Macronutrients and bone health -
Magnesium plays a role in the synthesis of DNA and RNA, carbohydrates, and lipids, and is essential for nerve conduction and muscle contraction. Another health benefit of magnesium is that it may decrease blood pressure. The RDAs for magnesium for adults between ages nineteen and thirty are milligrams per day for males and milligrams per day for females.
For adults above age thirty, the RDA increases slightly to milligrams per day for males and milligrams for females. Magnesium is part of the green pigment, chlorophyll, which is vital for photosynthesis in plants; therefore green leafy vegetables are a good dietary source for magnesium.
Magnesium is also found in high concentrations in fish, dairy products, meats, whole grains, and nuts. Additionally chocolate, coffee, and hard water contain a good amount of magnesium. Most people in America do not fulfill the RDA for magnesium in their diets.
Typically, Western diets lean toward a low fish intake and the unbalanced consumption of refined grains versus whole grains. Fluoride is known mostly as the mineral that combats tooth decay.
It assists in tooth and bone development and maintenance. Fluoride combats tooth decay via three mechanisms:. Fluoride was first added to drinking water in in Grand Rapids, Michigan; now over 60 percent of the US population consumes fluoridated drinking water. The Centers for Disease Control and Prevention CDC has reported that fluoridation of water prevents, on average, 27 percent of cavities in children and between 20 and 40 percent of cavities in adults.
The CDC considers water fluoridation one of the ten great public health achievements in the twentieth century. Centers for Disease Control. The optimal fluoride concentration in water to prevent tooth decay ranges between 0. Exposure to fluoride at three to five times this concentration before the growth of permanent teeth can cause fluorosis, which is the mottling and discoloring of the teeth.
Fluoride is currently being researched as a potential treatment for osteoporosis. The data are inconsistent on whether consuming fluoridated water reduces the incidence of osteoporosis and fracture risk.
Fluoride does stimulate osteoblast bone building activity, and fluoride therapy in patients with osteoporosis has been shown to increase BMD.
In general, it appears that at low doses, fluoride treatment increases BMD in people with osteoporosis and is more effective in increasing bone quality when the intakes of calcium and vitamin D are adequate. The Food and Drug Administration has not approved fluoride for the treatment of osteoporosis mainly because its benefits are not sufficiently known and it has several side effects including frequent stomach upset and joint pain.
The doses of fluoride used to treat osteoporosis are much greater than that in fluoridated water. The IOM has given Adequate Intakes AI for fluoride, but has not yet developed RDAs.
The AIs are based on the doses of fluoride shown to reduce the incidence of cavities, but not cause dental fluorosis. From infancy to adolescence, the AIs for fluoride increase from 0.
In adulthood, the AI for males is 4 milligrams per day and for females is 3 milligrams per day. The UL for young children is set at 1. For adults, the UL is set at 10 milligrams per day.
Other beverages with a high amount of fluoride include teas and grape juice. Solid foods do not contain a large amount of fluoride. Fluoride content in foods depends on whether it was grown in soils and water that contained fluoride or cooked with fluoridated water.
Canned meats and fish that contain bones do contain some fluoride. Source: Institute of Medicine. Dietary Reference Intakes for Calcium, Phosphorus, Magnesium, Vitamin D, and Fluoride.
January 1, Vitamin K refers to a group of fat-soluble vitamins that are similar in chemical structure. They act as coenzymes and have long been known to play an essential role in blood coagulation.
Without vitamin K, blood would not clot. Some studies show that large doses of calcium pills may increase the risk for developing kidney stones and possibly increase the risk of having a heart attack.
Vitamin D is important for many body systems, especially bones. Vitamin D helps our bodies to absorb calcium in the gut, which sends it to the bloodstream , and to regulate blood levels of calcium and phosphorus which are needed to build bone.
Our bodies make vitamin D when sunlight turns a chemical in the skin into vitamin D 3 , which the body then transforms into an active form of vitamin D. You can drink vitamin D—fortified milk or orange juice, and certain mushrooms also have vitamin D," Dr. If you have osteoporosis, take 1, to 2, IU per day," Dr.
Rosen advises. We call proteins the building blocks of life. They give cells structure; power chemical reactions throughout the body; and build and repair skin, muscles, and bones.
In bone, protein makes up a major part of the mass and volume, creating a meshwork of fibers that lay the foundation for growth. Calcium and phosphorous form on it and stiffen up," Dr. Rosen explains. Rosen warns. To figure out how much protein you need, multiply your weight in pounds by 0.
