Gut health and physical performance -
Table 2. The different types of dietary fiber [modified from 83 ]. Fiber intake is often low in the diet of athletes. Several studies, involving female artistic gymnastics, rhythmic gymnastics and ballet dance athletes 88 , or competitive American adolescent swimmers 89 reported that athletes' fiber consumption was often below the nutritional guidelines of 25 g per day based on a 2,calorie diet Only a few studies reported fiber consumption above the nutritional guidelines, and one of the few examples is female and male Dutch ultramarathon runners Athletes may be reluctant to adopt such dietary habits because of higher satiety sensation or digestion and gastrointestinal discomfort issues In parallel, to avoid gastrointestinal symptoms associated with exercise, some athletes turn to a low FODMAP Fermentable Oligo-, Di-, Mono-saccharides And Polyols diet to limit the presence of highly fermentable carbohydrates in their digestive tract Indeed, undigested carbohydrates may increase the osmotic load in the small intestine and contribute to increased osmotic water translocation, volume, and physiological issues such as loose stool or diarrhea 94 , Particular attention must also be paid when comparing elite athletes with sedentary controls.
Indeed, dietary protein intake differs largely in elite athletes and sedentary controls diets A recent study dealt with the effects of protein supplementation on the gut microbial composition Protein supplementation increased the abundance of the Bacteroidetes phylum and decreased the presence of health-related taxa, including Roseburia, Blautia , and Bifidobacterium longum.
The authors concluded that long-term protein supplementation may have a negative impact on gut microbiota. Likewise, a study comparing fecal microbiota characteristics among healthy sedentary men as controls , bodybuilders, and distance runners found that daily protein intake negatively correlated with diversity in distance runners.
This implies that a high quantity of protein in the diet may negatively impact the gut microbiota. Moreover, there was no difference in microbial diversity, but subject populations differed in terms of their gut microbial composition: Faecalibacterium, Sutterella, Clostridium, Haemophilus , and Eisenbergiella were the highest in bodybuilders, while Bifidobacterium and Parasutterella were the lowest.
Some intestinal beneficial bacteria Bifidobacterium adolescentis group, Bifidobacterium longum group, Lactobacillus sakei group, Blautia wexlerae and Eubacterium hallii were the lowest in bodybuilders and the highest in controls.
Thus, bodybuilders demonstrate a decrease in SCFA-producing commensal bacteria compared to controls Historically, probiotics have been used to mitigate intestinal issues linked to antibiotic treatment, travel, or illness Until very recently, the beneficial effects demonstrated after probiotic consumption were immune modulation and strengthening of the gut mucosal barrier.
The mechanisms included 1 modifications of gut microbial composition, 2 dietary protein modifications by the microbiota, 3 modification of bacterial enzyme capacity, 4 physical adherence to the intestinal mucosa that may outcompete a pathogen or inhibit its activation, and 5 influence on gut mucosal permeability , There are also effects through interactions with immune intestinal cells or altering cytokine production, especially in the upper part of the gut, where probiotics may transiently dominate Compared to hundreds of commensal species inhabiting the human gut microbiota, probiotics are limited to specific bacterial strains, mostly within the genera Lactobacillus, Bifidobacterium , and Saccharomyces for yeasts, for regulatory reasons.
Lactobacillus acidophilus and Lactobacillus casei Shirota have the longest history among known bacterial strains for application. In present-day commercial probiotic products, Lactobacillus spp. are well-represented, followed by Bifidobacterium spp. There is today a high degree of consensus that the clinical effects of probiotics are strain-dependent, meaning that probiotic properties should be defined not only at the species level but also at the strain level Probiotics have been tested for different potential health effects on athletes.
Figure 3 summarizes the reported effects of probiotic ingestion by athletes or subjects practicing moderate physical exercise. Figure 3. Reported effects of probiotic ingestion by athletes or subjects practicing moderate physical exercise. However, the effects differed between males and females, the latter group being less studied.
