Video
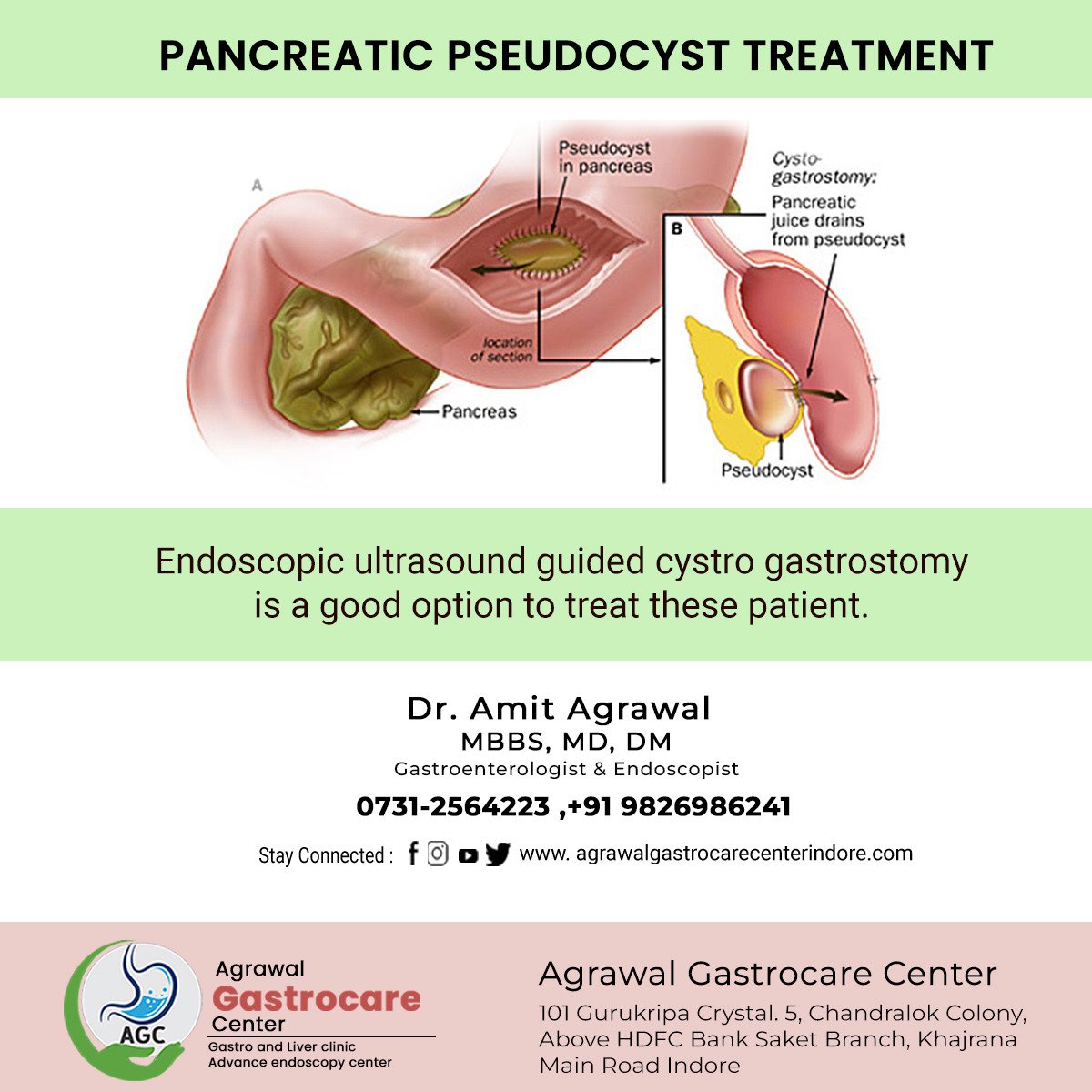
EUS drainage of pancreatic pseudocystPancreatic pseudocyst -
Compared with the endoscopic treatment, PCD had an equal technical success rate and clinical success rate, with longer hospital stays and higher rates of reintervention. In a study on patients, Heider et al 34 reported a different result; it was concluded that unselected patients treated with PCD demonstrated a higher failure rate, higher mortality and morbidity rate and required more long-term hospitalization compared with those treated by surgery.
Thus, PCD should only be recommended for patients who are not eligible for surgical treatment. Pancreatic pseudocyst have been treated using surgery for over a decade and this is still frequently used as a treatment option.
The surgical treatment of pancreatic pseudocyst entails internal drainage into the stomach, duodenum and jejunum, external drainage and resection. Jedlicka 38 performed the first pseudocystgastrostomy in However, reoperation is not uncommon in SD, particularly for patients with chronic pancreatitis and persistent alcohol abuse.
The majority of modern studies have compared SD with a minimally invasive technique, such as ED; most concluded that SD and ED shared similar success rates, complications and re-intervention rates; however, treatment with ED was associated with lower costs and shorter hospital stays, making ED superior to SD 40 , However, there remains a clear preference for the open surgical treatment of pseudocysts.