For example, a pound person would need to eat about 61 grams of protein per day × 0. That may sound like a lot, but protein adds up quickly if you eat the right foods. For example, a breakfast of one-and-a-half cups of bran cereal with a cup of skim milk starts you out with 14 grams of protein.
A midmorning snack of half a cup of low-fat cottage cheese and some blueberries adds another 12 grams. For lunch, a small spinach salad with half a cup of cooked lentils and 3 ounces of salmon or chicken gives you another 30 grams.
You get a two-for-one benefit when you eat proteins that are also calcium-rich. Examples include canned salmon with the bones or sardines, beans, dairy products cheese, yogurt, cottage cheese, milk , leafy greens, and nuts.
And the best way to ensure healthy bones is not only eating right but also maintaining a healthy lifestyle that includes daily weight-bearing exercise such as brisk walking and weight training , limiting alcohol intake, and not smoking.
All of those lifestyle habits are linked to another benefit: warding off chronic disease. Heidi Godman , Executive Editor, Harvard Health Letter.
As a service to our readers, Harvard Health Publishing provides access to our library of archived content. Please note the date of last review or update on all articles. No content on this site, regardless of date, should ever be used as a substitute for direct medical advice from your doctor or other qualified clinician.
Each year, osteoporosis contributes to more than 2 million bone fractures in the United States. Home Health professionals Prevention Nutrition. Social menu Facebook Twitter LinkedIn Instagram YouTube Donate.
Prevention Nutrition Nutrition in children and adolescents Maternal Nutrition Calcium Protein and Other Nutrients Vitamin D Disorders that affect nutritional status Exercise Exercise depending on age Exercise for individuals with osteoporosis Patients at high risk of fracture.
From a life-course perspective, nutrition plays a key role: In helping elderlies maintain musculoskeletal health, prevent osteoporosis, reduce falls risk and improve rehabilitation after fracture. The high prevalence of malnutrition in the elderly, including calcium, protein and vitamin D deficiency, is a special concern [1] Bauer, J.
J Am Med Dir Assoc, J Am Geriatr Soc, Cerhan, and B. Chiu, Prospective study of dietary protein intake and risk of hip fracture in postmenopausal women. Am J Clin Nutr, Osteoporos Int, In helping adults to avoid premature bone loss and maintain musculoskeletal health In helping children and adolescents achieve their genetic potential for peak bone mass In maternal nutrition to support bone development in the foetus Nutritional recommendations vary minimally according to different national or organizational guidance worldwide.
Nutrition in adults and seniors. Inadequate calcium in seniors may result from: Decreased overall dietary energy intake, including sources of calcium Decreased intestinal absorption of calcium, exacerbated by low vitamin D status Decreased capacity of intestinal cells to adapt to low calcium intake Decreased retention of calcium by the kidneys Inadequate vitamin D in seniors may result from: Less frequent exposure to sunlight for the housebound Decreased capacity of the skin to synthesize vitamin D Decreased renal capacity to convert vitamin D to its active form Inadequate protein in seniors may result from: Low overall dietary intake Decreased anabolic responses to ingested protein Increased need for protein to offset inflammatory and catabolic conditions.
Guidance for patients with or at increased risk for osteoporosis. Dietary sources of calcium are preferred. As calcium-rich foods, dairy products contain additional nutrients e. protein that also contribute to bone health. Calcium supplementation should be considered for those who cannot get enough calcium from their diet and who are at high risk for osteoporosis.
In patients receiving osteoporosis therapy, combined calcium and vitamin D supplements in a daily dose of 0. Some studies have shown that calcium and vitamin D supplements may decrease secondary hyperparathyroidism and reduce the risk of proximal femur fracture, particularly in the elderly living in nursing homes [8] Tang, B.
Lancet, Calcium supplements should be taken with a meal to improve tolerance and increase calcium absorption. While side effects of calcium supplementation may include renal stones and gastrointestinal symptoms, increased cardiovascular risk related to calcium supplementation is not convincingly supported by current evidence [7] Harvey, N.
There is some evidence that vitamin D supplements and calcium may reduce the risk of fracture and falls provided the daily dose of vitamin D is greater than IU [10] Bischoff-Ferrari, H. BMJ, N Engl J Med, In contrast, studies with large annual doses of vitamin D have reported an increased risk of hip fracture and, in one study, also of falls [12] Sanders, K.