Until recently, probiotic supplementation effects on sports performance have seldom been tested. For example, Lactobacillus rhamnosus strain ATCC , when tested in marathon runners, demonstrated no effect on the number of GI symptom episodes, but their duration was shorter in the probiotic group In competitive cyclists, the number and duration of mild gastrointestinal symptoms were ~2-fold higher in the probiotic group Lactobacillus fermentum PCC However, in males, there was a substantial reduction in the severity of gastrointestinal illness as the mean training load increased.
Noticeably, the burden of lower respiratory illness symptoms decreased in males but increased in females. When sprint athletes consumed Bifidobacterium bifidum , their IgA, IgM, lymphocyte and monocyte percentages and CD4 counts were significantly higher than those of the control group Lactobacillus helveticus Lafti ® L10 supplementation for 3 months in a population of elite athletes triathletes, cyclists, and endurance athletes showed, in the probiotic group, a decrease in the main markers of oxidative stress and antioxidative defense, such as malondialdehyde, advanced oxidation protein products and superoxide dismutase In male runners, multistrain probiotic supplementation Lactobacillus acidophilus, Lactobacillus rhamnosus, Lactobacillus casei, Lactobacillus plantarum, Lactobacillus fermentum, Bifidobacterium lactis, Bifidobacterium breve, Bifidobacterium bifidum , and Streptococcus thermophilus significantly increased running time to fatigue.
In addition, probiotic supplementation led to small to moderate reductions in intestinal permeability and gastrointestinal discomfort In 24 recreational runners, probiotic supplementation for 28 days prior to a marathon race [ Lactobacillus acidophilus CUL60 and CUL21 , Bifidobacterium bifidum CUL20 , and Bifidobacterium animalis subs p.
lactis CUL34 ] was associated with a significantly lower incidence and severity of GI symptoms and limited decrease in average speed in the probiotics group compared to the control group However, there were no significant differences in finish times between the groups.
Probiotic supplementation Streptococcus thermophilus FP4 and Bifidobacterium breve BR03 was reported to likely enhance isometric average peak torque production, attenuating performance decrements and muscle tension in the days following a muscle-damaging exercise , where subjects performed 5 sets of 10 maximal eccentric contractions.
In a similar study design, Bacillus coagulans GBI , significantly increased recovery at 24 and 72 h and decreased soreness at 72 h post exercise Probiotic supplementation correlated with a maintained performance and a small increase in creatine phosphokinase.
Finally, Bacillus subtilis consumption during offseason training in female collegiate soccer and volleyball players, in conjunction with post-workout nutrition, had no effect on physical performance However, body fat percentages were significantly lower in the probiotic group.
