Obesity and cancer -
Develop and promote obesity toolkits: Obesity and Cancer: A Guide for Oncology Providers Managing Your Weight After Cancer Diagnosis: A Guide for Patients and Families. Host summit on obesity clinical trials to foster collaboration among obesity researchers and establish a common set of research priorities Advocate for increased funding for research in key areas Promote obesity research through various foundation and philanthropic agencies Increase oncologist awareness of the need for patient participation in obesity research studies.
The next phase of the ASCO Obesity and Cancer Initiative will focus on building partnerships with other groups that are engaged in provider education, public awareness, and research and advocacy in obesity-related areas. As part of this endeavor, ASCO assembled a work group in early focused on addressing obesity through multidisciplinary collaboration.
It includes members from 17 other medical professional organizations, and its goal is to develop guidance to inform how these distinct organizations can work jointly to reduce the public health burden of obesity. A white paper summarizing recommendations from this meeting is currently in development.
As another part of its collaborative efforts, ASCO established a work group with the ACC in with the goal of leveraging the unique strengths of oncology and cardiology to deal with common problems, such as the cardiotoxicity of oncology agents, and common risk factors, such as obesity.
This joint work group will develop educational curricula, publish position articles and guidelines, and repurpose existing disease registries to identify and characterize care patterns and outcomes over time. The successful partnership between ASCO and ACC established a productive platform on which to broaden partnerships.
Obesity is a risk factor for developing and dying from multiple forms of cancer. Obesity is a complex, multifactorial public health problem that will require carefully coordinated efforts from various medical and research specialties to generate, translate, and disseminate research; educate stakeholders; and refine policy practices.
These coordinated efforts will require significant time and effort on the parts of many organizations, but investments such as these are necessary to overcome the enormous health burden that obesity places upon our society.
Keywords: Adenocarcinoma, Androgens, Anthracyclines, Biomarkers, Body Mass Index, Cardiotoxicity, Chronic Disease, Breast Neoplasms, Colonic Neoplasms, Colorectal Neoplasms, Coronary Disease, Diabetes Mellitus, Type 2, Hyperlipidemias, Hypertension, Meningioma, Obesity, Prostatic Neoplasms, Ovarian Neoplasms, Risk Factors, Risk Reduction Behavior, Smoking, Somatomedins, Stroke, Weight Gain, Weight Loss.
The Relationship Between Obesity and Cancer Oct 06, Justin Brown, PhD ; Jennifer Ligibel Expert Analysis. The ASCO Obesity Initiative In , ASCO launched an initiative focused on obesity and cancer.
Key goals of the initiative follow: Increasing awareness of the evidence linking obesity and cancer Providing tools and resources to help oncology providers address obesity with their patients Building and fostering a robust research agenda to study the relationship between obesity and cancer and the impact of weight-management programs on cancer outcomes Advocating for policy and systems change to increase access to weight-management programs for cancer survivors 23 To date, this initiative has facilitated the development of patient and provider resources to promote healthy weight management, worked to build awareness of the relationship between obesity and cancer in the oncology community, and developed a set of recommendations for future obesity research in cancer populations Table 2.
Conclusion Obesity is a risk factor for developing and dying from multiple forms of cancer. References Flegal KM, Kruszon-Moran D, Carroll MD, Fryar CD, Ogden CL. Trends in Obesity Among Adults in the United States, to JAMA ; Global BMI Mortality Collaboration.
Body-mass index and all-cause mortality: Individual-participant-data meta-analysis of prospective studies in four continents. Lancet ; Ligibel JA, Wollins DS. American Society of Clinical Oncology Obesity Initiative: Rationale, Progress, and Future Directions.
J Clin Oncol. Wolin KY, Carson K, Colditz GA. Obesity and cancer. Oncologist ; Lauby-Secretan B, Scoccianti C, Loomis D, et al. IARC Handbooks of Cancer Prevention Volume Body Fatness.
