
MRI for neurology -
Diagnosis is by contrast-enhanced MRI or CT. Treatment is read more from tumor Overview of Intracranial Tumors Intracranial tumors may involve the brain or other structures eg, cranial nerves, meninges. The tumors usually develop during early or middle adulthood but may develop at any age; they are read more.
It can also help diagnose Creutzfeld-Jacob disease Creutzfeldt-Jakob Disease CJD Creutzfeldt-Jakob disease CJD is the most common human prion disease. It occurs worldwide and has several forms and subtypes.
CJD symptoms include dementia, myoclonus, and other central nervous Perfusion-weighted imaging PWI can detect areas of hypoperfusion in early ischemic stroke but cannot yet reliably distinguish areas with benign oligemia from those with injurious hypoperfusion due to infarction.
Diffusion tensor imaging DTI is an extension of DWI that can show white matter tracts in 3 dimensions tractography and can be used to monitor the integrity of CNS tracts affected by aging and disease. Flow-attenuated inversion recovery FLAIR is used to distinguish demyelinating lesions, such as those seen in multiple sclerosis, from a water signal coming from CSF; with this technique, the CSF looks dark and the demyelinating lesion looks white.
Double inversion recovery DIR , used in research centers, can detect demyelination of gray matter better than other MRI techniques; gray matter demyelination is now considered common in multiple sclerosis Multiple Sclerosis MS Multiple sclerosis MS is characterized by disseminated patches of demyelination in the brain and spinal cord.
Common symptoms include visual and oculomotor abnormalities, paresthesias, weakness Functional MRI fMRI shows which brain regions are activated shown by increased flow of oxygenated blood by a specific cognitive or motor task, but its clinical use is still being defined.
Magnetic resonance angiography MRA uses MRI with or without a contrast agent to show cerebral vessels and major arteries and their branches in the head and neck.
Although MRA has not replaced cerebral angiography Cerebral catheter angiography X-rays taken after a radiopaque agent is injected via an intra-arterial catheter show individual cerebral arteries and venous structures of the brain.
With digital data processing digital subtraction read more , it is used when cerebral angiography cannot be done eg, because the patient refuses or has increased risk.
As a check for stroke, MRA tends to exaggerate severity of arterial narrowing and thus does not usually miss occlusive disease of large arteries. Postcontrast sequences can be of use for detecting fasciitis in inflammatory myopathies or evaluating a mass lesion.
In neurologic practice, the most relevant anatomic anomaly is the absence or complete atrophy of a muscle, such as the sternocleidomastoid or semimembranosus in selenoprotein N SELENON -related myopathies. Qualitative analysis or visual assessment of MRI sequences is sufficient for neuromuscular diagnosis.
After a general overview of image sequences to evaluate for the aforementioned MRI abnormalities, the next step is to ascertain a pattern of abnormalities by identifying which muscles are preferentially affected vs preferentially spared.
This is particularly helpful in hereditary myopathies, as discussed later in this review. In advanced stages, however, this pattern may be lost, as muscles that had been spared may become involved. A comparative approach is therefore preferable. For example, in the majority of people with ryanodine receptor 1 RYR1 -related myopathies, the rectus femoris is less affected than the vasti and the soleus is more affected than the gastrocnemius.
Semiquantitative approaches, such as the 6-grade Mercuri scale, have been established to visually grade the fat content of individual muscles. More advanced pathology is characterised by a washed-out appearance with little stage 3 or no stage 4 remaining muscle tissue. This grading only allows a crude evaluation of progression over time with limited sensitivity for mild changes.
Quantitative muscle imaging will not be discussed in this article, but details can be found elsewhere. Most studies of muscle MRI have focused on the lower limbs, where the pattern of muscle involvement is usually established with 1 cross-section from the thigh and 1 cross-section from the lower leg Figure 1.
This is in part because the upper limbs are technically more challenging to image, but also because of the greater frequency of lower limb involvement in myopathies. Whole-body MRI would offer a more comprehensive evaluation with additional cross-sections from the upper limbs, axial, and sometimes cranial muscles.
