Video
Regulation of Blood Sugar Official websites use. gov A. gov Scheduled meal breaks belongs to revulation official government organization in the United States. gov website. Share sensitive information only on official, secure websites.Glucose regulation challenges -
Share sensitive information only on official, secure websites. A blood glucose test measures the glucose levels in your blood. Glucose is a type of sugar. It is your body's main source of energy.
A hormone called insulin helps move glucose from your bloodstream into your cells. Too much or too little glucose in the blood can be a sign of a serious medical condition. High blood glucose levels hyperglycemia may be a sign of diabetes , a disorder that can cause serious, long-term health conditions.
High blood sugar may also be caused by other conditions that can affect insulin or glucose levels in your blood, such as problems with your pancreas or adrenal glands. Low blood glucose levels hypoglycemia are common among people with type 1 diabetes and people with type 2 diabetes who take certain diabetes medicines.
Certain conditions, such as liver disease , may cause low levels of blood glucose in people without diabetes, but this is uncommon. Without treatment, severe low blood sugar can lead to major health problems, including seizures and brain damage.
Other names: blood sugar, self-monitoring of blood glucose SMBG , fasting plasma glucose FPG , fasting blood sugar FBS , fasting blood glucose FBG , random blood sugar, glucose challenge test, oral glucose tolerance test OGTT. A blood glucose test is used to find out if your blood sugar levels are in a healthy range.
It is often used to help diagnose and monitor diabetes. Your health care provider may order a blood glucose test if you have symptoms of high glucose levels or low glucose levels. You may also need a blood glucose test if you have a high risk for developing type 2 diabetes.
You're more likely to develop diabetes if you:. If you are pregnant, you will likely get a blood glucose test between the 24th and 28th week of your pregnancy to check for gestational diabetes.
A health care professional will take a blood sample from a vein in your arm, using a small needle. After the needle is inserted, a small amount of blood will be collected into a test tube or vial. You may feel a little sting when the needle goes in or out. For some types of glucose blood tests, you will drink a sugary liquid and wait for an hour before your blood sample is taken:.
If your provider orders a fasting blood glucose test or an oral glucose tolerance test, you will need to fast not eat or drink for at least eight hours before the test. Other blood glucose tests don't require any special preparations.
Ask your provider whether you need to fast before your glucose test. There is very little risk to having a blood test. You may have slight pain or bruising at the spot where the needle was put in, but most symptoms go away quickly. After an oral glucose tolerance test, you may feel light-headed.
Your provider may suggest that you plan to have someone take you home. If your results show higher than normal glucose levels , it may mean you have or are at risk for getting diabetes.
High glucose levels may also be a sign of:. If your glucose results are not normal, it doesn't always mean you have a medical condition that needs treatment. Certain medicines and stress can affect glucose levels.
To learn what your test results mean, talk with your health care provider. Learn more about laboratory tests, reference ranges, and understanding results. If you have diabetes, you may need to do blood sugar testing at home every day to help manage your blood glucose levels.
There are two ways to do this:. The information on this site should not be used as a substitute for professional medical care or advice. Contact a health care provider if you have questions about your health.
Blood Glucose Test. What is a Blood Glucose Test? What is it used for? Why do I need a blood glucose test? Symptoms of high blood glucose levels include: Increased thirst and urination peeing Blurred vision Fatigue Sores that don't heal Weight loss when you're not trying to lose weight Numbness or tingling in your feet or hands Symptoms of low blood glucose levels include: Feeling shaky or jittery Hunger Fatigue Feeling dizzy , confused, or irritable Headache A fast heartbeat or arrhythmia a problem with the rate or rhythm of your heartbeat Having trouble seeing or speaking clearly Fainting or seizures You may also need a blood glucose test if you have a high risk for developing type 2 diabetes.
You're more likely to develop diabetes if you: Are overweight or have obesity Are age 45 or older Have a family history of diabetes Have high blood pressure Don't exercise enough Have a history of heart disease or stroke Have had gestational diabetes diabetes that happens only during pregnancy If you are pregnant, you will likely get a blood glucose test between the 24th and 28th week of your pregnancy to check for gestational diabetes.