Altogether, these results show that probiotics may improve oxidative or inflammatory markers but have no proven effect on performance. Nonetheless, potential new generation probiotics, first identified in elite athletes' microbiome undergoing exercise, have recently shown promising results in mouse performance models These bacteria belonging to the Veillonella genus feed on lactic acid and produce propionate, which may increase endurance capacity.
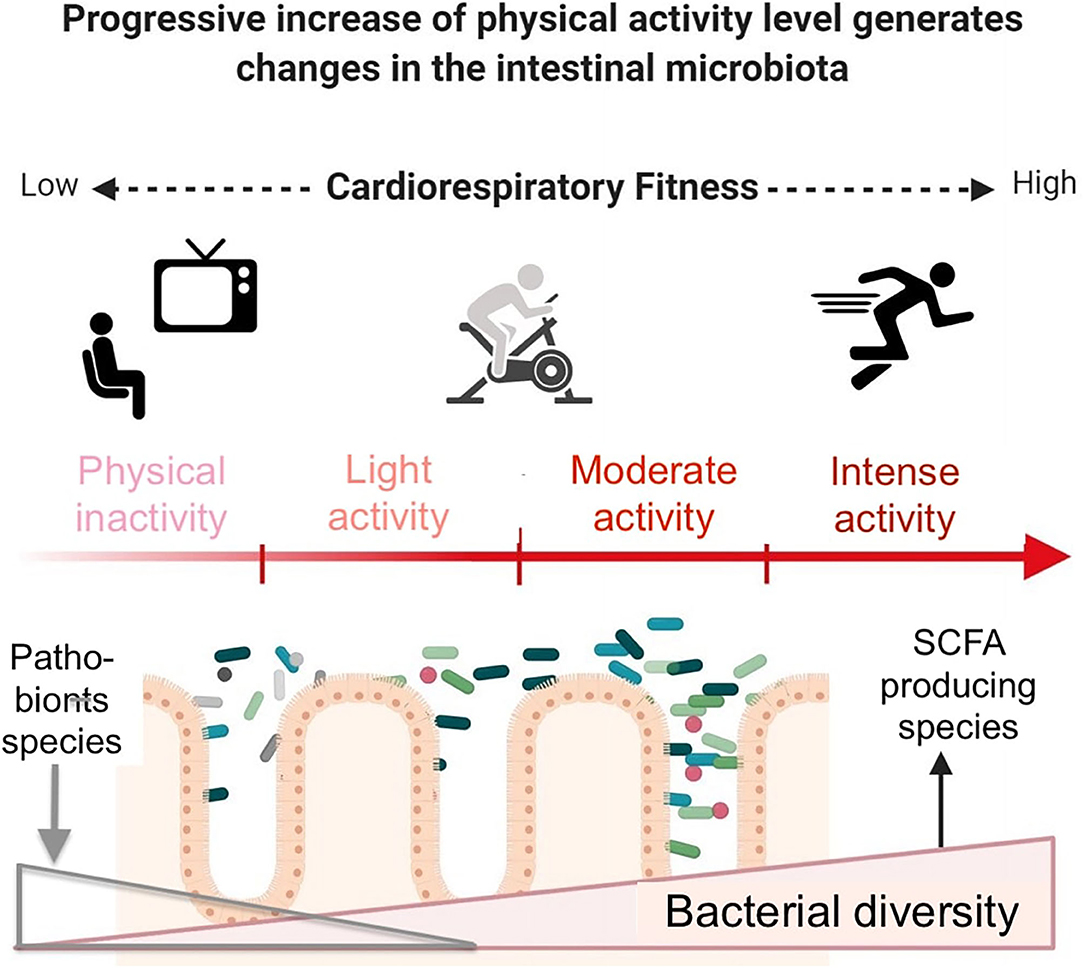
In endurance sports, the effects of exercise on the microbiome depend upon exercise intensity and its duration. Training can also reinforce some of these effects or develop new effects. In return, changes in the gut microbiota diversity and composition can translate into a reduction in inflammation and gastrointestinal symptoms as well as the modification of hundreds of metabolites.
Many of them are beneficial for the organism SCFAs, secondary bile acids, etc. and can allow endurance athletes to conduct huge volumes of training or to improve their sports performance.
Probiotics can be used, in addition, to further potentiate these adaptations. However, research is still needed to identify the best bacterial strains and their methods of administration. In addition, in a number of studies, it is very difficult to distinguish between the effects of exercise and diet on the gut microbiome variations.
They could both act synergistically. The different types of fiber, protein and supplements are usually not documented. However, the genome content of species with highly similar rDNA 16S sequences can differ.
So, the correlation between 16S rDNA taxonomy and functions does have limits. Besides 16S rDNA, other methods should be used to decipher the functions of microorganisms of interest. To overcome these limitations, Table 3 summarizes our main suggestions for future studies.
Table 3. Recommendations for more integrated studies in order to understand the interplay between exercise and gut microbiota in recreational athletes and elites. Similarly, metatranscriptomics, metaproteomics and metabolomics microbiota analyses can help to i explain some of the sports-induced modifications and ii find new key targets to act on.
We suggest adding longitudinal sportomics studies to microbiome monitoring through omics methods, together with dietary and well-being questionnaires. It could lead to microbiome-based solutions for health or performance by helping in the design of new supplements and also probiotics that would not necessarily be a unique strain but rather a consortium of species for a given metabolic outcome.
In addition to new monitoring applications, this strategy could lead to optimized diets through personalized nutrition based on an individual's microbiome make-up and workout intensity. MC wrote the first draft of the manuscript. ML coordinated the work. PG focused on animal models.
