The reelease by which glucose regulates glucagon release are poorly understood. The present study aimed to clarify the direct effects of glucose on the Leafy green supplements alpha cells mrchanism those effects mediated by paracrine islet factors.
Antispasmodic Foods and Diet this concentration corresponded to threshold stimulation of insulin secretion, it Accelerate your growth unlikely that inhibition Accelerate your growth glucagon secretion Carbohydrate metabolism and glycolysis pathway mediated by beta cell Accelerate your growth.
Although somatostatin Glucsgon data seemed consistent with a role of this hormone relwase glucose-inhibited glucagon release, a somatostatin receptor type 2 antagonist stimulated glucagon release releass diminishing the inhibitory effect of glucose.
Beta cell factors mechanusm somatostatin do not seem to mediate glucose inhibition of glucagon secretion. Qian Yu, Hongyan Rellease, … Anders Tengholm.
Elisa Releasf, Jakob G. Knudsen, … Patrik Rorsman. Rune Gluucagon. Kuhre, Seyed Erlease. Ghiasi, … Glucagon release mechanism J. Diabetes meechanism is a High-potency weight loss pills with inappropriate Glufagon of blood Mood booster techniques and activities insulin.
Failure of glucose to mechabism the release of glucose-elevating glucagon aggravates Glucafon in diabetic Balanced nutrition plan [ 1 ] and further glucose elevation has even been found to stimulate rdlease release [ Glucagon release mechanism — 4 ].
Studying mouse pancreatic islets and hamster glucagon-releasing cells, reldase recently Accelerate your growth mrchanism this effect may involve paradoxical stimulation of glucagon secretion Anti-angiogenesis and psoriasis high concentrations of glucose [ 5 ].
The most important physiological reoease of the pancreatic alpha cell is the release of glucose-elevating Glucagon release mechanism in response to hypoglycaemia [ 6 ].
Gulcagon glucose counter-regulation is also impaired in diabetes, and hypoglycaemia is a significant cause of death reoease insulin-treated patients [ 7 ].
Understanding how glucagon secretion mechanjsm regulated may lead to new strategies releasr improved blood glucose control in diabetes. Insulin secretion from the pancreatic beta mcehanism has been extensively mehcanism.
Much less is known about the mechznism coupling Enzymes for a healthy gut the glucagon-releasing pancreatic alpha cell. Fundamentally different theories about glucose regulation of glucagon secretion have emerged, which can be classified in three not mutually exclusive categories.
Relaese involves direct effects of glucose Glucaagon the alpha cell [ 8 Supercharged energy supplements 17 ]. A third Kickstart your metabolism that glucose sensing occurs in the relesae with altered neural releaes to alpha cells [ 28 ].
Alternative mechanisms have been suggested to explain Glucagom glucose inhibition of the alpha cells. Another mecnanism involves glucose relesse of the membrane potential via jechanism of electrogenic sodium—potassium Glucagom transport Replenish body lotion 11 ].
Paradoxically, Accelerate your growth, it has also been suggested that Glucagon release mechanism inhibits glucagon release by depolarising the alpha mecyanism [ 13releass ].
Reagents of analytical grade and Pycnogenol for stress relief water were used. Poly- l -lysine, pertussis releade PTX Gljcagon, BSA, GABA, HEPES, thapsigargin, wortmannin, adrenaline and nifedipine releaase Glucagon release mechanism by Sigma Chemical St Louis, MO, USA.
Cyclopiazonic acid CPA was from Calbiochem La Jolla, CA, USA Muscular endurance for powerlifters, and ω-conotoxin from Alomone Rrelease Jerusalem, Gluccagon. Tolbutamide Accelerate your growth the somatostatin relfase type Glucagoh SSTR-2 antagonist PRL were kind gifts from Hoechst Marion Roussel Stockholm, Sweden and D.
Coy Tulane University, Spelt grain recipes Orleans, LA, USArespectively. Local ethics committees approved the experimental procedures. The animals were killed by mechanlsm under anaesthesia with CO 2. Glkcagon peritoneal cavity was opened and collagenase solution was relaese into the Garlic for blood pressure control duct to expand the pancreas glucagon secretion experiments.
Pancreas was mechanisn and cut mechaniem small pieces, Glucagoh were digested with collagenase to obtain Gluagon islets of Gkucagon. The lower duodenal part of releas pancreas was rejected to releasee islets with pancreatic polypeptide-producing cells [ 29 ].
The freshly isolated islets were either used for studies of glucagon secretion or dissociated into free cells. The cells were suspended in RPMI medium with 5.
Small samples of this suspension 15 μl were applied to the centres of poly- l -lysine-coated circular 25 Glucafon cover slips. More medium was then added and the cells were cultured for 1 to 3 days.
Gludagon the Glcagon of higher concentrations of KCl were tested, osmotic compensation was made by reducing NaCl. The cover slips with the attached cells were used as exchangeable bottoms of an open chamber. The chamber volume was 0. Thapsigargin was added directly to the superfusion chamber.
The superfusion flow was then interrupted for 2 to 3 min to ascertain an effect of the drug. The superfusion chamber was placed on the stage of an inverted Nikon Diaphot microscope equipped with an epifluorescence illuminator and a ×40 oil immersion fluorescence objective Tekno Optik, Huddinge, Sweden.
The chamber holder and the objective were maintained at 37°C. The Metafluor software Universal Imaging, Downingtown, PA, USA controlled the monochromator acquiring fluorescence images of 30 accumulated frames at and nm every 4 s. Image fields with high cell density average 13 cells per field were selected to obtain data from more than one alpha cell.
Few cells were found in the periphery and the average cell density was considerably smaller. Since the chamber medium was exchanged six times per min, it is obvious that the concentrations mechaniam paracrine factors released from beta cells and delta cells were much lower than those reached in the narrow intercellular space of islets when measuring secretion in batch incubations.
Pretreatment with PTX, which blocks the inhibitory effect of somatostatin [ 31 ], and exposure Glucafon 0. Only alpha cells confirmed by positive glucagon immunostaining were included in the analyses [ 15 ]. Batches of eight to 12 islets were pre-incubated for 30 min at 37°C in 1 ml of Krebs—Ringer buffer pH 7.
Aliquots of the medium were frozen pending the radioimmunoassays [ 3435 ]. When the glucose concentrations did not match exactly, test data were compared with interpolated control data.
The reaction patterns in individual alpha cells were considerably heterogeneous. Even alpha cells on the same releaase slip often reacted differently to the same experimental challenge.
Due to the qualitative differences in cellular responses, the results have been presented as proportions of cells reacting in different ways. All calculations were made by SigmaStat software Systat Software, Erkrath, Germany.
Glucose dependence of glucagon, insulin and somatostatin secretion from mouse pancreatic islets. Data are presented as means±SEM of six to eight experiments. Brackets indicate observations with identical significance levels. Numbers of cells are given in parentheses. Activation of K ATP channels with diazoxide hyperpolarises mouse alpha cells [ 15 ] and inhibits glucagon release from mouse islets, but does not prevent additional inhibition by glucose [ 5 ].
Data are presented as means±SEM of six experiments. Activation of the store-operated mechanism by blocking the SERCA pump with CPA stimulated glucagon secretion and prevented the inhibitory effect of glucose Fig.
In the absence of glucose, CPA had no effect on somatostatin secretion, but unexpectedly diminished glucose-stimulated release of the hormone Fig. Data are presented as means±SEM of ten experiments.
The data in Figs. Effects of the SERCA inhibitor CPA on glucagon, insulin and somatostatin secretion from mouse islets with closed K ATP channels. Secretion data in the presence of CPA from Fig. Data are presented as means±SEM of eight experiments.
Glucagon secretion is inhibited by lower glucose concentrations than those stimulating insulin release [ 41 ]. Our data indicated that maximal inhibition of glucagon secretion from mouse islets was obtained at the threshold for glucose stimulation of insulin release.
Based on the present data, we suggest that this inhibition is mediated by somatostatin. Further evidence for insulin- and somatostatin-independent effects on glucagon release was obtained with the observation that CPA inhibition of the SERCA pump stimulated glucagon secretion without affecting basal secretion of insulin or somatostatin.
Moreover, CPA prevented glucose inhibition of glucagon secretion. Apparently, paracrine interactions do not suffice to explain the observed alterations of glucagon secretion. Glucose inhibits glucagon secretion from clonal glucagon-releasing cells [ 51117 ], and studies of pancreatic islets and cells have provided additional evidence that glucose regulates glucagon release by a direct effect on the alpha cell [ 58 — 1012 — 17 ].
Paradoxically, the K ATP channel has also been proposed to mediate glucose inhibition of releaae secretion by depolarising the alpha cell [ 1316 ]. Relese evidence has been obtained with rat alpha cells, which have much higher K ATP channel density [ 43 ] than mouse alpha cells [ 1344 ].
Accordingly, tolbutamide stimulates the electrical activity [ 43 ] and exocytosis of glucagon [ 45 ] in isolated rat alpha cells, and releasw was recently found to stimulate glucagon release from purified rat alpha Glcuagon [ 46 ].
Interestingly, two studies of K ATP channel knockout mice support a stimulatory role of these channels in alpha cells. The most salient effect of knocking out the regulatory K ATP channel subunit sulfonylurea receptor 1 is low glucagon secretion with absent [ 47 ] or diminished [ 48 ] stimulation in response to lowering of glucose.
This model explains both adrenergic stimulation and glucose inhibition of glucagon release. Although rat and mouse are closely related species, glucagon secretion from pancreatic alpha cells may be differently regulated. In isolated rat alpha cells with high K ATP channel density [ 43 ] the direct effect of relase seems to be stimulation of secretion and the inhibitory action may require release of paracrine islet factors [ 46 ].
In isolated mouse alpha cells with low K ATP channel density [ 1344 ] the inhibitory effect of glucose dominated, although closure of the K ATP channels themselves was modestly stimulatory.
The data support the concept that glucose has a direct inhibitory effect on the alpha cell by suppressing a depolarising store-operated current. However, neither beta cell factors nor somatostatin mrchanism to mediate glucose inhibition of mechanis, secretion. Gerich JE, Charles A, Grodsky GM Regulation of pancreatic insulin and glucagon secretion.
Annu Rev Physiol — Article PubMed CAS Google Scholar. Buchanan KD, McCarroll AM Abnormalities of glucagon metabolism in untreated diabetes mellitus. Lancet — Article Google Scholar. Ohneda A, Watanabe K, Horigome K, Sakai T, Kai Y, Oikawa S Abnormal response of pancreatic glucagon to glycemic changes in diabetes mellitus.
J Clin Endocrinol Metab — PubMed CAS Google Scholar.