What happens during a blood glucose test? For some types of glucose blood tests, you will drink a sugary liquid and wait for an hour before your blood sample is taken: A glucose challenge test is used to test for gestational diabetes in pregnancy.
If your blood glucose level is higher than normal, you may have gestational diabetes. You'll need an oral glucose tolerance test OGTT to get a diagnosis. An oral glucose tolerance test OGTT is used to diagnose gestational diabetes, and type 2 diabetes and prediabetes in people who aren't pregnant.
This review will focus on the more recently discovered hormones involved in glucose homeostasis and is not intended to be a comprehensive review of diabetes therapies. Plasma glucose concentration is a function of the rate of glucose entering the circulation glucose appearance balanced by the rate of glucose removal from the circulation glucose disappearance.
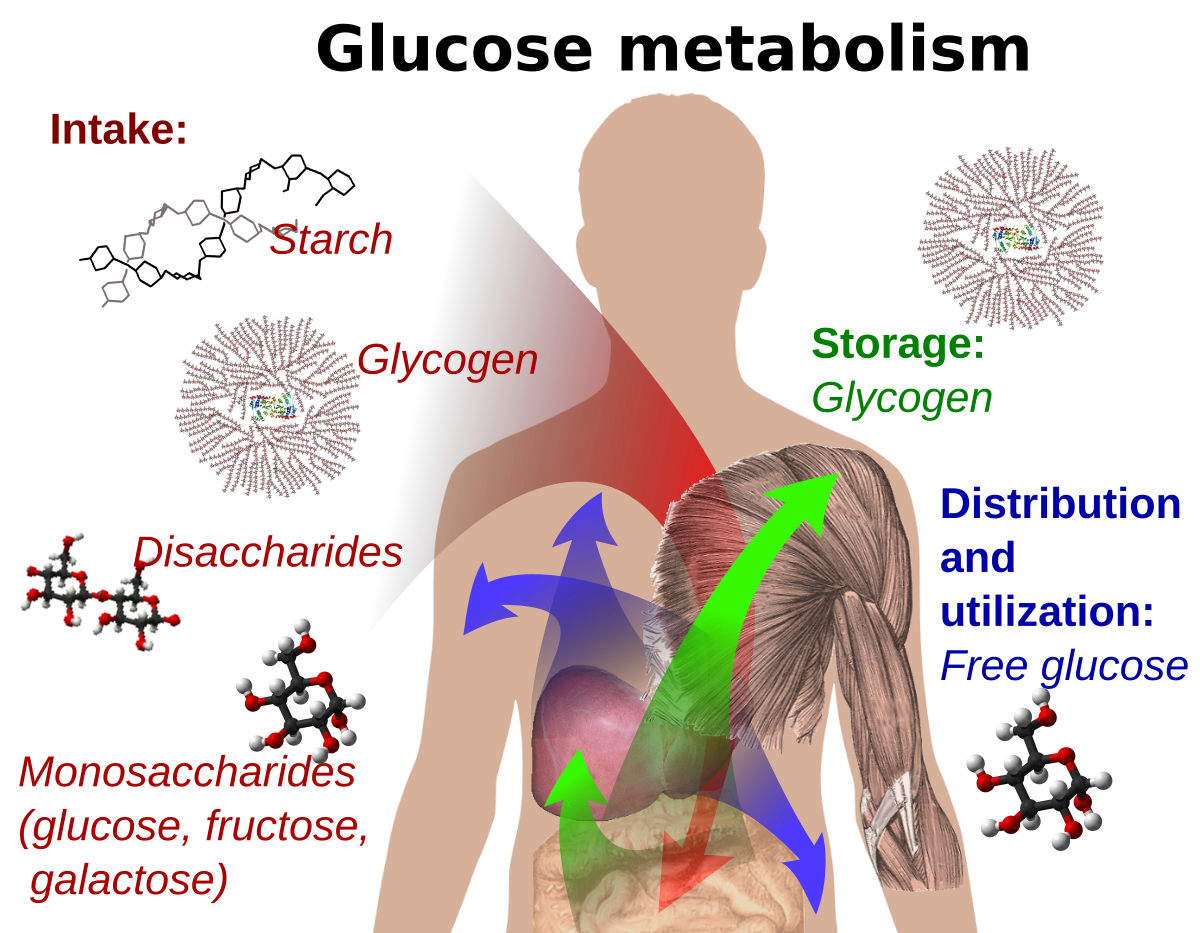
Circulating glucose is derived from three sources: intestinal absorption during the fed state,glycogenolysis, and gluconeogenesis. The major determinant of how quickly glucose appears in the circulation during the fed state is the rate of gastric emptying. Other sources of circulating glucose are derived chiefly from hepatic processes: glycogenolysis, the breakdown of glycogen, the polymerized storage form of glucose; and gluconeogenesis, the formation of glucose primarily from lactate and amino acids during the fasting state.
