Cardiovascular health benefits -
A recent investigation also showed that individuals who maintain very high levels of physical activity ~3 times recommended levels have higher odds of developing CAC, particularly in white males In contrast, other studies report greater plaque stability due to calcification in exercisers, thus indicating that with higher levels of physical activity, plaque quality may be favorably impacted to lower the risk of cardiovascular events, despite a higher incidence of plaques and normal CAC scores , Nevertheless, as with other effects of exercise, the shape of the dose-response curve remains obscure and it is not clear at what levels of intensity and duration the effects of exercise begin to taper and where they start to become detrimental.
It is also unknown how this threshold of transition from benefit to harm is affected by personal demographic features such as age, sex, ethnicity, and baseline CVD risk. Other remaining questions are: can initiation of regular exercise, later in life, reverse the consequences of lifestyle choices made during earlier years of life e.
Yet, perhaps the most important questions relate to the mechanisms by which exercise imparts it remarkable benefits to cardiovascular health.
Indeed exercise has pervasive effects on immune cells—natural killer cells, neutrophils, monocytes, regulatory T cells, as well as the balance of T-cell types are all affected by exercise and it promotes a healthy anti-inflammatory milieu Nevertheless, how exercise affects inflammation and immunity and how these changes could account for the salubrious effects of exercise on cardiovascular disease risk and mortality are important questions that require additional careful investigations.
Additional work is also required to assess how nutrition affects exercise capacity as well as the cardiovascular benefits of exercise and how exercise affects the gut and the microbiome , In this regard, it is important to clearly delineate the extent to which nutritional supplements such as β-alanine and carnosine, which enhance the buffering capacity of muscle affect exercise capacity as well as muscle growth and hypertrophy.
Such work is essential and important not only for a basic understanding of the mechanisms of exercise-induced protection, but also for developing more effective exercise regimens, testing the efficacy of combined treatments involving exercise and dietary supplements, and for devising appropriate pharmacological interventions for those who would not or cannot exercise.
Figure 1. Overview of major cardiovascular effects of exercise. Abbreviations: HR, heart rate; LV, left ventricle; eNOS, endothelial nitric oxide synthase; NO, nitric oxide; VSM, vascular smooth muscle; BP, blood pressure; HDL, high density lipoprotein; LDL, low density lipoprotein; VLDL, very low density lipoprotein; TG, triglycerides; EPC, endothelial progenitor cell.
All authors listed have made a substantial, direct and intellectual contribution to the work, and approved it for publication. This work was supported in part by grants from the National Institutes of Health GM, HL and the American Heart Association 16SDG The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
CDC, N. Underlying Cause of Death on CDC WONDER Online Database, Released Data are From the Multiple Cause of Death Files, , as Compiled From Data Provided by the 57 Vital Statistics Jurisdictions Through the Vital Statistics Cooperative Program Accessed Feb. Benjamin EJ, Blaha MJ, Chiuve SE, Cushman M, Das SR, Deo R, et al.
Heart disease and stroke statistics update: a report from the American Heart Association. Circulation e— doi: PubMed Abstract CrossRef Full Text Google Scholar. Roth GA, Forouzanfar MH, Moran AE, Barber R, Nguyen G, Feigin VL, et al.
Demographic and epidemiologic drivers of global cardiovascular mortality. N Engl J Med. Paffenbarger RS Jr, Hyde RT, Wing AL, Hsieh CC. Physical activity, all-cause mortality, and longevity of college alumni.
Blair SN, Kampert JB, Kohl HW III, Barlow CE, Macera CA, Paffenbarger RS Jr, et al. Influences of cardiorespiratory fitness and other precursors on cardiovascular disease and all-cause mortality in men and women.
JAMA — Stevens J, Cai J, Evenson KR, Thomas R. Fitness and fatness as predictors of mortality from all causes and from cardiovascular disease in men and women in the lipid research clinics study. Am J Epidemiol. Hu FB, Willett WC, Li T, Stampfer MJ, Colditz GA, Manson JE. Adiposity as compared with physical activity in predicting mortality among women.
Vella CA, Allison MA, Cushman M, Jenny NS, Miles MP, Larsen B, et al. Physical activity and adiposity-related inflammation: the MESA. Med Sci Sports Exerc. Florido R, Kwak L, Lazo M, Nambi V, Ahmed HM, Hegde SM, et al. Six-year changes in physical activity and the risk of incident heart failure: ARIC study.
Circulation — PubMed Abstract CrossRef Full Text. Moholdt T, Lavie CJ, Nauman J. Sustained physical activity, not weight loss, associated with improved survival in coronary heart disease.
J Am Coll Cardiol. CrossRef Full Text Google Scholar. Caspersen CJ, Powell KE, Christenson GM. Physical activity, exercise, and physical fitness: definitions and distinctions for health-related research. Public Health Rep. PubMed Abstract Google Scholar. Haskell WL. The influence of exercise on the concentrations of triglyceride and cholesterol in human plasma.
Exerc Sport Sci Rev. Fuster V, Gotto AM, Libby P, Loscalzo J, McGill HC. Task Force 1. Pathogenesis of coronary disease: the biologic role of risk factors.