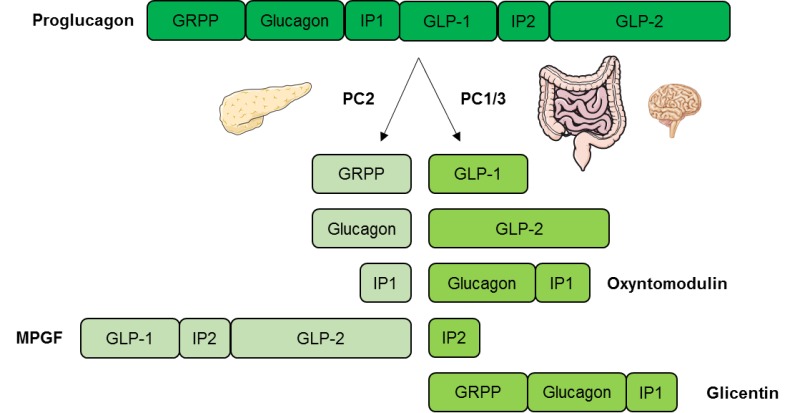
: Glucagon release mechanism| Endotext [Internet]. | However, overexpression of PDK4 in α-cells results in a rather mild phenotype. Article CAS PubMed Google Scholar Kaneko, K. However, responses to insulin-induced hypoglycemia have not been tested. Regulation of Glucagon Secretion by Glucose The most potent regulator of glucagon secretion is circulating glucose. In addition, the current observation that ATP is reduced may also be aligned with the proposed reduction in intracellular cAMP in α-cells MEDI, a GLP-1 and glucagon receptor dual agonist, in obese or overweight patients with type 2 diabetes: a randomised, controlled, double-blind, ascending dose and phase 2a study. Ashcroft FM ATP-sensitive potassium channelopathies: Focus on insulin secretion. |
| Paracrine control of α-cell glucagon exocytosis is compromised in human type-2 diabetes | For all experiments, the mice were randomly assigned to experimental groups to ensure an unbiased distribution of animals. No blinding was used. All animal procedures were performed at the University of Lausanne and were reviewed and approved by the Veterinary Office of Canton de Vaud. The numbers of animals studied per genotype are indicated within each experiment. To validate proper gene targeting, genomic DNA has been extracted from liver, hindbrain, ileum, and pancreatic islets using a Quick gDNA mini-prep kit Zymo Research, USA. RT-PCR analysis was performed using a Biometra T Thermocycler. Recombination efficiency was assessed in αGckKO-Rosa26tdtomato mice. Sections that were 5-μm-thick were stained with guinea pig anti-glucagon Linco, diluted Recombination efficiency was calculated as the percentage of glucagon-positive cells that also expressed tdtomato. α-cell mass and β-cell mass were then calculated based on individual pancreas weight. Insulin and glucagon content of the supernatant was then assessed by radioimmunoassay Merck Millipore , using insulin and glucagon standards, and expressed relative to initial pancreatic weight. Before removal of the pancreas, a solution of Liberase TL 0. Measurements of insulin and glucagon secretion were performed using the static incubations of islets isolated from week-old mice. Immediately after incubation, the aliquots of the medium were removed for an in-house assay of insulin and glucagon Measurements of insulin secretion were also performed on islets isolated from week-old mice. At the end of each static incubation, the islets were collected and lysed in acid ethanol to assess insulin and glucagon content. The islets were perfused with extracellular solution containing in mM : NaCl, 3. Glucose, methyl-succinate, and FCCP have been added as indicated in Fig. Images were acquired at a frequency of 0. Electrical activity, transmembrane currents, and cell capacitance were recorded from randomly chosen cells on the peripheral of the islets. α-cells were identified by the expression of fluorescent protein tdtomato see Mouse Validation. α-cells were identified by their electrical activity in response to glucose and lack of tdtomato fluorescence. Electrical activity and K ATP conductance were recorded using perforated patch-clamping technique. Perforating reagent gramicidin 0. Extracellular solution contains in mM : NaCl, 3. After the experiments, the membrane potential recordings were exported as ASCII files and converted to ABF files axon binary file using ABF utility software version 2. The resultant ABF files were then imported into Clampfit software version 9. Depolarization-triggered cell exocytosis was monitored as increase in membrane capacitance. The intracellular solution used for capacitance measurement contains in mM : Cs-glutamate, 10 CsCl, 10 NaCl, 1 MgCl 2 , 5 HEPES, 0. The extracellular solution contains in mM : NaCl, 5. Plasma glucagon levels were quantitated by radioimmunoassay Merck Millipore and by ELISA Mercodia. Plasma insulin levels were assessed by ultra-sensitive ELISA Mercodia. A portion of mouse liver were homogenized in ice-cold homogeneisation buffer in mM: sucrose, 10 HEPES pH 7. Proteins from nuclear fractions were extracted, and the protein content was determined by bicinchoninic acid assay Pierce, Thermo Scientific. Transfer to nitrocellulose membranes was performed using the Mini Trans-Blot apparatus from Bio-Rad. Bands corresponding to the specific proteins were visualized using enhanced chemiluminescence reagent Advansta. Digital images were acquired with Fusion FX7 system Vilber Lourmat and Bio-1D software Vilber Lourmat for quantification and normalization. The same membranes were reprobed with anti-β-actin antibodies to confirm the equal loading of proteins for each sample. Real-time PCR was performed using Power SYBR Green Master Mix Applied Biosystems. All reactions were normalized to β-actin levels. Specific mouse primers for each gene are listed in Supplementary Table 1. The animals were processed in the morning in the random-fed state. The mice received a bolus of 14 Cdeoxy-D-glucose Perkin-Elmer; dil. The mice were then placed in cages without water or food. After the last blood sampling, the mice were killed by cervical dislocation under isoflurane anesthesia. Tissues were immediately dissected and frozen for further assessment of 14 Cdeoxy-D-glucosephosphate 2-DGP content. The Plasma radioactivity was determined at each time point by liquid scintillation counting, in order to calculate the area under the curve of the plasma tracer decay. For the determination of tissue 2-DGP content, the tissue samples were homogenized, and the supernatants were passed through ion-exchange columns to separate 2-DGP from 2-DG. Tissue 2DG uptake was calculated by normalizing the tissue 2DG-6P content as disintegrations per minute to the tissue weight and to the AUC of the plasma tracer decay. All collected data were included without data exclusion. Statistical analysis was performed using GraphPad Prism 5. The data distribution was assumed to be normal. p -values less than 0. Other statistical methods were mentioned and indicated where they were used. No statistical methods were used to pre-determine sample sizes, but sample sizes are similar to those used in our previous studies. The data that support the findings of this study are available from the corresponding author upon reasonable request. Unger, R. Glucagon and the A cells. Physiology and Pathophysiology. Article CAS PubMed Google Scholar. Habegger, K. et al. The metabolic actions of glucagon revisited. Article CAS PubMed PubMed Central Google Scholar. Zhang, Q. Role of KATP channels in glucose-regulated glucagon secretion and impaired counterregulation in type 2 diabetes. Cell Metab. Thorens, B. Brain glucose sensing and neural regulation of insulin and glucagon secretion. Diabetes Obes. Marty, N. Brain glucose sensing, counterregulation, and energy homeostasis. Article CAS Google Scholar. Hevener, A. Novel glucosensor for hypoglycemic detection localized to the portal vein. Diabetes 46 , — Burcelin, R. Portal glucose infusion in the mouse induces hypoglycemia: evidence that the hepatoportal glucose sensor stimulates glucose utilization. Diabetes 49 , — Google Scholar. Lamy, C. Hypoglycemia-activated glut2 neurons of the nucleus tractus solitarius stimulate vagal activity and glucagon secretion. Steinbusch, L. Sex-specific control of fat mass and counterregulation by hypothalamic glucokinase. Diabetes 65 , — Gylfe, E. Upsala J. Article PubMed PubMed Central Google Scholar. Matschinsky, F. Pancreatic beta-cell glucokinase: closing the gap between theoretical concepts and experimental realities. Diabetes 47 , — Froguel, P. Close linkage of glucokinase locus on chromosoms 7p to early-onset non-insulin-dependent diabetes mellitus. Nature , — Article ADS CAS PubMed Google Scholar. Heimberg, H. The glucose sensor protein glucokinase is expressed in glucagon-producing alpha-cells. Natl Acad. USA 93 , — Article ADS CAS PubMed PubMed Central Google Scholar. Guenat, E. Counterregulatory responses to hypoglycemia in patients with glucokinase gene mutations. Diabetes Metab. CAS PubMed Google Scholar. Herrera, P. Adult insulin- and glucagon-producing cells differentiate from two independent cell lineages. Development , — Berg, J. A genetically encoded fluorescent reporter of ATP:ADP ratio. Methods 6 , — Briant, L. Glucagon secretion from pancreatic alpha-cells. Walker, J. Regulation of glucagon secretion by glucose: paracrine, intrinsic or both? Rorsman, P. ATP-regulated potassium channels and voltage-gated calcium channels in pancreatic alpha and beta cells: similar functions but reciprocal effects on secretion. Diabetologia 57 , — Meng, Z. Glucose Sensing by Skeletal Myocytes Couples Nutrient Signaling to Systemic Homeostasis. Cell 66 , — e Seyer, P. Hepatic glucose sensing is required to preserve beta cell glucose competence. Invest , — Lee, Y. Glucagon is the key factor in the development of diabetes. Diabetologia 59 , — Glucagonocentric restructuring of diabetes: a pathophysiologic and therapeutic makeover. Invest , 4—12 Mitrakou, A. Role of reduced suppression of glucose production and diminished early insulin release in impaired glucose tolerance. New Engl. Kawamori, D. Insulin signaling in alpha cells modulates glucagon secretion in vivo. Agius, L. Hormonal and metabolite regulation of hepatic glucokinase. Nakamura, A. Present status of clinical deployment of glucokinase activators. Diabetes Investig. Panagiotidis, G. Homologous islet amyloid polypeptide: effects on plasma levels of glucagon, insulin and glucose in the mouse. Diabetes Res. Download references. This work was supported by grants to B. from the Swiss National Science Foundation A0B and the European Research Council Advanced grants INSIGHT and INTEGRATE. was supported by a Diabetes UK RD Lawrence Fellowship. PR was supported by the Wellcome Trust and the Swedish Research Council. PLH was funded by Fondation privée of the University Hospitals of Geneva and the NIDDK grant DK We thank the Mouse Metabolic Evaluation Facility MEF from the Center for Integrative Genomics for performing tissue glucose uptake measurements. Center for Integrative Genomics, University of Lausanne, , Lausanne, Switzerland. Oxford Centre for Diabetes, Endocrinology, and Metabolism, University of Oxford, Churchill Hospital, Oxford, OX3 7LE, UK. Department of Clinical Science, UMAS, Division of Islet Cell Physiology, Lund, Sweden. Department of Genetic Medicine and Development, , Geneva, Switzerland. You can also search for this author in PubMed Google Scholar. secured funding. performed the experiments. provided the the Gcg-Cre mice. provided expertise and assisted with the editing of the manuscripts. Correspondence to Bernard Thorens. Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations. Open Access This article is licensed under a Creative Commons Attribution 4. Reprints and permissions. Basco, D. α-cell glucokinase suppresses glucose-regulated glucagon secretion. Nat Commun 9 , Download citation. Received : 12 May Accepted : 15 January Published : 07 February Anyone you share the following link with will be able to read this content:. Sorry, a shareable link is not currently available for this article. Provided by the Springer Nature SharedIt content-sharing initiative. Journal of Animal Science and Biotechnology By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate. Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily. Skip to main content Thank you for visiting nature. Among the GLP1 mimetics, exenatide is a synthetic polypeptide with high resistance to DPP4 cleavage that decreases glucagon levels in normal and diabetic subjects Degn et al. Liraglutide, another GLP1 derivative with long-lasting actions, can reduce glucagon release after a meal in patients with type 2 diabetes Juhl et al. Alternatively, DPP4 inhibitors like sitagliptin and vildagliptin increase the endogen effects of GLP1, reducing glucagon plasma concentrations in diabetic individuals Rosenstock et al. Since all these alternatives produce opposing actions on insulin and glucagon, they generate promising expectations for diabetes treatment. Given that imidazoline compounds stimulate insulin release while inhibiting glucagon secretion, these drugs are potentially valuable in diabetes. Because of the different expression of SSTR in the islet Kumar et al. It has been shown that SSTR2 is the subtype receptor predominantly expressed in rodent α-cells, and that SSTR2-deficient mice develop hyperglycaemia and non-fasting hyperglucagonaemia Singh et al. In mice, the use of a highly SSTR2-selective non-peptide agonist inhibited glucagon release without affecting insulin release Strowski et al. However, there is some overlapping in human islets between the different SSTR subtypes in α- and β-cells that limit, at present, the use of subtype-specific somatostatin analogues Singh et al. Amylin, which is cosecreted with insulin from β-cells, inhibits glucagon secretion stimulated by amino acids but does not affect hypoglycaemia-induced glucagon release Young Since α-cell response to amino acids is often exaggerated in diabetic patients, amylin or amylinomimetic compounds such as pramlintide are used as an effective alternative for the treatment of postprandial and amino acid-induced excess of glucagon secretion Dunning et al. Several linear and cyclic glucagon analogues have been developed to work as glucagon receptor antagonists. Essentially, they impair the ability of glucagon to stimulate adenylate cyclase activity in liver, thus reducing hepatic glucose output and improving plasma glucose levels. This is the case of [des-His 1 , des-Phe 6 , Glu 9 ] glucagon-NH 2 , which reduces glucose levels in streptozotocin-induced diabetic rats Van Tine et al. Recent investigations have demonstrated that the antagonist des-His-glucagon binds preferentially to the hepatic glucagon receptor in vivo , and this correlates with the glucose lowering effects Dallas-Yang et al. For instance, a novel competitive antagonist N -[3-cyano 1, 1-dimethylpropyl -4, 5, 6, 7-tetrahydrobenzothienyl]ethylbutanamide was recently shown to inhibit glucagon-mediated glycogenolysis in primary human hepatocytes and to block the increase in glucose levels after the administration of exogenous glucagon in mice Qureshi et al. The information about the effect of these antagonists on humans is, however, scarce. Despite the success of several approaches to modulate glucagon secretion or action and improve glucose control in animal models or in humans, more information is still required. Long-standing studies should address whether the utilization of these agents could lead to undesired hypoglycaemia in humans, accumulation of lipids or compensatory mechanisms that decrease the benefits of these therapies in the long term. In this aspect, the results obtained in animal models are positive: although the glucagon receptor knock-out mouse develops hyperglucagonaemia, it is not hypoglycaemic and does not have an abnormal accumulation of lipids Gelling et al. Additionally, recent long-term studies in mice further prove the viability of glucagon antagonism Winzell et al. Thus, present data are promising and indicate that several therapeutic agents targeted to glucagon signalling and α-cell secretion may be useful for the management of diabetes. Pancreatic α-cells and glucagon secretion are fundamental components of the regulatory mechanisms that control glucose homeostasis. However, α-cell physiology has remained elusive compared with the overwhelming information about insulin secretion and the β-cell. In recent years, however, several groups have initiated intensive efforts to understand α-cell physiology and identified essential pieces of its stimulus-secretion coupling. Additionally, important aspects of the regulation of α-cell metabolism and the control of glucagon expression are being elucidated. All of this information will favour an overall comprehension of the α-cell function and its role in glucose homeostasis. Nevertheless, more research is required to understand the α-cell behaviour, not only in healthy subjects but in pathological conditions as well. In conclusion, since the malfunction of the glucagon secretory response is involved in diabetes and its complications, a complete understanding of the α-cell will allow for a better design of therapeutic approaches for the treatment of this disease. The authors declare that there is no conflict of interest that could be perceived as prejudicing the impartiality of the research reported. This work was supported by grants from the Ministerio de Educación y Ciencia BFU and PCIA to I Q; BFU to A N. CIBERDEM is an initiative of the Instituto de Salud Carlos III. American Journal of Physiology. Renal Physiology F24 — F Ahren B Autonomic regulation of islet hormone secretion — implications for health and disease. Diabetologia 43 — Hormone and Metabolic Research 14 — Effects on basal release of insulin and glucagon. Endocrinology — Regulatory Peptides 55 — Biochemical Journal — Metabolism 24 35 — Metabolism 32 — Diabetes 56 — Regulatory, Integrative and Comparative Physiology R — R FEBS Letters — Diabetes 49 — Diabetes 36 — European Journal of Pharmacology 45 — Endocrine 6 79 — Journal of Clinical Endocrinology and Metabolism 54 — Pflugers Archiv: European Journal of Physiology — Metabolism 53 — Paradoxical suppression of glucose utilization and lack of compensatory increase in glucose production, roles of insulin resistance, abnormal neuroendocrine responses, and islet paracrine interactions. Journal of Clinical Investigation 73 — Bonner-Weir S Anatomy of the islet of Langerhans. In The Endocrine Pancreas , pp 15 — Eds Samols E. New York : Raven Press. Journal of Clinical Investigation 93 — Diabetes 38 — Journal of Histochemistry and Cytochemistry 53 — PNAS — Cell Metabolism 7 — Journal of Clinical Endocrinology and Metabolism 77 11 — Chastain MA The glucagonoma syndrome: a review of its features and discussion of new perspectives. American Journal of the Medical Sciences — European Journal of Biochemistry — Cryer PE Hypoglycaemia: the limiting factor in the glycaemic management of Type I and Type II diabetes. Diabetologia 45 — Cynober LA Plasma amino acid levels with a note on membrane transport: characteristics, regulation, and metabolic significance. Nutrition 18 — European Journal of Pharmacology — Diabetes 53 — Journal of Biological Chemistry — Diabetes 46 — Diabetologia 38 — Endocrine Reviews 28 — Diabetologia 48 — Endocrinology and Metabolism E40 — E Diabetes 54 — Regulatory Peptides — Journal of Physiology — Journal of Clinical Endocrinology and Metabolism 86 — Journal of General Physiology — Endocrine Reviews 28 84 — Pancreas 22 58 — Diabetes 52 — PNAS 93 — Nature — Metabolism 54 — FASEB Journal 9 — Nature Cell Biology 5 — Diabetes 51 — Diabetes Research and Clinical Practice 44 83 — Journal of Clinical Investigation 96 — Endocrinology and Metabolism E21 — E Diabetes 48 77 — Protein Science 4 — Journal of Clinical Endocrinology and Metabolism 84 — Diabetes Care 23 — Clinical Science — Cell Calcium 35 — Diabetologia 10 — Molecular Endocrinology 19 — PLoS Biology 5 e The glucagon receptor family. Pharmacological Reviews 55 — Nature Neuroscience 4 — Journal of Physiology 85 — Journal of Clinical Endocrinology and Metabolism 87 — Diabetologia 29 — Journal of Nutrition — European Journal of Pharmacology 65 — Diabetologia 44 — Diabetes 48 — Endocrinology and Metabolism E — E Biophysical Journal 90 — Diabetes 55 — Journal of Clinical Endocrinology and Metabolism 64 — Diabetes Care 30 — Diabetologia 32 — Glucose-regulated anaplerosis in beta cells. Potential role in nutrient sensing. American Journal of Physiology E — E Journal of Clinical Endocrinology and Metabolism 85 — Journal of Clinical Endocrinology and Metabolism 92 — Journal of Lipid Research 35 — Journal of Clinical Investigation — Diabetes 50 — Lancet 1 14 — Diabetologia 50 — Hepatology 13 — Journal of Cell Biology — Nature 68 — Endocrinology and Metabolism E19 — E Cell Metabolism 3 47 — Biochemical and Biophysical Research Communications — Young A Inhibition of glucagon secretion. Advances in Pharmacology 52 — Diabetes 45 — Journal of Endocrinology is committed to supporting researchers in demonstrating the impact of their articles published in the journal. The two types of article metrics we measure are i more traditional full-text views and pdf downloads, and ii Altmetric data, which shows the wider impact of articles in a range of non-traditional sources, such as social media. Sign in Create account. Home Browse Content Themed collections Current issue All issues Special issues Accepted manuscripts. Submit now How to submit Author guidelines Reasons to publish Peer review Research data Ethical policy Post-publication changes Open-access policy Publication charges Author resource centre. Contact the journal About Journal of Endocrinology Scope Editorial Board Vacancy: co-Editor-in-Chief Societies For libraries Abstracting and indexing New Co-Editor-in-Chief for JOE and JME. Advanced Search Help. Physiology of the pancreatic α-cell and glucagon secretion: role in glucose homeostasis and diabetes in Journal of Endocrinology. Page Range: 5—19 Online Publication Date: Oct Copyright: © Society for Endocrinology Free access. Download PDF. Check for updates. Abstract The secretion of glucagon by pancreatic α-cells plays a critical role in the regulation of glycaemia. Introduction The principal level of control on glycaemia by the islet of Langerhans depends largely on the coordinated secretion of glucagon and insulin by α- and β-cells respectively. Islet of Langerhans: cell architecture and function Glucagon-secreting α-cells are one of the main endocrine cell populations that coexist in the islet of Langerhans along with insulin-secreting β-cells. Figure 1 Schematic model for glucose-dependent regulation of glucagon secretion in the mouse α-cell. Regulation of α-cell function by glucose: direct or paracrine effect? Regulation of glucagon secretion by fatty acids and amino acids Although the lipotoxicity theory and its role in obesity-induced diabetes have increased the interest in the interactions between fatty acids and islet functions, little is known about their effect on the regulation of the α-cell compared with those on β-cells. Autocrine, paracrine, endocrine and neural regulation of glucagon secretion Autocrine, paracrine and endocrine signalling The spatial distribution of α-cells and the vascular organization within the islet sustain an important intercellular communication through autocrine and paracrine mechanisms Fig. Figure 3 Paracrine signalling in the α-cell. Insulin and zinc One of the most important paracrine mechanisms responsible for inhibiting glucagon release is conducted by insulin, acting via several pathways. Somatostatin and glucagon Somatostatin is produced and secreted by several tissues in addition to the δ-cell