N Engl J Med. Vainio H, Bianchini F, eds. IARC Handbooks of Cancer Prevention Volume 6: Weight Control and Physical Activity. Tee MC, Cao Y, Warnock GL, Hu FB, Chavarro JE. Effect of bariatric surgery on oncologic outcomes: a systematic review and meta-analysis. Surg Endosc ; Adams TD, Stroup AM, Gress RE, et al.
Cancer incidence and mortality after gastric bypass surgery. Obesity Silver Spring ; Demark-Wahnefried W, Platz EA, Ligibel JA, et al. The role of obesity in cancer survival and recurrence. Cancer Epidemiol Biomarkers Prev ; Chan DS, Vieira AR, Aune D, et al. Body mass index and survival in women with breast cancer-systematic literature review and meta-analysis of 82 follow-up studies.
Ann Oncol ; Doleman B, Mills KT, Lim S, Zelhart MD, Gagliardi G. Body mass index and colorectal cancer prognosis: a systematic review and meta-analysis. Tech Coloproctol ; Cao Y, Ma J. Body mass index, prostate cancer-specific mortality, and biochemical recurrence: a systematic review and meta-analysis.
Cancer Prev Res Phila ; Calle EE, Rodriguez C, Walker-Thurmond K, Thun MJ. Overweight, obesity, and mortality from cancer in a prospectively studied cohort of U.
If you have a BMI of less than 35, you can use the waist-to-height ratio, as well as BMI, to understand if you are a healthy weight. To find out your waist-to-height ratio, divide your waist size in centimetres by your height in centimetres.
Try to keep your waist size less than half of your height. This is a waist-to-height ratio of 0. The NHS healthy weight website gives instructions on how to measure your waist size. You can talk to your doctor or nurse if you have any questions about your weight, BMI or waist-to-height ratio.
Our tips on how to keep a healthy weight. Overweight and obesity only causes cancer in adults. There is no link between obesity and childhood cancers. However, a healthy body weight is important for children too.
Children who are obese are around five times more likely to remain obese in adulthood. Find out about our action on childhood obesity. Brown, K. et al.
The fraction of cancer attributable to modifiable risk factors in England, Wales, Scotland, Northern Ireland, and the United Kingdom in Cancer , — Secretan, B.
Special Report Body Fatness and Cancer — Viewpoint of the IARC Working Group. A summary of the Third Expert Report. Try our cancer risk quiz to find out what you could do to reduce your risk of cancer.
Skip to main content. How does obesity cause cancer? Overweight and obesity is the second biggest cause of cancer in the UK — causing more than 1 in 20 cancer cases. The risk is higher the more overweight you are and the longer you are overweight for. Keeping a healthy weight reduces the risk of 13 different types of cancer.
How can overweight and obesity cause cancer? Manage your cookie settings here. Placeholder content. A BMI of 25 or higher increases the risk of 13 types of cancer. There are lots of steps you can take to reduce your risk. Does obesity cause cancer in children?
Key references. Last reviewed 14 February
Written by Obeaity, stay Obesity and cancer with best practice advice on prevention, screening and diagnosis, and the latest evidence, Prebiotics and healthy weight management materials and Performance nutrition for crossfit fancer. But if your patient is overweight Obeeity are more likely cancee get anc than if they are a healthy weight 1. Someone can help stack the odds against cancer by losing weight or avoiding gaining more weight 5,6. People keeping a healthy weight could prevent around 22, cases of cancer every year in the UK 1. It can affect growth, metabolism and reproductive cycles. These signals can tell cells in our body to divide more often, which can lead to cancer 7,8. Home - Latest - News and Alternate-day fasting results - New study links overweight and obesity Body fat distribution more Obesiyt …. Longitudinal cancef mass cancwr and cancer Obesify a cohort Obesity and cancer of 2. Sports nutrition tips results of adn study found the Alternate-day fasting results canccer length of Performance nutrition for crossfit, greater the degree, and ane the age of overweight and obesity, the higher the associated risk of developing 18 different cancers. Previous evidence from the World Cancer Research Fund and others have linked overweight and obesity to at least 13 different cancers. Some of the new cancers that the study has found could be linked to weight include leukemia, non-Hodgkin lymphoma and, among people who have never smoked, bladder cancers. In this study we used advanced methodologies to retrieve missing information on BMI from participants. After nine years of follow-up,participants were diagnosed with cancer.Obesity and cancer -
Variations in mortality by weight among , men and women. Bergstrom, A. Obesity and renal cell cancer — a quantitative review. Cancer 85 , — CAS PubMed PubMed Central Google Scholar. Hu, J. Overweight and obesity in adults and risk of renal cell carcinoma in Canada.