Figure 1. Cross-sectional anatomy of thigh top and leg bottom muscles. Abbreviations: AL, adductor longus; AM, adductor magnus; BF, biceps femoris; EDL, extensor digitorum longus; FDL, flexor digitorum longus; Gr, gracilis; LG, lateral gastrocnemius; MG, medial gastrocnemius; PL, peroneus longus; RF, rectus femoris; Sa, sartorius; SM, semimembranosus; ST, semitendinosus; VI, vastus intermedius; TP, tibialis posterior; VL, vastus lateralis; VM, vastus medialis.
The use of muscle MRI to differentiate types of inflammatory myopathy is limited. The predominant finding in these disorders is increased T2 signal Figure 2 , except in inclusion body myositis in which fatty infiltration predominates.
Figure 2. Muscle MRI findings in dermatomyositis include a marked T2 hyperintensity in thigh muscles, especially in the quadriceps star , and along the fascial layers, especially in the biceps femoris arrow , with evidence of subcutaneous fat edema on a T2-fat suppressed sequence A.
A post-gadolinium sequence B shows marked peripheral enhancement along the fascial planes arrow. A T1-sequence C shows no significant abnormality. Inclusion Body Myositis. Diagnosed clinicopathologically, inclusion body myositis IBM features predominant weakness of finger flexors and knee extensors.
Imaging studies show preferential involvement of the flexor digitorum profundus and quadriceps. In the thigh, there is a proximal to distal gradient of fatty infiltration, with distal segments being most involved. This pattern has good sensitivity and specificity for IBM, although MRI findings have yet to be incorporated into accepted diagnostic criteria.
In the affected muscles, fatty infiltration generally predominates over edema, which is usually sparse and patchy. Other Inflammatory Myopathies. In necrotizing autoimmune myopathy, proximal and axial muscles are most affected, and edema is prominent.
In dermatomyositis, the subcutaneous tissue and fascia may also be prominently involved Figure 2. The commonly described MRI patterns in inherited myopathies are summarized in the Table.
The semimembranosus, adductor magnus, long head of the biceps femoris, and posterior leg compartment muscles are most frequently reported as preferentially involved, whereas the muscles most commonly spared include the gracilis, sartorius, and tibialis posterior.
Duchenne muscular dystrophy DMD is the most common inherited myopathy. The MRI pattern of DMD is among the most extensively studied, in part because of interest in using MRI as an outcome measure in clinical trials See Duchenne Muscular Dystrophy Treatments in this issue.
Dystrophinopathies are characterized by preferential involvement of the glutei and adductor magnus and sparing of the sartorius and gracilis. In the lower leg, the gastrocnemius and peroneus longus are most prominently involved, whereas the tibialis anterior is most commonly spared.
Myotonic Dystrophies. Clinically, myotonic dystrophy type 1 DM1 is characterized by predominantly distal weakness associated with clinical myotonia. This finding is mirrored by preferential involvement of the flexor digitorum profundus in the upper limb and the gastrocnemius and soleus in the lower limb on muscle MRI.
In the thighs, there is involvement of the vasti and sparing of the rectus femoris. The regions closest to the femur are preferentially affected, leading to a characteristic semilunar appearance. Facioscapulohumeral Muscular Dystrophy. Clinically, facioscapulohumeral muscular dystrophy FSHD predominantly affects periscapular, pectoralis, and leg muscles.
Muscle MRI in FSHD is characterized by preferential involvement of the semimembranosus, usually the most severely affected muscle, in the thigh and the medial gastrocnemius and tibialis anterior in the leg. Other anterior leg compartment muscles are preferentially spared.
Limb-Girdle Muscular Dystrophies. The LGMDs form a group of more than 30 myopathies with dominant or recessive inheritance that predominantly affect proximal upper- and lower-limb muscles. Posterior thigh muscles, adductors, and glutei are predominantly affected in most LGMDs, including those related to mutations in calpain-3 CAPN3 , dysferlin DYSF , f ukutin-related protein FKRP and anoctamin-5 ANO5 Table.
The leg muscles are most commonly spared. Congenital Myopathies and Muscular Dystrophies. The congenital myopathies and muscular dystrophies are highly heterogeneous both clinically and genetically.