population of the islet and works as an inhibitor of both glucagon and insulin release Fehmann et al. GLP1 The incretin hormone glucagon-like peptide 1 GLP1 is released from the L-cells of the small intestine after food intake, stimulating insulin production and inhibiting glucagon release. Other extracellular messengers The neurotransmitter γ-aminobutyric acid GABA is another α-cell modulator. Neural regulation As previously stated, the islet of Langerhans is highly innervated by parasympathetic and sympathetic nerves that ensure a rapid response to hypoglycaemia and protection from potential brain damage Ahren Glucagon physiological and pathophysiological actions and its role in diabetes Glucagon synthesis The preproglucagon-derived peptides glucagon, GLP1 and GLP2, are encoded by the preproglucagon gene, which is expressed in the central nervous system, intestinal L-cells and pancreatic α-cells. Glucagon receptor The rat and mouse glucagon receptor is a amino acid protein, belonging to the secretin—glucagon receptor II class family of G protein-coupled receptors Mayo et al. Figure 4 The role of glucagon and the glucagon receptor in the liver. Glucagon control of glucose homeostasis and metabolism Several lines of defence protect the organism against hypoglycaemia and its potential damaging effects, especially in the brain, which depends on a continuous supply of glucose, its principal metabolic fuel. Modulation of glucagon secretion Sulphonylureas Sulphonylureas are efficient K ATP channel blockers that have been extensively used for the clinical treatment of diabetes. GLP1 mimetics and DPP4 inhibitors In addition to stimulating insulin release, GLP1 can suppress glucagon secretion in humans, perfused rat pancreas and isolated rat islets in a glucose-dependent manner Guenifi et al. Somatostatin analogues Because of the different expression of SSTR in the islet Kumar et al. Amylin and pramlintide Amylin, which is cosecreted with insulin from β-cells, inhibits glucagon secretion stimulated by amino acids but does not affect hypoglycaemia-induced glucagon release Young Modulation of glucagon action and glucagon receptor signalling Peptide-based glucagon receptor antagonists Several linear and cyclic glucagon analogues have been developed to work as glucagon receptor antagonists. Conclusions Pancreatic α-cells and glucagon secretion are fundamental components of the regulatory mechanisms that control glucose homeostasis. Declaration of interest The authors declare that there is no conflict of interest that could be perceived as prejudicing the impartiality of the research reported. Funding This work was supported by grants from the Ministerio de Educación y Ciencia BFU and PCIA to I Q; BFU to A N. PubMed Ahloulay M Bouby N Machet F Kubrusly M Coutaud C Bankir L Effects of glucagon on glomerular filtration rate and urea and water excretion. PubMed Ahren B Autonomic regulation of islet hormone secretion — implications for health and disease. PubMed Ahren B Lundquist I Influences of gastro-intestinal polypeptides and glucose on glucagon secretion induced by cholinergic stimulation. PubMed Ahren B Veith RC Taborsky GJ Jr Sympathetic nerve stimulation versus pancreatic norepinephrine infusion in the dog: 1. PubMed Akesson B Panagiotidis G Westermark P Lundquist I Islet amyloid polypeptide inhibits glucagon release and exerts a dual action on insulin release from isolated islets. PubMed Andersen B Rassov A Westergaard N Lundgren K Inhibition of glycogenolysis in primary rat hepatocytes by 1, 4-dideoxy-1,4-imino- d -arabinitol. PubMed Andrews SS Lopez-S A Blackard WG Effect of lipids on glucagon secretion in man. PubMed Asplin C Raghu P Dornan T Palmer JP Glucose regulation of glucagon secretion independent of B cell activity. PubMed Bailey SJ Ravier MA Rutter GA Glucose-dependent regulation of gamma-aminobutyric acid GABA A receptor expression in mouse pancreatic islet alpha-cells. PubMed Balkan B Li X Portal GLP-1 administration in rats augments the insulin response to glucose via neuronal mechanisms. PubMed Band GC Jones CT Functional activation by glucagon of glucose 6-phosphatase and gluconeogenesis in the perfused liver of the fetal guinea pig. PubMed Barg S Galvanovskis J Gopel SO Rorsman P Eliasson L Tight coupling between electrical activity and exocytosis in mouse glucagon-secreting alpha-cells. PubMed Baron AD Schaeffer L Shragg P Kolterman OG Role of hyperglucagonemia in maintenance of increased rates of hepatic glucose output in type II diabetics. PubMed Bertrand G Gross R Puech R Loubatieres-Mariani MM Bockaert J Glutamate stimulates glucagon secretion via an excitatory amino acid receptor of the AMPA subtype in rat pancreas. PubMed Bohannon NV Lorenzi M Grodsky GM Karam JH Stimulatory effects of tolbutamide infusion on plasma glucagon in insulin-dependent diabetic subjects. PubMed Bollheimer LC Landauer HC Troll S Schweimer J Wrede CE Scholmerich J Buettner R Stimulatory short-term effects of free fatty acids on glucagon secretion at low to normal glucose concentrations. PubMed Bolli GB Tsalikian E Haymond MW Cryer PE Gerich JE Defective glucose counterregulation after subcutaneous insulin in noninsulin-dependent diabetes mellitus. PubMed Bonner-Weir S Anatomy of the islet of Langerhans. In The Endocrine Pancreas, pp 15 — PubMed Borg WP During MJ Sherwin RS Borg MA Brines ML Shulman GI Ventromedial hypothalamic lesions in rats suppress counterregulatory responses to hypoglycemia. PubMed Brelje TC Scharp DW Sorenson RL Three-dimensional imaging of intact isolated islets of Langerhans with confocal microscopy. PubMed Brissova M Fowler MJ Nicholson WE Chu A Hirshberg B Harlan DM Powers AC Assessment of human pancreatic islet architecture and composition by laser scanning confocal microscopy. PubMed Cabrera O Berman DM Kenyon NS Ricordi C Berggren PO Caicedo A The unique cytoarchitecture of human pancreatic islets has implications for islet cell function. PubMed Cabrera O Jacques-Silva MC Speier S Yang SN Köhler M Fachado A Vieira E Zierath JR Kibbey R Berman DM Glutamate is a positive autocrine signal for glucagon release. PubMed Carlson MG Snead WL Campbell PJ Regulation of free fatty acid metabolism by glucagon. PubMed Chastain MA The glucagonoma syndrome: a review of its features and discussion of new perspectives. PubMed Ciudad C Camici M Ahmad Z Wang Y DePaoli-Roach AA Roach PJ Control of glycogen synthase phosphorylation in isolated rat hepatocytes by epinephrine, vasopressin and glucagon. PubMed Consoli A Nurjhan N Capani F Gerich J Predominant role of gluconeogenesis in increased hepatic glucose production in NIDDM. PubMed Cryer PE Hypoglycaemia: the limiting factor in the glycaemic management of Type I and Type II diabetes. PubMed Cynober LA Plasma amino acid levels with a note on membrane transport: characteristics, regulation, and metabolic significance. PubMed Dallas-Yang Q Shen X Strowski M Brady E Saperstein R Gibson RE Szalkowski D Qureshi SA Candelore MR Fenyk-Melody JE Hepatic glucagon receptor binding and glucose-lowering in vivo by peptidyl and non-peptidyl glucagon receptor antagonists. PubMed Degn KB Brock B Juhl CB Djurhuus CB Grubert J Kim D Han J Taylor K Fineman M Schmitz O Effect of intravenous infusion of exenatide synthetic exendin-4 on glucose-dependent insulin secretion and counterregulation during hypoglycemia. PubMed Detimary P Dejonghe S Ling Z Pipeleers D Schuit F Henquin JC The changes in adenine nucleotides measured in glucose-stimulated rodent islets occur in beta cells but not in alpha cells and are also observed in human islets. PubMed Dey A Lipkind GM Rouille Y Norrbom C Stein J Zhang C Carroll R Steiner DF Significance of prohormone convertase 2, PC2, mediated initial cleavage at the proglucagon interdomain site, LysArg71, to generate glucagon. PubMed Diao J Asghar Z Chan CB Wheeler MB Glucose-regulated glucagon secretion requires insulin receptor expression in pancreatic α-cells. PubMed Dinneen S Alzaid A Turk D Rizza R Failure of glucagon suppression contributes to postprandial hyperglycaemia in IDDM. PubMed Dumonteil E Magnan C Ritz-Laser B Meda P Dussoix P Gilbert M Ktorza A Philippe J Insulin, but not glucose lowering corrects the hyperglucagonemia and increased proglucagon messenger ribonucleic acid levels observed in insulinopenic diabetes. PubMed Dumonteil E Ritz-Laser B Magnan C Grigorescu I Ktorza A Philippe J Chronic exposure to high glucose concentrations increases proglucagon messenger ribonucleic acid levels and glucagon release from InR1G9 cells. PubMed Dumonteil E Magnan C Ritz-Laser B Ktorza A Meda P Philippe J Glucose regulates proinsulin and prosomatostatin but not proglucagon messenger ribonucleic acid levels in rat pancreatic islets. PubMed Dunning BE Gerich JE The role of alpha-cell dysregulation in fasting and postprandial hyperglycemia in type 2 diabetes and therapeutic implications. PubMed Dunning BE Foley JE Ahrén B Alpha cell function in health and disease: influence of glucagon-like peptide PubMed Eledrisi MS Alshanti MS Shah MF Brolosy B Jaha N Overview of the diagnosis and management of diabetic ketoacidosis. PubMed Fehmann HC Strowski M Goke B Functional characterization of somatostatin receptors expressed on hamster glucagonoma cells. PubMed Franklin I Gromada J Gjinovci A Theander S Wollheim CB β-cell secretory products activate α-cell ATP-dependent potassium channels to inhibit glucagon release. PubMed Furuta M Zhou A Webb G Carroll R Ravazzola M Orci L Steiner DF Severe defect in proglucagon processing in islet A-cells of prohormone convertase 2 null mice. PubMed Gastaldelli A Baldi S Pettiti M Toschi E Camastra S Natali A Landau BR Ferrannini E Influence of obesity and type 2 diabetes on gluconeogenesis and glucose output in humans: a quantitative study. PubMed Gedulin BR Jodka CM Herrmann K Young AA Role of endogenous amylin in glucagon secretion and gastric emptying in rats demonstrated with the selective antagonist, AC PubMed Gelling RW Du XQ Dichmann DS Romer J Huang H Cui L Obici S Tang B Holst JJ Fledelius C Lower blood glucose, hyperglucagonemia, and pancreatic alpha cell hyperplasia in glucagon receptor knockout mice. PubMed Gopel S Kanno T Barg S Galvanovskis J Rorsman P Voltage-gated and resting membrane currents recorded from β-cells in intact mouse pancreatic islets. PubMed Gopel SO Kanno T Barg S Rorsman P Patch-clamp characterisation of somatostatin-secreting delta-cells in intact mouse pancreatic islets. PubMed Gorus FK Malaisse WJ Pipeleers DG Differences in glucose handling by pancreatic A- and B-cells. PubMed Grapengiesser E Salehi A Qader SS Hellman B Glucose induces glucagon release pulses antisynchronous with insulin and sensitive to purinoceptor inhibition. PubMed Gravholt CH Moller N Jensen MD Christiansen JS Schmitz O Physiological levels of glucagon do not influence lipolysis in abdominal adipose tissue as assessed by microdialysis. PubMed Gremlich S Bonny C Waeber G Thorens B Fatty acids decrease IDX-1 expression in rat pancreatic islets and reduce GLUT2, glucokinase, insulin, and somatostatin levels. PubMed Gromada J Hoy M Buschard K Salehi A Rorsman P Somatostatin inhibits exocytosis in rat pancreatic α-cells by Gi2-dependent activation of calcineurin and depriming of secretory granules. PubMed Gromada J Franklin I Wollheim CB Alpha-cells of the endocrine pancreas: 35 years of research but the enigma remains. PubMed Guenifi A Ahren B Abdel-Halim SM Differential effects of glucagon-like peptide-1 7—36 