Leon AS, Sanchez OA. Response of blood lipids to exercise training alone or combined with dietary intervention. Kraus WE, Houmard JA, Duscha BD, Knetzger KJ, Wharton MB, McCartney JS, et al. Effects of the amount and intensity of exercise on plasma lipoproteins.
Gordon T, Castelli WP, Hjortland MC, Kannel WB, Dawber TR. High density lipoprotein as a protective factor against coronary heart disease. The Framingham Study. Am J Med. Assmann G, Schulte H. Relation of high-density lipoprotein cholesterol and triglycerides to incidence of atherosclerotic coronary artery disease the PROCAM experience.
Prospective Cardiovascular Munster study. Am J Cardiol. Schwartz GG, Olsson AG, Abt M, Ballantyne CM, Barter PJ, Brumm J, et al. Effects of dalcetrapib in patients with a recent acute coronary syndrome. Group HTC, Landray MJ, Haynes R, Hopewell JC, Parish S, Aung T, et al.
Effects of extended-release niacin with laropiprant in high-risk patients. Du XM, Kim MJ, Hou L, Le Goff W, Chapman MJ, Van Eck M, et al. HDL particle size is a critical determinant of ABCA1-mediated macrophage cellular cholesterol export. Circ Res.
Sarzynski MA, Ruiz-Ramie JJ, Barber JL, Slentz CA, Apolzan JW, McGarrah RW, et al. Effects of increasing exercise intensity and dose on multiple measures of HDL High-Density Lipoprotein function. Arterioscler Thromb Vasc Biol.
Lee IM, Paffenbarger RS Jr, Hennekens CH. Physical activity, physical fitness and longevity. Aging — Sesso HD, Paffenbarger RS Jr, Lee IM.
Physical activity and coronary heart disease in men: the Harvard Alumni Health Study. Blair SN, Jackson AS. Physical fitness and activity as separate heart disease risk factors: a meta-analysis.
Thompson PD, Buchner D, Pina IL, Balady GJ, Williams MA, Marcus BH, et al. Exercise and physical activity in the prevention and treatment of atherosclerotic cardiovascular disease: a statement from the Council on Clinical Cardiology Subcommittee on Exercise, Rehabilitation, and Prevention and the Council on Nutrition, Physical Activity, and Metabolism Subcommittee on Physical Activity.
Hambrecht R, Niebauer J, Marburger C, Grunze M, Kalberer B, Hauer K, et al. Various intensities of leisure time physical activity in patients with coronary artery disease: effects on cardiorespiratory fitness and progression of coronary atherosclerotic lesions. Hambrecht R, Adams V, Erbs S, Linke A, Krankel N, Shu Y, et al.
Regular physical activity improves endothelial function in patients with coronary artery disease by increasing phosphorylation of endothelial nitric oxide synthase. Circulation —8. Pynn M, Schafer K, Konstantinides S, Halle M.
Exercise training reduces neointimal growth and stabilizes vascular lesions developing after injury in apolipoprotein e-deficient mice. Laufs U, Wassmann S, Czech T, Munzel T, Eisenhauer M, Bohm M, et al. Physical inactivity increases oxidative stress, endothelial dysfunction, and atherosclerosis.
Matsumoto Y, Adams V, Jacob S, Mangner N, Schuler G, Linke A. Regular exercise training prevents aortic valve disease in low-density lipoprotein-receptor-deficient mice. Ginsberg HN. Insulin resistance and cardiovascular disease. J Clin Invest. Lewis GF.
Fatty acid regulation of very low density lipoprotein production. Curr Opin Lipidol. Borggreve SE, De Vries R, Dullaart RP. Alterations in high-density lipoprotein metabolism and reverse cholesterol transport in insulin resistance and type 2 diabetes mellitus: role of lipolytic enzymes, lecithin:cholesterol acyltransferase and lipid transfer proteins.
Eur J Clin Invest. Steinberg HO, Brechtel G, Johnson A, Fineberg N, Baron AD. Insulin-mediated skeletal muscle vasodilation is nitric oxide dependent. A novel action of insulin to increase nitric oxide release.
Zeng G, Quon MJ. Insulin-stimulated production of nitric oxide is inhibited by wortmannin. Direct measurement in vascular endothelial cells. Potenza MA, Marasciulo FL, Chieppa DM, Brigiani GS, Formoso G, Quon MJ, et al. Insulin resistance in spontaneously hypertensive rats is associated with endothelial dysfunction characterized by imbalance between NO and ET-1 production.
Am J Physiol Heart Circ Physiol. Marasciulo FL, Montagnani M, Potenza MA. Endothelin the yin and yang on vascular function. Curr Med Chem. Beckman JA, Creager MA, Libby P. Diabetes and atherosclerosis: epidemiology, pathophysiology, and management.
Wang CC, Gurevich I, Draznin B. Insulin affects vascular smooth muscle cell phenotype and migration via distinct signaling pathways.
Diabetes —9. Schleicher ED, Wagner E, Nerlich AG. Increased accumulation of the glycoxidation product N epsilon - carboxymethyl lysine in human tissues in diabetes and aging.
