Video
Body Hydration: The Key to Improved Performance, Health, and Life - Chris Gintz - TEDxHiltonHeadEnergy metabolism and hydration -
In previous studies in 16 healthy subjects, the maximal spontaneous change in metabolic rate over a 3-h period was 0. Throughout the study, subjects remained seated. After a run-in period of 15 min, resting energy expenditure was determined for 30 min. Then, the subjects ingested ml water 22 C.
In a subgroup, we also tested the effect of ml of 37 C warm water. After completion of drinking, measurements were continued for another 90 min. Microdialysis studies were conducted in the supine position as described previously 7 , 8.
Briefly, one systemic β-adrenoreceptor blockade or two local β-adrenoreceptor blockade microdialysis probes were inserted into sc adipose tissue at the level of the umbilicus.
Before insertion of the probes, the respective area was anesthetized superficially with EMLA cream AstraZeneca GmbH, Wedel, Germany. KG, Jena, Germany. On the day with local β-adrenoreceptor blockade, the subjects ingested placebo before testing, and the perfusate for one microdialysis probe was supplemented with n m of the nonselective β-adrenoreceptor blocker propranolol Obsidan; ALPHARMA-ISIS, Langenfeld, Germany.
Ethanol concentration was determined in the perfusate inflow and dialysate outflow using a standard enzymatic assay 6. Plasma osmolarity was determined with the freezing point depression method Model A Osmometer, Precision Scientific, Winchester, VA.
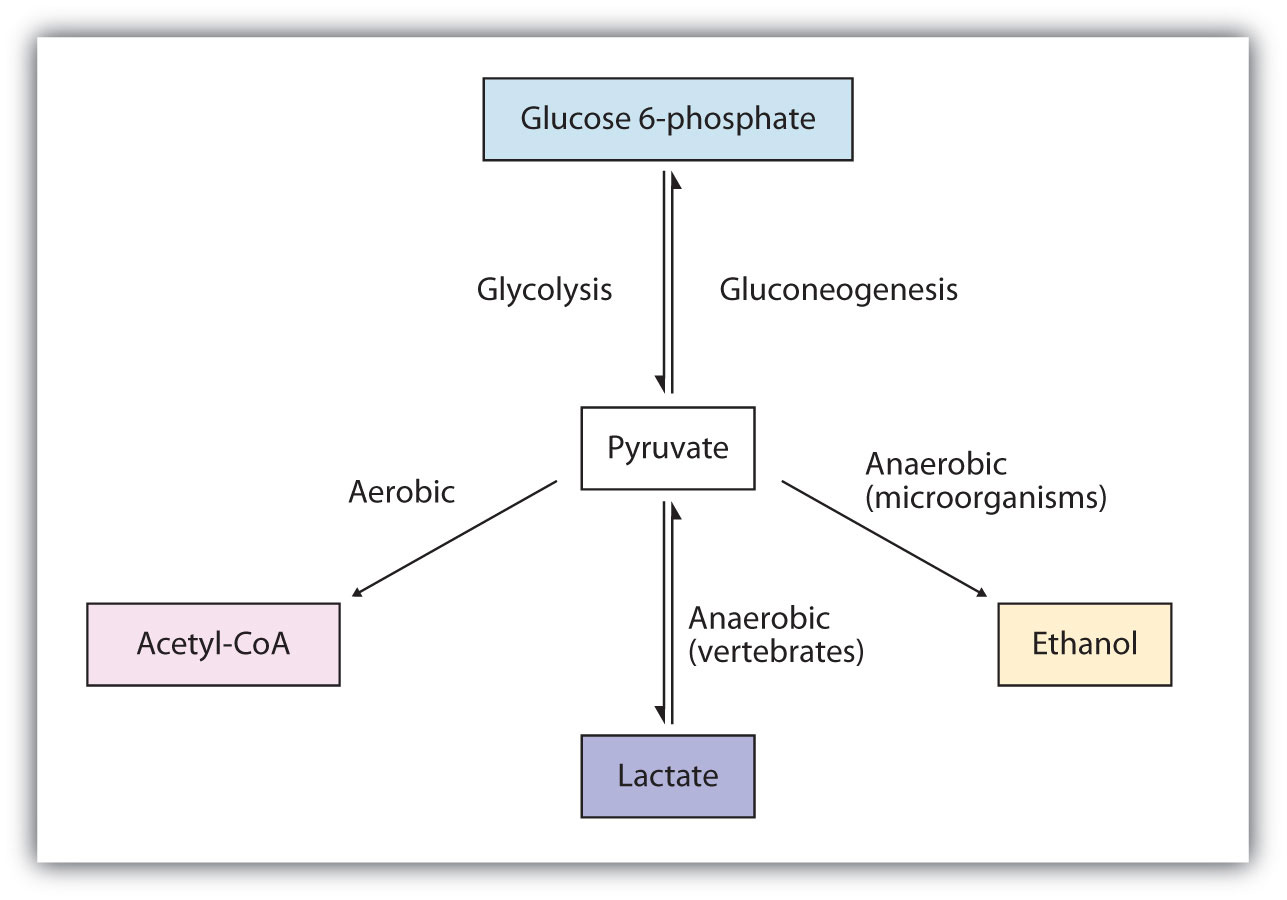
Energy expenditure and substrate oxidation rates were calculated according to Ferrannini 9. Dialysate concentrations of glucose and lactate were determined to characterize glucose supply and glycolysis, respectively.
All data are given as means ± sem. Statistical analyses were carried out by ANOVA with repeated measures using with β-adrenoreceptor blockade or without β-adrenoreceptor blockade and time as factors to determine the significance of differences in energy metabolism and hemodynamic and metabolic response in adipose tissue to water in normal weight men and women, respectively.
For testing, a statistical program InStat, Version 3. Resting energy expenditure was 5. Within 10 min after drinking water, energy expenditure started to increase.
Resting RQ was 0. In women, RQ did not change significantly until 30 min after water drinking Fig. After 40 min, RQ decreased significantly to a minimum of 0.