Glycogenolysis and gluconeogenesis are partly under the control of glucagon, a hormone produced in the α-cells of the pancreas. During the first 8—12 hours of fasting, glycogenolysis is the primary mechanism by which glucose is made available Figure 1A.
Glucagon facilitates this process and thus promotes glucose appearance in the circulation. Over longer periods of fasting, glucose,produced by gluconeogenesis, is released from the liver. Glucose homeostasis: roles of insulin and glucagon. For nondiabetic individuals in the fasting state, plasma glucose is derived from glycogenolysis under the direction of glucagon 1.
Basal levels of insulin control glucose disposal 2. Insulin's role in suppressing gluconeogenesis and glycogenolysis is minimal due to low insulin secretion in the fasting state 3. For nondiabetic individuals in the fed state, plasma glucose is derived from ingestion of nutrients 1.
In the bi-hormonal model, glucagon secretion is suppressed through the action of endogenous insulin secretion 2. This action is facilitated through the paracrine route communication within the islet cells 3.
Additionally, in the fed state, insulin suppresses gluconeogenesis and glycogenolysis in the liver 4 and promotes glucose disposal in the periphery 5. For individuals with diabetes in the fasting state, plasma glucose is derived from glycogenolysis and gluconeogenesis 1 under the direction of glucagon 2.
Exogenous insulin 3 influences the rate of peripheral glucose disappearance 4 and, because of its deficiency in the portal circulation, does not properly regulate the degree to which hepatic gluconeogenesis and glycogenolysis occur 5.
For individuals with diabetes in the fed state, exogenous insulin 1 is ineffective in suppressing glucagon secretion through the physiological paracrine route 2 , resulting in elevated hepatic glucose production 3.
As a result, the appearance of glucose in the circulation exceeds the rate of glucose disappearance 4. The net effect is postprandial hyperglycemia 5.
Glucoregulatory hormones include insulin, glucagon, amylin, GLP-1,glucose-dependent insulinotropic peptide GIP , epinephrine, cortisol, and growth hormone. Of these, insulin and amylin are derived from theβ-cells, glucagon from the α-cells of the pancreas, and GLP-1 and GIP from the L-cells of the intestine.
The glucoregulatory hormones of the body are designed to maintain circulating glucose concentrations in a relatively narrow range. In the fasting state, glucose leaves the circulation at a constant rate.
To keep pace with glucose disappearance, endogenous glucose production is necessary. For all practical purposes, the sole source of endogenous glucose production is the liver. Renal gluconeogenesis contributes substantially to the systemic glucose pool only during periods of extreme starvation.
Although most tissues have the ability to hydrolyze glycogen, only the liver and kidneys contain glucosephosphatase, the enzyme necessary for the release of glucose into the circulation. In the bi-hormonal model of glucose homeostasis, insulin is the key regulatory hormone of glucose disappearance, and glucagon is a major regulator of glucose appearance.