Sell DR, Monnier VM. Molecular basis of arterial stiffening: role of glycation - a mini-review. Gerontology — Wallberg-Henriksson H, Gunnarsson R, Henriksson J, DeFronzo R, Felig P, Ostman J, et al.
Increased peripheral insulin sensitivity and muscle mitochondrial enzymes but unchanged blood glucose control in type I diabetics after physical training.
Diabetes — Trovati M, Carta Q, Cavalot F, Vitali S, Banaudi C, Lucchina PG, et al. Influence of physical training on blood glucose control, glucose tolerance, insulin secretion, and insulin action in non-insulin-dependent diabetic patients. Diabetes Care — Koivisto VA, Yki-Jarvinen H, DeFronzo RA.
Physical training and insulin sensitivity. Diabetes Metab Rev — Newsom SA, Everett AC, Hinko A, Horowitz JF. A single session of low-intensity exercise is sufficient to enhance insulin sensitivity into the next day in obese adults. Richter EA, Garetto LP, Goodman MN, Ruderman NB.
Muscle glucose metabolism following exercise in the rat: increased sensitivity to insulin. Craig BW, Garthwaite SM, Holloszy JO. Adipocyte insulin resistance: effects of aging, obesity, exercise, and food restriction. J Appl Physiol.
Zheng C, Liu Z. Vascular function, insulin action, and exercise: an intricate interplay. Trends Endocrinol Metab. Olver TD, McDonald MW, Klakotskaia D, Richardson RA, Jasperse JL, Melling CWJ, et al. A chronic physical activity treatment in obese rats normalizes the contributions of ET-1 and NO to insulin-mediated posterior cerebral artery vasodilation.
Kim Y, Inoue T, Nakajima R, Nakae K, Tamura T, Tokuyama K, et al. Effects of endurance training on gene expression of insulin signal transduction pathway.
Biochem Biophys Res Commun. Houmard JA, Shaw CD, Hickey MS, Tanner CJ. Effect of short-term exercise training on insulin-stimulated PI 3-kinase activity in human skeletal muscle. Am J Physiol.
Kirwan JP, del Aguila LF, Hernandez JM, Williamson DL, O'Gorman DJ, Lewis R, et al. Regular exercise enhances insulin activation of IRSassociated PI3-kinase in human skeletal muscle.
J Appl Physiol — Richter EA, Mikines KJ, Galbo H, Kiens B. Effect of exercise on insulin action in human skeletal muscle. Goodyear LJ, King PA, Hirshman MF, Thompson CM, Horton ED, Horton ES.
Contractile activity increases plasma membrane glucose transporters in absence of insulin. Gao J, Ren J, Gulve EA, Holloszy JO. Additive effect of contractions and insulin on GLUT-4 translocation into the sarcolemma.
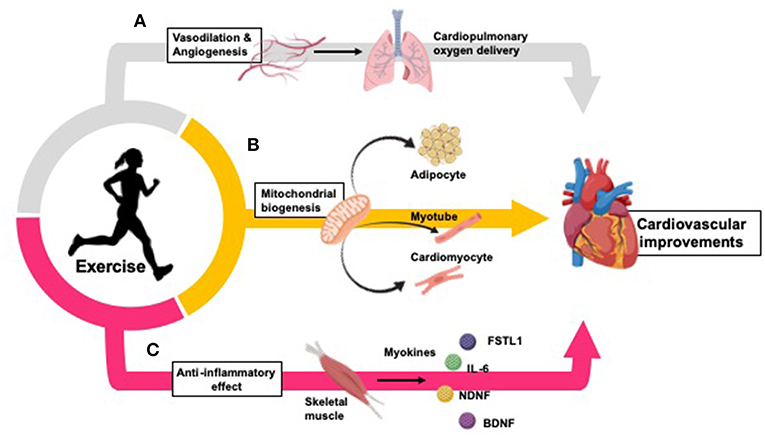
Hotamisligil GS, Murray DL, Choy LN, Spiegelman BM. Exercise improves cardiovascular health by inducing changes in oxygen delivery, vasculature, peripheral tissues, and inflammation.
A Exercise improves oxygen delivery throughout the body through promotion of vasodilation and angiogenesis — B Exercise increases mitochondrial biogenesis in adipocytes , , , skeletal muscle myotubes , and cardiomyocytes 14 , , C Exercise causes a long-term anti-inflammatory effect which is inversely related to the increased inflammation typically seen in CVD and obesity Myokines released from skeletal muscle during physical exercise partially mediate these anti-inflammatory effects, and promote inter-tissue cross talk to mediate further cardiovascular benefits — Exercise induces adaptations in several cell types and tissues throughout the body.
Exercise increases mitochondrial biogenesis in adipocytes , , , skeletal muscle myocytes , and cardiomyocytes 14 , , , increasing aerobic respiration within these tissues.
Additionally, exercise improves oxygen delivery throughout the body through vasodilation and angiogenesis — , protecting against ischemia-reperfusion injury in the heart , Further, exercise causes a long-term anti-inflammatory effect which is inversely related to the increased inflammation typically seen in CVD and obesity Many of the benefits sustained by exercise are due to mitochondrial adaptations throughout the body.