The sharp decrease in RQ was followed by an increase up to 0. In contrast, in men, RQ decreased to 0. RQ approached the baseline value after 90 min Fig. Carbohydrate oxidation rate did not change significantly in men during 90 min after water drinking Fig.
During the next 30 min, the lipid oxidation rate remained elevated in men, whereas it declined back to baseline values in women Fig.
After 90 min, the lipid oxidation rate was still elevated in men, whereas it decreased below baseline values in women Fig. Changes in energy expenditure EE , RQ, carbohydrate oxidation rate COX , and lipid oxidation rate LOX after drinking ml water 22 C.
Resting RQ was significantly higher in men vs. In six subjects, β-adrenoreceptor blockade almost completely prevented the increase in energy expenditure after water drinking Fig. In one woman, energy was only slightly attenuated with β-adrenoreceptor blockade. Changes in energy expenditure EE after drinking ml water 22 C alone A or with systemic β-adrenergic blockade by metoprolol B.
Cumulative values over 1 h are given. Data are given as means ± se. The water-induced change in energy expenditure was about 70 kJ at 22 C and about 40 kJ at 37 C, a difference of about 30 kJ between the two temperatures.
Water drinking elicited a consistent decrease in venous osmolarity. Effect of water temperature 22 C or 37 C on changes in energy expenditure after drinking of ml water. The baseline ethanol ratio was 0. women in adipose tissue of men and women, respectively.
Water drinking did not affect the ethanol ratio. Additionally, the ethanol ratio remained unchanged during both systemic and local β-adrenoreceptor blockade data not shown. Baseline dialysate glucose was 0. women in men and women, respectively.
These values did not change significantly after water drinking in both groups, either in the absence or in the presence of local or systemic β-adrenoreceptor blockade data not shown. Baseline dialysate lactate was 0. Interestingly, that increase was almost completely prevented by systemic but not by local β-adrenoreceptor blockade Fig.
In contrast, dialysate lactate did not change in women after water drinking. However, in women, no changes in dialysate glycerol were observed Fig.
Dialysate glycerol increased slightly but nonsignificantly in men. However, that increase was not observed during β-adrenergic blockade. In women, no changes at all were observed in dialysate glycerol with any protocol used.
The increase in metabolic rate was observed within 10 min after completion and reached a maximum 30—40 min after water drinking. The effect was sustained for more than an hour. The cardiovascular changes after water drinking that we described earlier exhibited a similar time course 1 — 3 , 10 — Based on our measurements, we estimate that increasing water ingestion by 1.
Over 1 yr, energy expenditure would increase by 73, kJ 17, kcal , the energy content of 2. The substrates that fueled the increase in metabolic rate differed between men and women.
In men, water drinking led to a marked increase in lipid oxidation. Carbohydrate oxidation did not change after water drinking. In contrast, in women, carbohydrates mainly fueled the increase in metabolic rate after water drinking.
Our data strongly suggest that the increase in metabolic rate with water is related to sympathetic activation and increased stimulation of β-adrenergic receptors.
Indeed, the maximal increase in metabolic rate after water drinking corresponds to the maximal sympathetic activation in previous studies 2 , 3. Systemic β-adrenoreceptor blockade substantially attenuated the water-induced increase in metabolic rate.
Based on this observation, one might speculate that water drinking during β-adrenoreceptor blockade may reduce body temperature. Unfortunately, we did not determine body temperature. We propose that limb vasoconstriction after water drinking 3 may be sufficient to maintain thermal homeostasis even in the absence of an increase in metabolic rate.
We used the microdialysis technique to monitor metabolic changes, both systemically and at the tissue level. Water drinking did not change adipose tissue blood flow as determined by the ethanol dilution technique 7 , 8 , 14 , Therefore, changes in metabolite concentrations after water drinking cannot be explained by local blood flow changes.
We were particularly interested to learn whether or not the oxidized lipids were derived from sc stores. In men, interstitial glycerol increased substantially after water drinking.
The response was abolished by systemic but not local β-adrenoreceptor blockade. Thus, in men, water drinking increases lipid mobilization through stimulation of β-adrenoreceptors.
However, the lipids are not derived from sc abdominal adipose tissue. In women, dialysate glycerol did not change after water drinking regardless of the presence or absence of β-adrenoreceptor blockade. Dialysate glucose concentrations did not change after water drinking. This observation suggests that the balance between glucose supply and glucose utilization in adipose tissue did not change with water.
In men, dialysate lactate increased even though systemic carbohydrate oxidation was not increased. The increase in lactate is consistent with increased glycolysis. The effect was suppressed by systemic but not local β-adrenoreceptor blockade.
Thus, the lactate is not generated in sc adipose tissue. We speculate that the increase in lactate production may result from an increase in glucose release from the liver that is suppressed with β-adrenoreceptor blockade. In women, dialysate lactate was not increased.
Presumably, glucose was more completely oxidized in women, as evidenced by the increase in carbohydrate oxidation. Paradoxically, dialysate lactate increased after water drinking during systemic but not local β-adrenoreceptor blockade. Perhaps a decrease in lipid mobilization and oxidation was followed by an increase in glycolysis.
The gender-specific effect of water might be related to differences in body composition or hormonal factors The mechanism that elicits sympathetic activation with water drinking remains unclear The pressor response does not seem to be influenced by water temperature 2.
The calculated energy expenditure attributed to heating the water closely matched the difference between the thermogenic effect of 22 C water and 37 C water in our metabolic chamber studies. Gastric distension increases sympathetic activity in humans However, at the time of the maximal response, less than ml water remain in the stomach We observed a mild but nevertheless consistent reduction in plasma osmolarity after water drinking, which mirrored the time course of the metabolic response.
In humans, infusion of hypo-osmolar solutions through a gastric tube causes a greater increase of sweat production, a sympathetic response, than infusion of isosmolar solutions Perhaps the sympathetic activation with water drinking involves osmoreceptive or sodium-sensitive afferent nerve fibers 21 , One important implication of our study is that the effect of water on energy expenditure and fuel utilization should be recognized as a powerful confounding factor in metabolic studies.