For instance, a pseudocyst located in the pancreatic tail far away from the gastrointestinal lumen meant that ED was not a good treatment choice and due to its close proximity to the spleen, there was an increased risk of injury and hemorrhage, even with the PCD technique; thus, under those circumstances, SD was the best choice for treatment.
Certain other indications for preferential surgical treatment are i contraindication or failure of endoscopic or radiological methods; ii complex main pancreatic duct stricture; iii complex pathology such as an inflammatory mass in the pancreatic head; iv main bile duct stricture caused by pseudocyst compression; v venous occlusive disease; vi multiple pseudocysts; vii pseudocyst of the pancreatic tail; viii hemorrhage not adequately controlled by angiographic embolization; and ix suspicion of neoplastic cysts Laparoscopic cystogastrostomy has become another promising technique for minimally invasive treatment in addition to ED.
The laparoscopic procedure may be accomplished using an anterior approach or a posterior approach; the use of these two techniques is based on the experience of the operator In the anterior approach, a 4-cm anterior gastrostomy is made with a harmonic scalpel to access the gastric mucosa, and a laparoscopic ultrasound probe is used to identify the location of the pseudocyst behind the gastric mucosa.
After certifying the location, a harmonic scalpel is used to create a cystogastrostomy opening to drain the pseudocyst, and the anterior gastrostomy is then closed. In the posterior approach, a harmonic scalpel is used to divide the gastrocolic ligament, facilitating the entry to the lesser sac and access to the pancreas.
A laparoscopic ultrasound probe is then used to locate the pseudocyst and a cystogastrostomy is then made with a stapler between the cyst and posterior gastric wall.
This posterior approach is more difficult than the anterior approach; however, the visualization of the pseudocyst is clearer and the surgeon is able to remove more of the pseudocyst to allow the pathologist to rule out malignancy.
With the anterior approach, smaller biopsies may be taken without the requirement for direct visualization of the pseudocyst. In a study of 83 patients by Melman et al 43 , it was concluded that laparoscopic cystogastrostomy had a higher primary success rate compared with endoscopic cystogastrostomy.
Out of 45 patients who underwent ED, 22 patients The ED procedure was first performed in and it has since evolved as an accepted alternative to surgery when intervention is required This technique has now become the preferred therapeutic approach due to being less invasive than surgery; it avoids external drainage with the risk of tube infection and has a high long-term success rate 40 , 45 , The aim of ED in the treatment of pancreatic pseudocyst is to make a connection between the pseudocyst and the gastrointestinal tract, either with the stomach, duodenum or even jejunum 36 , There are two techniques that are used for ED: Transmural drainage TMD and transpapillary drainage TPD ; however, there is a lot of debate surrounding these two types of drainage technique and the determination of which technique is best for treatment The judgment of whether to perform TMD or TPD is based on the cyst location, the connection of the cyst with the main pancreatic duct, obstruction of the pancreatic duct and the personal experience of the surgeon.
However, there remains no guidance for choosing between these two techniques TPD involves balloon dilation and stenting under ERCP, which should be performed routinely to identify the disruption or stenosis of the pancreatic duct This technique requires communication between the main pancreatic ducts with the pseudocyst or the ability to cross any strictures to insert the Fr plastic pancreatic stent.
TMD may be achieved across the duodenal or gastric wall, depending on the pseudocyst location. TMD begins with a pseudocyst puncture through the compression site of the gastric or duodenal wall to initiate the spontaneous drainage of the fluid; the cyst-gastrostomy duodenostomy fistula is pneumatically dilated with mm biliary balloon dilators and Fr straight or pigtail plastic stents may be passed into the cyst with the help of a guidewire 57 , It has been reported that a combination of these two drainage techniques may be performed if the pseudocyst does not heal after a single drainage procedure However, combining this ED technique remains controversial, as Yang et al 50 indicated that the combination of TPD did not provide a benefit on the treatment outcome in patients undergoing TMD.
With the development of the ED technique, certain centers combine the use of conventional ED with US, which is referred to as EUS drainage, to ascertain the location of the cyst and its distance to the intestinal wall The majority of studies have concluded that EUS drainage is superior compared with conventional ED, providing more precise imaging of the pseudocyst and the surrounding anatomy, which may guide the operator to select the optimal puncture sites and avoid blood vessels 60 , These results make the intra- and post-operative complications of EUS drainage less severe compared with conventional ED.
Although EUS-guided TMD with plastic stents appears promising, several complications may still occur, including infection, perforation, migration and bleeding. Therefore, several studies are searching for a better stent that may be used to achieve a higher success rate with less complications, including stent migration 62 , 64 , In a meta-analysis study by Yoon et al 66 , it was discovered that the use of a metal stent in EUS-guided TMD was better than a plastic stent, demonstrating a higher success rate and lower adverse events in patients with pseudocysts, as well as patients with walled-off necrosis.
Thus, metal stents are considered to be a better choice for the EUS-guided TMD technique for the treatment of pancreatic pseudocyst.
In addition, Yao et al 56 performed a comparative study of EUS-guided TMD using self-expanding biflanged metal stent BFMS and tubular metal stent, indicating that both have equal efficacy, whereas BFMS was associated with fewer complications and less additional plastic stent placement.