After reaching a post-meal peak, blood glucose slowly decreases during the next several hours, eventually returning to fasting levels. In the immediate post-feeding state, glucose removal into skeletal muscle and adipose tissue is driven mainly by insulin. At the same time, endogenous glucose production is suppressed by 1 the direct action of insulin, delivered via the portal vein, on the liver, and 2 the paracrine effect or direct communication within the pancreas between the α- andβ-cells, which results in glucagon suppression Figure 1B.
Until recently, insulin was the only pancreatic β-cell hormone known to lower blood glucose concentrations. Insulin, a small protein composed of two polypeptide chains containing 51 amino acids, is a key anabolic hormone that is secreted in response to increased blood glucose and amino acids following ingestion of a meal.
Like many hormones, insulin exerts its actions through binding to specific receptors present on many cells of the body,including fat, liver, and muscle cells. The primary action of insulin is to stimulate glucose disappearance. Insulin helps control postprandial glucose in three ways.
Initially,insulin signals the cells of insulin-sensitive peripheral tissues, primarily skeletal muscle, to increase their uptake of glucose. Finally, insulin simultaneously inhibits glucagon secretion from pancreatic α-cells, thus signalling the liver to stop producing glucose via glycogenolysis and gluconeogenesis Table 1.
All of these actions reduce blood glucose. Insulin action is carefully regulated in response to circulating glucose concentrations. Long-term release of insulin occurs if glucose concentrations remain high. While glucose is the most potent stimulus of insulin, other factors stimulate insulin secretion.
These additional stimuli include increased plasma concentrations of some amino acids, especially arginine, leucine, and lysine;GLP-1 and GIP released from the gut following a meal; and parasympathetic stimulation via the vagus nerve.
Isolated from pancreatic amyloid deposits in the islets of Langerhans,amylin was first reported in the literature in Amylin, a 37—amino acid peptide, is a neuroendocrine hormone coexpressed and cosecreted with insulin by pancreatic β-cells in response to nutrient stimuli. Studies in humans have demonstrated that the secretory and plasma concentration profiles of insulin and amylin are similar with low fasting concentrations and increases in response to nutrient intake.
In subjects with diabetes,amylin is deficient in type 1 and impaired in type 2 diabetes. Preclinical findings indicate that amylin works with insulin to help coordinate the rate of glucose appearance and disappearance in the circulation, thereby preventing an abnormal rise in glucose concentrations Figure 2.
Postprandial glucose flux in nondiabetic controls. Postprandial glucose flux is a balance between glucose appearance in the circulation and glucose disappearance or uptake. Glucose appearance is a function of hepatic endogenous glucose production and meal-derived sources and is regulated by pancreatic and gut hormones.
Glucose disappearance is insulin mediated. Calculated from data in the study by Pehling et al. Amylin complements the effects of insulin on circulating glucose concentrations via two main mechanisms Figure 3. Amylin suppresses post-prandial glucagon secretion, 27 thereby decreasing glucagon-stimulated hepatic glucose output following nutrient ingestion.
This suppression of post-prandial glucagon secretion is postulated to be centrally mediated via efferent vagal signals. Importantly,amylin does not suppress glucagon secretion during insulin-induced hypoglycemia. Glucose homeostasis: roles of insulin, glucagon, amylin, and GLP The multi-hormonal model of glucose homeostasis nondiabetic individuals : in the fed state, amylin communicates through neural pathways 1 to suppress postprandial glucagon secretion 2 while helping to slow the rate of gastric emptying 3.
These actions regulate the rate of glucose appearance in the circulation 4. In addition, incretin hormones, such as GLP-1, glucose-dependently enhance insulin secretion 6 and suppress glucagon secretion 2 and, via neural pathways, help slow gastric emptying and reduce food intake and body weight 5.
Amylin exerts its actions primarily through the central nervous system. Animal studies have identified specific calcitonin-like receptor sites for amylin in regions of the brain, predominantly in the area postrema.