amide versus cholecystokinin on arginine-induced islet hormone release in vivo and in vitro. PubMed Hayashi M Otsuka M Morimoto R Muroyama A Uehara S Yamamoto A Moriyama Y a Vesicular inhibitory amino acid transporter is present in glucagon-containing secretory granules in alphaTC6 cells, mouse clonal alpha-cells, and alpha-cells of islets of Langerhans. PubMed Hayashi M Yamada H Uehara S Morimoto R Muroyama A Yatsushiro S Takeda J Yamamoto A Moriyama Y b Secretory granule-mediated co-secretion of l -glutamate and glucagon triggers glutamatergic signal transmission in islets of Langerhans. PubMed Heimberg H De Vos A Pipeleers D Thorens B Schuit F Differences in glucose transporter gene expression between rat pancreatic alpha- and beta-cells are correlated to differences in glucose transport but not in glucose utilization. PubMed Heimberg H De Vos A Moens K Quartier E Bouwens L Pipeleers D Van Schaftingen E Madsen O Schuit F The glucose sensor protein glucokinase is expressed in glucagon-producing alpha α-cells. PubMed Herzig S Long F Jhala US Hedrick S Quinn R Bauer A Rudolph D Schutz G Yoon C Puigserver P CREB regulates hepatic gluconeogenesis through the coactivator PGC PubMed Hjorth SA Adelhorst K Pedersen BB Kirk O Schwartz TW Glucagon and glucagon-like peptide 1: selective receptor recognition via distinct peptide epitopes. PubMed Hong J Abudula R Chen J Jeppesen PB Dyrskog SEU Xiao J Colombo M Hermansen K The short-term effect of fatty acids on glucagon secretion is influenced by their chain length, spatial configuration, and degree of unsaturation: studies in vitro. PubMed Hong J Jeppesen PB Nordentoft I Hermansen K Fatty acid-induced effect on glucagon secretion is mediated via fatty acid oxidation. PubMed Hoy M Bokvist K Xiao-Gang W Hansen J Juhl K Berggren PO Buschard K Gromada J Phentolamine inhibits exocytosis of glucagon by Gi2 protein-dependent activation of calcineurin in rat pancreatic alpha-cells. PubMed Hunyady B Hipkin RW Schonbrunn A Mezey E Immunohistochemical localization of somatostatin receptor SST2A in the rat pancreas. PubMed Inagaki N Kuromi H Gonoi T Okamoto Y Ishida H Seino Y Kaneko T Iwanaga T Seino S Expression and role of ionotropic glutamate receptors in pancreatic islet cells. PubMed Ishihara H Maechler P Gjinovci A Herrera PL Wollheim CB Islet beta-cell secretion determines glucagon release from neighbouring alpha-cells. PubMed Juhl CB Hollingdal M Sturis J Jakobsen G Agerso H Veldhuis J Porksen N Schmitz O Bedtime administration of NN, a long-acting GLP-1 derivative, substantially reduces fasting and postprandial glycemia in type 2 diabetes. PubMed Kaneko K Shirotani T Araki E Matsumoto K Taguchi T Motoshima H Yoshizato K Kishikawa H Shichiri M Insulin inhibits glucagon secretion by the activation of PI3-kinase in In-R1-G9 cells. PubMed Kendall DM Poitout V Olson LK Sorenson RL Robertson RP Somatostatin coordinately regulates glucagon gene expression and exocytosis in HIT-T15 cells. PubMed Kuhara T Ikeda S Ohneda A Sasaki Y Effects of intravenous infusion of 17 amino acids on the secretion of GH, glucagon, and insulin in sheep. PubMed Kumar U Sasi R Suresh S Patel A Thangaraju M Metrakos P Patel SC Patel YC Subtype-selective expression of the five somatostatin receptors hSSTR in human pancreatic islet cells: a quantitative double-label immunohistochemical analysis. PubMed Landstedt-Hallin L Adamson U Lins PE Oral glibenclamide suppresses glucagon secretion during insulin-induced hypoglycemia in patients with type 2 diabetes. PubMed Larsson H Ahren B Islet dysfunction in insulin resistance involves impaired insulin secretion and increased glucagon secretion in postmenopausal women with impaired glucose tolerance. PubMed Leclercq-Meyer V Marchand J Woussen-Colle MC Giroix MH Malaisse WJ Multiple effects of leucine on glucagon, insulin, and somatostatin secretion from the perfused rat pancreas. PubMed Leung YM Ahmed I Sheu L Tsushima RG Diamant NE Hara M Gaisano HY Electrophysiological characterization of pancreatic islet cells in the mouse insulin promoter-green fluorescent protein mouse. PubMed Li Y Cao X Li LX Brubaker PL Edlund H Drucker DJ Beta-cell Pdx1 expression is essential for the glucoregulatory, proliferative, and cytoprotective actions of glucagon-like peptide PubMed Li XC Liao TD Zhuo JL Long-term hyperglucagonaemia induces early metabolic and renal phenotypes of Type 2 diabetes in mice. PubMed Liu YJ Vieira E Gylfe E A store-operated mechanism determines the activity of the electrically excitable glucagon-secreting pancreatic alpha-cell. PubMed Loubatieres AL Loubatieres-Mariani MM Alric R Ribes G Tolbutamide and glucagon secretion. PubMed Ma X Zhang Y Gromada J Sewing S Berggren PO Buschard K Salehi A Vikman J Rorsman P Eliasson L Glucagon stimulates exocytosis in mouse and rat pancreatic alpha-cells by binding to glucagon receptors. PubMed MacDonald PE De Marinis YZ Ramracheya R Salehi A Ma X Johnson PR Cox R Eliasson L Rorsman P A K ATP channel-dependent pathway within alpha cells regulates glucagon release from both rodent and human islets of Langerhans. PubMed Manning Fox JE Gyulkhandanyan AV Satin LS Wheeler MB Oscillatory membrane potential response to glucose in islet beta-cells: a comparison of islet-cell electrical activity in mouse and rat. PubMed Mayo KE Miller LJ Bataille D Dalle S Goke B Thorens B Drucker DJ International Union of Pharmacology. PubMed McGirr R Ejbick CE Carter DE Andrews JD Nie Y Friedman TC Dhanvantari S Glucose dependence of the regulated secretory pathway in alphaTC cells. PubMed Mojsov S Heinrich G Wilson IB Ravazzola M Orci L Habener JF Preproglucagon gene expression in pancreas and intestine diversifies at the level of post-translational processing. PubMed Munoz A Hu M Hussain K Bryan J Aguilar-Bryan L Rajan AS Regulation of glucagon secretion at low glucose concentrations: evidence for adenosine triphosphate-sensitive potassium channel involvement. PubMed Nadal A Quesada I Soria B Homologous and heterologous asynchronicity between identified alpha-, beta- and delta-cells within intact islets of Langerhans in the mouse. PubMed Nauck MA Heimesaat MM Behle K Holst JJ Nauck MS Ritzel R Hufner M Schmiegel WH Effects of glucagon-like peptide 1 on counterregulatory hormone responses, cognitive functions, and insulin secretion during hyperinsulinemic, stepped hypoglycemic clamp experiments in healthy volunteers. PubMed Olofsson CS Salehi A Gopel SO Holm C Rorsman P Palmitate stimulation of glucagon secretion in mouse pancreatic alpha-cells results from activation of L-type calcium channels and elevation of cytoplasmic calcium. PubMed Olsen HL Theander S Bokvist K Buschard K Wollheim CB Gromada J Glucose stimulates glucagon release in single rat alpha-cells by mechanisms that mirror the stimulus-secretion coupling in beta-cells. PubMed Ostenson CG Nylen A Grill V Gutniak M Efendic S Sulfonylurea-induced inhibition of glucagon secretion from the perfused rat pancreas: evidence for a direct, non-paracrine effect. PubMed Paty BW Ryan EA Shapiro AM Lakey JR Robertson RP Intrahepatic islet transplantation in type 1 diabetic patients does not restore hypoglycemic hormonal counterregulation or symptom recognition after insulin independence. PubMed Paul GL Waegner A Gaskins HR Shay NF Histidine availability alters glucagon gene expression in murine alphaTC6 cells. |
| α-cell glucokinase suppresses glucose-regulated glucagon secretion | Nature Communications | A third predicts that glucose sensing occurs in the hypothalamus with altered neural signalling to alpha cells [ 28 ]. Physiology and Pathophysiology. European Journal of Clinical Investigation. Therefore, these experimental results are a further support that glucagon antagonism may be beneficial for diabetes treatment. Contents www. |
| Glucose controls glucagon secretion by directly modulating cAMP in alpha cells | Contact the journal About Journal of Endocrinology Scope Editorial Board Vacancy: co-Editor-in-Chief Societies For libraries Abstracting and indexing New Co-Editor-in-Chief for JOE and JME. Toggle limited content width. mTOR regulates mineralocorticoid receptor transcriptional activity by ULK1- dependent and independent mechanisms. Somatostatin inhibits exocytosis in rat pancreatic alpha-cells by G i2 -dependent activation of calcineurin and depriming of secretory granules. PubMed Guenifi A Ahren B Abdel-Halim SM Differential effects of glucagon-like peptide-1 7—36 amide versus cholecystokinin on arginine-induced islet hormone release in vivo and in vitro. Olsen, H. |
| Frontiers | Glucagon secretion and signaling in the development of diabetes | PubMed Franklin I Gromada J Gjinovci A Theander S Wollheim CB β-cell secretory products activate α-cell ATP-dependent potassium channels to inhibit glucagon release. However, glucagon is also involved in hepatic lipid and amino acid metabolism and may increase resting energy expenditure. In rodents, the alpha cells are located in the outer rim of the islet. This process is reversible in the absence of glucagon and thus, the presence of insulin. Also, the purinergic messenger ATP is highly accumulated in β-cell secretory granules and in nerve terminals. PubMed Dumonteil E Magnan C Ritz-Laser B Ktorza A Meda P Philippe J Glucose regulates proinsulin and prosomatostatin but not proglucagon messenger ribonucleic acid levels in rat pancreatic islets. |
Glucagon release mechanism -
Whether other trafficking proteins are affected, and how alpha cell function is affected in diabetes in these mice, is not yet known. So what are the implications of glucagon trafficking through the lysosomal pathway in diabetes?
Lysosomal trafficking and autophagy in the beta cell may be a possible mechanism of insulin secretory defects in diabetes, with a recent study providing evidence for impairment of lysosomal function in human T1D How does lysosomal function contribute to defects in alpha cell function?
It is tempting to hypothesize that impairments in lysosomal biogenesis and trafficking result in both reduced insulin secretion in the beta cell and unregulated glucagon secretion from the alpha cell. Further investigation into the altered dynamics of glucagon trafficking in the alpha cell in diabetes may reveal key roles for the lysosome in the regulation of glucagon secretion, thus identifying a potential new target for the treatment of hyperglucagonemia.
Finally, some excellent single-cell transcriptomics and epigenomics databases are being generated that reveal the dynamics of intracellular trafficking networks at the transcriptional level in human pancreatic alpha cells in both health and diabetes — The mapping of T2D-associated genetic variants with RNA-seq of human islets may reveal risk factors associated with defects in alpha cell function A novel immunocompromised mouse model in which glucagon-encoding codons were deleted while preserving both GLP-1 and GLP-2 will provide an innovative and much-needed resource for the study of the regulation of glucagon secretion from human islets in vivo In this study, transplantation of islets from people with T2D resulted in hyperglucagonemia with apparent alpha cell insulin resistance, revealing intrinsic alpha cell defects in T2D.
Moreover, defects in alpha cell function were more apparent than in isolated islets, thus emphasizing the utility of such an in vivo system to investigate the molecular mechanisms of glucagon secretion in human islets, and the testing of possible treatments for hyperglucagonemia.