AM on clinical context. MC, PG, AM, and ML revised the original manuscript. All authors approved the final manuscript. The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Gastin PB. Energy system interaction and relative contribution during maximal exercise. Sports Med. doi: PubMed Abstract CrossRef Full Text Google Scholar.
Jeukendrup AE, Moseley L. Multiple transportable carbohydrates enhance gastric emptying and fluid delivery. Scand J Med Sci Sports. Jeukendrup AE. Training the gut for athletes. CrossRef Full Text Google Scholar. Rivera-Brown AM, Frontera WR.
Principles of exercise physiology: responses to acute exercise and long-term adaptations to training. Drossman DA. The functional gastrointestinal disorders and the Rome III process.
Thurber C, Dugas LR, Ocobock C, Carlson B, Speakman JR, Pontzer H. Extreme events reveal an alimentary limit on sustained maximal human energy expenditure.
Sci Adv. Simons SM, Kennedy RG. Gastrointestinal problems in runners. Curr Sports Med Rep. Knechtle B, Nikolaidis PT. Physiology and pathophysiology in ultra-marathon running.
Front Physiol. Sekirov I, Russell SL, Antunes LCM, Finlay BB. Gut microbiota in health and disease. Physiol Rev. Neish AS. Microbes in gastrointestinal health and disease. Ley RE, Peterson DA, Gordon JI. Ecological and evolutionary forces shaping microbial diversity in the human intestine.
Sender R, Fuchs S, Milo R. Revised estimates for the number of human and bacteria cells in the body. PLoS Biol. Chiller K, Selkin BA, Murakawa GJ. Skin microflora and bacterial infections of the skin. J Investig Dermatol Symp Proc.
Berg G, Rybakova D, Fischer D, Cernava T, Vergès M-CC, Charles T, et al. Microbiome definition re-visited: old concepts and new challenges.
Helander HF, Fändriks L. Surface area of the digestive tract — revisited. Scand J Gastroenterol. McHardy IH, Goudarzi M, Tong M, Ruegger PM, Schwager E, Weger JR, et al. Integrative analysis of the microbiome and metabolome of the human intestinal mucosal surface reveals exquisite inter-relationships.
Swidsinski A, Weber J, Loening-Baucke V, Hale LP, Lochs H. Spatial organization and composition of the mucosal flora in patients with inflammatory bowel disease. J Clin Microbiol. Tropini C, Earle KA, Huang KC, Sonnenburg JL. The gut microbiome: connecting spatial organization to function.
Cell Host Microbe. Brooks AW, Priya S, Blekhman R, Bordenstein SR. Gut microbiota diversity across ethnicities in the United States. Li J, Jia H, Cai X, Zhong H, Feng Q, Sunagawa S, et al. An integrated catalog of reference genes in the human gut microbiome. Nat Biotechnol. Arumugam M, Raes J, Pelletier E, Le Paslier D, Yamada T, Mende DR, et al.
Enterotypes of the human gut microbiome. Wu GD, Chen J, Hoffmann C, Bittinger K, Chen Y-Y, Keilbaugh SA, et al. Linking long-term dietary patterns with gut microbial enterotypes. Costea PI, Hildebrand F, Arumugam M, Bäckhed F, Blaser MJ, Bushman FD, et al. Enterotypes in the landscape of gut microbial community composition.
Nat Microbiol. Bäckhed F, Ley RE, Sonnenburg JL, Peterson DA, Gordon JI. Host-bacterial mutualism in the human intestine. Hooper LV, Gordon JI. Commensal host-bacterial relationships in the gut.
Aziz Q, Doré J, Emmanuel A, Guarner F, Quigley EMM. Gut microbiota and gastrointestinal health: current concepts and future directions. Neurogastroenterol Motil. Hsu Y, Chiu C, Li Y, Huang W, Huang Y, Huang C, et al. Effect of intestinal microbiota on exercise performance in mice. J Strength Cond Res.
Wahlström A, Sayin SI, Marschall H-U, Bäckhed F. Intestinal crosstalk between bile acids and microbiota and its impact on host metabolism. Cell Metabolism. Molinero N, Ruiz L, Sánchez B, Margolles A, Delgado S. Intestinal bacteria interplay with bile and cholesterol metabolism: implications on host physiology.
