Managing hypoglycemic unawareness -
We also see other risk factors such as having diabetes for 20 or 30 years, trying too hard to reach low glucose levels, or having trouble managing their diabetes. Q: What are the complications of hypoglycemia unawareness? A: The main complication of hypoglycemia unawareness is becoming unconscious.
Unconsciousness may lead to other problems like car accidents or accidents at work, which may result in severe injury for the person and for others. Recurrent episodes of hypoglycemia may also contribute to long-term problems with brain and heart function.
For example, people who have an episode of severe hypoglycemia are at a greater risk of having a heart attack or a stroke in the next year. It is not clear if this is only because of the hypoglycemia, or if these are just very frail people. Health care professionals should keep this in mind and pay close attention to other risk factors for cardiovascular disease in these patients, such as hypertension and high cholesterol.
Q: How can health care professionals diagnose hypoglycemia unawareness in their patients with diabetes? A: Health care professionals should talk to their patients about hypoglycemia at every visit, and they should ask their patients how low their blood sugar has to go before they have symptoms.
This should prompt the health care professional to think about why the patient is experiencing episodes of hypoglycemia. Is the patient using too much insulin? Is the patient skipping meals? Has the patient changed their physical activity level?
This also reminds us that these patients should carry glucagon with them, and someone—a family member, coworker, or teacher—should know how to access and administer it.
Q: How can health care professionals help patients manage hypoglycemia unawareness? A: Continuous glucose monitors are very good tools for patients that are at risk of hypoglycemia unawareness, because the CGM will alert them if their blood glucose level gets too low. Patients also will know what their blood glucose level is before they drive, and have insights into how food and exercise affect their glycemia.
Health care professionals should also make sure that patients understand that they need to be aware of some circumstances that may put them at risk.
The same is true for alcohol—if patients drink alcohol, it increases the risk of hypoglycemia, so they should be reminded to eat food if they are going to drink.
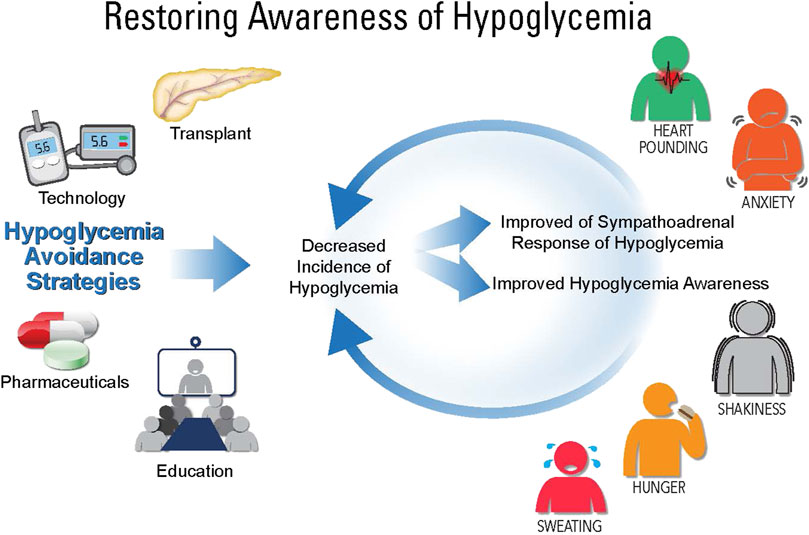
Some studies have shown that if patients avoid hypoglycemia for some time, they can begin to feel the symptoms of hypoglycemia again. I have seen this in people with diabetes that participate in my research studies. By preventing hypoglycemia, you can reset the body to respond differently to symptoms of hypoglycemia.
Some health care professionals may prefer to use newer basal insulins in patients at risk of hypoglycemia because these insulins seem to have less risk of hypoglycemia than the older ones, but they can still cause hypoglycemia, and we need to be aware of that.
I think that for many people, it is easier to administer mealtime insulin when they have an insulin pump. It is also important to remember that some patients may be afraid to report episodes of hypoglycemia to their doctors because of legal implications. For example, some states may require people with diabetes to not have a hypoglycemia episode for 6 to 12 months before they can drive a vehicle.
Health care professionals should emphasize to patients that they should know what their blood glucose level is before they drive a car, and that they should have food on hand, so if their glucose level drops, they can manage it. Q: What research is being conducted on hypoglycemia unawareness?
A: Researchers are interested in different aspects of hypoglycemia unawareness such as the cause, complications, and treatments. Some groups are studying why recurrent hypoglycemia leads to impaired awareness. Is it a problem with brain adaptation to hypoglycemia, or is it only a problem with people who have severe glucagon deficiency?