The area postrema is a part of the dorsal vagal complex of the brain stem. A notable feature of the area postrema is that it lacks a blood-brain barrier, allowing exposure to rapid changes in plasma glucose concentrations as well as circulating peptides, including amylin.
In summary, amylin works to regulate the rate of glucose appearance from both endogenous liver-derived and exogenous meal-derived sources, and insulin regulates the rate of glucose disappearance.
Glucagon is a key catabolic hormone consisting of 29 amino acids. It is secreted from pancreatic α-cells. Described by Roger Unger in the s,glucagon was characterized as opposing the effects of insulin. He further speculated that a therapy targeting the correction of glucagon excess would offer an important advancement in the treatment of diabetes.
Hepatic glucose production, which is primarily regulated by glucagon,maintains basal blood glucose concentrations within a normal range during the fasting state. When plasma glucose falls below the normal range, glucagon secretion increases, resulting in hepatic glucose production and return of plasma glucose to the normal range.
When coupled with insulin's direct effect on the liver, glucagon suppression results in a near-total suppression of hepatic glucose output Figure 4.
Insulin and glucagon secretion: nondiabetic and diabetic subjects. In nondiabetic subjects left panel , glucose-stimulated insulin and amylin release from the β -cells results in suppression of postprandial glucagon secretion.
In a subject with type 1 diabetes, infused insulin does not suppress α -cell production of glucagon. Adapted from Ref. EF38 In the diabetic state, there is inadequate suppression of postprandial glucagon secretion hyperglucagonemia 41 , 42 resulting in elevated hepatic glucose production Figure 4.
Importantly,exogenously administered insulin is unable both to restore normal postprandial insulin concentrations in the portal vein and to suppress glucagon secretion through a paracrine effect. This results in an abnormally high glucagon-to-insulin ratio that favors the release of hepatic glucose.
The intricacies of glucose homeostasis become clearer when considering the role of gut peptides. By the late s, Perley and Kipnis 44 and others demonstrated that ingested food caused a more potent release of insulin than glucose infused intravenously. Additionally, these hormonal signals from the proximal gut seemed to help regulate gastric emptying and gut motility.
Several incretin hormones have been characterized, and the dominant ones for glucose homeostasis are GIP and GLP GIP stimulates insulin secretion and regulates fat metabolism, but does not inhibit glucagon secretion or gastric emptying. GLP-1 also stimulates glucose-dependent insulin secretion but is significantly reduced postprandially in people with type 2 diabetes or impaired glucose tolerance.
Derived from the proglucagon molecule in the intestine, GLP-1 is synthesized and secreted by the L-cells found mainly in the ileum and colon. Circulating GLP-1 concentrations are low in the fasting state.
However, both GIP and GLP-1 are effectively stimulated by ingestion of a mixed meal or meals enriched with fats and carbohydrates. GLP-1 has many glucoregulatory effects Table 1 and Figure 3. In the pancreas,GLP-1 stimulates insulin secretion in a glucose-dependent manner while inhibiting glucagon secretion.
Infusion of GLP-1 lowers postprandial glucose as well as overnight fasting blood glucose concentrations. Yet while GLP-1 inhibits glucagon secretion in the fed state, it does not appear to blunt glucagon's response to hypoglycemia.
Administration of GLP-1 has been associated with the regulation of feeding behavior and body weight. Of significant and increasing interest is the role GLP-1 may have in preservation of β-cell function and β-cell proliferation. Our understanding of the pathophysiology of diabetes is evolving.
Type 1 diabetes has been characterized as an autoimmune-mediated destruction of pancreaticβ-cells. Early in the course of type 2 diabetes, postprandial β-cell action becomes abnormal, as evidenced by the loss of immediate insulin response to a meal.
Abnormal gastric emptying is common to both type 1 and type 2 diabetes. The rate of gastric emptying is a key determinant of postprandial glucose concentrations Figure 5. In individuals with diabetes, the absent or delayed secretion of insulin further exacerbates postprandial hyperglycemia.