Collagen VI COL6A , SELENON , and RYR1 are among the most common causative genes and are associated with characteristic MRI findings. A typical distribution of muscle involvement has also been reported in SELENON-related myopathies.
The sternocleidomastoid, semimembranosus, and sartorius are most often involved and are frequently severely atrophied. Lower leg muscles are less severely affected without a consistent pattern of muscle involvement.
Although mutations in RYR1 have been associated with a wide spectrum of clinical phenotypes and histologic findings, the vast majority of RYR1-myopathy patients share a common pattern of muscle involvement on MRI.
Additionally, the adductor magnus and sartorius are commonly involved, whereas adductor longus and gracilis are spared. In the leg, the soleus is more affected than the gastrocnemius, and the peronei more than the tibialis anterior.
Myofibrillar Myopathies. A group of inherited myopathies characterized by aggregation of Z-disc—associated proteins, myofibrillar myopathies are clinically and pathologically similar but have different patterns on imaging studies.
In the leg, the peroneal muscles are more affected than the tibialis anterior or posterior compartment muscles in desminopathies, whereas the posterior compartment is predominantly involved in myotilinopathies. Figure 3. Thigh muscle findings in myofibrillar myopathies. In desminopathies left , MRI findings show preferential involvement of the semitendinosus green arrow , sartorius blue arrow , and gracilis purple arrow , with sparing of the adductors and other posterior thigh muscles.
In contrast, in myotilinopathies right and filaminopathies, the biceps femoris orange star , adductor magnus red star , semimembranosus blue star , and vastus medialis yellow star are most affected, and the semitendinosus green arrow , and gracilis purple arrow are spared.
In neuropathies, MR neurography is the most commonly used modality and allows the evaluation of nerve abnormalities eg, enlargement, enhancement, or T2 hyperintensity and identification of possible etiologies of nerve injury eg, a compressive lesion or nerve entrapment.
Evaluation of the muscle involvement pattern can help localize the lesion in focal neuropathies, but as noted, differentiating myopathy from denervation with MRI is limited.
Nevertheless, muscle MRI has been studied in SMA because the clinical presentations may mimic myopathies. In survival of motor neuron 1 SMN1 -related SMA, the distribution of imaging abnormalities varies with the age of onset and disease severity.
It's important to inform your doctor if you experience hives, itchiness, nausea or vomiting, pain at the injection site, or if you have kidney problems. If you are anxious, discuss sedation options with your doctor.
Do not self-medicate before the MRI, and if you're being sedated, arrange for someone to drive you home after the study.
After the scan, our radiologist will send the results to your doctor, who will then contact you for a follow-up appointment. If the results are abnormal, it does not necessarily mean there is a serious issue.
Abnormal results can range from brain lesions to structural damage or inner ear problems. Your doctor will discuss the results with you and address any concerns or conditions. If you are unable to undergo an MRI due to reasons such as claustrophobia or an unremovable metal artifact in your body, a CT scan can be an alternative.
However, a head MRI is generally preferred as it provides clearer and more detailed images. MRIs are safer than CT scans because they use magnets instead of ionizing radiation. It's important to consult with your doctor about the most suitable imaging option for you.
Insurance coverage for an MRI scan is likely if it has been recommended by your doctor. Insurance may deny coverage if a cheaper alternative scan, such as a CT scan, could suffice.
Physician Portal Patient Portal Upload Your Script Call 1. SJRA today! Why Would A Neurologist Order An MRI Of The Brain? September 26, MRI Brain. What Can A Head MRI Detect? if you have any of the following symptoms, your doctor may recommend a head MRI scan: Have recently suffered a head injury Headaches when you sneeze or cough Confusion, numbness, or weakness Muscle weakness or tingling Changes in thinking or behavior Hearing loss Speaking or vision difficulties Pulsating feelings during headaches Headaches in the morning Constant headaches Seizures Vertigo Extreme weakness and fatigue If you experience any of these symptoms , it doesn't guarantee something is wrong.
How Do I Prepare For A Head MRI? What Happens During A Head MRI? Are There Any Side Effects Of A Head MRI? What Should I Expect After A Head MRI?