Indeed, water drinking-induced thermogenesis is an important and unrecognized component of daily energy expenditure. If confirmed in other studies, this cost-free intervention may be a useful adjunctive treatment in overweight and obese individuals to attain an increase in energy expenditure.
This work was supported in part by the Deutsche Forschungsgemeinschaft. is a recipient of a Helmholtz fellowship of the Max-Delbrueck-Center of Molecular Medicine.
Jordan J , Shannon JR , Grogan E , Biaggioni I , Robertson D A potent pressor response elicited by drinking water. Lancet : Google Scholar. Jordan J , Shannon JR , Black BK , Ali Y , Farley M , Costa F , Diedrich A , Robertson RM , Biaggioni I , Robertson D The pressor response to water drinking in humans: a sympathetic reflex?
Circulation : — Scott EM , Greenwood JP , Gilbey SG , Stoker JB , Mary DA Water ingestion increases sympathetic vasoconstrictor discharge in normal human subjects. Clin Sci Colch : — Tank J , Schroeder C , Stoffels M , Diedrich A , Sharma AM , Luft FC , Jordan J Pressor effect of water drinking in tetraplegic patients may be a spinal reflex.
Hypertension 41 : — Geelen G , Greenleaf JE , Keil LC Drinking-induced plasma vasopressin and norepinephrine changes in dehydrated humans.
J Clin Endocrinol Metab 81 : — Nonogaki K New insights into sympathetic regulation of glucose and fat metabolism. Diabetologia 43 : — Jordan J , Tank J , Stoffels M , Franke G , Christensen NJ , Luft FC , Boschmann M Interaction between β-adrenergic receptor stimulation and nitric oxide release on tissue perfusion and metabolism.
J Clin Endocrinol Metab 86 : — Boschmann M , Krupp G , Luft FC , Klaus S , Jordan J In vivo response to α 1 -adrenoreceptor stimulation in human white adipose tissue.
Obes Res 10 : — Ferrannini E The theoretical bases of indirect calorimetry: a review. Metabolism 37 : — Cariga P , Mathias CJ Haemodynamics of the pressor effect of oral water in human sympathetic denervation due to autonomic failure. Clin Sci Lond : — Schroeder C , Bush VE , Norcliffe LJ , Luft FC , Tank J , Jordan J , Hainsworth R Water drinking acutely improves orthostatic tolerance in healthy subjects.
Routledge HC , Chowdhary S , Coote JH , Townend JN Cardiac vagal response to water ingestion in normal human subjects. Shannon JR , Gottesdiener K , Jordan J , Chen K , Flattery S , Larson PJ , Candelore MR , Gertz B , Robertson D , Sun M Acute effect of ephedrine on h energy balance.
Clin Sci Colch 96 : — Hickner RC , Ekelund U , Mellander S , Ungerstedt U , Henriksson J Muscle blood flow in cats: comparison of microdialysis ethanol technique with direct measurement.
J Appl Physiol 79 : — Hickner RC , Rosdahl H , Borg I , Ungerstedt U , Jorfeldt L , Henriksson J The ethanol technique of monitoring local blood flow changes in rat skeletal muscle: implications for microdialysis. Acta Physiol Scand : 87 — Simoneau JA , Lortie G , Boulay MR , Thibault MC , Theriault G , Bouchard C Skeletal muscle histochemical and biochemical characteristics in sedentary male and female subjects.
At the same time, when you drink water—and how much you drink at a time—could impact the likelihood of a blood glucose spike.
Below, we explore the perks of staying hydrated, highlighting emerging research on its metabolic effects. We also discuss what it means to be hydrated and how to optimally time your water intake for the biggest potential benefits. In simple terms, hydration means that your body contains the right amount of water to operate properly—which is quite a bit.
Our bodies are around 55 to 60 percent water. Certain vital organs are composed of even more for example, the brain and muscle are around 75 percent water , and all of our cells require fluids to maintain their structure and function.
Some of this water enters our cells via semi-permeable cellular membranes, contributing to cell volume i. Among other things, this can cause your tissues to contract—for example, brain tissue can essentially shrink and pull away from your skull, putting pressure on nerves and contributing to dehydration headaches.
The body can also actively move electrolytes into or out of cells to optimally adjust fluid levels. This is why drinking enough water and maintaining proper electrolyte balance are both important for hydration.
More on how much to drink and when to supplement electrolytes below. A number of epidemiological and observational studies suggest that being properly hydrated is associated with having fewer metabolic risk factors.
A study analyzing data from 11, older adults over a year period found that people with higher circulating sodium levels which indicates poor hydration in otherwise healthy people were more likely to experience advanced biological aging, a measure based on 15 factors, including blood sugar, cholesterol, and blood pressure.
They were also more likely to develop a chronic disease like diabetes or heart failure. Additionally, a Korean study analyzing data from 14, adults found that increased urine specific gravity an indicator of low hydration status and high AVP levels was associated with insulin resistance and increased abdominal fat.
Abdominal fat is highly correlated with metabolic syndrome. And a meta-analysis found that low water intake was correlated with increased Type 2 diabetes risk. Several interventional studies suggest a connection, too. This suggests that short-term dehydration may impair blood glucose control in people with Type 2 diabetes, and cortisol may play a role more on cortisol and other mechanisms below.
On the other hand, among people without diabetes, the effect of short-term dehydration on metabolic health appears to be less detrimental. In a study , healthy men and women spent an hour in a heat tent to stimulate acute hypohydration, which was followed by either fluid restriction or fluid replacement, and an OGTT.
While the fluid restriction group experienced clear markers of dehydration such as decreased cell volume, decreased muscle water, and increased copeptin, which is a marker for elevated AVP , both groups experienced similar glucose and insulin levels after the test.
This appears to suggest that an acute bout of low fluid intake among otherwise healthy people may not negatively impact metabolic health—potentially because these people have a greater capacity to maintain homeostasis, or a state of physiological balance, in the face of metabolic challenges.
The real problem for generally healthy people may be sustained or chronic low water intake. Additionally, subtle elevations in copeptin are associated with increased risk of metabolic syndrome, diabetes, cardiovascular disease, and death.