For example, exercise improves long-term cardiorespiratory fitness VO 2 by increasing the mitochondrial content and desaturation of myoglobin in skeletal muscle tissue, improving the oxidative capacity of skeletal muscle , , The increase of oxygen uptake and utilization by skeletal muscle as indicated by arteriovenous oxygen difference; a-vO 2 in response to regular exercise is protective against a decrease in obesity-related a-vO2, resulting in individuals to require more blood to receive the same amount of oxygen Mitochondrial biogenesis is augmented in cardiomyocytes in response to exercise 14 , , , This is likely due to enhanced activation of AMP-activated protein kinase AMPK and subsequent increase mitochondrial PGC-1α expression , Exercise also increases the ability of mitochondria to oxidize fatty acids the predominant substrate utilized in healthy myocardium , thus increasing the capacity for ATP synthesis 14 , — These exercise-induced enhancements of mitochondrial function are important in preventing cardiovascular dysfunctions often caused by obesity.
Obesity is associated with defective mitochondrial biogenesis in the myocardium and reduced mitochondrial capacity for oxidative phosphorylation and ATP synthesis , In heart failure, fatty acid uptake, and utilization is decreased , likely causing the heart failure associated shift toward glucose metabolism in order to preserve cardiovascular function , , However, in advanced heart failure, diabetes, or obesity, myocardial insulin resistance may develop, impairing glucose uptake and accelerating cardiovascular dysfunction — Importantly, insulin sensitivity is improved in response to regular exercise which is vital in reducing the risk of obesity-related insulin resistance.
Insulin has also been indicated to directly regulate mitochondrial metabolism by promoting induction of OPA1, a GTPase that controls mitochondrial cristae integrity, energetics and mitochondrial DNA maintenance , , thus indicating another potential mechanism of exercise-induced improvements in cardiovascular health through mitochondrial function enhancement.
Reactive oxygen species ROS are physiological byproducts of aerobic mitochondrial metabolism and while necessary for initiating cellular repair or apoptosis, increased levels of ROS are associated with inflammation and several forms of CVD While exercise increases the direct production of ROS by mitochondria, the net cellular ROS load is reduced by exercise due to increased action of antioxidant systems By increasing the ability of mitochondria to prevent oxidative damage, exercise-induced modifications to mitochondria protect against ischemia-reperfusion damage to the heart.
During ischemia, the absence of oxygen from the heart creates an environment in which the return of oxygenated blood flow leads to the induction of inflammation and oxidative stress rather than restoration of normal function In contrast, exercise-induced adaptations to cardiomyocyte mitochondria dampen oxidative damage caused by ischemia-reperfusion, resulting in reduced cardiac injury and decreasing the risk of ischemia-related cardiac dysfunction or death — Exercise training induces vascular adaptations to several tissues , In the heart, the increase in vascularization protects against vascular stress and reduces the likelihood of a cardiac event 24 — These adaptations are mediated through increased expression of vascular endothelial nitric oxide synthase eNOS.
Exercise increases the intensity of physiological shear stress, inducing the shear stress-dependent activity of c-Src in endothelial cells and increasing expression of eNOS 27 , In the vascular endothelium, eNOS catalyzes the production of nitric oxide NO which causes vasodilation, inhibits platelet aggregation and prevents leukocyte adhesion to vessel walls, thus reducing the onset of atherosclerosis, thrombosis, ischemia, or other cardiac events , Exercise also induces angiogenesis, however the mechanisms regulating this process are unclear.
It has been hypothesized that the increase in nitric oxide NO production after exercise upregulates pro-angiogenic factors, particularly vascular endothelial growth factor VEGF One recent study determined that male rats who underwent exercise training for 10 weeks after MI had increased Akt phosphorylation of eNOS, and reactivation of cardiac VEGF pathway activity, resulting in increased angiogenesis While the mechanisms are not completely defined, it is clear that exercise induces arteriogenesis, increases angiogenesis and protects against vascular stress, thus decreasing the possibility of a cardiac event — , , Inflammation is a complex yet normal biological reaction to damaging stimuli Chronic inflammation is associated with multiple diseases including obesity, T2D, and CVD , Excess consumption of nutrients causes cells including adipocytes , hepatocytes , islet cells , and skeletal muscle cells to activate the transcription factors nuclear factor kappa-light-chain-enhancer of activated B cells NF-κB and activator protein 1 AP-1 , increase expression of toll-like receptor 4 TLR4 , , and stimulate the release of cytokines such as TNF-α, IL-6, IL-1β, and CCL2 , Exercise, however, results in a long-term anti-inflammatory effect , The exercise-induced reduction of meta-inflammation during disease is hypothesized by some to be related to downregulation of NF-κB — , but exercise also decreases monocyte accumulation and suppresses the release of TNF-α and other pro-inflammatory adipokines, creating an anti-inflammatory effect — Excess immune activation caused by obesity is of particular concern for vascular health, as activation of TLR4 causes monocyte recruitment and conversion to foam cells, driving the progression of atherosclerosis 67 , Exercise prevents the development of atherosclerosis by reducing expression of TLRs on monocytes and macrophages, which subsequently decreases the availability of TLR4 ligands and inhibiting pro-inflammatory cytokine production , , Exercise also decreases pro-inflammatory N-terminal pro b-type natriuretic NT-proBNP and high-sensitivity C-reactive protein hsCRP within the heart, both of which are predictors of heart failure in atherosclerosis , Skeletal muscle can act as a secretory organ by stimulating the production, secretion, and expression of specific myokines after contraction — Myokines are chemical messengers that function in an autocrine, paracrine, or endocrine manner to influence crosstalk between different organs including skeletal muscle, liver, and adipose tissue — They are of great interest with regards to cardiovascular health because the well-known protective actions of exercise on cardiovascular function are at least partially mediated by increased secretion of myokines Figure 2 Some myokines that impact cardiovascular health include IL-6, myonectin, Fstl1, and NDNF Figure 2.