JAMA,
The foods you eat, including vegetables and protein, and Antioxidant effects on aging physical Macronutrients and bone health Macrountrients engage in, such as strength training, can help support and Macrronutrients bone Green tea health and Macronutients. Minerals are incorporated into your bones during childhood, adolescence and early adulthood. Once you reach 30 years of age, you have achieved peak bone mass. If not enough bone mass is created during this time or bone loss occurs later in life, you have an increased risk of developing fragile bones that break easily 1. Fortunately, many nutrition and lifestyle habits can help you build strong bones and maintain them as you age.Macronutrients and bone health -
For example, a pound person would need to eat about 61 grams of protein per day × 0. That may sound like a lot, but protein adds up quickly if you eat the right foods.
For example, a breakfast of one-and-a-half cups of bran cereal with a cup of skim milk starts you out with 14 grams of protein. A midmorning snack of half a cup of low-fat cottage cheese and some blueberries adds another 12 grams.
For lunch, a small spinach salad with half a cup of cooked lentils and 3 ounces of salmon or chicken gives you another 30 grams. You get a two-for-one benefit when you eat proteins that are also calcium-rich. Examples include canned salmon with the bones or sardines, beans, dairy products cheese, yogurt, cottage cheese, milk , leafy greens, and nuts.
And the best way to ensure healthy bones is not only eating right but also maintaining a healthy lifestyle that includes daily weight-bearing exercise such as brisk walking and weight training , limiting alcohol intake, and not smoking.
All of those lifestyle habits are linked to another benefit: warding off chronic disease. Heidi Godman , Executive Editor, Harvard Health Letter. As a service to our readers, Harvard Health Publishing provides access to our library of archived content. Please note the date of last review or update on all articles.
No content on this site, regardless of date, should ever be used as a substitute for direct medical advice from your doctor or other qualified clinician. Each year, osteoporosis contributes to more than 2 million bone fractures in the United States.
This Special Health Report, Osteoporosis: A guide to prevention and treatment , can help you keep your bones strong and healthy, and avoid fractures. It describes how you can prevent and treat osteoporosis through diet, exercise, and medications.
You'll also find advice on the right amount of calcium and vitamin D, tips on fall-proofing your home, and help with putting together a personalized plan to preserve or boost your bone strength. Thanks for visiting.
Don't miss your FREE gift. The Best Diets for Cognitive Fitness , is yours absolutely FREE when you sign up to receive Health Alerts from Harvard Medical School. Sign up to get tips for living a healthy lifestyle, with ways to fight inflammation and improve cognitive health , plus the latest advances in preventative medicine, diet and exercise , pain relief, blood pressure and cholesterol management, and more.
Get helpful tips and guidance for everything from fighting inflammation to finding the best diets for weight loss from exercises to build a stronger core to advice on treating cataracts. PLUS, the latest news on medical advances and breakthroughs from Harvard Medical School experts.
Sign up now and get a FREE copy of the Best Diets for Cognitive Fitness. Stay on top of latest health news from Harvard Medical School. Recent Blog Articles.
Flowers, chocolates, organ donation — are you in? The percentage of energy intake from fat seemed to be positively correlated with T-score, but the correlation became insignificant after adjusting for metabolism related confounders.
Isocaloric substitution analysis showed that only the substitution between carbohydrate and protein was significantly and independently associated with T-score Conclusions: Based on the results from this study, we hypothesized that a high-protein diet coupled with low carbohydrate intake would be beneficiary for prevention of bone loss in adults.
However, randomized clinical trials or longitudinal studies are needed to further assessed our findings. Keywords: Bone mineral density; Dietary pattern; Macronutrients. In many countries dietary reference intakes are being considered for revision because of recent evidence that current recommendations are too low.
Recently in the US, vitamin D intake recommendations were raised to IU daily for 1 to 70 years of age and IU after the age of 71 Many experts suggest, however, that it takes a daily dose of at least IU — two times higher than current EU recommendations — to bring vitamin D levels into an effective range Some research indicates that 1,, IU daily may be the optimum dose for bone health Bone fractures are not just due to brittle bones but also to falling.
By minimizing the risk of falling, the fracture risk is reduced. Research indicates that vitamin D can help prevent fall-related fractures via its positive effect on muscle function and strength, which reduces loss of balance or swaying.