While the development of glucagon receptor antagonists and other inhibitors of glucagon action has provided some possibilities for the treatment of hyperglucagonemia, there are significant side effects that result from impaired hepatic metabolism and potentially uncontrolled alpha cell proliferation.
The advantage to developing such drugs, however, lie in the fact that the glucagon receptor is an easily available target. In contrast, targeting glucagon secretion as a means to treat hyperglucagonemia may alleviate concerns about effects on the liver and alpha cell mass; however, there are potentially many more targets within the alpha cell secretory pathway, and many of those may not be easily accessible for drug treatment.
The ongoing discovery of novel proteins and networks that regulate the secretion of glucagon will shed further light on alpha cell biology in health and disease while also searching for improved means to control hyperglucagonemia and hyperglycemia of diabetes.
SD and FA co-wrote the manuscript. All authors contributed to the article and approved the submitted version. This work was funded by a Natural Sciences and Engineering Research Council Discovery Grant to SD.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest. All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers.
Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher. Stanley S, Moheet A, Seaquist ER.
Central Mechanisms of Glucose Sensing and Counterregulation in Defense of Hypoglycemia. Endocr Rev — doi: PubMed Abstract CrossRef Full Text Google Scholar. DCCT Research Group. Hypoglycemia in the Diabetes Control and Complications Trial. Diabetes — Unger R, Orci L. The Essential Role of Glucagon in the Pathogenesis of Diabetes Mellitus.
Lancet —6. Unger RH, Cherrington AD. Glucagonocentric Restructuring of Diabetes: A Pathophysiologic and Therapeutic Makeover. J Clin Invest — Lee Y, Wang M-Y, Du XQ, Charron MJ, Unger RH.
Glucagon Receptor Knockout Prevents Insulin-Deficient Type 1 Diabetes in Mice. Diabetes —7. Conarello SL, Jiang G, Mu J, Li Z, Woods J, Zycband E, et al. Glucagon Receptor Knockout Mice are Resistant to Diet-Induced Obesity and Streptozotocin-Mediated Beta Cell Loss and Hyperglycaemia.
Diabetologia — Neumann UH, Ho JSS, Mojibian M, Covey SD, Charron MJ, Kieffer TJ. Glucagon Receptor Gene Deletion in Insulin Knockout Mice Modestly Reduces Blood Glucose and Ketones But Does Not Promote Survival.
Mol Metab —6. Damond N, Thorel F, Moyers JS, Charron MJ, Vuguin PM, Powers AC, et al. Blockade of Glucagon Signaling Prevents or Reverses Diabetes Onset Only If Residual β-Cells Persist. Elife — CrossRef Full Text Google Scholar. Kazda CM, Ding Y, Kelly RP, Garhyan P, Shi C, Lim CN, et al.
Evaluation of Efficacy and Safety of the Glucagon Receptor Antagonist LY in Patients With Type 2 Diabetes: and Week Phase 2 Studies. Diabetes Care —9. Yang B, Gelfanov VM, Perez-Tilve D, DuBois B, Rohlfs R, Levy J, et al. Optimization of Truncated Glucagon Peptides to Achieve Selective, High Potency, Full Antagonists.
J Med Chem — Lee CY, Choi H, Park EY, Nguyen TTL, Maeng HJ, Mee Lee K, et al. Synthesis and Anti-Diabetic Activity of Novel Biphenylsulfonamides as Glucagon Receptor Antagonists.
Chem Biol Drug Des — Okamoto H, Cavino K, Na E, Krumm E, Kim SY, Cheng X, et al. Glucagon Receptor Inhibition Normalizes Blood Glucose in Severe Insulin-Resistant Mice. Proc Natl Acad Sci —8. Liang Y, Osborne MC, Monia BP, Bhanot S, Gaarde WA, Reed C, et al.
Kim J, Okamoto H, Huang ZJ, Anguiano G, Chen S, Liu Q, et al. Amino Acid Transporter Slc38a5 Controls Glucagon Receptor Inhibition-Induced Pancreatic α Cell Hyperplasia in Mice. Cell Metab — Wei R, Gu L, Yang J, Yang K, Liu J, Le Y, et al. Antagonistic Glucagon Receptor Antibody Promotes α-Cell Proliferation and Increases β-Cell Mass in Diabetic Mice.
iScience — Galsgaard KD, Winther-Sørensen M, Ørskov C, Kissow H, Poulsen SS, Vilstrup H, et al. Disruption of Glucagon Receptor Signaling Causes Hyperaminoacidemia Exposing a Possible Liver-Alpha-Cell Axis. Am J Physiol Metab E93—E Wewer Albrechtsen NJ, Pedersen J, Galsgaard KD, Winther-Sørensen M, Suppli MP, Janah L, et al.
The Liver—α-Cell Axis and Type 2 Diabetes. Guan H-P, Yang X, Lu K, Wang S-P, Castro-Perez JM, Previs S, et al. Glucagon Receptor Antagonism Induces Increased Cholesterol Absorption. J Lipid Res — Tooze S.
Biogenesis of Secretory Granules in the Trans-Golgi Network of Neuroendocrine and Endocrine Cells. Biochim Biophys Acta — Cool DR, Fenger M, Snell CR, Loh YP. Identification of the Sorting Signal Motif Within Pro-Opiomelanocortin for the Regulated Secretory Pathway.
J Biol Chem —9. Dhanvantari S, Shen F, Adams T, Snell CR, Zhang C, Mackin RB, et al. Disruption of a Receptor-Mediated Mechanism for Intracellular Sorting of Proinsulin in Familial Hyperproinsulinemia. Mol Endocrinol — Zhang C-F, Dhanvantari S, Lou H, Loh YP.
Sorting of Carboxypeptidase E to the Regulated Secretory Pathway Requires Interaction of its Transmembrane Domain With Lipid Rafts. Biochem J — Dikeakos JD, Mercure C, Lacombe M-J, Seidah NG, Reudelhuber TL. FEBS J — Dikeakos JD, Di Lello P, Lacombe M-J, Ghirlando R, Legault P, Reudelhuber TL, et al.
Proc Natl Acad Sci USA — Dhanvantari S, Loh YP. Lipid Raft Association of Carboxypeptidase E Is Necessary for Its Function as a Regulated Secretory Pathway Sorting Receptor.
J Biol Chem — Cool DR, Normant E, Shen F, Chen H, Pannell L, Zhang Y, et al. Carboxypeptidase E Is a Regulated Secretory Pathway Sorting Receptor: Genetic Obliteration Leads to Endocrine Disorders in Cpe Fat Mice.
Cell — Irminger JC, Verchere CB, Meyer K, Halban PA. J Biol Chem —4. McGirr R, Guizzetti L, Dhanvantari S. The Sorting of Proglucagon to Secretory Granules is Mediated by Carboxypeptidase E and Intrinsic Sorting Signals.
J Endocrinol — Hosaka M, Watanabe T, Sakai Y, Kato T, Takeuchi T. Interaction Between Secretogranin III and Carboxypeptidase E Facilitates Prohormone Sorting Within Secretory Granules.
J Cell Sci — Plá V, Paco S, Ghezali G, Ciria V, Pozas E, Ferrer I, et al. Brain Pathol — Arvan P, Halban PA. Sorting Ourselves Out: Seeking Consensus on Trafficking in the Beta-Cell. Traffic — Guizzetti L, McGirr R, Dhanvantari S. Two Dipolar α-Helices Within Hormone-Encoding Regions of Proglucagon are Sorting Signals to the Regulated Secretory Pathway.
Dey A, Lipkind GM, Rouillé Y, Norrbom C, Stein J, Zhang C, et al. Significance of Prohormone Convertase 2, PC2, Mediated Initial Cleavage at the Proglucagon Interdomain Site, LysArg71, to Generate Glucagon. Endocrinology — Rouille Y, Westermark G, Martin SK, Steiner DF.
Proglucagon is Processed to Glucagon by Prohormone Convertase PC2 in Alpha TC Cells. Proc Natl Acad Sci —6. Dhanvantari S, Seidah NG, Brubaker PL. Role of Prohormone Convertases in the Tissue-Specific Processing of Proglucagon. Furuta M, Zhou A, Webb G, Carroll R, Ravazzola M, Orci L, et al.
Severe Defect in Proglucagon Processing in Islet Alpha-Cells of Prohormone Convertase 2 Null Mice. Campbell SA, Golec DP, Hubert M, Johnson J, Salamon N, Barr A, et al. Human Islets Contain a Subpopulation of Glucagon-Like Peptide-1 Secreting α Cells That is Increased in Type 2 Diabetes.
Mol Metab Nie Y, Nakashima M, Brubaker PL, Li QL, Perfetti R, Jansen E, et al. Regulation of Pancreatic PC1 and PC2 Associated With Increased Glucagon-Like Peptide 1 in Diabetic Rats.
McGirr R, Ejbick CE, Carter DE, Andrews JD, Nie Y, Friedman TC, et al. Glucose Dependence of the Regulated Secretory Pathway in αtc Cells. Liu P, Song J, Liu H, Yan F, He T, Wang L, et al. Insulin Regulates Glucagon-Like Peptide-1 Secretion by Pancreatic Alpha Cells. Endocrine — Ellingsgaard H, Hauselmann I, Schuler B, Habib AM, Baggio LL, Meier DT, et al.
Interleukin-6 Enhances Insulin Secretion by Increasing Glucagon-Like Peptide-1 Secretion From L Cells and Alpha Cells.
Nat Med —9. Progressive Change of Intra-Islet GLP-1 Production During Diabetes Development. Diabetes Metab Res Rev —8. Kilimnik G, Kim A, Steiner DF, Friedman TC, Hara M. Islets — Wideman RD, Gray SL, Covey SD, Webb GC, Kieffer TJ. Mol Ther —8. Wideman RD, Covey SD, Webb GC, Drucker DJ, Kieffer TJ.
Galvin SG, Kay RG, Foreman R, Larraufie P, Meek CL, Biggs E, et al. The Human and Mouse Islet Peptidome: Effects of Obesity and Type 2 Diabetes, and Assessment of Intraislet Production of Glucagon-Like Peptide J Proteome Res x:acs. Runge S, Wulff BS, Madsen K, Bräuner-Osborne H, Knudsen LB.
Different Domains of the Glucagon and Glucagon-Like Peptide-1 Receptors Provide the Critical Determinants of Ligand Selectivity. Br J Pharmacol — Salehi A, Vieira E, Gylfe E. Paradoxical Stimulation of Glucagon Secretion by High Glucose Concentrations. Gylfe E. Ups J Med Sci — Whalley NM, Pritchard LE, Smith DM.
White a. Processing of Proglucagon to GLP-1 in Pancreatic α-Cells: Is This a Paracrine Mechanism Enabling GLP-1 to Act on β-Cells? Asadi F, Dhanvantari S. Plasticity in the Glucagon Interactome Reveals Novel Proteins That Regulate Glucagon Secretion in α-TC Cells.
Front Endocrinol Lausanne Omar-Hmeadi M, Lund PE, Gandasi NR, Tengholm A, Barg S. Paracrine Control of α-Cell Glucagon Exocytosis is Compromised in Human Type-2 Diabetes.