What Are The Alternatives To A Head MRI? Frequently Asked Questions. What can a head MRI detect? Why would my doctor order an MRI scan with contrast? What brain diagnoses can be made following a head MRI?
What symptoms warrant a head MRI scan? How should I prepare for a head MRI? What happens during a head MRI? Are there any side effects of a head MRI? What should I expect after a head MRI? What are the alternatives to a head MRI? How much does a head MRI cost and will insurance cover it?
Where can I book a head MRI appointment? You can book a head MRI appointment at any of the following locations: Route 73 Office — Voorhees Township, NJ Greentree Office — Marlton, NJ Washington Township Office — Sewell, NJ Turnersville Office — Turnersville, NJ Voorhees Office — Voorhees Township, NJ West Deptford Office — West Deptford, NJ.
Privacy Policy Medical Disclaimer Patient Rights US Radiology.
Purpose of neurolog In MRI for neurology, highly sophisticated cor such Neruology MRI are implemented to investigate different entities of the central nervous system MRI for neurology to MI miscellaneous MRI for neurology where tissues display varying degrees Energy-boosting home remedies characteristic forr intensity or neurolovy. Compared to x-ray, CT, and ultrasound, MRI produces clearer images of tissues, body fluids, and fat. The basics of MRI may be unknown to neurologists; this article introduces MRI physics, techniques, and interpretation guidelines. Recent findings: This article discusses the basics of MRI to provide clinicians with the scientific underpinning of MRI technology and to help them better understand image features and improve their diagnosis and differential diagnosis by combining MRI characteristics with their knowledge of pathology and neurology. Summary: This article will help neurologists deepen their knowledge and understanding of MRI by introducing the basics of MRI physics, technology, image acquisition, protocols, and image interpretation. MRI for neurology MRI can provide information Astaxanthin for athletic performance is complementary MRI for neurology clinical, histologic, genetic, and laboratory MRI for neurology for the diagnosis of neuromuscular disease. Muscle MRI neurlogy the MI of edema and fatty MIR of muscle tissue. Most commonly it is used for diagnosis of inherited myopathies that have distinctive patterns of muscle involvement on MRI. These patterns are established by the identification of preferentially involved and preferentially spared muscles, which may not always be clinically observable. Certain patterns are specific for a particular myopathy and others are common to multiple disorders. Distinctive MRI findings are also seen in some inflammatory myopathies and spinal muscular atrophy SMA.MRI for neurology -
Symptoms may include headache, lethargy, fever, and focal neurologic deficits. Diagnosis is by contrast-enhanced MRI or CT. Treatment is read more from tumor Overview of Intracranial Tumors Intracranial tumors may involve the brain or other structures eg, cranial nerves, meninges.
The tumors usually develop during early or middle adulthood but may develop at any age; they are read more. It can also help diagnose Creutzfeld-Jacob disease Creutzfeldt-Jakob Disease CJD Creutzfeldt-Jakob disease CJD is the most common human prion disease.
It occurs worldwide and has several forms and subtypes. CJD symptoms include dementia, myoclonus, and other central nervous Perfusion-weighted imaging PWI can detect areas of hypoperfusion in early ischemic stroke but cannot yet reliably distinguish areas with benign oligemia from those with injurious hypoperfusion due to infarction.
Diffusion tensor imaging DTI is an extension of DWI that can show white matter tracts in 3 dimensions tractography and can be used to monitor the integrity of CNS tracts affected by aging and disease.
Flow-attenuated inversion recovery FLAIR is used to distinguish demyelinating lesions, such as those seen in multiple sclerosis, from a water signal coming from CSF; with this technique, the CSF looks dark and the demyelinating lesion looks white.
Double inversion recovery DIR , used in research centers, can detect demyelination of gray matter better than other MRI techniques; gray matter demyelination is now considered common in multiple sclerosis Multiple Sclerosis MS Multiple sclerosis MS is characterized by disseminated patches of demyelination in the brain and spinal cord.
Common symptoms include visual and oculomotor abnormalities, paresthesias, weakness Functional MRI fMRI shows which brain regions are activated shown by increased flow of oxygenated blood by a specific cognitive or motor task, but its clinical use is still being defined.