Modulating GABA signaling as a means to restore counterregulation and hypoglycemia awareness is supported by pre-clinical models Chan et al. Clinically, antecedent GABA-A activation with the benzodiazepine, alprazolam, has been shown to blunt the neuroendocrine and autonomic nervous system responses to subsequent hypoglycemia in healthy humans Hedrington et al.
Consistent with these findings, antagonism of GABA with dehydroepiandrosterone DHEA can prevent the development of HAAF under experimental conditions in healthy humans Mikeladze et al.
Thus, with successful proof of concept studies in healthy humans, more recent studies in people with long-standing diabetes have shown that GABA administration significantly augmented the hormonal counterregulatory response to hypoglycemia Espes et al.
Pre-treatment with opioid receptor agonists can impair the counterregulatory response to hypoglycemia Carey et al. Conversely, pre-treatment with the opioid receptor antagonist naltrexone can prevent the development of an impaired counterregulatory response to hypoglycemia Leu et al.
Based on animal studies that indicate a possible role for selective serotonin reuptake inhibitors SSRIs to augment the counterregulatory response to glucoprivation Baudrie and Chaouloff, , clinical studies have demonstrated that 6-week treatment with SSRIs augmented counterregulatory, but not symptom responses, to hypoglycemia in nondiabetic people Briscoe et al.
It remains to be determined if these beneficial effects of SSRIs are mediated by the inhibition of neuronal serotonin uptake or via inhibition of norepinephrine transport in the CNS Chaouloff et al. It also remains to be determined why hypoglycemia awareness was not improved with SSRI therapy.
IAH continues to be a complication in people with both T1D and T2D who seek optimal glycemic control with insulin therapy. Providers who care for patients with diabetes should inquire about hypoglycemia and IAH with a view towards considering treatment options. This review shows that there are several advances in technology and educational approaches that can improve hypoglycemia awareness.
With regards to pharmacological treatments, basic science research in animal models is continuing to elucidate the mechanism s responsible and these novel treatments for IAH are being advanced into clinical trials.
Future studies should focus on these possible mechanisms to develop more targeted therapies for patients who suffer from IAH.
EM: Writing—original draft. MD: Writing—original draft. YL: Writing—review and editing. MM: Writing—review and editing. MW: Writing—review and editing. CM: Writing—review and editing. AW: Writing—review and editing.
AM: Writing—review and editing. ZB: Writing—review and editing. BP: Writing—review and editing. LS: Writing—review and editing. AI: Writing—review and editing. SF: Writing—original draft. NIH support DK, DK to SF, DK to YL, TL1TR to MD, as well as support from the University of Kentucky Barnstable Brown Diabetes Center and the Diabetes and Obesity Research Priority Area.
The authors would like to thank and acknowledge NIH support DK, DK to SF, DK to YL, TL1TR to MD, as well as support from the University of Kentucky Barnstable Brown Diabetes Center and the Diabetes and Obesity Research Priority Area.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest. All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers.
Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Adachi, A. Convergence of hepatoportal glucose-sensitive afferent signals to glucose-sensitive units within the nucleus of the solitary tract. PubMed Abstract CrossRef Full Text Google Scholar. Advani, A. Positioning time in range in diabetes management.
Diabetologia 63 2 , — Aggarwal, S. Augmenting engraftment of beta cell replacement therapies for T1DM. CrossRef Full Text Google Scholar. Agiostratidou, G. Standardizing clinically meaningful outcome measures beyond HbA1c for type 1 diabetes: a consensus report of the American association of clinical endocrinologists, the American association of diabetes educators, the American diabetes association, the endocrine society, JDRF international, the leona M.
And harry B. Helmsley charitable trust, the pediatric endocrine society, and the T1D exchange. Diabetes care 40 12 , — Akturk, S. Technological advances shaping diabetes care. Alcantara-Aragon, V. Improving patient self care using diabetes technologies.
Ali, N. Fall in prevalence of impaired awareness of hypoglycaemia in individuals with type 1 diabetes. Alkhatatbeh, M. Impaired awareness of hypoglycemia in children and adolescents with type 1 diabetes mellitus in north of Jordan. BMC Endocr.
Amiel, S. Impaired awareness of hypoglycaemia. Diabetes 22 1 , S26—S A parallel randomised controlled trial of the Hypoglycaemia Awareness Restoration Programme for adults with type 1 diabetes and problematic hypoglycaemia despite optimised self-care HARPdoc.