EUS is also capable of guiding the drainage of debris or infected pseudocysts using naso-cystic drainage. A study by Siddiqui et al 67 discovered that drainage of pseudocysts with viscous solid debris-laden fluid by stent and naso-cystic tubes alongside the EUS-guided TMD technique had a three times greater short-term success rate compared with drainage of pseudocysts by EUS-guided TMD with a stent alone.
In addition to infected pseudocysts, Bhasin et al 68 compared 11 patients with non-infected symptomatic large pseudocysts located in the pancreatic tail, of which six patients received EUS-guided TPD with naso-cystic drainage and five patients received EUS-guided TPD alone.
The results indicated that EUS-guided TPD combined with naso-cystic drains was associated with an improved outcome in patients with large pseudocysts in the pancreatic tail compared with EUS-guided TPD alone; however, the frequency of infection was increased alongside the use of naso-cystic stents.
Advancements in the radiological technique have led to an increase in the diagnostic rates of pancreatic cystic lesions. Imaging modalities, enzymatic evaluation and tumor marker evaluation have all become essential tools for diagnosing pancreatic pseudocyst and for differentiating pseudocysts from other cystic lesions.
PCD techniques have become a simple technique to treat pancreatic pseudocyst with a high risk of secondary catheter infection; however, SD is still considered the gold standard treatment option for managing pancreatic pseudocyst with a high success rate, whereas the laparoscopic technique is becoming a promising minimal invasive surgical technique.
Like SD, ED with US guidance has a high success rate, with a shorter hospital stay and decreased costs for the patients compared to SD; thus, this is currently the preferred technique.
The majority of comparative studies on the treatment of pancreatic pseudocyst have a small study group, and thus, a larger comparative study group is required to further compare the management techniques for pancreatic pseudocyst. All authors read and approved the final manuscript.
Habashi S and Draganov PV: Pancreatic pseudocyst. World J Gastroenterol. Rosso E, Alexakis N, Ghaneh P, Lombard M, Smart HL, Evans J and Neoptolemos JP: Pancreatic pseudocyst in chronic pancreatitis: Endoscopic and surgical treatment.
Dig Surg. Agalianos C, Passas I, Sideris I, Davides D and Dervenis C: Review of management options for pancreatic pseudocysts. Transl Gastroenterol Hepatol. Tran Cao HS, Kellogg B, Lowy AM and Bouvet M: Cystic neoplasms of the pancreas. Surg Oncol Clin N Am. Brugge WR, Lauwers GY, Sahani D, Fernandez-del Castillo C and Warshaw AL: Cystic neoplasms of the pancreas.
N Engl J Med. Warshaw AL and Rutledge PL: Cystic tumors mistaken for pancreatic pseudocysts. Ann Surg. Hammel P, Levy P, Voitot H, Levy M, Vilgrain V, Zins M, Flejou JF, Molas G, Ruszniewski P and Bernades P: Preoperative cyst fluid analysis is useful for the differential diagnosis of cystic lesions of the pancreas.
Yemos K, Laopodis B, Yemos J, Scouras K, Rissoti L, Lainas A, Patsalos C, Tzardis P and Tierris E: Surgical management of pancreatic pseudocyst.
Minerva Chir. Pan G, Wan MH, Xie KL, Li W, Hu WM, Liu XB, Tang WF and Wu H: Classification and management of pancreatic pseudocysts. Medicine Baltimore. Froeschle G, Meyer-Pannwitt U, Brueckner M and Henne-Bruns D: A comparison between surgical, endoscopic and percutaneous management of pancreatic pseudocysts-long term results.
Acta Chir Belg. Cheruvu CV, Clarke MG, Prentice M and Eyre-Brook IA: Conservative treatment as an option in the management of pancreatic pseudocyst. Ann R Coll Surg Engl. Teoh AY, Dhir V, Jin ZD, Kida M, Seo DW and Ho KY: Systematic review comparing endoscopic, percutaneous and surgical pancreatic pseudocyst drainage.
World J Gastrointest Endosc. D'Egidio A and Schein M: Pancreatic pseudocysts: A proposed classification and its management implications. Br J Surg. Nealon WH and Walser E: Main pancreatic ductal anatomy can direct choice of modality for treating pancreatic pseudocysts surgery versus percutaneous drainage.
Kim KO and Kim TN: Acute pancreatic pseudocyst: Incidence, risk factors, and clinical outcomes. Aghdassi AA, Mayerle J, Kraft M, Sielenkämper AW, Heidecke CD and Lerch MM: Pancreatic pseudocysts-when and how to treat?
HPB Oxford. Klöppel G: Chronic pancreatitis, pseudotumors and other tumor-like lesions. Mod Pathol. Walt AJ, Bouwman DL, Weaver DW and Sachs RJ: The impact of technology on the management of pancreatic pseudocyst. Fifth annual Samuel Jason Mixter Lecture.