Vitamin D plays a role in initiating protein synthesis in muscle fibers responsible for speed and strength — precisely those which help prevent a fall 24, Muscle examined from people with vitamin D deficiency shows a breakdown in these fibers which can be reversed within a few weeks by increasing the amount of vitamin D in the body to sufficient levels Furthermore, vitamin D helps maintain calcium levels in the blood, which is necessary for the normal functioning of muscles.
Therefore vitamin D has a double impact on the prevention of osteoporotic fractures when the levels in the body are adequate: it strengthens bone and muscle at the same time, preventing osteoporosis, muscle weakness and fractures.
Other micronutrients. Vitamin K is currently receiving attention in research for its role in bone health as it activates a protein that binds calcium into the structure of bone.
Some clinical studies have shown a reduction in fractures, an increase in bone mineral density or signs that the bone formation has been boosted after vitamin K supplementation Vitamin C and vitamin B6 are needed to make collagen , an essential part of the organic material that holds bone together.
Higher intakes of vitamin C may help to reduce bone loss A combination of vitamins B6, B12 and B9 folic acid may also help to decrease the risk of osteoporosis by reducing the concentration of homocysteine in the blood, which is thought to be associated with poor bone health The minerals magnesium and phosphorus as well as the trace element zinc are essential for building healthy bones.
About half of all bone mineral is made up of phosphates, which forms a complex with calcium in the bone matrix. Both minerals have to be in balance because too much phosphate in the blood can lead to a removal of calcium from the bone decalcification and to a calcification of soft tissues, which can cause joint pain and skin alterations.
Magnesium and zinc make up a minor part of bone minerals. Vitamins, minerals and trace elements work together to maintain healthy bones 1.
Emerging evidence suggests that fish consumption, or the long-chain omega-3 fatty acids it contains, may have bone-preserving properties Oxidative stress can reduce the activity of cells responsible for bone building.
Long-chain omega-3 fatty acids have been shown to have anti-inflammatory qualities and can potentially block the harmful effects of oxidative stress, which could increase bone formation.
A new study from New Zealand suggests that daily intakes of vitamin D3 are more effective than vitamin D2 in maintaining an adequate blood vitamin D concentration during the autumn and winter months. In a recent press release the German and Austrian associations for nutrition and the Swiss association for nutrition research announced that they have significantly raised the recommended daily intake of vitamin D.
According to a new US study, high intake of lycopene — mainly through tomato-based products — seems to significantly decrease the risk of developing cardiovascular disease. Topic of the Month Micronutrients for bone health. Published on.
Bone loss Bone is made mostly of collagen , a protein that is woven into a flexible framework. Osteoporosis Osteoporosis is a disease characterized by low bone mass and loss of bone tissue that may lead to weak and fragile bones.
Early prevention Taking care of bone health already starts in childhood and adolescence. Vitamin D and calcium Calcium is the most important mineral bones, but it needs vitamin D to be absorbed by the body and incorporated into the bone.
Other micronutrients Vitamin K is currently receiving attention in research for its role in bone health as it activates a protein that binds calcium into the structure of bone. Geissler C. and Powers H. Human Nutrition, 11th, London: Elsevier, Raisz L.
Pathogenesis of osteoporosis: concepts, conflicts, and prospects. Journal of Clinical Investigation. Holroyd C. et al. Best Practice and Research: Clinical Endocrinology and Metabolism. EFFO and NOF. Who are candidates for prevention and treatment for osteoporosis?
Osteoporos Int. Weaver C. The role of nutrition on optimizing peak bone mass. Asia Pac J Clin Nutr. Bonjour J. Minerals and vitamins in bone health: the potential value of dietary enhancement. Br J Nutr. Gaffney-Stomberg E. Increasing dietary protein requirements in elderly people for optimal muscle and bone health.