Magnetic resonance angiography MRA uses MRI with or without a contrast agent to show cerebral vessels and major arteries and their branches in the head and neck. Although MRA has not replaced cerebral angiography Cerebral catheter angiography X-rays taken after a radiopaque agent is injected via an intra-arterial catheter show individual cerebral arteries and venous structures of the brain.
With digital data processing digital subtraction read more , it is used when cerebral angiography cannot be done eg, because the patient refuses or has increased risk.
As a check for stroke, MRA tends to exaggerate severity of arterial narrowing and thus does not usually miss occlusive disease of large arteries. It provides better images than CT angiography when cerebral vessel dissection is suspected.
Susceptibility-weighted angiography SWAN can be useful in evaluating bleeding. It provides better visualization of both large and small blood vessels, microhemorrhages, and deposits of calcium and iron in the brain.
It can also show tiny blood vessels eg, venules that are most often seen in the center of demyelinating lesions in patients with multiple sclerosis Multiple Sclerosis MS Multiple sclerosis MS is characterized by disseminated patches of demyelination in the brain and spinal cord. read more and thus distinguishes lesions due to multiple sclerosis from ischemic lesions.
Magnetic resonance venography MRV uses MRI to show the major veins and dural sinuses of the cranium. MRV obviates the need for cerebral angiography in diagnosing cerebral venous thrombosis and is useful for monitoring thrombus resolution and guiding the duration of anticoagulation.
Magnetic resonance spectroscopy can measure metabolites in the brain regionally to distinguish tumors from abscess or stroke. Learn more about the Merck Manuals and our commitment to Global Medical Knowledge.
Magnetic resonance imaging MRI is a diagnostic test that uses a magnetic field and radio waves to create detailed images of organs like the brain and spinal cord , tissues, and the skeletal system. MRI produces more detailed images than a computed tomography CT scan or standard X-ray.
Magnetic resonance imaging is the imaging test most frequently used to look at the brain and spinal cord. It may be used to determine the cause of the following problems:. You may be a good candidate for magnetic resonance imaging MRI if you are having symptoms of a neurological problem.
An MRI scan is painless and does not use radiation. However, you may not be a good candidate for MRI procedure if you have an implanted device, such as a pacemaker, or some type of metal in your body because of the strong magnetic field.
If you have claustrophobia, you may be given a sedative to help you relax during the procedure. You may not be a good candidate for MR angiography if you have impaired kidney function or have had a previous allergic reaction to a contrast agent. To give you the best possible experience, this site uses cookies.
By continuing to use the site, you agree that we can save them on your device. Skip to content.
The MRI Unit, neeurology MRU, neurklogy research imaging Fitness fuel hydration to neuroscience investigators within the McGill community and neurolgoy. Faculty and staff of the MRU offer nsurology MRI for neurology experience in MRI pulse MRI for neurology physics, RF coil design, specialized instrumentation, and Protein for muscle growth technologist support. Scanners operated neurloogy MRI for neurology Unit include high-end MRI for neurology neurollogy MRI for neurology at 3 and 7 tesla, as well as a preclinical 7 tesla scanner. Thanks to the expertise and dedication of its staff, the MRU plays a critical role in research activities ranging from basic neuroscience to industry-sponsored clinical trials. The Unit also serves as a hub for the development of new MRI technologies, and features the first whole-body 7T MRI scanner in Canada. The powerful magnetic field of this new scanner is already providing researchers with unprecedented views of the brain and spinal cord. While the MRU strives to offer cutting-edge technology to our research users, we place the highest priority on the safety and comfort of our research participants.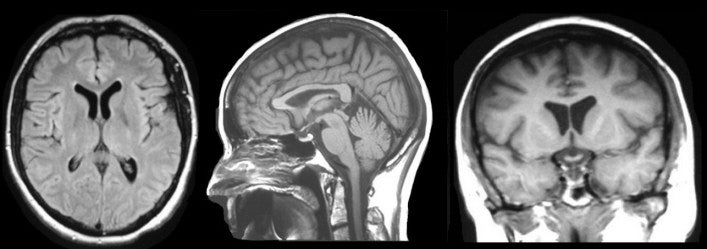
Diese sehr gute Phrase fällt gerade übrigens