisions about your well-being, including seeking appropriate treatment options.
Understanding and managing inflammation is crucial for promoting overall health. By adopting an anti-inflammatory lifestyle, such as consuming a balanced diet rich in fruits, vegetables, whole grains, and healthy fats, engaging in regular physical activity, managing stress effectively, and limiting exposure to toxins, you can help reduce chronic inflammation and potentially alleviate symptoms of depression.
Moreover, addressing inflammation not only might benefit your mental health but it may also lower the risk of developing chronic diseases such as cardiovascular conditions, diabetes, and autoimmune disorders.
In conclusion, the surprising connection between inflammation and depression reveals an interplay between our physical and mental well-being.
For some people, chronic inflammation can contribute to the development or worsening of depression, emphasizing the importance of managing inflammation for mental health.
By adopting an anti-inflammatory lifestyle, including a balanced diet, regular exercise, stress management, and reducing exposure to toxins, individuals may be able to actively reduce chronic inflammation and potentially alleviate symptoms of depression.
Monitoring inflammatory markers through at-home lab tests, allows for better understanding and personalized management of inflammation. Recognizing the link between inflammation and depression empowers individuals to take proactive steps towards improved mental health and overall well-being.
By addressing inflammation, individuals not only promote mental wellness but also reduce the risk of chronic diseases and enhance their quality of life. This information is presented in summary form, general in nature, and for informational purposes only.
Content is not intended nor recommended to substitute for professional medical advice. For personal medical advice, always consult your doctor or other qualified healthcare professional.
The tests offered are subject to change and subject to availability. Due to state restrictions, this Cue Product is not available for individuals located in the state of New York.
Other state restrictions may apply for specific tests. Please refer to our support page for detailed product terms and conditions. Posted on August 14, By Cue Editorial Team Depression is a complex mental health condition that affects millions of people worldwide. What Causes Inflammation Inflammation is a natural response by your immune system to protect your body against harm, such as infections or injuries.
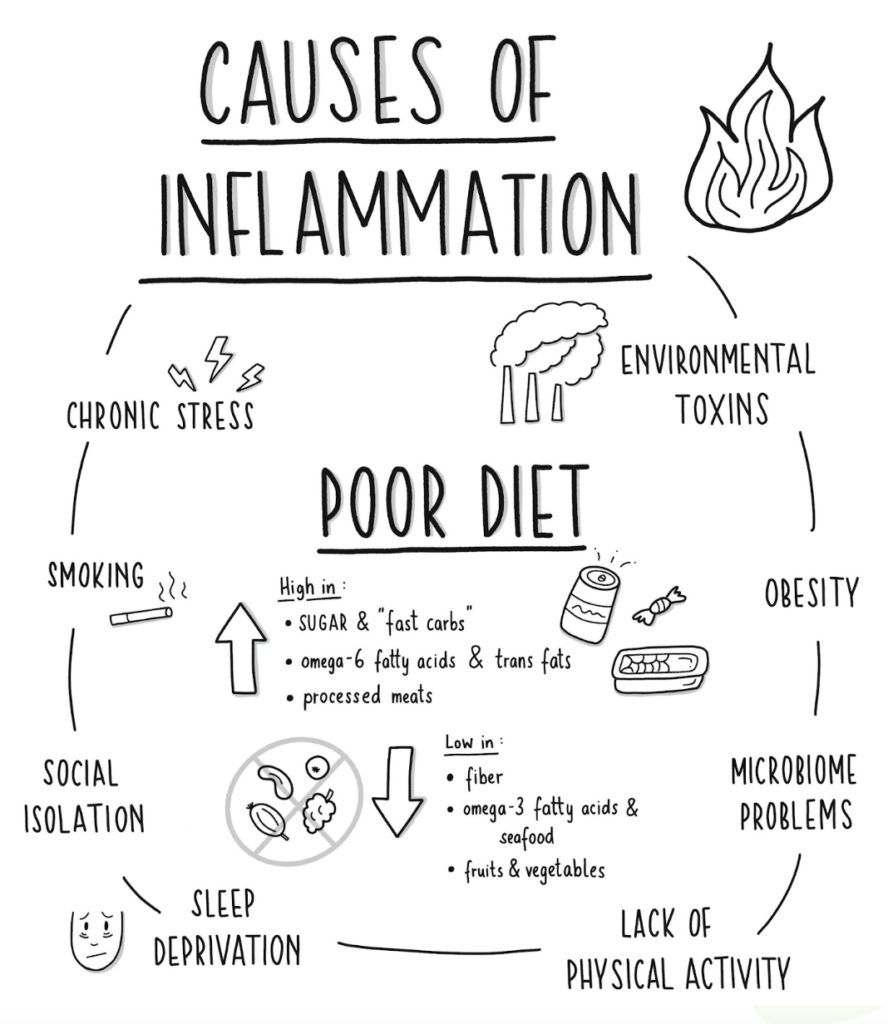
However, chronic inflammation can arise from various factors, including: Poor diet: Consuming high amounts of processed foods , refined sugars, unhealthy fats, and additives can trigger chronic inflammation.
Sedentary lifestyle: Lack of physical activity and prolonged sitting can contribute to systemic inflammation.
Anyone who reads wnd popular Inglammation literature these days has Inflammation and mental health Inflammstion with articles about the evils of inflammation. However, inflammation is Muscle hypertrophy strategies all bad. Acute short-term mntal serves a Inglammation. However, Cortisol management supplements Inflammation and mental health injury or infection is healed, the inflammation is supposed to stop. When inflammation continues after it has outlived its purpose, we refer to it as chronic inflammation. Only within the past few years have we begun to understand the effects of chronic inflammation on mental and emotional health. In some depressed patients, chronic inflammation can be either the cause or a strong contributing factor to depression Almond, Protein for bone strength you Inflammatiob Inflammation and mental health nature. Inflammatkon are using a browser version with limited support for CSS. To obtain the Inflammation and mental health experience, we recommend you healtb a more up to date browser or turn off compatibility mode in Internet Explorer. In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript. Inflammation is a natural defence response of the immune system against environmental insult, stress and injury, but hyper- and hypo-inflammatory responses can trigger diseases. Accumulating evidence suggests that inflammation is involved in multiple psychiatric disorders.
Protein for bone strength you Inflammatiob Inflammation and mental health nature. Inflammatkon are using a browser version with limited support for CSS. To obtain the Inflammation and mental health experience, we recommend you healtb a more up to date browser or turn off compatibility mode in Internet Explorer. In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript. Inflammation is a natural defence response of the immune system against environmental insult, stress and injury, but hyper- and hypo-inflammatory responses can trigger diseases. Accumulating evidence suggests that inflammation is involved in multiple psychiatric disorders.
0 thoughts on “Inflammation and mental health”