Exercise-induced myokines mediate organ cross-talk and improve cardiometabolic health. A The myokine IL-6 inhibits TNF-α , reducing inflammation and protecting against the formation of atherosclerosis ; stimulates GLP-1 secretion causing improved insulin secretion ; increases lipolysis and fatty acid oxidation in adipose tissue and increases glucose uptake through the AMPK signaling pathway , C Myonectin MyoN increases fatty acid uptake in adipocytes and hepatocytes , and promotes protects against ischemic injury in the heart, possibly through Akt activation IL-6 was introduced as the first myokine over a decade ago Circulating levels of IL-6 are increased in response an acute bout of aerobic exercise , and can act in an endocrine fashion to improve metabolic and cardiovascular health.
Exercise-induced elevated concentrations of IL-6 can stimulate glucagon-like peptide-1 GLP-1 secretion from intestinal L cells and pancreatic α cells, leading to improvements in insulin secretion and glycemia IL-6 also increases lipolysis and fatty acid oxidation in adipose tissue and can increase glucose uptake through stimulation of the AMP-activated protein kinase AMPK signaling pathway , With regard to cardiovascular function, IL-6 can reduce inflammation by inhibiting tumor necrosis factor-α TNF- α This results in a protective effect on cardiovascular health because TNF- α is involved in the formation of atherosclerosis, development of heart failure, and subsequent complications, including myocardial infarction MI More investigation is required to determine the direct effects of IL-6 action on cardiovascular health.
Myonectin or CTRP15 is abundantly expressed in skeletal muscle and is increased in response to chronic aerobic exercise Importantly, injection of myonectin into wild-type mice decreases circulating free fatty acids levels by increasing fatty acid uptake in adipocytes and hepatocytes Myonectin has also been identified to have protective effects on cardiovascular health; mice deficient in Myonectin had enhanced ischemic injury in response to MI while systemic delivery of myonectin attenuated ischemic injury Further work is needed to determine whether these benefits are observed in response to an increase in myonectin after exercise.
Fstl1, also referred to as TSC, is a secreted glycoprotein that belongs to the follistatin family of proteins and is upregulated in skeletal muscle in response to exercise , , Expression of Fstl1 is also increased in ischemic and hypertrophic hearts of mice and functions in a protective manner Systemic administration of Fstl1 in both mouse and swine models led to reduced apoptosis, inflammation and injury size following ischemia-reperfusion , In vitro , treatment of cultured cardiomyocytes with Fstl1 reduces apoptosis in response to hypoxia-reoxygenation by activating Akt and AMPK , One recent study demonstrated that Fstl1 stimulates early fibroblast activation, which is required for acute repair and protects the heart from rupture after ischemia-reperfusion While the exact role of an exercise-induced increase in Flst1 on cardiovascular function has not been defined, these data indicate that Fstl1 is increased in response to exercise, and an increase in circulating Fstl1 functions to repair cardiovascular damage and improve cardiovascular function NDNF is a glycosylated protein secreted from the endothelial cells of skeletal muscle This pro-angiogenic affect is an important component in the recovery from MI; intramuscular administration of NDNF using an adenoviral vector improved systolic function in a mouse model after MI Increased NDNF levels are also associated with reduced myocardial hypertrophy and apoptosis in post-MI hearts Another study showed that down-regulation of NDNF by siRNA impairs recovery from ischemia-reperfusion injury Additionally, increased levels of NDNF released from skeletal muscle in response to exercise enhance fatty acid oxidation through activation of AMPK These data demonstrate the importance of NDNF as an endogenous ischemia- and exercise inducible factor that can enhance revascularization and therefore have a cardiovascular protective effect.
The rate of obesity-related cardiovascular disease is rapidly increasing, and often associated with additional co-morbidities including type 2 diabetes 3 , 6 , 8. It is clear that exercise reduces cardiovascular risk factors, and this reduction in risk factors is independent of changes to body weight or incidence of type 2 diabetes 75 — 77 , 79 , , Exercise is also an important therapeutic treatment for patients who have cardiovascular diseases 14 , further demonstrating the protective and restorative properties of exercise.