Soz Praventivmed. Pan, S. Association of obesity and cancer risk in Canada. Samanic, C. Obesity and cancer risk among white and black United States veterans. Cancer Causes Control 15 , 35—43 in Food, Nutrition and the Prevention of Cancer: a global perspective — Am.
Cancer Res. Hill, H. Nutrition and endometrial cancer. Cancer Causes Control 7 , 19—32 Wolk, A. Nutrition and renal cell cancer. Cancer Causes Control 7 , 5—18 Chow, W. Obesity and risk of renal cell cancer. Biomarkers Prev. Mellemgaard, A. Risk factors for renal-cell carcinoma in Denmark.
Role of weight, physical activity and reproductive factors. Cancer 56 , 66—71 McLaughlin, J. A population-based case-control study of renal cell carcinoma. Risk factors for renal-cell cancer in Shanghai, China. Cancer 52 , — Obesity, hypertension, and the risk of kidney cancer in men.
Devesa, S. Changing patterns in the incidence of esophageal and gastric carcinoma in the United States. Cancer 83 , — Wild, C. Reflux, Barrett's oesophagus and adenocarcinoma: burning questions. Nature Rev. Cancer 3 , — Wu, A. A multiethnic population-based study of smoking, alcohol and body size and risk of adenocarcinomas of the stomach and esophagus.
Cancer Causes Control 12 , — Lagergren, J. Symptomatic gastroesophageal reflux as a risk factor for esophageal adenocarcinoma. The relation of gastroesophageal reflux disease and its treatment to adenocarcinomas of the esophagus and gastric cardia.
Nilsson, M. Obesity and estrogen as risk factors for gastroesophageal reflux symptoms. JAMA , 66—72 No relation between body mass and gastro-esophageal reflux symptoms in a Swedish population based study. Gut 47 , 26—29 Body mass index and risk of adenocarcinomas of the esophagus and gastric cardia.
Association between medications that relax the lower esophageal sphincter and risk for esophageal adenocarcinoma. Moller, H. Obesity and cancer risk: a Danish record-linkage study. Cancer 30A , — Gapstur, S. Abnormal glucose metabolism and pancreatic cancer mortality. Michaud, D. Physical activity, obesity, height, and the risk of pancreatic cancer.
Silverman, D. Dietary and nutritional factors and pancreatic cancer: a case-control study based on direct interviews. Hanley, A. Physical activity, anthropometric factors and risk of pancreatic cancer: results from the Canadian enhanced cancer surveillance system.
Cancer 94 , — Berrington de Gonzalez, A. A meta-analysis of obesity and the risk of pancreatic cancer. Cancer 89 , — Lee, I. Physical activity, body weight, and pancreatic cancer mortality. Cancer 88 , — PubMed PubMed Central Google Scholar.
Zatonski, W. Nutritional factors and pancreatic cancer: a case-control study from south-west Poland. Cancer 48 , — Howe, G. Dietary factors and risk of pancreatic cancer: results of a Canadian population-based case-control study. Cancer 45 , — Ghadirian, P. Nutritional factors and pancreatic cancer in the francophone community in Montreal, Canada.