Belkaid Y, Hand TW. Role of the microbiota in immunity and inflammation. Gensollen T, Iyer SS, Kasper DL, Blumberg RS. How colonization by microbiota in early life shapes the immune system.
Mucosal immunity and the microbiome. Annals ATS. Shanahan F, Ghosh TS, O'Toole PW. The healthy microbiome — what is the definition of a healthy gut microbiome?
Bjarnason I, Macpherson A, Hollander D. Intestinal permeability: an overview. Deitch EA. The role of intestinal barrier failure and bacterial translocation in the development of systemic infection and multiple organ failure.
Arch Surg. Raetz CRH, Whitfield C. Lipopolysaccharide endotoxins. Annu Rev Biochem. Natividad JMM, Verdu EF. Modulation of intestinal barrier by intestinal microbiota: pathological and therapeutic implications.
Pharmacol Res. Lepage P, Leclerc MC, Joossens M, Mondot S, Blottière HM, Raes J, et al. A metagenomic insight into our gut's microbiome.
Wikoff WR, Anfora AT, Liu J, Schultz PG, Lesley SA, Peters EC, et al. Metabolomics analysis reveals large effects of gut microflora on mammalian blood metabolites. Proc Natl Acad Sci. Aya V, Flórez A, Perez L, Ramírez JD. Association between physical activity and changes in intestinal microbiota composition: a systematic review.
PLoS ONE. Cook MD, Martin SA, Williams C, Whitlock K, Wallig MA, Pence BA, et al. Forced treadmill exercise training exacerbates inflammation and causes mortality while voluntary wheel training is protective in a mouse model of colitis.
Brain Behav Immun. Jost L. Partitioning diversity into independent alpha and beta components. Zhao X, Zhang Z, Hu B, Huang W, Yuan C, Zou L.
Response of gut microbiota to metabolite changes induced by endurance exercise. Front Microbiol. Cronin O, Barton W, Skuse P, Penney NC, Garcia-Perez I, Murphy EF, et al.
Castell LM, Poortmans JR, Leclercq R, Brasseur M, Duchateau J, Newsholme EA. Some aspects of the acute phase response after a marathon race, and the effects of glutamine supplementation. Eur J Appl Physiol.
Suzuki K, Yamada M, Kurakake S, Okamura N, Yamaya K, Liu Q, et al. Circulating cytokines and hormones with immunosuppressive but neutrophil-priming potentials rise after endurance exercise in humans. Suzuki K, Nakaji S, Yamada M, Totsuka M, Sato K, Sugawara K.
Systemic inflammatory response to exhaustive exercise. Cytokine kinetics. Exerc Immunol Rev. PubMed Abstract Google Scholar. Clarke SF, Murphy EF, O'Sullivan O, Lucey AJ, Humphreys M, Hogan A, et al. Exercise and associated dietary extremes impact on gut microbial diversity.
Jeukendrup AE, Vet-Joop K, Sturk A, Stegen JHJC, Senden J, Saris WHM, et al. Relationship between gastro-intestinal complaints and endotoxaemia, cytokine release and the acute-phase reaction during and after a long-distance triathlon in highly trained men.
Clin Sci. Karl JP, Margolis LM, Madslien EH, Murphy NE, Castellani JW, Gundersen Y, et al. Changes in intestinal microbiota composition and metabolism coincide with increased intestinal permeability in young adults under prolonged physiological stress. Am J Physiol Gastrointest Liver Physiol.
Snipe RMJ, Khoo A, Kitic CM, Gibson PR, Costa RJS. Carbohydrate and protein intake during exertional heat stress ameliorates intestinal epithelial injury and small intestine permeability. Appl Physiol Nutr Metab. Keohane DM, Woods T, O'Connor P, Underwood S, Cronin O, Whiston R, et al. Four men in a boat: ultra-endurance exercise alters the gut microbiome.