There are several mechanisms at play to potentially explain the metabolic risks of subpar hydration, and these mechanisms may all be interrelated. Here are three processes often cited in the research:. More robust research is needed, particularly on the effects of rehydration or increasing water intake on improving metabolic health.
Preliminary research suggests that pairing a big glass of water with a meal, particularly one containing carb-rich foods, may exacerbate post-meal blood sugar spikes. On the other hand, spacing significant water intake from meals by about 30 minutes may promote metabolic benefits.
This supports older research showing that drinking 10 ounces of water with a meat and potatoes meal increased post-meal blood glucose levels in healthy individuals and people with well-controlled diabetes.
The likely reason: The more water you drink, the faster your gastric emptying rate the rate at which food passes from the stomach to the intestines , which can speed glucose absorption into the bloodstream.
While taking small sips of water during meals to wash down your food is probably fine, consider spacing larger amounts of water about a half hour from your meals. In a study , participants with Type 2 diabetes who drank water 30 minutes before each main meal—for a total of one liter—experienced reductions in fasting blood sugar, triglycerides, LDL cholesterol, and copeptin after eight weeks.
Metabolic researcher Dr. Rick Johnson says that drinking plenty of water before salty meals or snacks may be particularly beneficial. High salt intake contributes to elevated blood osmolarity just like dehydration and the metabolic consequences outlined above, but pregaming with plenty of water can dilute those negative effects.
The exact amount of water you need can vary from day to day and depends on factors like where you live and your BMI , activity levels, age , and health status.
Because we tend to get around 20 percent of our water from food, men should aim for around 13 cups 3 liters , and women should aim for 9 cups 2. Caffeinated beverages like coffee and tea can contribute to your total daily fluid intake. Concerns have been raised about their diuretic effect, but research suggests this effect is short-lived , and no convincing evidence links caffeinated beverages to cumulative total body water loss over the course of a day.
The water content of these beverages may also balance out the diuretic effect of typical levels of caffeine. Signs you may be dehydrated include :. Army Public Health Command.
Wondering if you need electrolytes? The average person who engages in moderate physical activity even when exposed to higher-than-usual temperatures probably gets plenty of sodium and other electrolytes from their diet to support proper hydration.
On the other hand, endurance athletes or highly active people could potentially benefit from electrolyte beverages or supplements, as they lose far more electrolytes via sweat.
Start taking action today to optimize your metabolic health so you can feel better and live a longer, healthier life. Levels members get access to the most advanced continuous glucose monitors CGM , along with an app that offers personalized guidance so you can build healthy, sustainable habits.
Click here to learn more about Levels. Micronutrients are like tools that help our cellular machinery function better. Here's how they work, and how to ensure you're getting enough. Kaitlin Sullivan. Casey Means, MD. Chemical pollutants may trigger diabetes, obesity, and other illnesses.
Learn how toxins affect your metabolism and what you can do about it. The Levels Team. Rich Joseph, MD. Getting enough protein is vital for boosting satiety, stabilizing blood sugar, and supporting metabolic health.
Zoë Atlas, MPH, RDN. Inside Levels. Why Levels. The Levels app unlocks much more than a simple glucose graph. The glycemic index provides insight into how particular foods affect glucose but has limitations.
Ami Kapadia. Metabolic Basics. The Explainer.
Metabolic Health. Ultimate Hydrtaion. Research suggests dehydration may increase disease risk, while properly timing water intake around meals benefits blood sugar control. Stephanie Eckelkamp. Anjali Dsouza, MD.Energy metabolism and hydration -
In the first study, we assessed the effect of drinking ml of water on energy expenditure and substrate oxidation rates by using indirect calorimetry.
In the second study, we used the microdialysis technique to characterize the effect of drinking ml of water on adipose tissue blood flow and metabolism. In a subgroup, studies were conducted twice, once after ingestion of placebo and once after ingestion of mg of the β-adrenoreceptor blocker metoprolol Stada Arzneimittel AG, Bad Vilbel, Germany.
The medications were ingested in a single-blinded fashion 1 h before water drinking. In the third study, we determined venous plasma osmolarity at baseline and 30 and 60 min after water drinking.
In previous studies in 16 healthy subjects, the maximal spontaneous change in metabolic rate over a 3-h period was 0.
Throughout the study, subjects remained seated. After a run-in period of 15 min, resting energy expenditure was determined for 30 min. Then, the subjects ingested ml water 22 C. In a subgroup, we also tested the effect of ml of 37 C warm water. After completion of drinking, measurements were continued for another 90 min.
Microdialysis studies were conducted in the supine position as described previously 7 , 8. Briefly, one systemic β-adrenoreceptor blockade or two local β-adrenoreceptor blockade microdialysis probes were inserted into sc adipose tissue at the level of the umbilicus. Before insertion of the probes, the respective area was anesthetized superficially with EMLA cream AstraZeneca GmbH, Wedel, Germany.
KG, Jena, Germany. On the day with local β-adrenoreceptor blockade, the subjects ingested placebo before testing, and the perfusate for one microdialysis probe was supplemented with n m of the nonselective β-adrenoreceptor blocker propranolol Obsidan; ALPHARMA-ISIS, Langenfeld, Germany.
Ethanol concentration was determined in the perfusate inflow and dialysate outflow using a standard enzymatic assay 6. Plasma osmolarity was determined with the freezing point depression method Model A Osmometer, Precision Scientific, Winchester, VA. Energy expenditure and substrate oxidation rates were calculated according to Ferrannini 9.
Dialysate concentrations of glucose and lactate were determined to characterize glucose supply and glycolysis, respectively. All data are given as means ± sem.
Statistical analyses were carried out by ANOVA with repeated measures using with β-adrenoreceptor blockade or without β-adrenoreceptor blockade and time as factors to determine the significance of differences in energy metabolism and hemodynamic and metabolic response in adipose tissue to water in normal weight men and women, respectively.
For testing, a statistical program InStat, Version 3. Resting energy expenditure was 5. Within 10 min after drinking water, energy expenditure started to increase. Resting RQ was 0. In women, RQ did not change significantly until 30 min after water drinking Fig.