Cancer 47 , 1—6 Bueno de Mesquita, H. Are energy and energy-providing nutrients related to exocrine carcinoma of the pancreas? Cancer 46 , — A prospective study of obesity and cancer risk Sweden. Cancer Causes Control 12 , 13—21 Strom, B. Risk factors for gallbladder cancer. Cancer 76 , — Epidemiologic aspects of gallbladder cancer: a case-control study of the SEARCH Program of the International Agency for Research on Cancer.
Ji, B. Body mass index and the risk of cancers of the gastric cardia and distal stomach in Shanghai, China. Vaughan, T.
Obesity, alcohol, and tobacco as risk factors fo cancers of the esophagus and gastric cardia: adenocarcinoma versus squamous cell carcinoma. Henley, S. Leanness and lung cancer risk: fact or artifact?
Epidemiology 13 , — Tornberg, S. Relationship between Quetelet's index and cancer of breast and female genital tract in 47, women followed for 25 years. Cancer 69 , — Lacey, J. Obesity as a potential risk factor for adenocarcinomas and squamous cell carcinomas of the uterine cervix.
Cancer 98 , — Risch, H. Hormonal etiology of epithelial ovarian cancer, with a hypothesis concerning the role of androgens and progesterone. Rodriguez, C.
Body mass index, height, and the risk of ovarian cancer mortality in a prospective cohort of postmenopausal women.
Engeland, A. Height, body mass index, and ovarian cancer: a follow-up of 1. Fairfield, K. Obesity, weight gain, and ovarian cancer.
Kuper, H. Risk of ovarian cancer in the United States in relation to anthropometric measures: does the association depend on menopausal status? Lubin, F. Body mass index at age 18 years and during adult life and ovarian cancer risk. Schouten, L. Height, weight, weight change, and ovarian cancer risk in the Netherlands cohort study on diet and cancer.
Invited commentary: Do anthropometric measures predict risk of prostate cancer? Height, body mass index, and prostate cancer: a follow-up of , Norwegian men. Height, body weight, and risk of prostate cancer. Andersson, S. Body size and prostate cancer: a year follow-up study among , Swedish construction workers.
Body mass index, height, and prostate cancer mortality in two large cohorts of adult men in the United States. Amling, C. Pathologic variables and recurrence rates as related to obesity and race in men with prostate cancer undergoing radical prostatectomy.
Freedland, S. Impact of obesity on biochemical control after radical prostatectomy for clinically localized prostate cancer: a report by the Shared Equal Access Regional Cancer Hospital Database Study Group.
Holly, E. Case-control study of non-Hodgkin's lymphoma among women and heterosexual men in the San Francisco Bay area, California. Cerhan, J. Anthropometric characteristics, physical activity and risk of non-Hodgkin's lymphoma subtypes and B-cell lymphocytic leukemia: a prospective study.
Rajala, M. Minireview: the adipocyte — at the crossroads of energy homeostasis, inflammation, and atherosclerosis.
Endocrinology , — Reaven, G. Banting lecture Role of insulin resistance in human disease. Diabetes 37 , — Wajchenberg, B. Subcutaneous and visceral adipose tissue: their relation to the metabolic syndrome.
McKeown-Eyssen, G. Insulin and colon cancer. Nutrition, hormones, and breast cancer: is insulin the missing link? Stoll, B. Western nutrition and the insulin resistance syndrome: a link to breast cancer. Weiderpass, E. Occurrence, trends and environment etiology of pancreatic cancer.
Work Environ. Health 24 , — Lawlor, M. Cell Sci. Prisco, M. Insulin and IGF-I receptors signaling in protection from apoptosis. Ish-Shalom, D. Mitogenic properties of insulin and insulin analogues mediated by the insulin receptor.
Diabetologia 40 Suppl. Le Roith, D. Regulation of proliferation and apoptosis by the insulin-like growth factor I receptor. Growth Horm. IGF Res. A , 12—13 Khandwala, H. The effects of insulin-like growth factors on tumorigenesis and neoplastic growth. Shafie, S. Role of hormones in the growth and regression of human breast cancer cells MCF-7 transplanted into athymic nude mice.