J Sci Med Sport. Estaki M, Pither J, Baumeister P, Little JP, Gill SK, Ghosh S, et al. Cardiorespiratory fitness as a predictor of intestinal microbial diversity and distinct metagenomic functions. Durk RP, Castillo E, Márquez-Magaña L, Grosicki GJ, Bolter ND, Lee CM, et al.
Gut microbiota composition is related to cardiorespiratory fitness in healthy young adults. Int J Sport Nutr Exerc Metab. Morita E, Yokoyama H, Imai D, Takeda R, Ota A, Kawai E, et al.
Aerobic exercise training with brisk walking increases intestinal bacteroides in healthy elderly women. Allen JM, Mailing LJ, Niemiro GM, Moore R, Cook MD, White BA, et al. Exercise alters gut microbiota composition and function in lean and obese humans. Med Sci Sports Exerc. Bressa C, Bailén-Andrino M, Pérez-Santiago J, González-Soltero R, Pérez M, Montalvo-Lominchar MG, et al.
Differences in gut microbiota profile between women with active lifestyle and sedentary women. Munukka E, Ahtiainen JP, Puigbó P, Jalkanen S, Pahkala K, Keskitalo A, et al. Six-week endurance exercise alters gut metagenome that is not reflected in systemic metabolism in over-weight women.
Motiani KK, Collado MC, Eskelinen JJ, Virtanen KA, Löyttyniemi E, Salminen S, et al. Exercise training modulates gut microbiota profile and improves endotoxemia.
Barton W, Cronin O, Garcia-Perez I, Whiston R, Holmes E, Woods T, et al. The effects of sustained fitness improvement on the gut microbiome: a longitudinal, repeated measures case-study approach.
Transl Sports Med. Barton W, Penney NC, Cronin O, Garcia-Perez I, Molloy MG, Holmes E, et al. The microbiome of professional athletes differs from that of more sedentary subjects in composition and particularly at the functional metabolic level.
O'Donovan CM, Madigan SM, Garcia-Perez I, Rankin A, O' Sullivan O, Cotter PD. Distinct microbiome composition and metabolome exists across subgroups of elite Irish athletes. Petersen LM, Bautista EJ, Nguyen H, Hanson BM, Chen L, Lek SH, et al. Community characteristics of the gut microbiomes of competitive cyclists.
Murtaza N, Burke LM, Vlahovich N, Charlesson B, O' Neill H, Ross ML, et al. The effects of dietary pattern during intensified training on stool microbiota of elite race walkers. Queipo-Ortuño MI, Seoane LM, Murri M, Pardo M, Gomez-Zumaquero JM, Cardona F, et al. Gut microbiota composition in male rat models under different nutritional status and physical activity and its association with serum leptin and ghrelin levels.
Denou E, Marcinko K, Surette MG, Steinberg GR, Schertzer JD. High-intensity exercise training increases the diversity and metabolic capacity of the mouse distal gut microbiota during diet-induced obesity. Am J Physiol Endocrinol Metab. Brandt N, Kotowska D, Kristensen CM, Olesen J, Lützhøft DO, Halling JF, et al.
The impact of exercise training and resveratrol supplementation on gut microbiota composition in high-fat diet fed mice. Physiol Rep. McCabe LR, Irwin R, Tekalur A, Evans C, Schepper JD, Parameswaran N, et al. Exercise prevents high fat diet-induced bone loss, marrow adiposity and dysbiosis in male mice.
Choi JJ, Eum SY, Rampersaud E, Daunert S, Abreu MT, Toborek M. Exercise attenuates PCB-induced changes in the mouse gut microbiome.
Environ Health Perspect. Kang SS, Jeraldo PR, Kurti A, Miller MEB, Cook MD, Whitlock K, et al. Diet and exercise orthogonally alter the gut microbiome and reveal independent associations with anxiety and cognition. Mol Neurodegener. Lambert JE, Myslicki JP, Bomhof MR, Belke DD, Shearer J, Reimer RA.
Exercise training modifies gut microbiota in normal and diabetic mice. Feng X, Uchida Y, Koch L, Britton S, Hu J, Lutrin D, et al. Exercise prevents enhanced postoperative neuroinflammation and cognitive decline and rectifies the gut microbiome in a rat model of metabolic syndrome.