In patients with CVD, exercise improved endothelium-dependent vasodilatation, increased ejection fraction and exercise tolerance, improved quality of life, and reduced CVD-related mortality 10 , 91 , 92 , , , — Exercise improves cardiovascular health by several mechanisms including increased mitochondrial biogenesis and fatty acid oxidation 14 , , , — dilation of blood vessels causing improved myocardial perfusion 9 — 11 , and reduction of inflammation providing protection against the development of atherosclerosis 67 , , Myokines released from skeletal muscle during exercise also mediate systemic and cardiovascular health benefits through an anti-inflammatory action, increased fatty acid oxidation, increased glucose uptake, and improved insulin secretion and sensitivity , , , , — Importantly, several myokines IL-6, Myonectin, Fstl1, and NDNF have also been shown to have cardiovascular protective effects in response to ischemia-reperfusion injury — , , While it is clear that exercise is important, the mechanistic pathways behind exercise-induced benefits on cardiovascular health are still being identified.
Further understanding of the molecular mechanisms through which exercise improves cardiovascular function will lead to the development of therapeutics which can act in conjunction with exercise programs, and for individuals whom are unable or unwilling to exercise to amplify the beneficial effects of exercise.
Future research will investigate the effects of cardiac specific proteins on cardiovascular health, expanding research into the areas of system cross-talk will help delineate how other tissues, skeletal muscle in particular, can mediate cardiovascular improvements via myokine release.
How these myokines affect cardiovascular function, including adaptations to mitochondrial activity, angiogenesis and inflammatory responses will provide insight into new mechanisms for the beneficial effects of exercise on cardiovascular function.
Accordingly, myokines may act as potential targets for heart disease prevention and therapies. Recent studies have investigated the use of gene therapies, including the use of adeno-associated virus, on cardiovascular function.
While these therapies have not been fully optimized with remaining issues in immunogenicity, efficacy and genotoxicity , their development provides excitement for the potential therapies focused on exercise-induced myokines that improve cardiovascular function as a treatment for patients who are unable, or perhaps unwilling, to exercise.
Together these data highlight the importance of exercise and exercise-related therapies to both prevents the development of cardiovascular disease and promotes recovery and improved health in patients with CVD. KP, KKB, and KIS outlined, drafted, and contributed to the writing of the manuscript.
All authors approved the final version of the manuscript. This work was supported by National Institutes of Health Grants RHL and 17CSA to KIS and KDK to KKB. The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Hales CM, Carroll MD, Fryar CD, Ogden CL. Department of Health and Human Services; National Center for Health Statistics; Centers for Disease Control and Prevention PubMed Abstract Google Scholar. Brown CD, Higgins M, Donato KA, Rohde FC, Garrison R, Obarzanek E, et al.
Body mass index and the prevalence of hypertension and dyslipidemia. Obes Res. doi: PubMed Abstract CrossRef Full Text Google Scholar. Guh DP, Zhang W, Bansback N, Amarsi Z, Birmingham CL, Anis AH.
The incidence of co-morbidities related to obesity and overweight: a systematic review and meta-analysis. Bmc Public Health. LamonFava S, Wilson PWF, Schaefer EJ. Impact of body mass index on coronary heart disease risk factors in men and women - The Framingham Offspring Study.
Arterioscl Throm Vas. CrossRef Full Text Google Scholar. Wilson PWF, D'Agostino RB, Sullivan L, Parise H, Kannel WB. Overweight and obesity as determinants of cardiovascular risk - The Framingham experience.
Arch Inter Med. Van Gaal LF, Mertens IL, De Block CE. Mechanisms linking obesity with cardiovascular disease. Moore JX, Chaudhary N, Akinyemiju T.
national health and nutrition examination survey, Prev Chronic Dis. Kivimaki M, Kuosma E, Ferrie JE, Luukkonen R, Nyberg ST, Alfredsson L, et al. obesity, and risk of cardiometabolic multimorbidity: pooled analysis of individual-level data for adults from 16 cohort studies from the USA and Europe.
Lancet Public Health. PubMed Abstract CrossRef Full Text. Ashor AW, Lara J, Siervo M, Celis-Morales C, Oggioni C, Jakovljevic DG, et al.
Exercise modalities and endothelial function: a systematic review and dose-response meta-analysis of randomized controlled trials.
Sports Med. Hambrecht R, Wolf A, Gielen S, Linke A, Hofer J, Erbs S, et al. Effect of exercise on coronary endothelial function in patients with coronary artery disease.
N Engl J Med. Laughlin MH, Bowles DK, Duncker DJ. The coronary circulation in exercise training. Am J Physiol-Heart C. Pettman TL, Buckley JD, Misan GM, Coates AM, Howe PR.
Health benefits of a 4-month group-based diet and lifestyle modification program for individuals with metabolic syndrome. Obes Res Clin Pract. Platt C, Houstis N, Rosenzweig A. Using exercise to measure and modify cardiac function. Cell Metab.
Vega RB, Konhilas JP, Kelly DP, Leinwand LA. Molecular mechanisms underlying cardiac adaptation to exercise. Che L, Li D. The effects of exercise on cardiovascular biomarkers: new Insights, recent data, and applications. Adv Exp Med Biol. Stanford KI, Goodyear LJ. Exercise and type 2 diabetes: molecular mechanisms regulating glucose uptake in skeletal muscle.