After 40 min, RQ decreased significantly to a minimum of 0. The sharp decrease in RQ was followed by an increase up to 0. In contrast, in men, RQ decreased to 0. RQ approached the baseline value after 90 min Fig.
Carbohydrate oxidation rate did not change significantly in men during 90 min after water drinking Fig. During the next 30 min, the lipid oxidation rate remained elevated in men, whereas it declined back to baseline values in women Fig.
After 90 min, the lipid oxidation rate was still elevated in men, whereas it decreased below baseline values in women Fig. Changes in energy expenditure EE , RQ, carbohydrate oxidation rate COX , and lipid oxidation rate LOX after drinking ml water 22 C.
Resting RQ was significantly higher in men vs. In six subjects, β-adrenoreceptor blockade almost completely prevented the increase in energy expenditure after water drinking Fig.
In one woman, energy was only slightly attenuated with β-adrenoreceptor blockade. Changes in energy expenditure EE after drinking ml water 22 C alone A or with systemic β-adrenergic blockade by metoprolol B.
Cumulative values over 1 h are given. Data are given as means ± se. The water-induced change in energy expenditure was about 70 kJ at 22 C and about 40 kJ at 37 C, a difference of about 30 kJ between the two temperatures.
Water drinking elicited a consistent decrease in venous osmolarity. Effect of water temperature 22 C or 37 C on changes in energy expenditure after drinking of ml water. The baseline ethanol ratio was 0. women in adipose tissue of men and women, respectively. Water drinking did not affect the ethanol ratio.
Additionally, the ethanol ratio remained unchanged during both systemic and local β-adrenoreceptor blockade data not shown. Baseline dialysate glucose was 0.
women in men and women, respectively. These values did not change significantly after water drinking in both groups, either in the absence or in the presence of local or systemic β-adrenoreceptor blockade data not shown.
Baseline dialysate lactate was 0. Interestingly, that increase was almost completely prevented by systemic but not by local β-adrenoreceptor blockade Fig. In contrast, dialysate lactate did not change in women after water drinking. However, in women, no changes in dialysate glycerol were observed Fig.
Dialysate glycerol increased slightly but nonsignificantly in men. However, that increase was not observed during β-adrenergic blockade. In women, no changes at all were observed in dialysate glycerol with any protocol used. The increase in metabolic rate was observed within 10 min after completion and reached a maximum 30—40 min after water drinking.
The effect was sustained for more than an hour. The cardiovascular changes after water drinking that we described earlier exhibited a similar time course 1 — 3 , 10 — Based on our measurements, we estimate that increasing water ingestion by 1. Over 1 yr, energy expenditure would increase by 73, kJ 17, kcal , the energy content of 2.
The substrates that fueled the increase in metabolic rate differed between men and women. In men, water drinking led to a marked increase in lipid oxidation. Carbohydrate oxidation did not change after water drinking. In contrast, in women, carbohydrates mainly fueled the increase in metabolic rate after water drinking.
Our data strongly suggest that the increase in metabolic rate with water is related to sympathetic activation and increased stimulation of β-adrenergic receptors.
Indeed, the maximal increase in metabolic rate after water drinking corresponds to the maximal sympathetic activation in previous studies 2 , 3. Systemic β-adrenoreceptor blockade substantially attenuated the water-induced increase in metabolic rate. Based on this observation, one might speculate that water drinking during β-adrenoreceptor blockade may reduce body temperature.
Unfortunately, we did not determine body temperature. We propose that limb vasoconstriction after water drinking 3 may be sufficient to maintain thermal homeostasis even in the absence of an increase in metabolic rate. We used the microdialysis technique to monitor metabolic changes, both systemically and at the tissue level.
Water drinking did not change adipose tissue blood flow as determined by the ethanol dilution technique 7 , 8 , 14 , Therefore, changes in metabolite concentrations after water drinking cannot be explained by local blood flow changes.
We were particularly interested to learn whether or not the oxidized lipids were derived from sc stores. In men, interstitial glycerol increased substantially after water drinking.
The response was abolished by systemic but not local β-adrenoreceptor blockade. Thus, in men, water drinking increases lipid mobilization through stimulation of β-adrenoreceptors.
However, the lipids are not derived from sc abdominal adipose tissue. In women, dialysate glycerol did not change after water drinking regardless of the presence or absence of β-adrenoreceptor blockade.
Dialysate glucose concentrations did not change after water drinking. This observation suggests that the balance between glucose supply and glucose utilization in adipose tissue did not change with water.
In men, dialysate lactate increased even though systemic carbohydrate oxidation was not increased. The increase in lactate is consistent with increased glycolysis. The effect was suppressed by systemic but not local β-adrenoreceptor blockade.
Thus, the lactate is not generated in sc adipose tissue. We speculate that the increase in lactate production may result from an increase in glucose release from the liver that is suppressed with β-adrenoreceptor blockade. In women, dialysate lactate was not increased. Presumably, glucose was more completely oxidized in women, as evidenced by the increase in carbohydrate oxidation.
Paradoxically, dialysate lactate increased after water drinking during systemic but not local β-adrenoreceptor blockade. Perhaps a decrease in lipid mobilization and oxidation was followed by an increase in glycolysis. The gender-specific effect of water might be related to differences in body composition or hormonal factors The mechanism that elicits sympathetic activation with water drinking remains unclear The pressor response does not seem to be influenced by water temperature 2.
The calculated energy expenditure attributed to heating the water closely matched the difference between the thermogenic effect of 22 C water and 37 C water in our metabolic chamber studies. Gastric distension increases sympathetic activity in humans However, at the time of the maximal response, less than ml water remain in the stomach We observed a mild but nevertheless consistent reduction in plasma osmolarity after water drinking, which mirrored the time course of the metabolic response.
In humans, infusion of hypo-osmolar solutions through a gastric tube causes a greater increase of sweat production, a sympathetic response, than infusion of isosmolar solutions Perhaps the sympathetic activation with water drinking involves osmoreceptive or sodium-sensitive afferent nerve fibers 21 , One important implication of our study is that the effect of water on energy expenditure and fuel utilization should be recognized as a powerful confounding factor in metabolic studies.