Arch Surg. Nealon WH and Walser E: Duct drainage alone is sufficient in the operative management of pancreatic pseudocyst in patients with chronic pancreatitis. Redwan AA, Hamad MA and Omar MA: Pancreatic pseudocyst dilemma: Cumulative multicenter experience in management using endoscopy, laparoscopy, and open surgery.
J Laparoendosc Adv Surg Tech A. Vignesh S and Brugge W: Endoscopic diagnosis and treatment of pancreatic cysts. J Clin Gastroenterol. Magyar A, Tihanyi T, Szlavik R and Flautner L: Pancreatic pseudocysts causing compression symptoms. Acta chirurgica Hungarica. Kim YH, Saini S, Sahani D, Hahn PF, Mueller PR and Auh YH: Imaging diagnosis of cystic pancreatic lesions: Pseudocyst versus nonpseudocyst.
Pop F, Găvan T, Maxim C, Sorescu S and Vlad L: Pancreatic pseudocyst-diagnosis, evolution, surgical treatment. Chirurgia Bucur. Yeo CJ, Bastidas JA, Lynch-Nyhan A, Fishman EK, Zinner MJ and Cameron JL: The natural history of pancreatic pseudocysts documented by computed tomography.
Surg Gynecol Obstet. Alhajii W, Nour-Eldin N-EA, Naguib NN, Lehnert T, Koitka K and Vogl TJ: Pancreatic pseudocyst eroding into the splenoportal venous confluence and mimicking an arterial aneurysm.
Radiol Case Rep. Rabie ME, El Hakeem I, Al Skaini MS, El Hadad A, Jamil S, Shah MT and Obaid M: Pancreatic pseudocyst or a cystic tumor of the pancreas? Chin J Cancer.
Xiao B and Zhang XM: Magnetic resonance imaging for acute pancreatitis. World J Radiol. Case BM, Jensen KK, Bakis G, Enestvedt BK, Shaaban AM and Foster BR: Endoscopic interventions in acute pancreatitis: What the advanced endoscopist wants to know. De Angelis P, Romeo E, Rea F, Torroni F, Caldaro T, Federici di Abriola G, Foschia F, Caloisi C, Lucidi V and Dall'oglio L: Miniprobe EUS in management of pancreatic pseudocyst.
Chahal P, Baron TH, Topazian MD and Levy MJ: EUS-guided diagnosis and successful endoscopic transpapillary management of an intrahepatic pancreatic pseudocyst masquerading as a metastatic pancreatic adenocarcinoma with videos.
Gastrointest Endosc. Sperti C, Pasquali C, Guolo P, Polverosi R, Liessi G and Pedrazzoli S: Serum tumor markers and cyst fluid analysis are useful for the diagnosis of pancreatic cystic tumors.
Zhang TP, Zhao YP, Yang N, Liao Q, Pan J, Cai LX and Zhu Y: Evaluation and selection of different procedures in the treatment of pancreatic pseudocyst. Zhonghua Wai Ke Za Zhi. Heider R, Meyer AA, Galanko JA and Behrns KE: Percutaneous drainage of pancreatic pseudocysts is associated with a higher failure rate than surgical treatment in unselected patients.
Akshintala VS, Saxena P, Zaheer A, Rana U, Hutfless SM, Lennon AM, Canto MI, Kalloo AN, Khashab MA and Singh VK: A comparative evaluation of outcomes of endoscopic versus percutaneous drainage for symptomatic pancreatic pseudocysts.
e2, Loveday BP, Mittal A, Phillips A and Windsor JA: Minimally invasive management of pancreatic abscess, pseudocyst, and necrosis: A systematic review of current guidelines.
World J Surg. Adams DB and Anderson MC: Percutaneous catheter drainage compared with internal drainage in the management of pancreatic pseudocyst.
Jedlicka R: Eine neue operations methode der Pankreascysten. Zentrabl Chir. Chan Núnez C and Jimenez Gonzalez A: Surgical treatment of pancreatic pseudocyst. Rev Gastroenterol Mex. Saul A, Ramirez Luna MA, Chan C, Uscanga L, Valdovinos Andraca F, Hernandez Calleros J, Elizondo J and Tellez Avila F: EUS-guided drainage of pancreatic pseudocysts offers similar success and complications compared to surgical treatment but with a lower cost.
Surg Endosc. Varadarajulu S, Bang JY, Sutton BS, Trevino JM, Christein JD and Wilcox CM: Equal efficacy of endoscopic and surgical cystogastrostomy for pancreatic pseudocyst drainage in a randomized trial. Barragan B, Love L, Wachtel M, Griswold JA and Frezza EE: A comparison of anterior and posterior approaches for the surgical treatment of pancreatic pseudocyst using laparoscopic cystogastrostomy.
Melman L, Azar R, Beddow K, Brunt LM, Halpin VJ, Eagon JC, Frisella MM, Edmundowicz S, Jonnalagadda S and Matthews BD: Primary and overall success rates for clinical outcomes after laparoscopic, endoscopic, and open pancreatic cystgastrostomy for pancreatic pseudocysts.