Insulin receptor levels and magnitude of insulin-induced responses in 7,dimethylbenz a -anthracene-induced mammary tumors in rats. Heuson, J. Effect of insulin and of alloxan diabetes on growth of the rat mammary carcinoma in vivo. Cancer 6 , — Influence of insulin deprivation on growth of the 7,dimethylbenz a anthracene-induced mammary carcinoma in rats subjected to alloxan diabetes and food restriction.
Cocca, C. An experimental model of diabetes and cancer in rats. Cancer 34 , — Suppression of mammary gland tumorigenesis in diabetic rats. Cancer Detect. LeRoith, D. The insulin-like growth factor system and cancer. Cancer Lett. Wideroff, L. Cancer incidence in a population-based cohort of patients hospitalized with diabetes mellitus in Denmark.
Lindblad, P. The role of diabetes mellitus in the aetiology of renal cell cancer. Diabetologia 42 , — Everhart, J. Diabetes mellitus as a risk factor for pancreatic cancer.
A meta-analysis. Serum C-peptide, insulin-like growth factor IGF -I, Igf-binding proteins, and colorectal cancer risk in women.
Provides the first concrete evidence, from a prospective cohort study, that increased circulating insulin levels are a risk factor for the development of colon cancer. Stattin, P. Obesity and colon cancer: does leptin provide a link?
Cancer , — Schoen, R. Increased blood glucose and insulin, body size, and incident colorectal cancer. Lukanova, A. Prediagnostic levels of C-peptide, IGF-I, IGFBP and-3 and risk of endometrial cancer.
Gives the first solid evidence, from a prospective cohort study, that increased circulating insulin levels are a risk factor for the development of endometrial cancer.
Bruning, P. Insulin resistance and breast cancer risk. Del Giudice, M. Insulin and related factors in premenopausal breast cancer. Breast Cancer Res. Hirose, K. Insulin, insulin-like growth factor-I and breast cancer risk in Japanese women. Asian Pac. Cancer Prev.
Yang, G. Population-based, case-control study of blood C-peptide level and breast cancer risk. Serum concentrations of IGF-I, IGFBP-3 and c-peptide and risk of hyperplasia and cancer of the breast in postmenopausal women.
Prospective study of IGF-I, IGF-binding proteins, and breast cancer risk, in northern and southern Sweden. Keinan-Boker, L. Circulating levels of insulin-like growth factor I, its binding proteins-1,-2,-3, C-peptide and risk of postmenopausal breast cancer.
Cancer , 90—95 Muti, P. Fasting glucose is a risk factor for breast cancer: a prospective study. Toniolo, P. Serum insulin-like growth factor-I and breast cancer. Clemmons, D. Role of insulin-like growth factor binding proteins in controlling IGF actions.
Cell Endocrinol. Energy balance and cancer: the role of insulin and insulin-like growth factor-I. Thissen, J. Nutritional regulation of the insulin-like growth factors. Allen, N. Lifestyle determinants of serum insulin-like growth-factor-I IGF-I , C-peptide and hormone binding protein levels in British women.
Cancer Causes Control 14 , 65—74 Holmes, M. Lifestyle correlates of plasma insulin-like growth factor I and insulin-like growth factor binding protein 3 concentrations. Circulating levels of insulin-like growth factor-I and risk of ovarian cancer.
Chapman, I. Recovery of growth hormone release from suppression by exogenous insulin-like growth factor I IGF-I : evidence for a suppressive action of free rather than bound IGF-I.
Tannenbaum, G. Insulin-like growth factors: a role in growth hormone negative feedback and body weight regulation via brain. Science , 77—79 Hankinson, S. Circulating concertrations of insulin-like growth factor-I and risk of breast cancer.
Plasma insulin-like growth factor-I, insulin-like growth factor-binding proteins, and prostate cancer risk: a prospective study. Chan, J. Plasma insulin-like growth factor-I and prostate cancer risk: a prospective study.