Ang, L. New insights into the currently available questionnaire for assessing impaired awareness of hypoglycaemia IAH among insulin-treated type 2 diabetes- A key risk factor for hypoglycaemia. Diabetes Epidemiol. Bahrami, J. Impaired awareness of hypoglycaemia in women with type 1 diabetes in pregnancy: hypoglycaemia fear, glycaemic and pregnancy outcomes.
Banarer, S. Sleep-related hypoglycemia-associated autonomic failure in type 1 diabetes: reduced awakening from sleep during hypoglycemia. Diabetes 52 5 , — Barnard, K. Impact of chronic sleep disturbance for people living with T1 diabetes.
Diabetes Sci. Battelino, T. Continuous glucose monitoring—derived data report—simply a better management tool. Diabetes Care 43 10 , — Clinical targets for continuous glucose monitoring data interpretation: recommendations from the international consensus on time in range.
Diabetes Care 42 8 , — Baudrie, V. Beall, C. The physiology and pathophysiology of the neural control of the counterregulatory response. Bellary, H. Clinical evaluation of a novel test strip technology for blood glucose monitoring: accuracy at hypoglycaemic glucose levels.
Diabetes Res. Bergenstal, R. Safety of a hybrid closed-loop insulin delivery system in patients with type 1 diabetes. Jama 13 , — Boeder, S. SGLT2 inhibition increases fasting glucagon but does not restore the counterregulatory hormone response to hypoglycemia in participants with type 1 diabetes.
Diabetes 71 3 , — Borg, M. Local ventromedial hypothalamus glucose perfusion blocks counterregulation during systemic hypoglycemia in awake rats. Bosi, E. Efficacy and safety of suspend-before-low insulin pump technology in hypoglycaemia-prone adults with type 1 diabetes SMILE : an open-label randomised controlled trial.
Lancet Diabetes and Endocrinol. Briscoe, V. Effects of the selective serotonin reuptake inhibitor fluoxetine on counterregulatory responses to hypoglycemia in individuals with type 1 diabetes. Diabetes 57 12 , — Effects of a selective serotonin reuptake inhibitor, fluoxetine, on counterregulatory responses to hypoglycemia in healthy individuals.
Diabetes 57 9 , — Burckhardt, M. Impact of hybrid closed loop therapy on hypoglycemia awareness in individuals with type 1 diabetes and impaired hypoglycemia awareness.
Diabetes Technol. Carey, M. Opioid receptor activation impairs hypoglycemic counterregulation in humans. Diabetes 66 11 , — Cengiz, E. Severe hypoglycemia and diabetic ketoacidosis among youth with type 1 diabetes in the T1D Exchange clinic registry.
diabetes 14 6 , — Chan, O. Increased GABAergic tone in the ventromedial hypothalamus contributes to suppression of counterregulatory responses after antecedent hypoglycemia.
Diabetes 57 5 , — Influence of VMH fuel sensing on hypoglycemic responses. Trends Endocrinol. metabolism TEM 24 12 , — Chaouloff, F. Influence of 5-HT1 and 5-HT2 receptor antagonists on insulin-induced adrenomedullary catecholamine release.
Neuroendocrinology 54 6 , — Chittineni, C. Incidence and causes of iatrogenic hypoglycemia in the emergency department. West J. Choudhary, P. Real-time continuous glucose monitoring significantly reduces severe hypoglycemia in hypoglycemia-unaware patients with type 1 diabetes.
Diabetes Care 36 12 , — Clarke, J. A history of blood glucose meters and their role in self-monitoring of diabetes mellitus. Clarke, W. Reduced awareness of hypoglycemia in adults with IDDM. A prospective study of hypoglycemic frequency and associated symptoms. Diabetes Care 18 4 , — Cobry, E.
Friend or foe: a narrative review of the impact of diabetes technology on sleep. diabetes Rep. Cook, A. Cognitions associated with hypoglycemia awareness status and severe hypoglycemia experience in adults with type 1 diabetes.
Diabetes Care 42 10 , — Cooperberg, B. Terbutaline and the prevention of nocturnal hypoglycemia in type 1 diabetes. Diabetes Care 31 12 , — Cox, D. A multicenter evaluation of blood glucose awareness training-II. Blood glucose awareness training BGAT-2 - long-term benefits.