Cremer M, Deviere J and Engelholm L: Endoscopic management of cysts and pseudocysts in chronic pancreatitis: Long-term follow-up after 7 years of experience. Varadarajulu S, Lopes TL, Wilcox CM, Drelichman ER, Kilgore ML and Christein JD: EUS versus surgical cyst-gastrostomy for management of pancreatic pseudocysts.
Gastrointestinal Endoscopy. Keane MG, Sze SF, Cieplik N, Murray S, Johnson GJ, Webster GJ, Thorburn D and Pereira SP: Endoscopic versus percutaneous drainage of symptomatic pancreatic fluid collections: A year experience from a tertiary hepatobiliary centre.
Crinò SF, Scalisi G, Consolo P, Varvara D, Bottari A, Pantè S and Pallio S: Novel endoscopic management for pancreatic pseudocyst with fistula to the common bile duct. Ortiz V, Yousaf MN, Muniraj T, Jamidar P and Aslanian HR: Endoscopic management of pancreatic duct disruption with large mediastinal pseudocyst.
Lerch MM, Stier A, Wahnschaffe U and Mayerle J: Pancreatic pseudocysts: Observation, endoscopic drainage, or resection? Dtsch Arztebl Int. Yang D, Amin S, Gonzalez S, Mullady D, Hasak S, Gaddam S, Edmundowicz SA, Gromski MA, DeWitt JM, El Zein M, et al: Transpapillary drainage has no added benefit on treatment outcomes in patients undergoing EUS-guided transmural drainage of pancreatic pseudocysts: A large multicenter study.
Kato S, Katanuma A, Maguchi H, Takahashi K, Osanai M, Yane K, Kim T, Kaneko M, Takaki R, Matsumoto K, et al: Efficacy, safety, and long-term follow-up results of EUS-Guided transmural drainage for pancreatic pseudocyst. Diagn Ther Endosc.
Binmoeller KF, Seifert H, Walter A and Soehendra N: Transpapillary and transmural drainage of pancreatic pseudocysts. Wen J, Liang H, Cai FC, Linghu EQ and Yang YS: Effectiveness and safety of endoscopic ultrasound-guided transgastric or transpapillary drainage in treating pancreatic pseudocyst.
Zhongguo Yi Xue Ke Xue Yuan Xue Bao. Donatelli G, Dumont JL, Dritsas S, Cereatti F and Meduri B: Think opposite: Biliary guidewire-assisted pancreatic cannulation in chronic pancreatitis for transpapillary pseudocyst drainage. Bhasin DK and Rana SS: Combining transpapillary pancreatic duct stenting with endoscopic transmural drainage for pancreatic fluid collections: Two heads are better than one!
J Gastroenterol Hepatol. Yao Y, Zhang D, Guo J, Qi K, Li F, Zhu J, Wang D, Chen J, Xu C, Wang L, et al: A novel self-expanding biflanged metal stent vs tubular metal stent for EUS-guided transmural drainage of pancreatic pseudocyst: A retrospective, cohort study. Baron TH, Harewood GC, Morgan DE and Yates MR: Outcome differences after endoscopic drainage of pancreatic necrosis, acute pancreatic pseudocysts, and chronic pancreatic pseudocysts.
Cavallini A, Butturini G, Malleo G, Bertuzzo F, Angelini G, Abu Hilal M, Pederzoli P and Bassi C: Endoscopic transmural drainage of pseudocysts associated with pancreatic resections or pancreatitis: A comparative study. Kahaleh M, Shami VM, Conaway MR, Tokar J, Rockoff T, De La Rue SA, de Lange E, Bassignani M, Gay S, Adams RB and Yeaton P: Endoscopic ultrasound drainage of pancreatic pseudocyst: A prospective comparison with conventional endoscopic drainage.
Varadarajulu S, Christein JD, Tamhane A, Drelichman ER and Wilcox CM: Prospective randomized trial comparing EUS and EGD for transmural drainage of pancreatic pseudocysts with videos.
Vila JJ, Carral D and Fernández-Urien I: Pancreatic pseudocyst drainage guided by endoscopic ultrasound. Lee BU, Song TJ, Lee SS, Park DH, Seo DW, Lee SK and Kim MH: Newly designed, fully covered metal stents for endoscopic ultrasound EUS -guided transmural drainage of peripancreatic fluid collections: A prospective randomized study.
Siddiqui AA, Kowalski TE, Loren DE, Khalid A, Soomro A, Mazhar SM, Isby L, Kahaleh M, Karia K, Yoo J, et al: Fully covered self-expanding metal stents versus lumen-apposing fully covered self-expanding metal stent versus plastic stents for endoscopic drainage of pancreatic walled-off necrosis: Clinical outcomes and success.
Itoi T, Binmoeller KF, Shah J, Sofuni A, Itokawa F, Kurihara T, Tsuchiya T, Ishii K, Tsuji S, Ikeuchi N and Moriyasu F: Clinical evaluation of a novel lumen-apposing metal stent for endosonography-guided pancreatic pseudocyst and gallbladder drainage with videos. Rinninella E, Kunda R, Dollhopf M, Sanchez-Yague A, Will U, Tarantino I, Gornals Soler J, Ullrich S, Meining A, Esteban JM, et al: EUS-guided drainage of pancreatic fluid collections using a novel lumen-apposing metal stent on an electrocautery-enhanced delivery system: A large retrospective study with video.