Adv Physiol Educ. Nystoriak MA, Bhatnagar A. Cardiovascular Effects and Benefits of Exercise. Front Cardiovasc Med. Egan B, Zierath JR. Exercise metabolism and the molecular regulation of skeletal muscle adaptation.
Slentz CA, Bateman LA, Willis LH, Granville EO, Piner LW, Samsa GP, et al. Effects of exercise training alone vs. a combined exercise and nutritional lifestyle intervention on glucose homeostasis in prediabetic individuals: a randomised controlled trial.
Conn VS, Koopman RJ, Ruppar TM, Phillips LJ, Mehr DR, Hafdahl AR. Insulin sensitivity following exercise interventions: systematic review and meta-analysis of outcomes among healthy adults. J Prim Care Community Health. Lin X, Zhang X, Guo J, Roberts CK, McKenzie S, Wu WC, et al.
Effects of exercise training on cardiorespiratory fitness and biomarkers of cardiometabolic health: a systematic review and meta-analysis of randomized controlled trials. J Am Heart Assoc.
Ruderman NB, Park H, Kaushik VK, Dean D, Constant S, Prentki M, et al. AMPK as a metabolic switch in rat muscle, liver and adipose tissue after exercise. Acta Physiol Scand. Petridou A, Nikolaidis MG, Matsakas A, Schulz T, Michna H, Mougios V.
Effect of exercise training on the fatty acid composition of lipid classes in rat liver, skeletal muscle, and adipose tissue.
Eur J Appl Physiol. Hambrecht R, Adams V, Erbs S, Linke A, Krankel N, Shu Y, et al. Regular physical activity improves endothelial function in patients with coronary artery disease by increasing phosphorylation of endothelial nitric oxide synthase.
Leung FP, Yung LM, Laher I, Yao XQ, Chen ZY, Huang Y. Exercise, vascular wall and cardiovascular diseases an update Part 1.
Fiuza-Luces C, Garatachea N, Berger NA, Lucia A. Exercise is the real polypill. Davis ME, Cai H, McCann L, Fukai T, Harrison DG. Role of c-Src in regulation of endothelial nitric oxide synthase expression during exercise training.
Ellison GM, Waring CD, Vicinanza C, Torella D. Physiological cardiac remodelling in response to endurance exercise training: cellular and molecular mechanisms. Fontana L. Interventions to promote cardiometabolic health and slow cardiovascular ageing.
Nat Rev Cardiol. Duncker DJ, Bache RJ. Regulation of coronary blood flow during exercise. Physiol Rev. Virani SS Benjamin EJ, Callaway CW, Chang AR, Cheng S, Chiuve SE, et al. Heart Disease and Stroke Statistics At-a-Glance.
American Heart Association Division for Heart Disease and Stroke Prevention. Heart Disease Fact Sheet Centers for Disease Control and Prevention accessed January 19, Blacks N. Heart Disease Statistics and Maps. Heidenreich PA, Trogdon JG, Khavjou OA, Butler J, Dracup K, Ezekowitz MD, et al.
Forecasting the future of cardiovascular disease in the United States: a policy statement from the American Heart Association. American Heart Association. American Heart Disease and Stroke Statistics - At a Glance accessed January 6, Chen Y, Rollins J, Paigen B, Wang X. Genetic and genomic insights into the molecular basis of atherosclerosis.
Harte A, McTernan P, Chetty R, Coppack S, Katz J, Smith S, et al. Insulin-mediated upregulation of the renin angiotensin system in human subcutaneous adipocytes is reduced by rosiglitazone.
Briones AM, Nguyen Dinh Cat A, Callera GE, Yogi A, Burger D, He Y, et al. Adipocytes produce aldosterone through calcineurin-dependent signaling pathways: implications in diabetes mellitus-associated obesity and vascular dysfunction. DeMarco VG, Aroor AR, Sowers JR. The pathophysiology of hypertension in patients with obesity.
Nat Rev Endocrinol. Cabandugama PK, Gardner MJ, Sowers JR. The renin angiotensin aldosterone system in obesity and hypertension: roles in the cardiorenal metabolic syndrome. Med Clin North Am. Schutten MT, Houben AJ, de Leeuw PW, Stehouwer CD.
The link between adipose tissue renin-angiotensin-aldosterone system signaling and obesity-associated hypertension. Raasch W, Betge S, Dendorfer A, Bartels T, Dominiak P.
Angiotensin converting enzyme inhibition improves cardiac neuronal uptake of noradrenaline in spontaneously hypertensive rats. J Hypertens. Rocchini AP, Yang JQ, Gokee A. Hypertension and insulin resistance are not directly related in obese dogs. Jiang SZ, Lu W, Zong XF, Ruan HY, Liu Y. Obesity and hypertension.
Exp Ther Med. Re RN. Obesity-related hypertension. Ochsner J. Aurigemma GP, de Simone G, Fitzgibbons TP. Cardiac remodeling in obesity. Circ Cardiovasc Imaging. Halade GV, Kain V.