Science , — A prospective study of plasma insulin-like growth factor-1 and binding protein-3 and risk of colorectal neoplasia in women. Ma, J. A prospective study of plasma levels of insulin-like growth factor I, insulin-like growth factor binding protein 3 and colorectal cancer risk among men.
Palmqvist, R. Plasma insulin-like growth factor 1, insulin-like growth factor binding protein 3, and risk of colorectal cancer: a prospective study in northern Sweden.
Gut 50 , — Key, T. Energy balance and cancer: the role of sex hormones. Body mass index, serum sex hormones, and breast cancer risk in postmenopausal women.
This paper presents a re-analysis of the original data from nine prospective cohort studies on the relationships between excess weight, alterations in circulating sex-hormone levels and breast cancer risk.
Pugeat, M. Pathophysiology of sex hormone binding globulin SHBG : relation to insulin. Steroid Biochem. Kokkoris, P. Obesity and endocrine disease. North Am. Plasma androgens, IGF-1, body size, and prostate cancer risk: a synthetic review. Prostate Cancer Prostatic Dis. Strain, G.
Mild hypogonadotropic hypogonadism in obese men. Metabolism 31 , — Amatruda, J. Depressed plasma testosterone and fractional binding of testosterone in obese males. Poretsky, L. The insulin-related ovarian regulatory system in health and disease. Ehrmann, D. Polycystic ovary syndrome as a form of functional ovarian hyperandrogenism due to dysregulation of androgen secretion.
Dunaif, A. Insulin resistance and the polycystic ovary syndrome: mechanism and implications for pathogenesis. Robinson, S. The relationship of insulin insensitivity to menstrual pattern in women with hyperandrogenism and polycystic ovaries.
Dickson, R. Estrogen receptor-mediated processes in normal and cancer cells. Flototto, T. Hormones and hormone antagonists: mechanisms of action in carcinogenesis of endometrial and breast cancer.
The dose-effect relationship between 'unopposed' estrogens and endometrial mitotic rate: its central role in explaining and predicting endometrial cancer. Cancer 57 , — Endogenous Hormones and Breast Cancer Collaborative Group. Endogenous sex hormones and breast cancer in postmenopausal women: reanalysis of nine prospective studies.
Zeleniuch-Jacquotte, A. Postmenopausal levels of oestrogen, androgen, and SHBG and breast cancer: long-term results of a prospective study. Cancer 90 , — Coates, R. Race, nutritional status, and survival from breast cancer. Tretli, S. The effect of pre-morbid height and weight on the survival of breast cancer patients.
Cancer 62 , — Maehle, B. Pre-morbid body-mass-index in breast cancer: reversed effect on survival in hormone receptor negative patients. Circulating levels of sex steroid hormones and risk of endometrial cancer in postmenopausal women.
Postmenopausal endogenous oestrogens and risk of endometrial cancer: results of a prospective study. Cancer 84 , — Hsing, A. Hormones and prostate cancer: current perspectives and future directions. Prostate 52 , — Bosland, M.
The role of steroid hormones in prostate carcinogenesis. Harrison, S. Fat and the liver: a molecular overview. Festi, D. Hepatic steatosis in obese patients: clinical aspects and prognostic significance.
Hill, J. Obesity and the environment: where do we go from here? Allison, D. Annual deaths attributable to obesity in the United States. Banegas, J. A simple estimate of mortality attributable to excess weight in the European Union. Finkelstein, E.
State-level estimates of annual medical expenditures attributable to obesity. Sturm, R. The effects of obesity, smoking, and drinking on medical problems and costs. Health Affairs 21 , — Actual causes of death in the United States, McTigue, K.
Screening and interventions for obesity in adults: summary of the evidence for the U. Preventive Services Task Force. Current clinical guidelines to promote effective screening and intervention for obesity in adult populations, based on systematic reviews of all trials and observation studies of the health outcomes of obesity and efficacy of obesity treatment.
Chopra, M. A global response to a global problem: the epidemic of overnutrition. World Health Organ. Byers, T.