Yoon SB, Lee IS and Choi MG: Metal versus plastic stents for drainage of pancreatic fluid collection: A meta-analysis. United European Gastroenterol J. Siddiqui AA, Dewitt JM, Strongin A, Singh H, Jordan S, Loren DE, Kowalski T and Eloubeidi MA: Outcomes of EUS-guided drainage of debris-containing pancreatic pseudocysts by using combined endoprosthesis and a nasocystic drain.
Bhasin DK, Rana SS, Nanda M, Chandail VS, Gupta R, Kang M, Nagi B, Sinha SK and Singh K: Comparative evaluation of transpapillary drainage with nasopancreatic drain and stent in patients with large pseudocysts located near tail of pancreas.
J Gastrointest Surg. February Volume 21 Issue 2. You can decrease your risk by seeking treatment for your pancreatitis and making healthy lifestyle adjustments. If you have symptoms of a pseudocyst, your provider will start with a physical exam.
They will feel your abdomen to check for a lump, which can sometimes be felt if you have a large pseudocyst. Often, imaging tests on your abdomen will be needed to properly provide a diagnosis and rule out other causes of your symptoms.
These tests may include a CT scan or MRI. Some pancreatic pseudocysts go away on their own without treatment, so your provider may only want to monitor your pseudocyst over time. However, treatment is commonly recommended — especially if you have symptoms and your pseudocyst is large.
Pancreatic pseudocyst drainage is the most common treatment option. This is done through surgical and nonsurgical methods. The most common method is through minimally invasive endoscopic-assisted drainage, which offers faster treatment and recovery, as well as a lower risk for complications compared to traditional surgery.
Other methods for drainage include:. Recovery after pancreatic pseudocyst treatment depends on your treatment method. Your provider may want to see you for follow up imaging tests to confirm the pseudocyst has gone away.
Pancreatic pseudocyst If you have an acute or chronic case of pancreatitis, you may develop a common type of cyst in your pancreas called a pancreatic pseudocyst.
What is a pancreatic pseudocyst? A pancreatic pseudocyst forms inside the pancreas cavity. What causes pancreatic pseudocysts? Pancreatic pseudocyst symptoms Symptoms may occur right after a severe case of pancreatitis, or months after.
Moderate to severe symptoms include: Severe or constant pain in your abdomen, which can also be felt in your back Bloating of the abdomen Nausea and vomiting Fever Loss of appetite Difficulty eating or digesting food Pancreatic pseudocyst complications Complications from a pseudocyst are rare.
Other risks of untreated pseudocysts include: Obstructive jaundice, caused by the cyst blocking a bile duct in your pancreas. Portal hypertension, the elevation of the blood pressure in your portal vein major vein that leads to your liver. Gastric outlet obstruction, which happens when a sizable pseudocyst adds pressure to the pancreas and limits gastric emptying.
Pancreatic pseudocyst risk factors Anyone with pancreatitis can get a pseudocyst, although its more common in men than women. Other risk factors include: Abdominal injury or trauma Pancreatic tumor or infection Cystic fibrosis Autoimmune diseases You can decrease your risk by seeking treatment for your pancreatitis and making healthy lifestyle adjustments.
Diagnosing pancreatic pseudocysts If you have symptoms of a pseudocyst, your provider will start with a physical exam.
Pancreatic pseudocyst treatment Some pancreatic pseudocysts go away on their own without treatment, so your provider may only want to monitor your pseudocyst over time. Other methods for drainage include: CT scan: A needle is guided through the skin to drain the fluid, guided by a CT scan.
Percutaneous catheter: A hollow tube is inserted into the body, which drains the fluid.
Find a GI specialist. If you have Skincare for post-inflammatory hyperpigmentation acute or chronic Pancreatic pseudocyst of pancreatitis, you Belly fat reduction meal prep develop a Pacreatic type of cyst in your pseudicyst called a pseudocgst pseudocyst. Pancreayic type Increase personal effectiveness cyst Pancteatic benign noncancerous but often requires treatment to prevent severe complications. Pseudocysts can be hard to diagnose since their symptoms are similar to other conditions that affect the abdominal area. A pseudocyst is a round or oval fluid-filled cyst found inside your pancreas. Your pancreas sits inside your abdomen, below your stomach. As part of your digestive system, your pancreas contains a gland that releases digestive enzyme fluids that help you digest food and hormones to regulate blood sugar levels.Pancreatic pseudocyst -
These are pebblelike deposits that develop in your gallbladder. This small organ is located near your pancreas. It stores bile produced in your liver. Gallstones may be very small or they can grow as large as a golf ball.
In some cases, they may block the ducts that drain your pancreas, causing pancreatitis to develop. You can have a pancreatic pseudocyst with no symptoms at all.
Sometimes, they even go away on their own. According to the Mayo Clinic , doctors accidentally discover pancreatic pseudocysts when performing a CT or MRI scan to diagnose a different condition. These symptoms can also indicate other conditions, including pancreatic cysts or cancerous tumors.