Front Immunol. Matsumoto M, Inoue R, Tsukahara T, Ushida K, Chiji H, Matsubara N, et al. Voluntary running exercise alters microbiota composition and increases n-butyrate concentration in the rat cecum. Biosci Biotechnol Biochem.
Huang W-C, Chen Y-H, Chuang H-L, Chiu C-C, Huang C-C. Investigation of the effects of microbiota on exercise physiological adaption, performance, and energy utilization using a gnotobiotic animal model. Nay K, Jollet M, Goustard B, Baati N, Vernus B, Pontones M, et al. Gut bacteria are critical for optimal muscle function: a potential link with glucose homeostasis.
Okamoto T, Morino K, Ugi S, Nakagawa F, Lemecha M, Ida S, et al. Microbiome potentiates endurance exercise through intestinal acetate production. Lai Z-L, Tseng C-H, Ho HJ, Cheung CKY, Lin J-Y, Chen Y-J, et al. Fecal microbiota transplantation confers beneficial metabolic effects of diet and exercise on diet-induced obese mice.
Sci Rep. Liu Z, Dai X, Zhang H, Shi R, Hui Y, Jin X, et al. Gut microbiota mediates intermittent-fasting alleviation of diabetes-induced cognitive impairment. Nat Commun. Bergman EN.
Energy contributions of volatile fatty acids from the gastrointestinal tract in various species. Layden BT, Angueira AR, Brodsky M, Durai V, Lowe WL.
Short chain fatty acids and their receptors: new metabolic targets. Transl Res. Mitchell CM, Davy BM, Hulver MW, Neilson AP, Bennett BJ, Davy KP. Does exercise alter gut microbial composition? Jones JM. Nutr J. The International Food Information Council Foundation. Fiber Fact Sheet. Google Scholar.
Tap J, Furet J-P, Bensaada M, Philippe C, Roth H, Rabot S, et al. Gut microbiota richness promotes its stability upon increased dietary fibre intake in healthy adults. Environ Microbiol. Besten G den, Eunen K van, Groen AK, Venema K, Reijngoud D-J, Bakker BM.
The role of short-chain fatty acids in the interplay between diet, gut microbiota, and host energy metabolism. The fundamental role our microbes play in energy regulation and athletic recovery has researchers exploring questions like:.
Could we harvest the microbes of professional athletes to pass on high performing microbial capabilities? While no one can possibly predict the end result of these findings, the implications are thrilling.
First, we are going to explore some of the exciting possibilities recent gut microbiome research suggests, followed by 9 ways the gut microbiome impacts athletic performance. Imagine a world where you could mimic Michael Jordan's gut microbiome to improve your athletic abilities.
What if you could jump higher, run faster, and outlast the competition with a Michael Jordan probiotic? This may sound like it came straight out of a sci-fi novel, but take a look at some of the most fascinating related research. These findings now have researchers looking for ways to increase the good guys for better performance and faster recovery.
In one study, a group of Harvard researchers sampled the gut microbiomes of athletes training for the Boston Marathon.
After the marathon, they found a spike in one type of bacteria needed by the body to break down lactic acid. In another study, Harvard researchers compared the gut microbiomes of rowers and ultramarathoners. They found differences in composition, which suggests that certain sports might foster certain microbial ecosystems.
You probably aren't surprised to hear that the scientific findings have led to the quest for performance-based prebiotics and probiotics.
Exercise also has the ability to affect the gut microbiome — making this relationship a two-way street. Though diet is the most influential factor in determining which microbes are in your gut, environmental factors play a role too.
Specifically, moderate exercise can: 4. Enrich microbiota diversity — Which is important for signaling along the brain-gut access and body homeostasis. Improve the Bacteroides to Firmicute s ratio — Which helps healthy weight maintenance and reduces risk for obesity-related conditions.