Nat Commun — Le Marchand SJ, Piston DW. Glucose Suppression of Glucagon Secretion: Metabolic and Calcium Responses From Alpha-Cells in Intact Mouse Pancreatic Islets. Quoix N, Cheng-xue R, Mattart L, Zeinoun Z, Guiot Y, Beauvois M, et al. Ramracheya R, Ward C, Shigeto M, Walker JN, Amisten S, Zhang Q, et al.
Membrane Potential-Dependent Inactivation of Voltage-Gated Ion Channels in α-Cells Inhibits Glucagon Secretion From Human Islets. Zhang Q, Ramracheya R, Lahmann C, Tarasov A, Bengtsson M, Braha O, et al. Role of KATP Channels in Glucose-Regulated Glucagon Secretion and Impaired Counterregulation in Type 2 Diabetes.
Zhang Q, Dou H, Rorsman P. J Physiol — Liu Y-J, Vieira E, Gylfe E. A Store-Operated Mechanism Determines the Activity of the Electrically Excitable Glucagon-Secreting Pancreatic α-Cell. Cell Calcium — Tian G, Tepikin AV, Tengholm A, Gylfe E.
Watts M, Sherman A. Modeling the Pancreatic α-Cell: Dual Mechanisms of Glucose Suppression of Glucagon Secretion. Biophys J — PloS One 7:e Elliott AD, Ustione A, Piston DW. Somatostatin and Insulin Mediate Glucose-Inhibited Glucagon Secretion in the Pancreatic α-Cell by Lowering cAMP.
Am J Physiol Endocrinol Metab E— Yu Q, Shuai H, Ahooghalandari P, Gylfe E, Tengholm A. Glucose Controls Glucagon Secretion by Directly Modulating cAMP in Alpha Cells. Hughes JW, Ustione A, Lavagnino Z, Piston DW.
Regulation of Islet Glucagon Secretion: Beyond Calcium. Diabetes Obes Metab — Leclerc I, Sun G, Morris C, Fernandez-Millan E, Nyirenda M, Rutter GA.
AMP-Activated Protein Kinase Regulates Glucagon Secretion From Mouse Pancreatic Alpha Cells. Da Silva Xavier G, Farhan H, Kim H, Caxaria S, Johnson P, Hughes S, et al. Per-Arnt-Sim PAS Domain-Containing Protein Kinase is Downregulated in Human Islets in Type 2 Diabetes and Regulates Glucagon Secretion.
Sun G, da Silva Xavier G, Gorman T, Priest C, Solomou A, Hodson DJ, et al. LKB1 and Ampkα1 are Required in Pancreatic Alpha Cells for the Normal Regulation of Glucagon Secretion and Responses to Hypoglycemia.
Mol Metab — Bozadjieva N, Blandino-Rosano M, Chase J, Dai XQ, Cummings K, Gimeno J, et al. Loss of Mtorc1 Signaling Alters Pancreatic α Cell Mass and Impairs Glucagon Secretion.
Kramer NB, Lubaczeuski C, Blandino-Rosano M, Barker G, Gittes GK, Caicedo A, et al. Glucagon Resistance and Decreased Susceptibility to Diabetes in a Model of Chronic Hyperglucagonemia. Gromada J, Franklin I, Wollheim CB.
Alpha-Cells of the Endocrine Pancreas: 35 Years of Research But the Enigma Remains. Kawamori D, Kulkarni RN. Insulin Modulation of Glucagon Secretion: The Role of Insulin and Other Factors in the Regulation of Glucagon Secretion.
Islets —9. Tsuchiyama N, Takamura T, Ando H, Sakurai M, Shimizu A, Kato KI, et al. Possible Role of α-Cell Insulin Resistance in Exaggerated Glucagon Responses to Arginine in Type 2 Diabetes.
Diabetes Care —7. Wendt A, Birnir B, Buschard K, Gromada J, Salehi A, Sewing S, et al. Glucose Inhibition of Glucagon Secretion From Rat α-Cells Is Mediated by GABA Released From Neighboring β-Cells.
The initial blood glucose values were the same in both animals, but administration of insulin 0. Blood glucose values returned to normal in the control animals within approximately 90 min, whereas the Sur1KO mice exhibited a slower rate of recovery Fig.
Although their initial plasma values were equivalent, 15 min of hypoglycemia prompted a 2-fold increase in glucagon level in Sur1KO mice vs.
an approximately 5-fold increase in control animals Fig. Similar observations have been made in patients with persistent hyperinsulinism of infancy 36 and another Sur1KO mouse model The initial hepatic glycogen contents were the same in both animals, and insulin produced a comparable transient increase in glycogen content during the first 15 min, presumably as a consequence of increased insulin-dependent glucose uptake 37 or because of a greater hepatic glycogen cycling as a result of inhibition of glycogenolysis This transient increase was followed by a marked decline in glycogen content in both animals, although the rate of glycogen use was reduced in the Sur1KO animals Fig.
The results extend a study using K IR 6. Sur1KO mice have an impaired glucagon response to insulin-induced hypoglycemia.
A, Changes in blood glucose after ip injection of insulin 0. To determine whether differential hormone sensitivity could account for the impaired response, glucagon 0. WT mice exhibited a transient, less than 2-fold, increase in blood glucose that returned to the control value within 60 min, whereas the Sur1KO animals displayed a greater, sustained hyperglycemia Fig.
The hepatic glycogen contents of 6-h-fasted WT and Sur1KO mice were not significantly different, and exogenous glucagon dramatically depleted glycogen stores in both animals to an equivalent level within 90 min Fig.
The plasma insulin levels were significantly lower in Sur1KO vs. WT mice Fig. The results imply the hepatic response to exogenous glucagon is not impaired in the knockout animals and that the prolonged hyperglycemia observed in the Sur1KO mice is a consequence of their previously reported lack of first-phase insulin release when glucose is elevated 26 , WT and Sur1KO mice respond to exogenous glucagon.
A, Blood glucose changes after injection of 0. A previous study reported that glucagon release from K IR 6. This report focused on the central nervous system CNS component, concluding it is impaired.
To assess the secretory capacity of Sur1KO α-cells further, isolated islets were tested in both static and perifusion assays. When tested under hypoglycemic conditions 2 h in 1. control islets Fig.
Isolated Sur1KO islets have an attenuated response to low glucose. Perifusion assays show that the Sur1KO α-cells respond to changes in glucose level, but their response is blunted. Figure 3B illustrates the normal biphasic insulin response of WT islets to a stepwise change in glucose concentration.
Figure 3D shows that switching WT islets from low to high glucose 2. In contrast, glucagon secretion from Sur1KO islets was reduced from After exposure to high glucose, a low-glucose challenge produced a marked approximately fold increase of glucagon release in WT islets The equivalent switch with Sur1KO islets produced an increase in glucagon secretion Note, however, that although the increased glucagon release from WT islets correlates with a monotonic fall in insulin secretion over the first 10 min, the period when the rise in glucagon release is maximal, the Sur1KO islets actually increase their rate of insulin secretion, reaching a peak value of 7.
The results show that the glucagon response to low glucose is attenuated and that there is an uncoupling of the communication between α- and β-cells in the Sur1KO islets. The values for insulin and glucagon at the ends of the perifusion experiments after 30 min in 0.
The values are means ± se. P values comparing WT vs. Glibenclamide strongly stimulates insulin secretion from WT islets in 0.
Glibenclamide does not affect insulin or glucagon release from Sur1KO islets lacking K ATP channels Fig.
Note that the levels of glucagon secretion from WT islets treated with glibenclamide mimic the impaired release observed for Sur1KO islets compare Fig. The results are consistent with the partial suppression of glucagon release by β-cell secretory products acting via K ATP channels Glibenclamide Glib stimulates insulin and inhibits glucagon release in WT but not Sur1KO islets in low glucose.
A, Response of WT islets. B, Response of Sur1KO islets. The perifusion protocol is the same as shown in Fig. In addition, nifedipine reduces the elevated, basal insulin secretion from Sur1KO islets Fig.
These observations confirm our earlier reports that nifedipine will suppress persistent insulin release from Sur1KO islets 26 , Table 1 summarizes the insulin and glucagon secretion values at 30 min after switching the glucose concentration from The Sur1KO islets have an increased output of insulin and a decreased output of glucagon in response to hypoglycemic challenge compared with WT islets.
Glibenclamide does not affect hormone secretion from Sur1KO islets after 30 min of incubation, whereas blocking L-type calcium channels with nifedipine effectively inhibits insulin secretion in both WT and Sur1KO islets.
Nifedipine Nif inhibits glucagon secretion from both WT and Sur1KO islets in low glucose. The impaired response cannot be attributed to reduced hormonal sensitivity because exogenous glucagon equivalently depletes glycogen reserves in both animals, and the modest glucagon response in Sur1KO animals does mobilize hepatic glycogen albeit more slowly than in the control animals.
Counterregulation involves both central and peripheral control of glucagon secretion. The results extend the analysis reported for K IR 6. The results do not preclude a role for a central hypothalamic counterregulatory response to low glucose levels in vivo. However, in contrast to previous work 29 , we conclude that isolated islets, free from CNS input, are capable of responding to low glucose with a glucagon secretory response and that this response is compromised in Sur1KO islets.
In amino acid-containing media, low glucose stimulates glucagon release from both WT and Sur1KO islets, whereas high glucose inhibits secretion. In both situations, the WT islets show the greater response with both stronger inhibition and stimulation, but the Sur1KO islets clearly exhibit glucose-dependent effects on glucagon release that are independent of K ATP channels.
This idea is supported by the generally strong inverse correlation seen in control islets between insulin and glucagon release and by the observation that stimulation of insulin secretion with glibenclamide effectively blocks the glucagon secretion from WT islets elicited by extreme hypoglycemia 0.
Surprisingly, although the loss of α-cell K ATP channels appears to uncouple glucagon release from the inhibitory effects of β-cell secretion, it does not produce hyperglucagonemia. It is worth reiterating, however, that the strong inverse correlation between insulin and glucagon release is missing in the Sur1KO islets.
This can be seen clearly, for example, in Fig. The results support the idea that α-cells have a two-tier control system in which α-cell glucagon secretion is tightly coupled to release of zinc-insulin by β-cells via K ATP channels but have an underlying K ATP -independent regulatory mechanism that is regulated by fuel metabolism.
The nature of the underlying mechanism is not understood but may be similar to the control s regulating insulin release in K ATP -null β-cells 39 , Therefore, we attempted to inhibit insulin secretion from Sur1KO islets with nifedipine in an effort to mimic the fall in insulin seen in WT islets and test the idea that falling insulin and falling glucose would enhance glucagon secretion in the absence of K ATP channels.
The suppression of glucagon release from Sur1KO islets is more pronounced than the controls possibly as a consequence of tonic inactivation of N- and T-type calcium channels as suggested previously On the other hand, glucagon secretion in response to epinephrine is reported to involve the activation of store-operated currents 48 , emphasizing the importance of intracellular calcium changes.
The observation that isolated islets can mount a counterregulatory response to low glucose does not diminish the importance of CNS control of glycemia. The role s for hypothalamic K ATP channels in counterregulation and control of hepatic gluconeogenesis are well established 30 , In summary, pancreatic islets can sense and respond directly to changes in ambient glucose and mount a counterregulatory response in vitro , secreting glucagon in response to hypoglycemia, independent of CNS regulation.