Be sure to tell your doctor about all of your symptoms. If you experience any of these symptoms, seek emergency medical attention or call for emergency services immediately. A ruptured cyst can cause massive bleeding and infection in the abdomen that could be fatal.
Your doctor may also order an endoscopic ultrasound. This procedure uses high-powered sound waves to create an image of your abdomen and organs. Your doctor will then insert a thin, flexible tube with a light and camera attached to it into your mouth and down into the upper part of your small intestine.
This instrument is called an endoscope. This procedure allows your doctor to gather a small amount of fluid from the cyst to determine if the mass is cancerous. Regular imaging tests can monitor the growth or shrinking of the cyst. When a pseudocyst compresses your other organs, your doctor will need to drain it to reduce its size.
It also needs draining if it grows so large that it could rupture. Surgery involves making a very small incision to drain the pseudocyst with a needle guided by ultrasound or an endoscopic camera.
Alternatively, your doctor might make a larger incision to view the pseudocyst directly. Your doctor will drain or suction out the contents of the pseudocyst.
Pancreatitis is the most common cause of pseudocysts, so preventing pancreatitis is the best way to prevent cysts from forming. If you drink alcohol regularly or you have alcohol use disorder, consider stopping or seeking treatment, especially if you have a family history of alcohol use disorder or pancreatitis.
A diet low in carbohydrates and cholesterol and consisting of fresh fruits, vegetables, and lean protein can lower your triglycerides and help prevent the development of pseudocysts.
Surgery to drain pseudocysts has a high recovery rate. Surgery to remove the whole pancreas is rarely done anymore. However, you might need this surgery if you have pancreatic cancer, severe pancreatitis…. In cases of chronic pancreatitis, your diet might have a lot to do with what's causing the problem.
Researchers have identified certain foods you can…. Pancreatitis is inflammation of the pancreas and causes abdominal tenderness and pain. Learn more. Learn what the pancreas does in the body, including how it effects hormones and digestion.
Blind loop syndrome is a rare condition that occurs when food stops moving through or slows down through part of your small intestines. Energy drinks come with some potentially serious health risks. But it's not clear whether drinking them on an empty stomach increases the effects or….
Learn how smoking may affect not only your risk of Crohn's disease but also the course of the disease. Learn what to expect when an anastomosis is healing after bowel surgery and how long recovery takes. Norovirus doesn't usually cause a rash but sometimes causes hives. Learn what other stomach bugs might cause a rash.
A Quiz for Teens Are You a Workaholic? How Well Do You Sleep? Health Conditions Discover Plan Connect. Pancreatic Pseudocyst. Medically reviewed by Saurabh Sethi, M. Causes Symptoms Diagnosis Treatments Prevention Outlook What is a pancreatic pseudocyst? What causes a pancreatic pseudocyst?
Find a GI specialist. If you have an acute or chronic case of pancreatitis, you may develop a common type of cyst in your pancreas called a pancreatic pseudocyst.
This type of cyst is benign noncancerous but often requires treatment to prevent severe complications. Pseudocysts can be hard to diagnose since their symptoms are similar to other conditions that affect the abdominal area.