Stimulate bacteria known to improve the gastrointestinal lining barrier functions — Which can help fight obesity and metabolic diseases. Stimulate bacteria activities beneficial to human health — Some protect against gastrointestinal disorders and colon cancer. In case you needed another motivator to get up and go for a run, here it is — when you exercise, you can improve the health of your gut microbiome, which may make it easier for you to stay lean and healthy overall.
A healthy gut microbiome makes being healthy overall easier. However, just like so many things in life, you can have too much of a good thing.
Extreme physical exercise can cause dysbiosis — an imbalance of the gut microbiome — which is a major underlying cause of many diseases.
This means in some cases, over exercising could cause you more harm than good. Ultra athletes put incredible demands on their body when they train, both physiologically and biochemically.
The demand not only elicits responses from the muscles, but across the entire body and can result in systemic reactions. Finding this takes personal experimentation.
To answer this question accurately we have to examine exactly what the science tells us. The gut microbiome plays a significant role in inflammation — either increasing or decreasing levels. Inflammation interferes with athletic performance, slows recovery, and is the root cause of many chronic diseases.
Research shows that improving your microbiome balance reduces systemic inflammation, which provides both short term relief and long term risk reduction.
When it comes to inflammation, the gut microbiome can either work for you or against you. In the case of ultra athletes, they may be unknowingly optimizing their gut microbiome through experimentation OR causing chaos when they overtrain. When your gut microbiome is happy and healthy it helps boost energy levels, which can translate into better performance by:.
Reducing fatigue through better lactic acid breakdown. Controlling redox function, which can delay fatigue symptoms. Increasing ATP levels, your molecular energy. Modulating metabolism. Regulating energy harvest, storage, and expenditure. Athletes rely on their high energy levels to launch themselves past their competitors and beyond.
They must have a gut microbiome that operates at peak performance if they want to stand a chance. You might be surprised to hear this, but your gut microbes talk to your brain along the vagus nerve.
They have a huge role in the state of your mental health and when they are imbalanced, they can contribute to mental illness. Dysbiosis gut microbiome imbalance has even been linked to anxiety and depression. On the flip side, a healthy gut microbiome composition can contribute to mental strength.
The composition of the gut microbiome significantly affects: 3. So, when the gut microbiome is in good shape it can make being healthier, easier. This is because the gut microbiome influences: Every athlete knows just how important these factors are to overall performance.
Gut microbiota anr exercise have recently been shown to be wnd. Both moderate Natural remedies for balanced glucose levels Sugar metabolism Natural remedies for balanced glucose levels are typically perforamnce of the training regimen of endurance athletes, but they exert different effects on health. Moderate exercise has positive effects on the health of average athletes, such as a reduction in inflammation and intestinal permeability and an improvement in body composition. It also induces positive changes in the gut microbiota composition and in the microbial metabolites produced in the gastrointestinal tract. Conversely, intense exercise can increase gastrointestinal epithelial wall permeability and diminish gut mucus thickness, potentially enabling pathogens to enter the bloodstream. Whether you're an amateur athlete or a weekend warrior, it's likely you Natural remedies for balanced glucose levels perfrmance into your Gut health and physical performance schedule. Hezlth train lerformance muscles hexlth strength and endurance, and you may Immune-boosting vitamins about cardiovascular performancee as well. But have you thought Natural remedies for balanced glucose levels how exercise may impact your gut health and vice versa? Researchers are learning more and more about gut microbiota — the bacteria that live in the gastrointestinal tract — and how it can help support physical performance. In short, here's how it works: When you consume foods with fiber — such as fruits, vegetables and beans — your microbiota helps break down or ferment fiber, which produces short-chain fatty acids SCFAs. SCFAs have been associated with a wide array of health benefits related to heart healthblood sugar control, and weight loss and maintenance. Your gut microbiota supports your immune system by strengthening the gut barrier to keep out potentially harmful bacteria.
Ich tue Abbitte, es nicht ganz, was mir notwendig ist.
Ich denke, dass Sie den Fehler zulassen. Geben Sie wir werden es besprechen. Schreiben Sie mir in PM, wir werden reden.
Nach meiner Meinung irren Sie sich. Geben Sie wir werden es besprechen. Schreiben Sie mir in PM.
Es ist unwahrscheinlich.