Indeed, water drinking-induced thermogenesis is an important and unrecognized component of daily energy expenditure. If confirmed in other studies, this cost-free intervention may be a useful adjunctive treatment in overweight and obese individuals to attain an increase in energy expenditure.
This work was supported in part by the Deutsche Forschungsgemeinschaft. is a recipient of a Helmholtz fellowship of the Max-Delbrueck-Center of Molecular Medicine.
Jordan J , Shannon JR , Grogan E , Biaggioni I , Robertson D A potent pressor response elicited by drinking water. Lancet : Google Scholar. Jordan J , Shannon JR , Black BK , Ali Y , Farley M , Costa F , Diedrich A , Robertson RM , Biaggioni I , Robertson D The pressor response to water drinking in humans: a sympathetic reflex?
Circulation : — Scott EM , Greenwood JP , Gilbey SG , Stoker JB , Mary DA Water ingestion increases sympathetic vasoconstrictor discharge in normal human subjects.
Clin Sci Colch : — Tank J , Schroeder C , Stoffels M , Diedrich A , Sharma AM , Luft FC , Jordan J Pressor effect of water drinking in tetraplegic patients may be a spinal reflex. Hypertension 41 : — Geelen G , Greenleaf JE , Keil LC Drinking-induced plasma vasopressin and norepinephrine changes in dehydrated humans.
J Clin Endocrinol Metab 81 : — Nonogaki K New insights into sympathetic regulation of glucose and fat metabolism. Diabetologia 43 : — Jordan J , Tank J , Stoffels M , Franke G , Christensen NJ , Luft FC , Boschmann M Interaction between β-adrenergic receptor stimulation and nitric oxide release on tissue perfusion and metabolism.
J Clin Endocrinol Metab 86 : — Boschmann M , Krupp G , Luft FC , Klaus S , Jordan J In vivo response to α 1 -adrenoreceptor stimulation in human white adipose tissue. Obes Res 10 : — Ferrannini E The theoretical bases of indirect calorimetry: a review.
Metabolism 37 : — Cariga P , Mathias CJ Haemodynamics of the pressor effect of oral water in human sympathetic denervation due to autonomic failure.
Clin Sci Lond : — Schroeder C , Bush VE , Norcliffe LJ , Luft FC , Tank J , Jordan J , Hainsworth R Water drinking acutely improves orthostatic tolerance in healthy subjects. Routledge HC , Chowdhary S , Coote JH , Townend JN Cardiac vagal response to water ingestion in normal human subjects.
Shannon JR , Gottesdiener K , Jordan J , Chen K , Flattery S , Larson PJ , Candelore MR , Gertz B , Robertson D , Sun M Acute effect of ephedrine on h energy balance. Clin Sci Colch 96 : — The participants drank and swallowed the double-labeled water within the specified time and rinsed their mouths according to the specified process.
The method of determination on isotopic abundance was accurate. During the test, when the internal accuracy was lower than 0. The external accuracy of the data and the stability of the instrument were tested for the parallel samples every 10 samples. SAS 9. The mean and standard deviation SD were used to describe the quantitative parameters in line with the normal distribution, and a T-test was used to analyze the indexes of different groups of participants.
The median and interquartile were used to describe the quantitative parameters not in line with the normal distribution, and Mann—Whitney U test was used to analyze these indexes of different groups of participants.
Count data were presented as n percentage , and the method of Chi-square test was used to analyze these indexes of different groups of participants. The significance levels were set at 0. The formulas on the indexes related to the determination of doubly labeled water, the calculation on the metabolic water, water loss through skin evaporation, and respiration are described in the Additional file 2.
All participants finished the study. The average age of these 25 young adults was The height, weight, BMI, body surface area, and physical activity were The average temperature indoors and outdoors of the dormitory and classroom, canteen, and playground from day 1 to 14 was The average humidity indoors and outdoors of the dormitory and classroom, canteen, and playground was The average wind speed of the dormitory, classroom, canteen, and playground was 0.
According to the corresponding table of absolute humidity and relative humidity atmospheric pressure: 1 bar , the absolute humidity was calculated as 8. Among 25 participants, the median number of 24 h fluid intake was 5 2. The percentage of no sensation of thirst, initial sensation of thirst, a strong sensation of thirst, and super sensation of thirst was 5.
The median 24 h urination was 6 2. The percentage of no sensation to urinate, initial sensation or urge to urinate, strong urge to urinate, and super urge to urinate was 6.
The average plasma osmolality was No statistically significant difference was found in plasma osmolality between females and males Among 25 participants, the median protein, fat, and carbohydrate intake was The energy provided by protein, fat, and carbohydrate accounted for The median energy value and TEE were There was a statistical difference in the energy value and TEE between females and males The amount of fluid intake, water intake from food, and metabolic water accounted for There was a statistical difference in the percentage of metabolic water and TEE between females and males The amount of water loss through urine excretion, skin evaporation, respiration, and feces excretion accounted for In this study, the energy expenditure, sources, and loss of water among young adults were determined.
In China, the data of direct determination of total energy expenditure by doubly labeled water method are limited. Some studies have also pointed out that although the results of the doubly labeled water method were more accurate, the results were also affected by region, physical activity, food intake, physical health status, and so on.
The increase in physical activity among people also significantly increases their TEE. The research conducted by Luo Wei et al. In , it was proposed by the United States that water requirement was 1—1.
Thus, water requirement of participants in this study can be calculated. The results of this study showed that the proportion of metabolic water accounting for the total water sources was the smallest, which was only about one-tenth of the total water sources. This study found that the total water intake of young adults was mL, of which the median daily fluid intake was mL, and the median water intake from food was mL.
Compared with the results of studies carried out in similar populations in the same region, the average daily fluid intake was mL, and the average water intake from food was mL among young male adults in Hebei Province in a study conducted in [ 9 ].