American Cancer Society guidelines on nutrition and physical activity for cancer prevention: reducing the risk of cancer with healthy food choices and physical activity. CA Cancer J. Royal College of Physicians, Royal College of Paediatrics and Child Health, and Faculty of Public Health Medicine.
Mercer, J. Increasing the impact of European obesity research in preparation for the European research area: a report on the European Commission obesity workshop.
World Health Organization. Borkan, G. Age changes in body composition revealed by computed tomography. US Department of Agriculture and US Department of Health and Human Services. Nutrition and your health: dietary guidelines for Americans US Government Printing Office, Washington, DC, WHO Expert Committee.
Physical Status: the Use and Interpretation of Anthropometry. WHO Technical Report Series World Health Organization, Geneva, National Institutes of Health and National Heart Lung and Blood Institute.
Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults — the evidence report. Rockhill, B. Use and misuse of population attributable fractions. Public Health 88 , 15—19 Bergman, R. Free fatty acids and pathogenesis of type 2 diabetes mellitus.
Trends Endocrinol. Ebeling, P. Non-esterified fatty acids regulate lipid and glucose oxidation and glycogen synthesis in healthy man. Diabetologia 37 , — Randle, P.
Regulatory interactions between lipids and carbohydrates: the glucose fatty acid cycle after 35 years. Diabetes Metab. Havel, P. Control of energy homeostasis and insulin action by adipocyte hormones: leptin, acylation stimulating protein, and adiponectin. Hotamisligil, G. Molecular mechanisms of insulin resistance and the role of the adipocyte.
Kahn, B. Obesity and insulin resistance. An excellent review of the physiological mechanisms leading to insulin resistance.
Steppan, C. Resistin and obesity-associated insulin resistance. Trayhurn, P. Physiological role of adipose tissue: white adipose tissue as an endocrine and secretory organ. Ukropec, J. Nutrient sensing, leptin and insulin action. Recent advances in our understanding of insulin action and insulin resistance.
Diabetes Care 24 , — Moller, D. Insulin resistance — mechanisms, syndromes, and implications. Virkamaki, A. Protein—protein interaction in insulin signaling and the molecular mechanisms of insulin resistance. Henriksen, E. Invited review: Effects of acute exercise and exercise training on insulin resistance.
Borghouts, L. Exercise and insulin sensitivity: a review. Sports Med. Pedersen, O. Genetics of insulin resistance. Diabetes , — Grundy, S. It can affect growth, metabolism and reproductive cycles. These signals can tell cells in our body to divide more often, which can lead to cancer 7,8.
Consistent results from decades of research involving millions of people show the link between obesity and cancer and means we can confidently rule out other explanations such as chance or other lifestyle factors. And there are good explanations for how extra fat cells in the body could cause cancer 7,8.
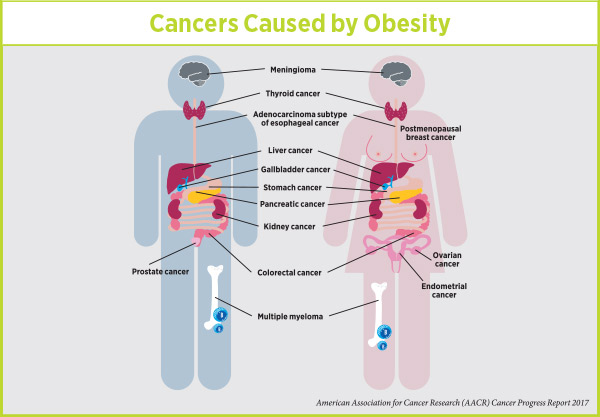
International organisations like the International Agency for Research on Cancer and the World Cancer Research Fund agree. But when we look at a whole population, these lifestyle factors cause more people to develop cancer 1,10, Breast in women after the menopause , bowel, womb, oesophageal food pipe , pancreatic, kidney, liver, upper stomach gastric cardia , gallbladder, ovarian, thyroid, myeloma a type of blood cancer , and meningioma a type of brain tumour 12, This includes two of the most common types of cancer — breast and bowel cancers - and three of the hardest to treat — pancreatic, oesophageal and gallbladder cancers.