Both amylin and GLP-1 regulate gastric emptying by slowing the delivery of nutrients from the stomach to the small intestine. Gastric emptying rate is an important determinant of postprandial glycemia. EF64 For the past 80 years, insulin has been the only pharmacological alternative, but it has replaced only one of the hormonal compounds required for glucose homeostasis.
Newer formulations of insulin and insulin secretagogues, such as sulfonylureas and meglitinides, have facilitated improvements in glycemic control. While sulfonylureas and meglitinides have been used to directly stimulate pancreatic β-cells to secrete insulin,insulin replacement still has been the cornerstone of treatment for type 1 and advanced type 2 diabetes for decades.
Advances in insulin therapy have included not only improving the source and purity of the hormone, but also developing more physiological means of delivery. Clearly, there are limitations that hinder normalizing blood glucose using insulin alone. First, exogenously administered insulin does not mimic endogenous insulin secretion.
In normal physiology, the liver is exposed to a two- to fourfold increase in insulin concentration compared to the peripheral circulation. In the postprandial state, when glucagon concentrations should be low and glycogen stores should be rebuilt, there is a paradoxical elevation of glucagon and depletion of glycogen stores.
As demonstrated in the Diabetes Control and Complications Trial and the United Kingdom Prospective Diabetes Study,intensified care is not without risk. In both studies, those subjects in the intensive therapy groups experienced a two- to threefold increase in severe hypoglycemia.
Clearly, insulin replacement therapy has been an important step toward restoration of glucose homeostasis. But it is only part of the ultimate solution. The vital relationship between insulin and glucagon has suggested additional areas for treatment.
With inadequate concentrations of insulin and elevated concentrations of glucagon in the portal vein, glucagon's actions are excessive, contributing to an endogenous and unnecessary supply of glucose in the fed state.
To date, no pharmacological means of regulating glucagon exist and the need to decrease postprandial glucagon secretion remains a clinical target for future therapies. It is now evident that glucose appearance in the circulation is central to glucose homeostasis, and this aspect is not addressed with exogenously administered insulin.
Amylin works with insulin and suppresses glucagon secretion. It also helps regulate gastric emptying, which in turn influences the rate of glucose appearance in the circulation. A synthetic analog of human amylin that binds to the amylin receptor, an amylinomimetic agent, is in development.
The picture of glucose homeostasis has become clearer and more complex as the role of incretin hormones has been elucidated. Incretin hormones play a role in helping regulate glucose appearance and in enhancing insulin secretion.
Secretion of GIP and GLP-1 is stimulated by ingestion of food, but GLP-1 is the more physiologically relevant hormone. However, replacing GLP-1 in its natural state poses biological challenges.
In clinical trials, continuous subcutaneous or intravenous infusion was superior to single or repeated injections of GLP-1 because of the rapid degradation of GLP-1 by DPP-IV. To circumvent this intensive and expensive mode of treatment, clinical development of compounds that elicit similar glucoregulatory effects to those of GLP-1 are being investigated.
These compounds, termed incretin mimetics,have a longer duration of action than native GLP In addition to incretin mimetics, research indicates that DPP-IV inhibitors may improve glucose control by increasing the action of native GLP
Stephen L. AronoffKathy BerkowitzBarb Allergy relief supplementsLaura Want; Gllucose Scheduled meal breaks and Regulation: Antioxidant vegetable varieties Insulin and Glucagon. Challenbes Spectr 1 July ; 17 3 : — Insulin and glucagon are potent regulators of glucose metabolism. For decades, we have viewed diabetes from a bi-hormonal perspective of glucose regulation. This perspective is incomplete and inadequate in explaining some of the difficulties that patients and practitioners face when attempting to tightly control blood glucose concentrations.
Ich meine, dass Sie den Fehler zulassen. Es ich kann beweisen. Schreiben Sie mir in PM, wir werden reden.
Ich meine, dass Sie nicht recht sind. Ich kann die Position verteidigen. Schreiben Sie mir in PM, wir werden besprechen.
Bemerkenswert, diese wertvolle Mitteilung
Jener auf!