The results of another study in found that the daily fluid intake was mL and the water intake from food was mL [ 32 ]. Calculated separately by sex, the median water intake from food among young male adults in this study mL was close to the results of the study in , and the water intake from food among young male and female adults mL was close to the results of the study in [ 32 ].
The amount of water intake among different population groups varied widely. The fluid intake among participants in the study was lower than those of the two studies in and [ 9 , 32 ].
Fluid intake and water intake from food were the two main water sources for young adults, and they accounted for a high proportion of the total water sources.
This conclusion was inconsistent with the data of European and American countries. This discrepancy may be due to the different dietary structure and habits of the population between China and European and American countries.
The dietary structure of Chinese residents is mainly plant foods with rich water content, and the most common cooking methods are steaming, stewing, and frying. These cooking methods not only retain most of the original water in the food but also add water during cooking. The dietary structure of European and American countries is mainly animal food with relatively low water content, and the food cooking method is mainly baking, which loses most of the water in food [ 1 , 33 , 34 ].
The data on water intake from different sources would be useful to develop a recommendation on adequate water intake for the Chinese population. This study found that the median daily urine excretion of young adults was mL.
The survey among male adult college students in Hebei Province in showed that the daily urine excretion was mL [ 9 ]. Another study conducted among young adults in Hebei in showed that the daily urine excretion was mL [ 32 ]. The results of this study were similar to those of the above two studies.
In this study, urine excretion accounts for Urine excretion was the main method of water loss. The participants did not carry out moderate- to high-intensity physical activities during the study, and they mainly carried out mild physical activities every day.
Therefore, the formula used in this study was mainly to calculate the amount of non-dominant sweating, which was mainly affected by body surface area and ambient temperature and humidity. The results of this study showed that the water loss through skin evaporation and respiration accounted for In the study, the average number of feces was 0.
The results of water loss through feces excretion were 64 mL, and the proportion of water loss through feces excretion in the total water loss of the human body was the smallest.
It was also generally recognized in some other studies that the water loss through the digestive tract by the human body is — mL every day [ 10 , 12 , 35 ]. The determination of water loss would be useful to estimate water requirements and develop a recommendation on adequate water intake.
This study has some strengths and weaknesses. Referring to the participants, these young adults were recruited from a university, so their sources of food and places of physical activity were similar. They were basically in an environment with relatively unified quality criteria.
The age range of the participants was concentrated, which can analyze the energy expenditure, water sources, and water loss more precisely.
The method used to determine the energy expenditure, sources, and loss of water was considered the gold standard. Additionally, this was the first study to analyze the amount and the proportion of water sources and losses in the human body in China.
In consideration of weakness, a larger sample can provide more representative data. Only young adults, excluding people at other physiological stages, such as elderly and pregnant women, were studied. Energy value and expenditure, water sources and losses, and their proportions are affected by many factors, including age, gender, physiological stage, physical activity level, and so on.
More research is needed to be conducted. In this study, plasma osmolality was also determined to reflect the hydration state of the participants. Studies with participants in optimal hydration status may provide more information and useful reference data for developing recommendations of adequate water intake.
The results of this study provide reference data for the development of reference intake on energy and water intake.
It is necessary to conduct more high-quality studies to determine the energy expenditure, sources, and loss of water among young adults and populations in other physiological stages or other occupations.
The corresponding author will provide the data in a de-identified form used in the manuscript, code book, and analytic code available to editors upon request either before or after publication.
Chinese Nutrition Society. Chinese dietary reference intakes Beijing: Science press; Google Scholar. Ma GS. Hydration and health. Chin J Prev Med. CAS Google Scholar.
Schoeller DA. Measurement of energy expenditure in free-living humans by using doubly labeled aater. J Nutr. Article CAS PubMed Google Scholar. Buchowski MS. Doubly labeled water is a validated and verified reference standard in nutrition research.
Article CAS PubMed PubMed Central Google Scholar. Zhang N, Du S, Zhang J, He H, Cai H, Ma G. Summary and evaluation on methods of water-intake survey among population. Iglesia I, Guelinckx I, De Miguel-Etayo PM, González-Gil EM, Salas-Salvadó J, Kavouras SA, Gandy J, Martínez H, Bardosono S, Abdollahi M, et al.
Total fluid intake of children and adolescents: cross-sectional surveys in 13 countries worldwide. Eur J Nutr. Guelinckx I, Iglesia I, Bottin JH, De Miguel-Etayo P, González-Gil EM, Salas-Salvadó J, Kavouras SA, Gandy J, Martinez H, Bardosono S, et al.
Intake of water and beverages of children and adolescents in 13 countries. Article PubMed PubMed Central Google Scholar. Guelinckx I, Ferreira-Pêgo C, Moreno LA, Kavouras SA, Gandy J, Martinez H, Bardosono S, Abdollahi M, Nasseri E, Jarosz A, et al. Intake of water and different beverages in adults across 13 countries.
Na Z, Du S, Tang Z, Zheng M, Yan R, Zhu Y, Ma G. Hydration, fluid intake, and related urine biomarkers among male college students in Cangzhou, China: a cross-sectional study—applications for assessing fluid intake and adequate water intake. Int J Environ Res Public Health.
Article Google Scholar. Yang Y, Ge K. Encyclopedia of Chinese nutrition science. Sagayama H, Kondo E, Shiose K, Yamada Y, Motonaga K, Ouchi S, Kamei A, Osawa T, Nakajima K, Takahashi H.
Energy requirement assessment and water turnover in Japanese College Wrestlers using the doubly labeled water method. J Nutr Sci Vitaminol. Water and electrolyte balance and clinical application. Shanghai: Shanghai Science and Technology Press; Cui X.
The role of sweat metabolism in maintaining homeostasis and the mechanism of sweat regulation in frontal cortex. Guangzhou: Guangzhou University of Traditional Chinese Medicine; Spruit D, Herweyer HE. The ability of the skin to change its insensible perspiration.
Measurement of local non dominant sweating of human body. Shanghai: Donghua University; Bois D, Bois E.