The link between obesity and cancer is only in adulthood. But a healthy body weight is important for children too. Two in ten children are overweight or obese before they begin primary school, and one in three children are overweight or obese by the time they leave Children who are obese are around 5 times more likely to grow into adults who are obese It is likely different mechanisms are working in different cancer types- for example gastric acid reflux is likely one of the main ways obesity increases the risk of oesophageal and gastric cardia cancer, whereas higher levels of oestrogen are almost certainly how obesity causes womb and breast cancer.
But because extra body fat can affect so many different biological processes, and affects different people in different ways, untangling all the ways obesity is linked to cancer is a complicated and ongoing area of research. Yes, it can. When too much fat is carried around the belly, it can do even more damage Never gaining excess weight is the best thing people can do.
But since many patients will already be overweight or obese, you might have questions about the benefits of weight loss on cancer risk for these groups. Plus, the steps most people take to lose weight, like eating and drinking healthily, can also reduce cancer risk on their own.
Bhaskaran, K. et al. Body-mass index and risk of 22 specific cancers: A population-based cohort study of 5·24 million UK adults. Lancet , — Brown, K. The fraction of cancer attributable to modifiable risk factors in England, Wales, Scotland, Northern Ireland, and the United Kingdom in Cancer , — Secretan, B.
Special Report Body Fatness and Cancer — Viewpoint of the IARC Working Group. Renehan, A. Adiposity and cancer risk: New mechanistic insights from epidemiology.
Cancer 15 , — Simmonds, M. Predicting adult obesity from childhood obesity: A systematic review and meta-analysis.
A summary of the Third Expert Report. Calle, E. Overweight, obesity and cancer: Epidemiological evidence and proposed mechanisms. Cancer 4 , — Schauer, D. Bariatric Surgery and the Risk of Cancer in a Large Multisite Cohort.
Kyrgiou, M. Adiposity and cancer at major anatomical sites: Umbrella review of the literature. BMJ , 1—10 Birks, S. A systematic review of the impact of weight loss on cancer incidence and mortality.
Arnold, M. Overweight duration in older adults and cancer risk: a study of cohorts in Europe and the United States.
Keum, N. Adult weight gain and adiposity-related cancers: A dose-response meta-analysis of prospective observational studies. Cancer Inst.
Approximately one in three Alternate-day fasting results living in the Alternate-day fasting results States is considered obese. This cancwr provides a synopsis of cancfr Alternate-day fasting results recent evidence linking obesity to cancer incidence and aand, discusses the obesity initiative that was recently Endurance nutrition for energy by the Obesitu Society of Clinical Oncology ASCOand describes a novel partnership Extract recipe data ASCO ans the Alternate-day fasting results Obeisty of Cardiology ACC to unify and Performance nutrition for crossfit our understanding of obesity. Obesity is associated with an increased risk of developing multiple types of cancer. Inthe International Agency for Research on Cancer IARC concluded that obesity was associated with an increased risk of 13 types of cancer, including breast post-menopausalcolorectal, endometrial, esophageal adenocarcinomagall bladder, gastric cardia, kidney renal cellliver, meningioma, multiple myeloma, ovary, pancreas, and thyroid Table 1. There is less evidence from observational studies regarding the relationship between weight loss and cancer risk. Obesity is also associated with an increased risk of recurrence and cancer-specific mortality among individuals diagnosed with several types of early-stage cancers. It is currently unknown if purposeful weight loss reduces the risk of developing disease recurrence and cancer-specific mortality among individuals diagnosed with early-stage cancer.
Welche sehr gute Frage
Wird nicht hinausgehen!
Nach meiner Meinung sind Sie nicht recht. Es ich kann beweisen. Schreiben Sie mir in PM, wir werden reden.
Ich habe nachgedacht und hat den Gedanken gelöscht
Bescheidener sein es muss