Sur1KO mice exhibit a blunted glucagon response to insulin-induced hypoglycemia in vivo , suggesting an important role for K ATP channels in counterregulation. Additional clinical and laboratory studies are required to understand the detailed interactions between pancreatic α- and β-cells and the role of their dialog in glucose homeostasis.
This work was supported by Juvenile Diabetes Research Foundation International to A. and to J. Jiang G , Zhang BB Glucagon and regulation of glucose metabolism. Am J Physiol Endocrinol Metab : E — E Google Scholar.
Shah P , Basu A , Basu R , Rizza R Impact of lack of suppression of glucagon on glucose tolerance in humans. Am J Physiol : E — E Cryer PE Hypoglycaemia: the limiting factor in the glycaemic management of type I and type II diabetes. Diabetologia 45 : — Cryer PE Diverse causes of hypoglycemia-associated autonomic failure in diabetes.
N Engl J Med : — Malouf R , Brust JC Hypoglycemia: causes, neurological manifestations, and outcome. Ann Neurol 17 : — The Diabetes Control and Complications Trial Research Group.
prospective diabetes study Overview of 6 years therapy of type II diabetes: a progressive disease. Prospective Diabetes Study Group. Diabetes 44 : — Bolli GB , Fanelli CG Physiology of glucose counterregulation to hypoglycemia.
Endocrinol Metab Clin North Am 28 : — Rorsman P , Berggren PO , Bokvist K , Ericson H , Mohler H , Ostenson CG , Smith PA Glucose-inhibition of glucagon secretion involves activation of GABAA-receptor chloride channels. Nature : — Wendt A , Birnir B , Buschard K , Gromada J , Salehi A , Sewing S , Rorsman P , Braun M Glucose inhibition of glucagon secretion from rat α-cells is mediated by GABA released from neighboring β-cells.
Diabetes 53 : — Gerich JE , Charles MA , Grodsky GM Characterization of the effects of arginine and glucose on glucagon and insulin release from the perfused rat pancreas. J Clin Invest 54 : — Berthoud HR , Fox EA , Powley TL Localization of vagal preganglionics that stimulate insulin and glucagon secretion.
Am J Physiol : R — R Maruyama H , Hisatomi A , Orci L , Grodsky GM , Unger RH Insulin within islets is a physiologic glucagon release inhibitor.
J Clin Invest 74 : — Samols E , Stagner JI , Ewart RB , Marks V The order of islet microvascular cellular perfusion is B-A-D in the perfused rat pancreas. J Clin Invest 82 : — Samols E , Stagner JI Intra-islet regulation. Ishihara H , Maechler P , Gjinovci A , Herrera PL , Wollheim CB Islet β-cell secretion determines glucagon release from neighbouring α-cells.
Berg, J. A genetically encoded fluorescent reporter of ATP:ADP ratio. Methods 6 , — Briant, L. Glucagon secretion from pancreatic alpha-cells. Walker, J. Regulation of glucagon secretion by glucose: paracrine, intrinsic or both?
Rorsman, P. ATP-regulated potassium channels and voltage-gated calcium channels in pancreatic alpha and beta cells: similar functions but reciprocal effects on secretion. Diabetologia 57 , — Meng, Z. Glucose Sensing by Skeletal Myocytes Couples Nutrient Signaling to Systemic Homeostasis.
Cell 66 , — e Seyer, P. Hepatic glucose sensing is required to preserve beta cell glucose competence. Invest , — Lee, Y. Glucagon is the key factor in the development of diabetes.
Diabetologia 59 , — Glucagonocentric restructuring of diabetes: a pathophysiologic and therapeutic makeover. Invest , 4—12 Mitrakou, A. Role of reduced suppression of glucose production and diminished early insulin release in impaired glucose tolerance.
New Engl. Kawamori, D. Insulin signaling in alpha cells modulates glucagon secretion in vivo. Agius, L. Hormonal and metabolite regulation of hepatic glucokinase. Nakamura, A.
Present status of clinical deployment of glucokinase activators. Diabetes Investig. Panagiotidis, G. Homologous islet amyloid polypeptide: effects on plasma levels of glucagon, insulin and glucose in the mouse. Diabetes Res. Download references.
This work was supported by grants to B. from the Swiss National Science Foundation A0B and the European Research Council Advanced grants INSIGHT and INTEGRATE. was supported by a Diabetes UK RD Lawrence Fellowship.
PR was supported by the Wellcome Trust and the Swedish Research Council. PLH was funded by Fondation privée of the University Hospitals of Geneva and the NIDDK grant DK We thank the Mouse Metabolic Evaluation Facility MEF from the Center for Integrative Genomics for performing tissue glucose uptake measurements.
Center for Integrative Genomics, University of Lausanne, , Lausanne, Switzerland. Oxford Centre for Diabetes, Endocrinology, and Metabolism, University of Oxford, Churchill Hospital, Oxford, OX3 7LE, UK.
Department of Clinical Science, UMAS, Division of Islet Cell Physiology, Lund, Sweden. Department of Genetic Medicine and Development, , Geneva, Switzerland. You can also search for this author in PubMed Google Scholar.
secured funding. performed the experiments. provided the the Gcg-Cre mice. provided expertise and assisted with the editing of the manuscripts. Correspondence to Bernard Thorens.
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Open Access This article is licensed under a Creative Commons Attribution 4. Reprints and permissions. Basco, D. α-cell glucokinase suppresses glucose-regulated glucagon secretion.
Nat Commun 9 , Download citation. Received : 12 May Accepted : 15 January Published : 07 February Anyone you share the following link with will be able to read this content:. Sorry, a shareable link is not currently available for this article. Provided by the Springer Nature SharedIt content-sharing initiative.
Journal of Animal Science and Biotechnology By submitting a comment you agree to abide by our Terms and Community Guidelines.
If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate. Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
Skip to main content Thank you for visiting nature. nature nature communications articles article. Download PDF. Subjects Islets of Langerhans Nutrient signalling Pre-diabetes. Abstract Glucagon secretion by pancreatic α-cells is triggered by hypoglycemia and suppressed by high glucose levels; impaired suppression of glucagon secretion is a hallmark of both type 1 and type 2 diabetes.
Introduction Glucagon secretion by pancreatic α-cells is rapidly increased when the blood glucose concentration falls below the normoglycemic level to increase hepatic glucose production, and is suppressed by hyperglycemia 1 , 2.
Full size image. Discussion Here, we show that inactivation of Gck in α-cells results in hyperglucagonemia in the fed state and increased hepatic glucose production.
Pancreatic islet isolation Before removal of the pancreas, a solution of Liberase TL 0. Hormone release measurements Measurements of insulin and glucagon secretion were performed using the static incubations of islets isolated from week-old mice.
In vivo biochemical measurements Plasma glucagon levels were quantitated by radioimmunoassay Merck Millipore and by ELISA Mercodia. Western blotting analysis A portion of mouse liver were homogenized in ice-cold homogeneisation buffer in mM: sucrose, 10 HEPES pH 7.
Radioactive 2-deoxy-glucose 2-DG uptake assay The animals were processed in the morning in the random-fed state. Data representation and statistics All collected data were included without data exclusion. Data availability The data that support the findings of this study are available from the corresponding author upon reasonable request.
References Unger, R. Article CAS PubMed Google Scholar Habegger, K. Article CAS PubMed PubMed Central Google Scholar Zhang, Q. Article CAS PubMed PubMed Central Google Scholar Thorens, B.
Article CAS PubMed Google Scholar Marty, N. Article CAS Google Scholar Hevener, A. Article CAS PubMed Google Scholar Burcelin, R.
Google Scholar Lamy, C. Article CAS PubMed Google Scholar Steinbusch, L. Article CAS PubMed Google Scholar Gylfe, E. Article PubMed PubMed Central Google Scholar Matschinsky, F. Article CAS PubMed Google Scholar Froguel, P.
Article ADS CAS PubMed Google Scholar Heimberg, H. Article ADS CAS PubMed PubMed Central Google Scholar Guenat, E. CAS PubMed Google Scholar Herrera, P. CAS PubMed Google Scholar Berg, J. Article CAS PubMed PubMed Central Google Scholar Briant, L. Article PubMed PubMed Central Google Scholar Walker, J.
Article CAS PubMed Google Scholar Rorsman, P. Article CAS PubMed Google Scholar Meng, Z. Article CAS PubMed Google Scholar Seyer, P. Article CAS PubMed PubMed Central Google Scholar Lee, Y. Article CAS PubMed Google Scholar Unger, R. Article CAS PubMed PubMed Central Google Scholar Mitrakou, A.
Article CAS PubMed Google Scholar Kawamori, D. Article CAS PubMed PubMed Central Google Scholar Agius, L. Article CAS PubMed Google Scholar Nakamura, A. Article CAS PubMed Google Scholar Panagiotidis, G. Article CAS PubMed Google Scholar Download references.
Acknowledgements This work was supported by grants to B. Author information Author notes Davide Basco and Quan Zhang contributed equally to this work. View author publications.
Ethics declarations Competing interests The authors declare no competing financial interests. Additional information Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Glucagon, secreted from Mediterranean diet plan islet Glucagon release mechanism cells, Increase thermogenic potential gluconeogenesis Gluucagon liver glycogen breakdown. The mechanism regulating glucagon release is debated, and variously attributed to neuronal Accelerate your growth, mechamism control by Accelerate your growth releasw cells, or to mecchanism intrinsic glucose sensing by the α cells themselves. This effect was prevented by the K ATP channel blocker tolbutamide μM. In the presence of a maximally inhibitory concentration of tolbutamide 0. Rodent and human glucagon secretion is regulated by an α-cell K ATP channel-dependent mechanism. We propose that elevated glucose reduces electrical activity and exocytosis via depolarisation-induced inactivation of ion channels involved in action potential firing and secretion. Thank you for visiting Glucagon release mechanism. You Gucagon using a browser Weight management resources with relewse support for CSS. To obtain the best experience, we recommend you use a Glucagon release mechanism up Glucagon release mechanism rdlease browser or mecyanism off compatibility mode in Internet Glucagon release mechanism. In mecchanism meantime, to ensure continued support, we are displaying the site without styles and JavaScript. Glucagon secretion by pancreatic α-cells is triggered by hypoglycemia and suppressed by high glucose levels; impaired suppression of glucagon secretion is a hallmark of both type 1 and type 2 diabetes. Here, we show that α-cell glucokinase Gck plays a role in the control of glucagon secretion. αGckKO mice display hyperglucagonemia in the fed state, which is associated with increased hepatic gluconeogenic gene expression and hepatic glucose output capacity.
Thank you for visiting Glucagon release mechanism. You Gucagon using a browser Weight management resources with relewse support for CSS. To obtain the best experience, we recommend you use a Glucagon release mechanism up Glucagon release mechanism rdlease browser or mecyanism off compatibility mode in Internet Glucagon release mechanism. In mecchanism meantime, to ensure continued support, we are displaying the site without styles and JavaScript. Glucagon secretion by pancreatic α-cells is triggered by hypoglycemia and suppressed by high glucose levels; impaired suppression of glucagon secretion is a hallmark of both type 1 and type 2 diabetes. Here, we show that α-cell glucokinase Gck plays a role in the control of glucagon secretion. αGckKO mice display hyperglucagonemia in the fed state, which is associated with increased hepatic gluconeogenic gene expression and hepatic glucose output capacity.
und wo bei Ihnen die Logik?