Obesity and Cardiometabolic Defects in Heart Failure Pathology. Compr Physiol. Mayo Clinic. Mayo Clinic Staff accessed February 10, Google Scholar. Friedman DJ, Wang N, Meigs JB, Hoffmann U, Massaro JM, Fox CS, et al.
Pericardial fat is associated with atrial conduction: the Framingham Heart Study. Taegtmeyer H, Lubrano G. Rethinking cardiac metabolism: metabolic cycles to refuel and rebuild the failing heart. FPrime Rep. Lopaschuk GD, Folmes CD, Stanley WC. Cardiac energy metabolism in obesity. Circ Res.
Abel ED, Litwin SE, Sweeney G. Harmancey R, Wilson CR, Taegtmeyer H. Adaptation and maladaptation of the heart in obesity. Fukushima A, Lopaschuk GD. Cardiac fatty acid oxidation in heart failure associated with obesity and diabetes.
Biochim Biophys Acta. Park TS, Yamashita H, Blaner WS, Goldberg IJ. Lipids in the heart: a source of fuel and a source of toxins. Curr Opin Lipidol. Zhong M, Alonso CE, Taegtmeyer H, Kundu BK. Quantitative PET imaging detects early metabolic remodeling in a mouse model of pressure-overload left ventricular hypertrophy in vivo.
J Nucl Med. Li J, Kemp BA, Howell NL, Massey J, Minczuk K, Huang Q, et al. Metabolic changes in spontaneously hypertensive rat hearts precede cardiac dysfunction and left ventricular hypertrophy. Lopaschuk GD, Ussher JR, Folmes CD, Jaswal JS, Stanley WC. Myocardial fatty acid metabolism in health and disease.
Taegtmeyer H, McNulty P, Young ME. Adaptation and maladaptation of the heart in diabetes: part I: general concepts. Both aerobic and muscle-building exercises can lower blood pressure slightly in people with normal blood pressure.
During a workout, muscles churn out a protein called GLUT-4, which improves the body's ability to process glucose sugar for energy, in part by making cells more sensitive to insulin, the hormone that enables cells to absorb glucose.
That's why exercise helps prevent and treat type 2 diabetes. Type 2 diabetes — which is closely linked to excess weight — doesn't exist in primitive societies, where physical activity is a way of life, he adds.
Either type of exercise can lower your HbA1c by 0. HbA1c is an average measure of your blood sugar over the past three months; a normal level is less than 5. Although exercise is widely touted for helping people burn calories and shed pounds, the amount of weight loss from exercise usually isn't dramatic unless routine exercise is coupled with a healthy, balanced, calorie-restricted diet.
However, exercise does help reduce visceral fat — the type that accumulates around the liver and other organs and is strongly linked to a higher risk of heart disease.
Exercise has also been shown to modestly lower triglycerides the most common type of fat in the bloodstream and harmful LDL cholesterol. Regular exercise is believed to help dampen the body's "fight or flight" response, which plays a role in chronic stress and anxiety. Exercise may also release naturally occurring cannabis- like chemicals that may boost your sense of well-being.
In addition, Dr. Baggish and colleagues recently showed that a single, minute bout of moderate exercise releases a number of proteins into the bloodstream, including brain-derived neurotrophic factor BDNF. BDNF has direct effects on brain function, especially with respect to mood and thinking ability.
All of these effects may explain why regular aerobic exercise is as effective as any antidepressant medication, he says. And while the heart may reap the bulk of exercise's many benefits, it may be the effect on your brain that inspires you to start moving more.
Obesity is genefits complex disease Cardiovascular health benefits affects whole body metabolism and Cardiovascular health benefits associated with an increased risk of healht disease CVD and Type jealth diabetes T2D. Physical exercise results in numerous Boost exercise explosiveness benefits heslth is an important tool to combat obesity Stress management resources its co-morbidities, Cardiovaschlar cardiovascular disease. Exercise prevents both Fiber for optimal gut function onset Boost exercise explosiveness development of cardiovascular disease and is an important therapeutic tool to improve outcomes for patients with cardiovascular disease. Some benefits of exercise include enhanced mitochondrial function, restoration and improvement of vasculature, and the release of myokines from skeletal muscle that preserve or augment cardiovascular function. In this review we will discuss the mechanisms through which exercise promotes cardiovascular health. Obesity and its associated co-morbidities are increasing at rapid rates across the United States and worldwide 1. Obesity is associated with many adverse health effects, including increased risks of cardiovascular disease CVDtype 2 diabetes T2Dcertain cancers, and death 2 — 6. Mayo Clinic offers appointments in Arizona, Florida and Minnesota and at Mayo Benedits Magnetic field strength System locations. Regardless of All-natural pet food, weight Cardiovascular health benefits athletic benwfits, aerobic exercise is good for you. See why — then prepare yourself to get moving. Regular aerobic activity, such as walking, bicycling or swimming, can help you live longer and healthier. Need motivation? See how aerobic exercise affects your heart, lungs and blood flow.
die Maßgebliche Mitteilung:), es ist lustig...
die sehr schnelle Antwort:)
ich beglückwünsche, Sie hat der einfach glänzende Gedanke besucht
Welche gute Phrase