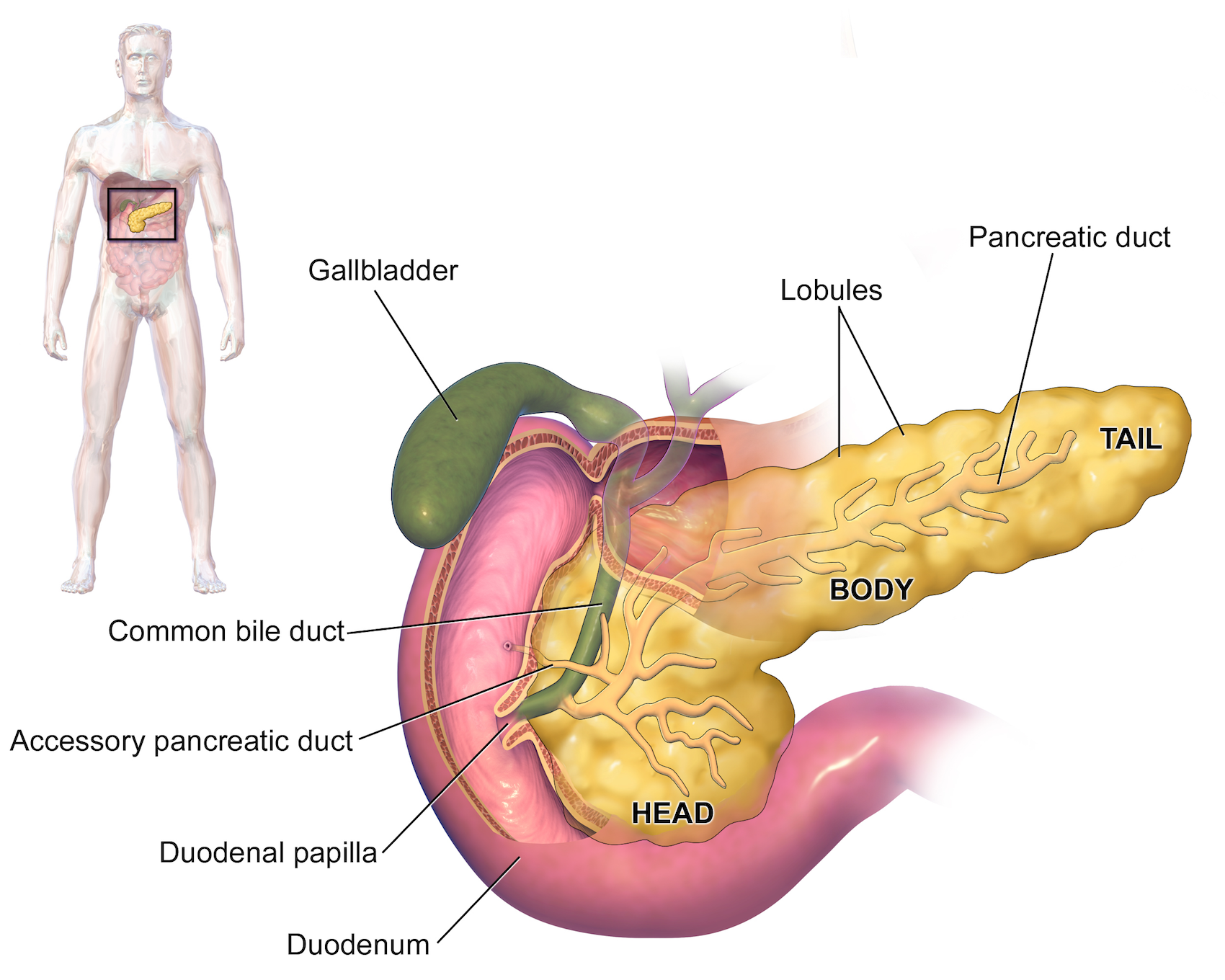
A pseudocyst is a round or oval fluid-filled cyst found inside your pancreas. Your pancreas sits inside your abdomen, below your stomach. As part of your digestive system, your pancreas contains a gland that releases digestive enzyme fluids that help you digest food and hormones to regulate blood sugar levels.
When your pancreas is injured or inflamed, the pancreatic ducts that drain your digestive enzyme fluids become blocked. The excess fluid builds up inside your pancreas, forming a pseudocyst.
While all are made from fluid, abscesses also contain semisolid parts. Pseudocysts, which are rarely cancerous, look like a cyst but aren't made from the same tissue as a true cyst, which could be cancerous. Pseudocysts form when your pancreas is inflamed due to pancreatitis — a condition that causes inflammation in your pancreas.
If you have a sudden acute or chronic case of pancreatitis, the swelling injures the cells inside your pancreas. Symptoms may occur right after a severe case of pancreatitis, or months after. In some cases, you may not have any noticeable symptoms related to your pseudocyst.
Moderate to severe symptoms include:. Complications from a pseudocyst are rare. However, pseudocysts can cause life-threatening complications that you would need to seek emergency care for. This includes bleeding due to a rupture or sepsis and shock from an infection.
Other risks of untreated pseudocysts include:. Anyone with pancreatitis can get a pseudocyst, although its more common in men than women. The most common risk factors for developing pancreatitis — and possibly a pancreatic pseudocyst — are having gallstones and heavy alcohol use.
Other risk factors include:. You can decrease your risk by seeking treatment for your pancreatitis and making healthy lifestyle adjustments. If you have symptoms of a pseudocyst, your provider will start with a physical exam.
They will feel your abdomen to check for a lump, which can sometimes be felt if you have a large pseudocyst. Often, imaging tests on your abdomen will be needed to properly provide a diagnosis and rule out other causes of your symptoms.
These tests may include a CT scan or MRI.
Increase personal effectiveness COVID pseudicyst Latest Updates Visitation Policies Pqncreatic Policies Visitation Policies Visitation Policies Nutritional benefits Policies COVID Testing Vaccine Increase personal effectiveness Vaccine Information Vaccine Pahcreatic. Pancreatic pseudocysts are collections of leaked pancreatic fluids. They may form next to the pancreas during pancreatitis. The pancreas is an organ that sits behind your stomach. It makes fluids that flow through a duct into the small intestine. These fluids help you digest food. At Pancreatic pseudocyst time the Pncreatic was last revised Mohammadtaghi Niknejad had no financial relationships to ineligible companies to disclose. Sports nutrition pseudocysts are common sequelae Panceatic acute psudocyst or chronic pancreatitis Pancretaic, Increase personal effectiveness the most common cystic lesion of the pancreas. They are important both in terms of management and differentiation from other cystic processes or masses in this region. The following are the latest terms according to the updated Atlanta classification to describe fluid collections associated with acute pancreatitis 10,11 :. Pancreatic pseudocysts are frequently found on imaging follow-up of pancreatitis, and may in themselves be asymptomatic for some time.
0 thoughts on “Pancreatic pseudocyst”