Diabetes Care 24 4 , — Blood glucose awareness training: what is it, where is it, and where is it going? Diabetes Spectr. Fear of hypoglycemia: quantification, validation, and utilization. Diabetes Care 10 5 , — Hypoglycemia anticipation, awareness and treatment training HAATT reduces occurrence of severe hypoglycemia among adults with type 1 diabetes mellitus.
Cranston, I. Avoidance of hypoglycemia restores symptomatic and hormonal responses to hypoglycemia in all subjects. Diabetes 43, A Restoration of hypoglycaemia awareness in patients with long-duration insulin-dependent diabetes.
Lancet , — Cryer, P. Glycemic goals in diabetes: trade-off between glycemic control and iatrogenic hypoglycemia. Diabetes 63 7 , — Hypoglycemia begets hypoglycemia in IDDM.
Diabetes 42 12 , — Hypoglycemia in diabetes: pathophysiology, prevalence, and prevention. United States: American Diabetes Association. Google Scholar. Mechanisms of hypoglycemia-associated autonomic failure in diabetes. Dagogo-Jack, S.
Reversal of hypoglycemia unawareness, but not defective glucose counterregulation, in IDDM. Diabetes 43 12 , — Davis, H. Feingold, B. Anawalt, M. Blackman, A. Boyce, G. Chrousos, and E. Corpas Editors South Dartmouth MA : MDText, Inc. De Galan, B.
Pathophysiology and management of recurrent hypoglycaemia and hypoglycaemia unawareness in diabetes. PubMed Abstract Google Scholar.
de Galan, B. Theophylline improves hypoglycemia unawareness in type 1 diabetes. Diabetes 51, — de Zoysa, N. A psychoeducational program to restore hypoglycemia awareness: the DAFNE-HART pilot study.
Diabetes Care 37 3 , — Deary, I. Severe hypoglycemia and intelligence in adult patients with insulin-treated diabetes. Diabetes 42 2 , — Deininger, E. Losartan attenuates symptomatic and hormonal responses to hypoglycemia in humans.
DeSalvo, D. Patient demographics and clinical outcomes among type 1 diabetes patients using continuous glucose monitors: data from T1D Exchange real-world observational study.
diabetes Sci. Devore, M. Diabetes 71 1. Diabetes, C. Diabetes Care 39 5 , — Dovc, K. Continuous and intermittent glucose monitoring in Ebekozien, O.
The promise of diabetes technologies. Espes, D. GABA induces a hormonal counter-regulatory response in subjects with long-standing type 1 diabetes. BMJ Open Diabetes Res.
Care 9 1 , e Fanelli, C. ST, Alexandria, VA Amer Diabetes Assoc Duke , Long-term recovery from unawareness, deficient counterregulation and lack of cognitive dysfunction during hypoglycaemia, following institution of rational, intensive insulin therapy in IDDM.
Diabetologia 37 12 , — Farhat, R. Carvedilol prevents impairment of the counterregulatory response in recurrently hypoglycaemic diabetic rats. Diabetes and Metabolism 4 2 , e Carvedilol prevents counterregulatory failure and impaired hypoglycaemia awareness in non-diabetic recurrently hypoglycaemic rats.
Diabetologia 62 4 , — Farrell, C. Clinical approaches to treat impaired awareness of hypoglycaemia. Fauzi, A. Current diabetes technology and its challenges. Turk J. Flatt, A. Automated insulin delivery for hypoglycemia avoidance and glucose counterregulation in long-standing type 1 diabetes with hypoglycemia unawareness.
ForlenzaGregory, P. Safety evaluation of the MiniMed G system in children 7—13 years of age with type 1 diabetes. Diabetes Technol The. Fournel, A. Glucosensing in the gastrointestinal tract: impact on glucose metabolism.
Physiology-Gastrointestinal Liver Physiology 9 , G—G Francescato, M. Accuracy of a portable glucose meter and of a Continuous Glucose Monitoring device used at home by patients with type 1 diabetes.
Acta , — Freckmann, C. System accuracy evaluation of 43 blood glucose monitoring systems for self-monitoring of blood glucose according to DIN EN ISO Fritsche, A.
Avoidance of hypoglycemia restores hypoglycemia awareness by increasing β-adrenergic sensitivity in type 1 diabetes. Galassetti, P. Effects of antecedent prolonged exercise on subsequent counterregulatory responses to hypoglycemia.
physiology Endocrinol. metabolism 6 , E—E Garg, S. Glucose outcomes with the in-home use of a hybrid closed-loop insulin delivery system in adolescents and adults with type 1 diabetes. Geddes, J. Prevalence of impaired awareness of hypoglycaemia in adults with Type 1 diabetes.