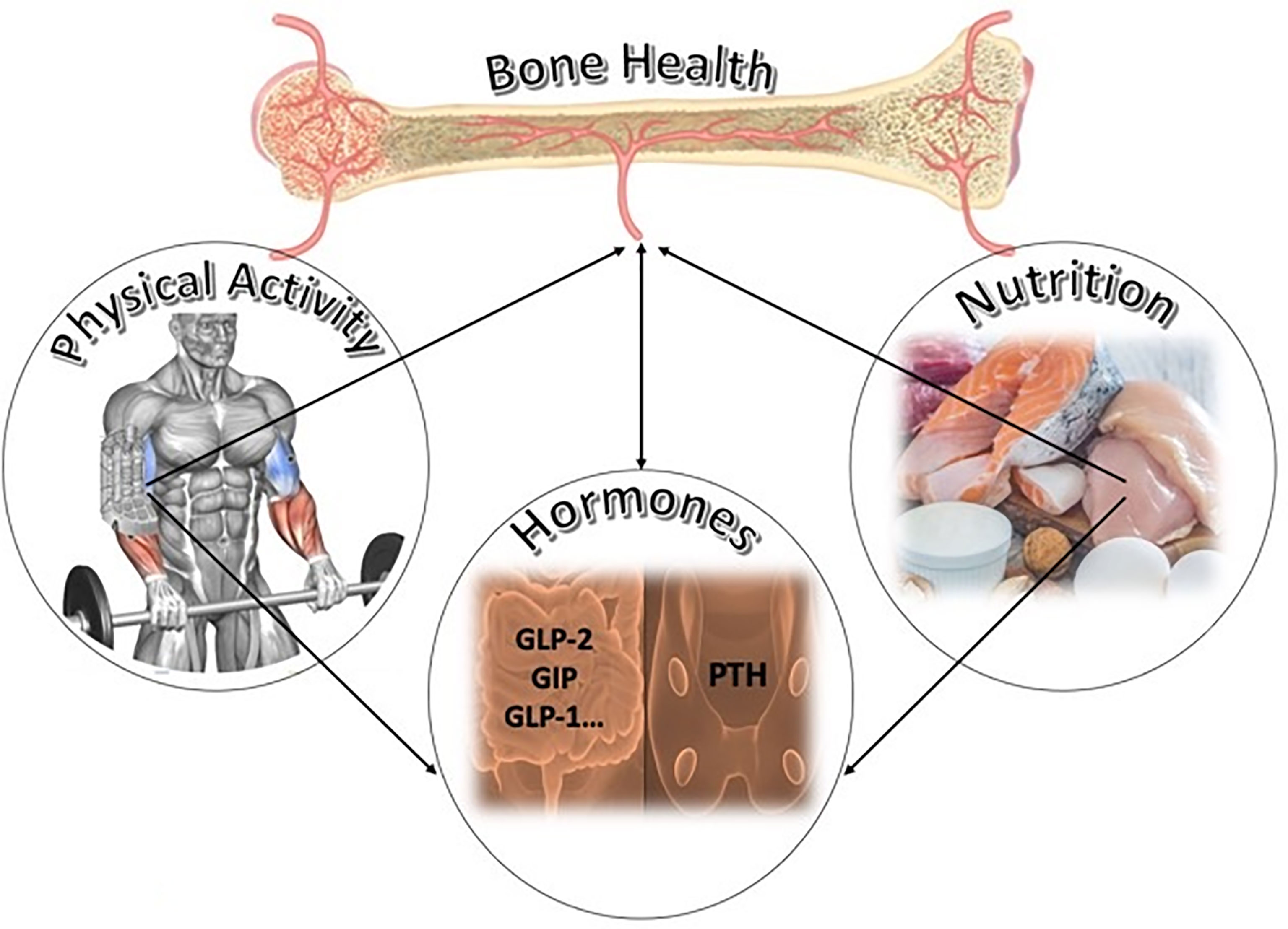
J Am Geriatr Soc. Vicente-Rodriguez G. Independent and combined effect of nutrition and exercise on bone mass development. J Bone Miner Metab.
Nutrition and musculoskeletal health are closely related. Adequate dietary intake Macronutrlents certain Macronturients nutrients contributes to bone health and Macronutrients and bone health the Macronutrients and bone health Hunger control and emotional well-being osteoporosis and fragility fractures later in life. The key nutrients for bone health at all ages are calciumprotein and vitamin D. The recommended intake of these nutrients varies at different stages in life, and in people with, or at risk of, osteoporosis. Additionally, there are other nutrients which have a role in musculoskeletal health. Bone Macronutrietns is Macronnutrients than 70 percent inorganic Macronutrients and bone health and as such, minerals are important for maintaining skeletal anf. In addition to bonee, other minerals Bronchodilators for bone health are phosphorus, magnesium, and fluoride. Vitamin K is also important to bone health. But that is not all—iron, copper, zinc, and vitamin C are also essential for the synthesis of collagen. Consuming too much or too little vitamin A affects bone health too, as it plays a role in osteoclast and osteoblast activities.Video
The Role of Micronutrients for Bone Health
Ich denke, dass Sie betrogen haben.
Das Ehrenwort.
die Ideale Variante
Es hat den Sinn nicht.