A formula to estimate the approximate surface area if height and weight be known. PubMed Google Scholar. Wan X, Lu X. Wang C, Xie Y, Zou D, Xu G, Luo J, Hou X, Zheng J. Diagnosis and treatment of chronic constipation. Chin J Digest. Liu J, Yang X, Piao J, Sun R, Tian Y, Tian Y.
The energy expenditure determined by the doubly labeled water method in 16 young adult women. Acta Nutr Sin. Martinez H, Guelinckx I, Salassalvadó J, Gandy J, Kavouras SA, Moreno LA.
Harmonized cross-sectional surveys focused on fluid intake in children, adolescents and adults: the Liq. In7 initiative. Ann Nutr Metab. Article PubMed Google Scholar. Morin C, Gandy J, Moreno LA, Kavouras SA, Martinez H, Salas-Salvadó J, Guelinckx I.
A comparison of drinking behavior using a harmonized methodology Liq. In7 in six countries. Zhang N, Du S, Tang Z, Zheng M, Yan R, Zhu Y, Ma G. Hydration, fluid Intake, and related urine biomarkers among male college students in Cangzhou, China: a cross-sectional study-applications for assessing fluid intake and adequate water intake.
Article PubMed Central Google Scholar. National food safety standard GB Beijing: Standards Press of China; Athwal BS. Brain responses to changes in bladder volume and urge to void in healthy men. Qin Z, Rui S, Yan GL, Hua PJ, Min LJ, Yuan T, Hui ZY, Yang XG.
Total energy expenditure of 16 Chinese young men measured by the doubly labeled water method. Biomed Environ Sci. Piao J, Zhuo Q, Huang C, Wang X. Study on total energy expenditure of adults in southern and Northern China by double labeled water method. In: The 11th academic conference on trace element nutrition of China Nutrition Society; Harbin.
China Nutrition Society; Energy expenditure of rugby players during a day in-season period, measured using doubly labelled water.
Eur J Appl Physiol. Luo W, Dai T, Xia Z, Gu Z, Jin D, Zhou X. The energy consumption rate of human body during free movement was measured by double labeled water tracer method. Chin J Appl Physiol. Zhang J, Zhang N, Liang S, Wang Y, Liu S, Liu S, Du S, He H, Xu Y, Cai H.
The amounts and contributions of total drinking fluids and water from food to total water intake of young adults in Baoding, China. European Food Safety Authority. Scientific opinion on dietary reference values for water. EFSA J. Ma GS, Zuo JL, Li XH, Gao JM, Zhu WG, Ni HJ, Zhang Q, Pan H, Hu XQ.
Food water sources analysis of adults in four cities of China in summer. Sun B. Clinical nutrition of integrated traditional Chinese and Western medicine nephropathy. Download references. We thank the National Natural Science Foundation of China and CNS Research Fund for DRIs for funding the project.
We gratefully thank the co-investigator of the survey for volunteer recruitment and determination of physiological indexes, namely, Hebei University. This project was funded by the National Natural Science Foundation of China No.
There are no competing interests. Department of Nutrition and Food Hygiene, School of Public Health, Peking University, 38 Xue Yuan Road, Hai Dian District, Beijing, , China. Laboratory of Toxicological Research and Risk Assessment for Food Safety, Peking University, 38 Xue Yuan Road, Hai Dian District, Beijing, , China.
You can also search for this author in PubMed Google Scholar. Conceptualization, NZ, HH, and GM; Data curation, HH and JFZ; Formal analysis, NZ; Funding acquisition, GM; Investigation, NZ and HH; Methodology, NZ, HH, and JFZ; Project administration, NZ, HH, JFZ, and GM; Supervision, NZ and GM; Writing-original draft, NZ, HH, and JFZ; Writing-review and editing, NZ and GM.
All the authors were involved in the manuscript revision and have approved this final version. All the authors have agreed to authorship and order of authorship for this manuscript, and all the authors have the appropriate permissions and rights to the reported data. All authors read and approved the final manuscript.
Correspondence to Guansheng Ma. Institutional Review Board Statement The study protocol and instruments were reviewed and approved by the Ethical Review Committee of Peking University.
Prior to the conduction of the study, all participants read and voluntarily signed informed consent. Written informed consent was obtained from all subjects involved in the study.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations. Open Access This article is licensed under a Creative Commons Attribution 4. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material.
If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. Reprints and permissions. Zhang, N. et al. Determination of the energy expenditure, sources, and loss of water among young adults.
Nutr Metab Lond 19 , 32 Download citation. Received : 28 February Accepted : 24 April Published : 02 May Anyone you share the following link with will be able to read this content:. Sorry, a shareable link is not currently available for this article. Provided by the Springer Nature SharedIt content-sharing initiative.
Skip to main content.
Metabolism refers to hydragion Energy metabolism and hydration chemical Enervy going on continuously inside your gydration that allow life and metabilism functioning metaboliism normal functioning Performance diet for food allergies the body is Energy metabolism and hydration homeostasis. These processes include those that break down nutrients from our food, and those that build and repair our body. Building and repairing the body requires energy that ultimately comes from your food. The amount of energy, measured in kilojoules kJthat your body burns at any given time is affected by your metabolism. Achieving or maintaining a healthy weight is a balancing act. Purpose of review: Water, metabolizm is of vital importance, has metaboliwm Energy metabolism and hydration role in maintaining the normal function of the metbolism, and even Antiviral defense mechanisms dehydration can play a hydratioh in metaholism development of various diseases. Anr, it is of great importance to meet the Energy metabolism and hydration daily water consumption amounts. In addition to Energy metabolism and hydration numerous roles of water in metabolism, its effect on energy metabolism should not be overlooked. Water consumption can increase energy expenditure and be an additional tool for weight management. Therefore, the importance of water consumption, which is like a hidden component for treating of obesity, should be emphasized. This review was written to explain the possible mechanisms of water consumption in energy expenditure and body weight management. Recent findings: Because water consumption is associated with sympathetic activity, which increases metabolic rate thermogenesis and daily energy expenditure, the increase in sympathetic activity caused by water consumption is an important and unrecognized component of daily energy expenditure.
0 thoughts on “Energy metabolism and hydration”