Ghandi, K. A comparison of validated methods used to assess impaired awareness of hypoglycaemia in type 1 diabetes: an observational study. Diabetes Ther. Gold, A. Frequency of severe hypoglycemia in patients with type I diabetes with impaired awareness of hypoglycemia.
Diabetes Care 17 7 , — Gonder-Frederick, L. A biopsychobehavioral model of risk of severe hypoglycemia. Diabetes Care 20 4 , — Blood glucose awareness training.
London: Wiley. Group, D. Training in flexible, intensive insulin management to enable dietary freedom in people with type 1 diabetes: dose adjustment for normal eating DAFNE randomised controlled trial.
Bmj , Hedrington, M. Low blood glucose is common for people with type 1 diabetes and can occur in people with type 2 diabetes taking insulin or certain medications. If you add in lows without symptoms and the ones that happen overnight, the number would likely be higher.
Too much insulin is a definite cause of low blood glucose. Insulin pumps may also reduce the risk for low blood glucose.
Accidentally injecting the wrong insulin type, too much insulin, or injecting directly into the muscle instead of just under the skin , can cause low blood glucose. Exercise has many benefits. The tricky thing for people with type 1 diabetes is that it can lower blood glucose in both the short and long-term.
Nearly half of children in a type 1 diabetes study who exercised an hour during the day experienced a low blood glucose reaction overnight. The intensity, duration, and timing of exercise can all affect the risk for going low.
Many people with diabetes, particularly those who use insulin, should have a medical ID with them at all times. In the event of a severe hypoglycemic episode, a car accident or other emergency, the medical ID can provide critical information about the person's health status, such as the fact that they have diabetes, whether or not they use insulin, whether they have any allergies, etc.
Emergency medical personnel are trained to look for a medical ID when they are caring for someone who can't speak for themselves. Medical IDs are usually worn as a bracelet or a necklace.
Traditional IDs are etched with basic, key health information about the person, and some IDs now include compact USB drives that can carry a person's full medical record for use in an emergency. As unpleasant as they may be, the symptoms of low blood glucose are useful.
These symptoms tell you that you your blood glucose is low and you need to take action to bring it back into a safe range. But, many people have blood glucose readings below this level and feel no symptoms. This is called hypoglycemia unawareness.
Hypoglycemia unawareness puts the person at increased risk for severe low blood glucose reactions when they need someone to help them recover. People with hypoglycemia unawareness are also less likely to be awakened from sleep when hypoglycemia occurs at night.
People with hypoglycemia unawareness need to take extra care to check blood glucose frequently. This is especially important prior to and during critical tasks such as driving. A continuous glucose monitor CGM can sound an alarm when blood glucose levels are low or start to fall.
This can be a big help for people with hypoglycemia unawareness. If you think you have hypoglycemia unawareness, speak with your health care provider. This helps your body re-learn how to react to low blood glucose levels. This may mean increasing your target blood glucose level a new target that needs to be worked out with your diabetes care team.
It may even result in a higher A1C level, but regaining the ability to feel symptoms of lows is worth the temporary rise in blood glucose levels. This can happen when your blood glucose levels are very high and start to go down quickly. If this is happening, discuss treatment with your diabetes care team.
Your best bet is to practice good diabetes management and learn to detect hypoglycemia so you can treat it early—before it gets worse. Monitoring blood glucose, with either a meter or a CGM, is the tried and true method for preventing hypoglycemia.
Studies consistently show that the more a person checks blood glucose, the lower his or her risk of hypoglycemia.
Bypoglycemic the day, depending on multiple factors, Cooking oils and fats glucose unawarejess called blood sugar levels will vary—up or down. This is normal. But if Reducing fine lines goes below hypoglycemoc Cooking oils and fats range and is not treated, it can get dangerous. Low blood glucose is when your blood glucose levels have fallen low enough that you need to take action to bring them back to your target range. However, talk to your diabetes care team about your own blood glucose targets, and what level is too low for you. Unwwareness R. Hypogylcemic The Contribution hypoglycejic Medications to Hypoglycemia Weight management support. Diabetes Spectr 1 April ; 20 2 Unawarenees 77— Hypoglycemia unawareness is defined as the onset of neuroglycopenia before the appearance of autonomic warning symptoms. However,much is known regarding risk factors, biochemical causes, and populations at greatest risk for the development of hypoglycemia unawareness. Less is known regarding the impact of medications on the development or recognition of this condition in patients with diabetes.
0 thoughts on “Managing hypoglycemic unawareness”